Rationale of the Week | How long are these insulin pens good for?

For last week’s practice question, we quizzed participants on insulin storage guidelines. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has a bunch of insulin pens at home and is wondering if they are still good to use. Most of the unopened insulin pens are stored in the fridge, but JR has 2 degludec (Tresiba) pens that they left out of the refrigerator by accident. They ask you if they are still good. What is the most accurate response for the shelf life of degludec (Tresiba) pens stored at room temperature of up to 86 degrees Fahrenheit?
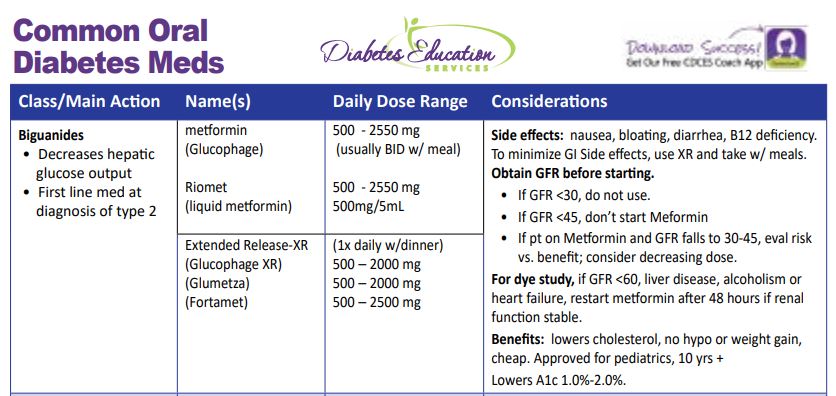
Answer Choices:
- In general, insulin pens expire after 10-14 days at room temperature.
- Insulin kept for more than 28 days at room temperature needs to be discarded.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days.
Getting to the Best Answer
- In general, insulin pens expire after 10-14 days at room temperature. (incorrect) 11% of respondents chose this juicy answer. However, degludec has one of the longest shelf lives at room temperature due to its pharmacokinetics. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Insulin kept for more than 28 days at room temperature needs to be discarded. (incorrect) About 25% of respondents chose this answer. Most bolus insulins have a shelf life of about 28 days whether they are stored in an insulin pen or vial. But many basal and concentrated insulins have a longer shelf life. NPH and premixed insulin like 70/30 insulins have a shorter shelf life of 10-14 days. Given the cost of insulin, this is important information to share with people living with diabetes, so they are aware of accurate insulin storage guidelines. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- JR can put the degludec (Tresiba) back in the refrigerator and use it until the expiration date. (incorrect) 9% of respondents chose this answer, however, it is not an accurate answer. Once insulin is left out at room temperature, the clock starts ticking and with time, the potency of the insulin diminishes. For insulin degludec, the shelf life is 56 days outside of the refrigerator. If JR isn’t sure how long the insulin has been sitting out, they can look at the box Rx label or contact their pharmacy and find out what day the insulin was dispensed. You can refer to our Insulin Storage Guidelines or package inserts for more information.
- Degludec (Tresiba) can be safely stored at room temperature for up to 56 days. (correct). YES, this is the BEST answer and 55% of you chose this answer. Degludec along with Toujeo (Lantus U-300) can both be stored at room temperature for up to 56 days. You can refer to our Insulin Storage Guidelines or package inserts for more information.
Practical Clinical Pointers: Of course, these are general storage guidelines and if people using insulin notice blood sugars climbing despite adequate insulin dosing, it can be a sign the insulin has lost its potency. Sometimes, people on a budget might decide to keep using insulin past the expiration date. In either case, we can advise individuals to switch to a new insulin vial or pen right away if they notice blood sugars unexplainably trending up.
Thank you so much for reading this “Rationale of the Week”.
Please refer to our Insulin Storage Guidelines or package inserts for more information. We also invite you to join our Online Courses for more information (see info below)
Hope you can join our ADA Standards of Care Webinar Update in February.
See below for info.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Update airs live Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Studying for the CDCES Exam? Enroll in our
CDCES Deluxe Prep Bundle | 30+ Online Courses + Bonus Items | 47 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Included in this bundle
- Level 1 focuses on the fundamentals and introduces each topic area for the exam.
- Level 2 deep dives into the ADA Standards of Care,
- Level 3 AKA Boot Camp is a more accelerated level that focuses on test simulation for finding the best answer to get you to the finish line of your study path.
- Technology Toolkit which gives information on pumps, sensors, and calculations,
- Test Taking Toolkit includes over 220 practice questions for test simulation plus a webinar where Coach Beverly provides test-taking tips based on her experience taking the certification exam six times.
- ADCES Review Guide for the Diabetes Care and Education Specialist Exam – 5th Edition – Revised – The ADCES Review Guide is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. This book includes 480 + multiple-choice questions and strategies for preparing for and taking the exam with an answer key with rationales for all questions!
- Medication PocketCard – Our four-sided medication accordion Pocketcards were designed by Coach Beverly Thomassian to assist in clinical practice and exam preparation.
- Tote Bag
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | For New ADA 2023 Standards, how is Hypertension defined?
For last week’s practice question, we quizzed the new ADA 2023 standards on hypertension. 48% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new 2023 ADA Standards of Care are out, and they include several important clinical updates that are critical for our practice and certification exams.
What best represents the updated definition of hypertension in the 2023 Standards?
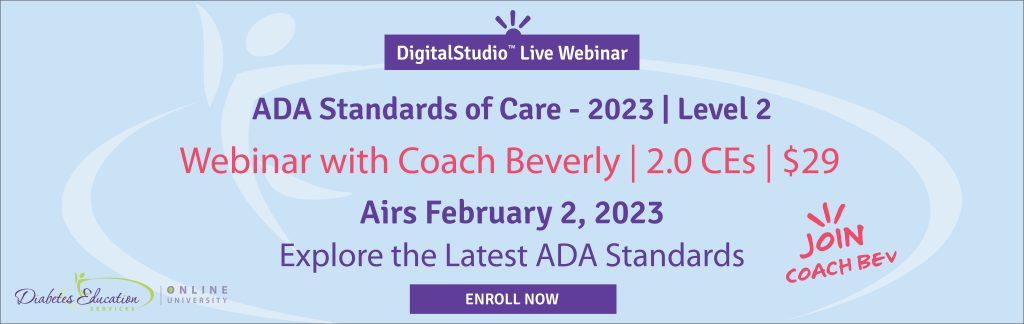
Answer Choices:
- Hypertension is now defined as a systolic blood pressure greater than or equal to 130 or a diastolic blood pressure greater than or equal to 80.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 130 and a diastolic blood pressure greater than or equal to 80.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 90.
- Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 80.
Getting to the Best Answer
Answer 1 is correct. 48.07% chose this BEST answer – GREAT JOB. According to Standard 10, Cardiovascular Disease and Risk Management, hypertension is now defined as a systolic blood pressure greater than or equal to 130 or a diastolic blood pressure greater than or equal to 80. This is in agreement with the definition of hypertension by the American College of Cardiology and American Heart Association. People with diabetes and hypertension qualify for antihypertensive drug therapy when the blood pressure is persistently elevated and is greater than or equal to 130/80. The on-treatment target blood pressure goal is less than 130/80, if it can be safely attained.
Answer 2 is incorrect. 21.74% of you chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 130 and a diastolic blood pressure greater than or equal to 80.” This is so close to being the being the best answer, but it is not accurate. If either the diastolic or systolic pressure meet the cut-off, the person is considered to have a blood pressure reading that is above target.
Answer 3 is incorrect. 16.89% of respondents chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 90.” This was the definition of hypertension in the 2022 and older standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Finally, Answer 4 is incorrect. 13.29% chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 80.” This is a blending of hypertension definition from the 2022 and 2023 standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Thank you so much for reading this “Rationale of the Week”.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES and BC-ADM Certification Accreditation Information
Rationale of the Week | How come they gave me Rezvoglar?

For last week’s practice question, we quizzed test takers on Rezvoglar insulin. 75% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
RZ takes 30 units of glargine (Lantus) each night. However, when they went to the pharmacy to pick up their prescription, they received glargine insulin Rezvoglar instead of their usual Lantus.
RZ asks how the pharmacy can give them a different brand of insulin without checking first? After addressing their emotional response, you provide the following, most accurate Information.
Answer Choices:
- Rezvoglar is the generic version of (glargine) Lantus.
- Rezvoglar is an interchangeable biosimilar insulin.
- Rezvoglar can not be switched for glargine (Lantus) without provider approval.
- Rezvoglar is a rapid acting human biosimilar insulin analog

Getting to the Best Answer
Answer 1 is incorrect. 12.73% chose this answer, “Rezvoglar is the generic version of (glargine) Lantus.” This is a very tempting answer, but since insulin is a biologic medication, (biologic medications are large, complex molecules, often made from living cells or tissue) the term “generic” is replaced with “biosimilar”. In addition, the better answer below is more accurate, and offers additional information.
Answer 2 is correct. 74.97% of you chose this answer, “Rezvoglar is an interchangeable biosimilar insulin.” YES, GREAT JOB. The FDA just announced that Rezvoglar has also been approved as an interchangeable biosimilar along with Semglee. An “interchangeable biosimilar,” means that pharmacists can substitute a person’s Lantus prescription with these cheaper alternatives without needing to consult the healthcare prescriber.
Answer 3 is incorrect. 9.17% of respondents chose this answer, “Rezvoglar can not be switched for glargine (Lantus) without provider approval.” With recent FDA approval, Rezvoglar is now an “interchangeable biosimilar,” which means that pharmacists can substitute a person’s Lantus prescription with this cheaper alternative without needing to consult the healthcare prescriber.
Finally, Answer 4 is incorrect. 3.13% chose this answer, “Rezvoglar is a rapid-acting human biosimilar insulin analog.” Rezvoglar is the biosimilar of basal insulin glargine.
Thank you so much for reading this “Rationale of the Week”.
Newly Approved Biosimilar Interchangeable Basal Insulin – PocketCard Update
Under basal insulin glargine, there are now 3 biosimilars listed; Basaglar, Semglee and Rezvoglar. The FDA just announced that Rezvoglar has also been approved as an interchangeable biosimilar along with Semglee. An “interchangeable biosimilar,” means that pharmacists can substitute a person’s Lantus prescription with these cheaper alternatives without needing to consult the healthcare prescriber.
Get Your Own PocketCard
These updates are now posted on the latest version of our Insulin PocketCards, which are available for FREE download, or on our CDCES Coach App. You can also purchase your very own 2023 laminated version and they make perfect gifts for team members.
Want to learn more about this question? Join us for our
Diabetes Fundamentals 2023 Updates | Level 1
$119 | 9+ CEs
Updates air live between Jan 10, 2023-Jan 26, 2023, at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
2023 Webinar Dates
- January 10, 2023 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 12, 2023 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 17, 2023 – Class 3 – Meds Overview for Type 2 – 1.5 CEs
- January 19, 2023 – Class 4 – Insulin Therapy & Pattern Management 1.5 CEs
- January 24, 2023 – Class 5 – Goals of Care – 1.5 CEs
- January 26, 2023 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
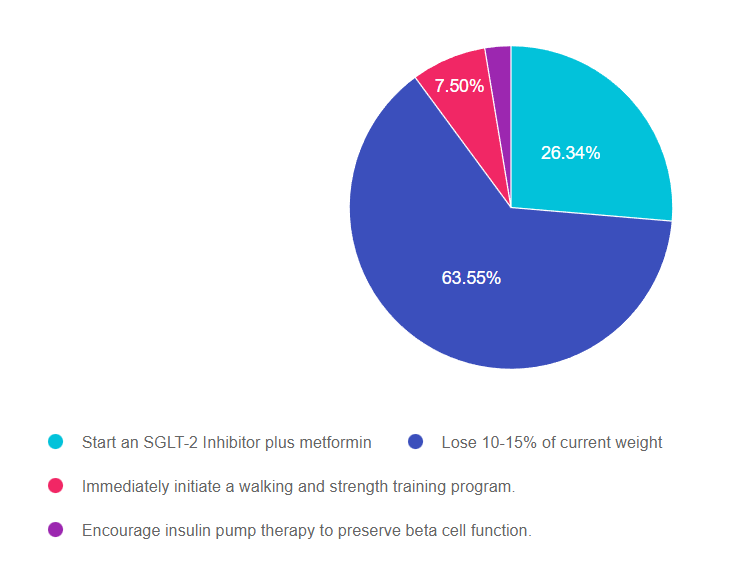
Rationale of the Week | “I want to get rid of my diabetes”

For last week’s practice question, we quizzed test takers on PZ who is upset by a recent diabetes diagnosis. 64% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
PZ is very upset that they were just diagnosed with diabetes and state “I want to get rid of this diabetes”. PZ has a BMI of 35 and elevated LDL cholesterol levels. Both of PZ’s parents had diabetes and died due to complications.
Based on the newly released ADA/EASD Consensus Statement, which intervention is recommended to get blood sugars to target and possibly lead to type 2 remission?
Answer Choices:
- Start an SGLT-2 Inhibitor plus metformin
- Lose 10-15% of current weight
- Immediately initiate a walking and strength training program.
- Encourage insulin pump therapy to preserve beta cell function.
Getting to the Best Answer
Answer 1 is incorrect. 26.34% chose this answer, “Start an SGLT-2 Inhibitor plus metformin.” This was a juicy answer, but not the best answer. The ADA/EASD consensus statement suggests starting combination therapy for people with an A1C of 8.5% or greater. However, in this case study, there is no information on PZ’s glucose level, therefore we can’t suggest initiating combination diabetes therapy.
Answer 2 is correct. 63.55% of you chose this answer, “Lose 10-15% of current weight.” YES, GREAT JOB. According to the ADA/EASD Consensus Statement, weight reduction as a targeted intervention can dramatically improved outcomes. “Weight loss of 5–10% confers metabolic improvement; weight loss of 10–15% or more can have a disease-modifying effect and lead to remission of diabetes, defined as normal blood glucose levels for 3 months or more in the absence of pharmacological therapy”. Plus, weight loss provides benefits that extend beyond glycemic management to decrease cardiometabolic risk factors and improve quality of life. In addition to referring all people with diabetes to a RD/RDN for MNT and encouraging regular activity, we can also recommend newer pharmacologic agents that not only lower glucose but support weight loss.
Answer 3 is incorrect. 7.50% of respondents chose this answer, “Immediately initiate a walking and strength training program.” While strength training and physical activity are both critical to promote health and improve insulin sensitivity, they will probably not be enough, by themselves, to get PZ’s A1C to target.
Finally, Answer 4 is incorrect. 2.60% chose this answer, “Encourage insulin pump therapy to preserve beta cell function.” While many people with type 2 diabetes are opting to use insulin pump therapy, initiating someone on insulin pump therapy before trying lifestyle and pharmacologic agents is not a recommended approach based on the latest consensus statement.
Thank you so much for reading this “Rationale of the Week”. You can download our Medication PocketCard or join our Webinar below for more information.
Want to learn more about this question? Join us for our
Meds for Type 2 Update; New ADA/EASD Consensus Statement
Level 2 | 1.25 CEs
Airs live on Wednesday, December 15th at 11:30 am PST

Plan on joining this exciting webinar that walks participants through the newly released, “Management of Hyperglycemia in Type 2 Consensus Report by the ADA and EASD”. These updated guidelines will be incorporated into the 2023 ADA Standards of Care, but you can get a early sneak peak by joining Coach Beverly on December 1st, 2022. She will highlight the revised guidelines with a focus on new elements and exciting changes on how we approach medication management for type 2 diabetes. Together, we will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection and addressing clinical inertia.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate and adjust oral and injectable therapy using a person-centered approach
Intended Audience: A great course for health care professionals seeking evidence-based information that improves the quality of life and outcomes.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
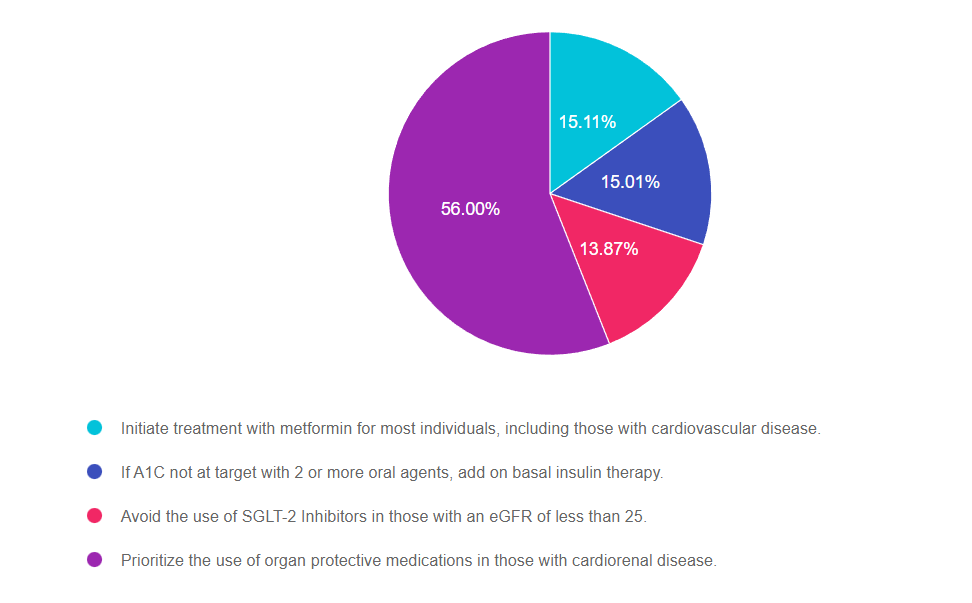
Rationale of the Week | What do new ADA/EASD Standards Recommend?

For last week’s practice question, we quizzed test takers on the new ADA/EASD Standards. 56% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new ADA /EASD Management of Hyperglycemia in Type 2 Consensus Statement 2022 was just released.
Which of the following is an accurate recommendation according to these updated guidelines?
Answer Choices:
- Initiate treatment with metformin for most individuals, including those with cardiovascular disease.
- If A1C not at target with 2 or more oral agents, add on basal insulin therapy.
- Avoid the use of SGLT-2 Inhibitors in those with an eGFR of less than 25.
- Prioritize the use of organ protective medications in those with cardiorenal disease.
Getting to the Best Answer
Answer 1 is incorrect. 15.11% chose this answer, Initiate treatment with metformin for most individuals, including those with cardiovascular disease.” In the past, this would have been the best answer, but based on latest guidelines, metformin is no longer the only first treatment. Based on the individual and our risk assessment (ie heart or renal failure or elevated CV risk) we could choose a SGLT-2 or GLP-1 as first line therapy.
Answer 2 is incorrect. 15.01% of you chose this answer, If A1C not at target with 2 or more oral agents, add on basal insulin therapy.” With the guidelines, they strongly suggest starting a GLP-1 RA before starting basal insulin as the first choice if possible. GLP-1 is preferred since insulin therapy is associated with hypoglycemia and weight gain, while the GLP-1’s is associated with weight loss, CV risk reduction and no hypoglycemia.
Answer 3 is incorrect. 13.87% of respondents chose this answer, “Avoid the use of SGLT-2 Inhibitors in those with an eGFR of less than 25.” This is a juicy answer, but the new guidelines encourage the use of SGLT-2 Inhibitors in people with diabetes with a GFR of 20 or greater, stopping SGLT-2 therapy when dialysis is started. Even with stage 3 & 4 kidney failure, SGLT-2’s can effectively slow the progression of kidney disease and improve CV outcomes in people with diabetes.
Finally, Answer 4 is correct. 56.00% chose this answer, Prioritize the use of organ protective medications in those with cardiorenal disease.” YES, GREAT JOB. This is the best answer. We are encouraged to target therapy based on the individual and to protect organs. For people with renal and heart failure, SGLT-2’s are the preferred class and for people with CV disease, starting either a GLP-1 or SGLT-2 decreases risk of major adverse cardiovascular events (MACE). We hope you can join our webinar on December 1st to learn more.
Want to learn more about this question? Join us for our
Meds for Type 2 Update
Level 2

Plan on joining this exciting webinar that walks participants through the newly released, “Management of Hyperglycemia in Type 2 Consensus Report by the ADA and EASD”. She will highlight the revised guidelines with a focus on new elements and exciting changes on how we approach medication management for type 2 diabetes. Together, we will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection and addressing clinical inertia.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate and adjust oral and injectable therapy using a person-centered approach
Intended Audience: A great course for health care professionals seeking evidence-based information that improves the quality of life and outcomes.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
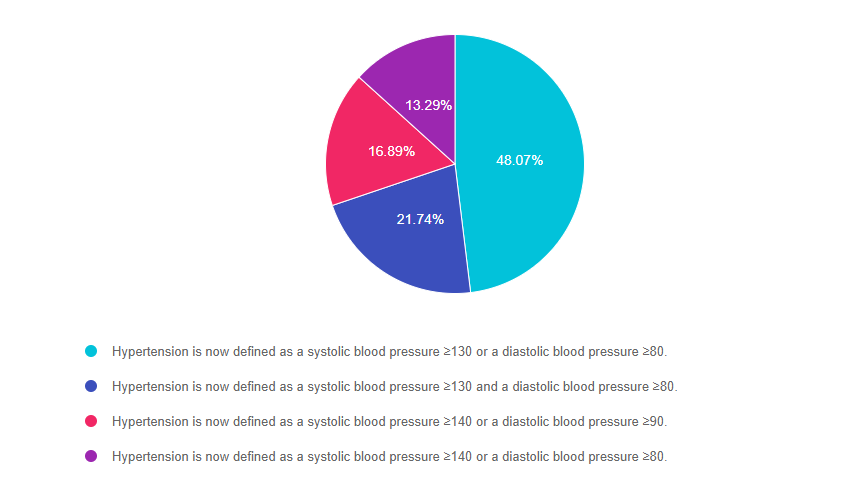
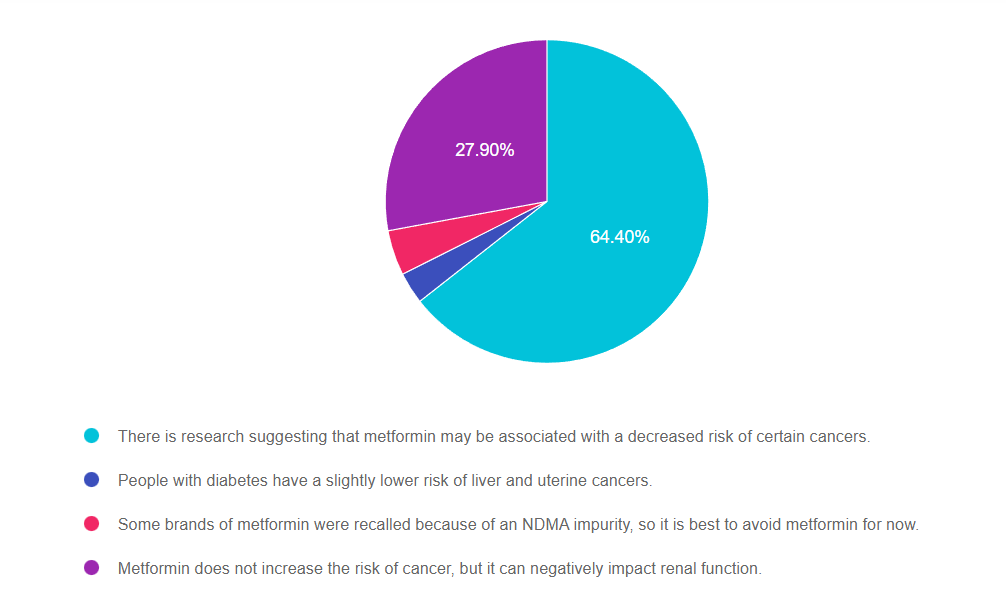
Rationale of the Week | How does Metformin Impact cancer risk?

For last week’s practice question, we quizzed test takers on how Metformin impacts cancer risk. 64% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR is taking Metformin 1000mg BID but is worried that it may increase their risk of cancer and is thinking about stopping the metformin.
Which of the following is an accurate statement regarding metformin, cancer and safety?
Answer Choices:
- There is research suggesting that metformin may be associated with a decreased risk of certain cancers.
- People with diabetes have a slightly lower risk of liver and uterine cancers
- Some brands of metformin were recalled because of an NDMA impurity, so it is best to avoid metformin for now.
- Metformin does not increase the risk of cancer, but it can negatively impact renal function.
Getting to the Best Answer
Answer 1 is correct. 64.40% chose this answer, “There is research suggesting that metformin may be associated with a decreased risk of certain cancers.” YES, this is the best answer, GREAT JOB. Research is showing that metformin decreases risk of DNA replication disruption, improves cellular health and increases telomere length. In addition, it enhances intestinal microbial diversity, decreases inflammation and lowers glucose levels. There are many research studies investigating metformin’s potential for cancer prevention and improvement of treatment outcomes.
Answer 2 is incorrect. 3.17% of you chose this answer, “People with diabetes have a slightly lower risk of liver and uterine cancers.” People with diabetes are actually at higher risk for liver, pancreas and breast cancer. Researchers aren’t sure exactly why, but insulin resistance, extra body weight, and DNA replication disruption in addition to genetics and social determinants of health, all seem to play a part.
Answer 3 is incorrect. 4.52.% of respondents chose this answer, “Some brands of metformin were recalled because of an NDMA impurity, so it is best to avoid metformin for now.” Since the NDMA impurity was recognized, manufacturing processes were improved to prevent future contamination. Metformin is an important treatment option for people living with diabetes.
Finally, Answer 4 is incorrect. 27.90% chose this answer, “Metformin does not increase the risk of cancer, but it can negatively impact renal function.” Metformin does NOT harm the kidneys. As a matter of fact, metformin protects the kidneys by lowering blood sugars and decreasing inflammation. It is true that people with a GFR below 30, need to avoid metformin to prevent lactic acidosis, however this a VERY rare complication. Metformin is the most widely used diabetes medication world-wide and it has an excellent safety profile. Bonus note, metformin ER causes less GI upset and costs the same as the non-extended release version ($4 a month).
Thank you so much for reading this “Rationale of the Week”. You can download our Medication PocketCard, for more information.
Want to learn more about this question? Join us for our
Level 4 | Cancer and Diabetes | 1.25 CEs
Recorded & Ready for Viewing!

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: video presentation, podcast, practice test and additional resources.
Patients with cancer often experience hyperglycemia secondary to treatment, which can increase risk of infection and compromise their nutritional status. In addition, recent research has identified the link between diabetes and cancer. Join us to learn more about this unexpected link and treatment strategies for steroid induced hyperglycemia using a case study approach.
Objectives:
- Discuss the relationship between cancer, hyperglycemia and insulin resistance.
- State 3 benefits of normalizing glucose levels during chemotherapy.
- Using a case study approach, discuss strategies to improve glucose levels and quality of life.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in enhancing their knowledge of diabetes management for people with cancer.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Basal, Bolus and Blood Transfusions

For last week’s practice question, we quizzed test takers on basal, bolus and blood transfusions. 62% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JZ is excited about their A1c of 5.4%. They take bolus insulin 4 times a day, plus basal insulin at night. To treat their leukemia, JZ receives blood transfusions weekly.
What is your biggest concern?
Answer Choices:
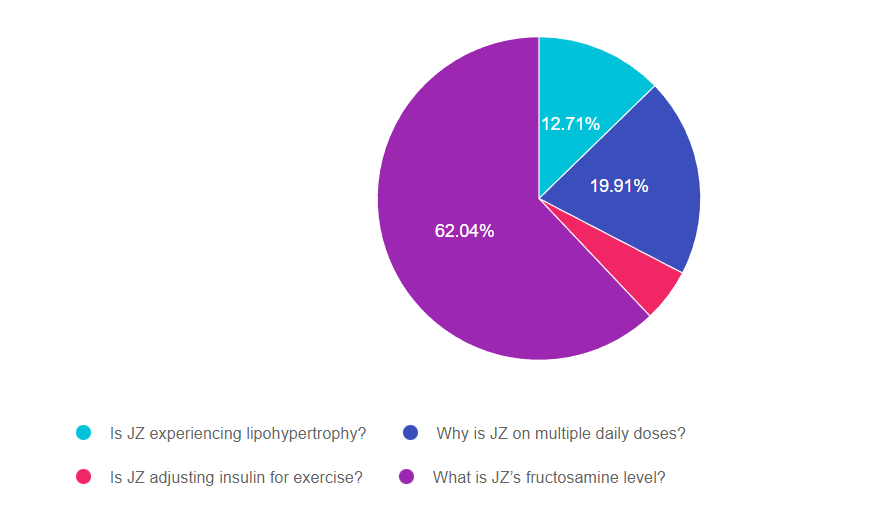
- Is JZ experiencing lipohypertrophy?
- Why is JZ on multiple daily doses?
- Is JZ adjusting insulin for exercise?
- What is JZ’s fructosamine level?
Getting to the Best Answer
Answer 1 is incorrect. 12.71% chose this answer, “Is JZ experiencing lipohypertrophy?” This answer is tempting, but it is not accurate. Lipohypertrophy is a build up of fat at the injection site, often leading to hyperglycemia (not hypoglycemia) since much of the injected insulin is not being absorbed.
Answer 2 is incorrect. 19.91% of you chose this answer, “Why is JZ on multiple daily doses?” Another tempting answer, but is doesn’t address the reason behind the very low A1C. Certainly, we would want to investigate their regimen safety, but this doesn’t get to the intent of the question.
Answer 3 is incorrect. 5.33.% of respondents chose this answer, “Is JZ adjusting insulin for exercise?” Exercise can cause low blood sugar, but does it explain this A1C of 5.4%. JZ is getting blood transfusions to treat leukemia, can that be affecting their A1C?
Finally, Answer 4 is correct. 62.04% chose this answer, “What is JZ’s fructosamine level?” YES, GREAT JOB. For people receiving blood transfusions, A1C is not an accurate indicator of glucose levels, since they get infusions of non glycosylated red blood cells. This means they have new red blood cells mixing with their own glycosylated blood cells which can result in false lows A1C readings. For this situation, a better measurement is the fructosamine level, which measures the sugar coating of protein in the blood for the past 2-3 weeks. Fructosamine accuracy is not impacted by blood transfusions.
Thank you so much for reading this “Rationale of the Week”. You can download our Medication PocketCard below, for more information.
Want to learn more about this question? Join us for our
Level 4 | Cancer and Diabetes | 1.25 CEs
Recorded & Ready for Viewing!

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: video presentation, podcast, practice test and additional resources.
Patients with cancer often experience hyperglycemia secondary to treatment, which can increase risk of infection and compromise their nutritional status. In addition, recent research has identified the link between diabetes and cancer. Join us to learn more about this unexpected link and treatment strategies for steroid induced hyperglycemia using a case study approach.
Objectives:
- Discuss the relationship between cancer, hyperglycemia and insulin resistance.
- State 3 benefits of normalizing glucose levels during chemotherapy.
- Using a case study approach, discuss strategies to improve glucose levels and quality of life.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in enhancing their knowledge of diabetes management for people with cancer.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | To Prevent Hypo’s, JR Stopped Taking Bolus Insulin

For last week’s practice question, we quizzed test takers on JR’s fear of hypoglycemia. 85% of respondents chose the best answer. GREAT JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR is 26 years old with type 1 diabetes for over a decade. JR keeps missing appointments and when you finally get a hold of them on the phone, they start crying and say “I am afraid my blood sugars will go too low, so I stopped using my bolus insulin”. They explain that they were too embarrassed to come in and have their data downloaded.
Based on this information, what would be the most helpful approach?
Answer Choices:
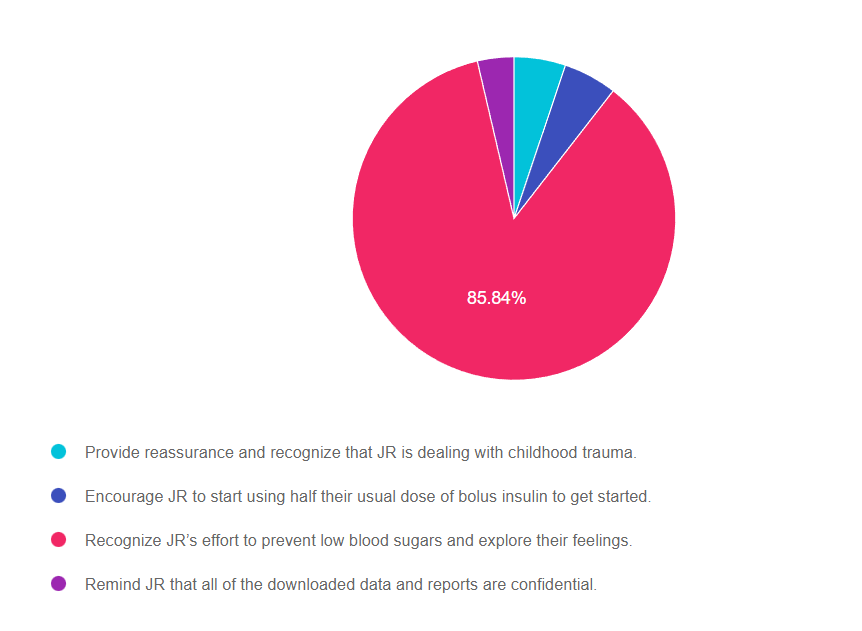
- Provide reassurance and recognize that JR is dealing with childhood trauma.
- Encourage JR to start using half their usual dose of bolus insulin to get started.
- Recognize JR’s effort to prevent low blood sugars and explore their feelings.
- Remind JR that all of the downloaded data and reports are confidential.
Getting to the Best Answer
Answer 1 is incorrect. 5.15% chose this answer, “Provide reassurance and recognize that JR is dealing with childhood trauma.” While there is a real possibility that JR experienced childhood trauma, there is no information to support that assumption in the question. However, providing JR with reassurance and helping with problem solving would be very helpful.
Answer 2 is incorrect. 5.36% of you chose this answer, “Encourage JR to start using half their usual dose of bolus insulin to get started.” Although taking half of the usual dose of bolus insulin is certainly better than taking no insulin, it is not a person centered approach. We need to engage JR in determining the best approach.
Answer 3 is correct. 85.84.% of respondents chose this answer, “Recognize JR’s effort to prevent low blood sugars and explore their feelings.” YES, great job, this is the best answer. We want to use a strength based approach and acknowledge that JR is making a big effort to prevent hypoglycemia and stay safe. We also want to recognize JR’s big emotions around hypoglycemia and explore them more closely. Finally, we will encourage JR to identify next steps.
Finally, Answer 4 is incorrect. 3.65% chose this answer, “Remind JR that all of the downloaded data and reports are confidential.” Not the best answer, but it is true that many people may have access to JR’s reports, which can add even more pressure to make sure everything looks good. When we look at JR’s report, we want to make sure we acknowledge the periods where things are going well before we dive into the troubled spots.
Thank you so much for reading this “Rationale of the Week”.
Want to learn more about this question? Join our NEW
ReVive 5 Diabetes Training Program
Save $100! Live Virtual Sessions Air July 19 & July 26th

Whether you are a novice or an expert in providing diabetes care, we invite you to attend this exciting training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management that will revolutionize your practice.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Join A Team of Experts – Save $100
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:

- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 14.0 CEs – Includes the 7-hour Session ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- Free Quarterly ReVive 5 Connect – connect with the instructors to help with problem solving for an hour four times a year.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Dates and Times for ReVive Virtual Training
- For your convenience, we have combined the 4 sessions into 2 half days. Same great content.
- July 19 and 26th from 9am to 12:30 pm PST. Space is limited, so save your space today!
Speakers Interviews – Learn more about the ReVive 5 Team
What is the Biggest Takeaway when Addressing Diabetes Distress? – Dr. Susan Guzman
Do you have to be a Mental Health Expert to Tackle Diabetes Distress? – Dr. Lawrence Fisher
Why I Transformed my Approach to Diabetes Self-Management Education- Coach Beverly
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.