Rationale of the Week | Best action before starting tirzepatide (Mounjaro)?

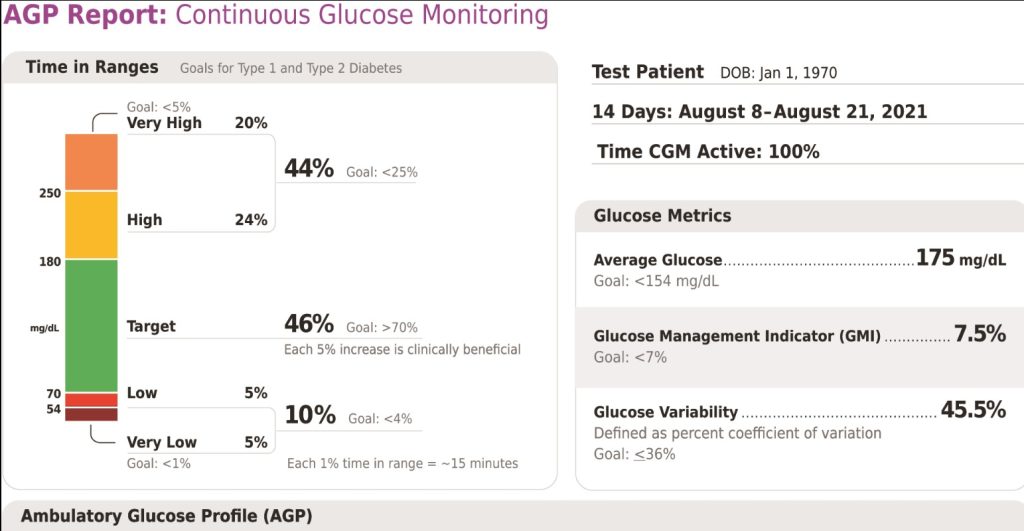
For last week’s practice question, we quizzed test takers on the best action before starting Tirzepatide (Mounjaro). 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
AR is 36 years old with type 2 diabetes and a BMI of over 40. Current A1C 7.9%, UACR less than 30, and GFR more than 60. Current diabetes medications include metformin, sitagliptin, and empagliflozin at maximum doses. AR is prescribed the new dual incretin tirzepatide (Mounjaro) to help improve glucose levels and support weight loss.
Before starting tirzepatide (Mounjaro), what action do you recommend to the provider?
Answer Choices:
- Repeat the UACR and GFR to verify kidney function.
- Stop the sitagliptin.
- Decrease metformin dose to prevent hypoglycemia.
- Evaluate thyroid function.
Getting to the Best Answer
Answer 1 is incorrect. 11.31% chose this answer, “Repeat the UACR and GFR to verify kidney function.” This is not the best answer because JR has great kidney function, evidenced by a normal UACR and GFR. So we do not need to recheck kidney function before starting this new dual incretin tirzepatide (Mounjaro).
Answer 2 is correct. 67.43% of you chose this answer, “Stop the sitagliptin.” YES, this is the best answer. The American Diabetes Association (ADA) and American Association of Clinical Endocrinologists recommend against combination therapy with a DPP4-inhibitor and a GLP-1 RA due to the lack of evidence that this strategy is beneficial. Initial research combining the two classes, reflect a negligible glucose lowering effect when GLP-1’s and DPP-4’s are combined. Given the approximate average wholesale price for the DPP-4 inhibitor of $434 and GLP-1 RA of $887, using both simultaneously is not cost effective or clinically beneficial.
Answer 3 is incorrect. 4.4.% of respondents chose this answer, “Decrease metformin dose to prevent hypoglycemia.” No need to decrease the metformin dose, since JR is not on any medication class that will cause hypoglycemia.
Finally, Answer 4 is incorrect. 16.82% chose this answer, “Evaluate thyroid function.” This class of medication is not recommended for any person with a history of medullary thyroid tumor. However, we don’t need to draw a TSH to see if this medication is safe, we would simply do a careful history to see if there is a family history of medullary thyroid tumor.
Thank you so much for reading this “Rationale of the Week”. You can download our Medication PocketCard below, for more information.
New Injectable – “TwinCretin” on Printed PocketCards
We have just added this novel, first in class, dual incretin hormone therapy, Tirzepatide (Mounjaro), to our printed version of our Diabetes Medication PocketCard.
This new twin therapy includes not only a GLP-1 Receptor Agonist, but also a Glucose-dependent insulinotropic polypeptide (GIP), which magnifies the therapeutic effectiveness. The SURPASS studies indicate that study participants experienced an A1C drop of up to 2.5% and weight loss of up to 10kg or more.
Want to learn more about Diabetes Medications?
Rationale of the Week | Ambulatory Glucose Profile Confusion

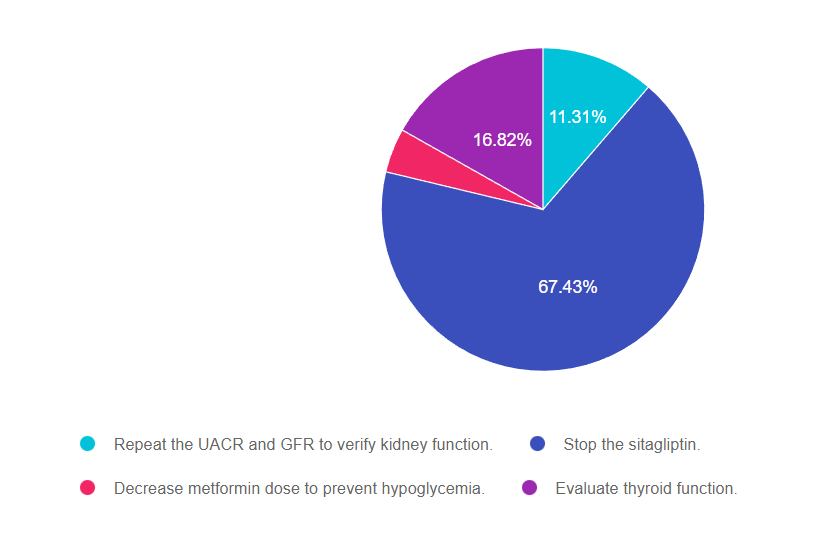
For last week’s practice question, we quizzed test takers on ambulatory glucose profile confusion. Only 62% of respondents chose the best answer, which indicates that there was some uncertainty. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
LS is 72 years old with type 2 diabetes and injects insulin 4 times a day. They were started on a CGM device last month and you are looking at the Ambulatory Glucose Profile (AGP) together. You notice their time in range is 60%, their time above range is 38%, in low range is 2% and their coefficient of variation is less than 36%.
What is the best response?
Answer Choices:
- We still need to improve your coefficient of variation.
- Based on these results, let’s decrease your insulin by 20%.
- Time in range should be 70% or greater for your age group.
- This information is going to help with problem solving.
Getting to the Best Answer
Answer 1 is incorrect. 11.89% chose this answer, “We still need to improve your coefficient of variation.” This is a juicy answer, but not the best one. If you refer to the Ambulatory Glucose Profile (AGP) below, you will see that the goal for Coefficient of Variation is less than 36%. In this question, LS has coefficient of variation is less than 36%, so they are meeting the target. This measure of glucose variability is important since it informs us of the intensity and duration of glucose levels fluctuations.
Answer 2 is incorrect. 5.26% of you chose this answer, “Based on these results, let’s decrease your insulin by 20%.” This is not the best answer either. Since their time in range of 60% is a little below target and 38% of the time they are above target, LS might actually need some more insulin. Of course, safety is always first, but their low blood sugar range is only 2%, well below the 5% target.
Answer 3 is incorrect. 20.91% of respondents chose this answer, “Time in range should be 70% or greater for your age group.” Another juicy answer, but just like A1C goals, time in range targets are based on the individual and other factors. For a 72 year old on multiple daily injections, 70% time in range may be too aggressive and put them at risk for hypoglycemia. The target time in range is not a “one size fits all” and needs to be customized to the individual. In addition, this statement uses the “should” word, which can evoke feelings of embarrassment or shame. Instead we might say, “Great job tracking your blood sugars. How are you feeling about your progress?
Finally, Answer 4 is correct. 61.94% chose this answer, “This information is going to help with problem solving.” YES, GREAT JOB, this is the best answer. It is person centered, acknowledges their effort and engages LS in participating in problem solving. This comment will definitely increase their feelings of mastery and empowerment.
Want to learn more about this topic?
Dr. Diana Isaacs is providing a fantastic technology update.
Coach Beverly will highlight diabetes language that is empowering.
Virtual DiabetesEd Training Conference | 30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Training Conference and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
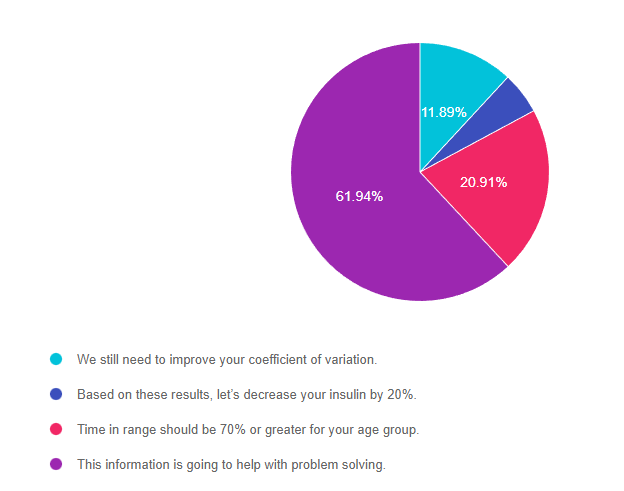
Rationale of the Week | Abdominal lumps and insulin injections

For last week’s practice question, we quizzed test takers on abdominal lumps and insulin injections. Only 46% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
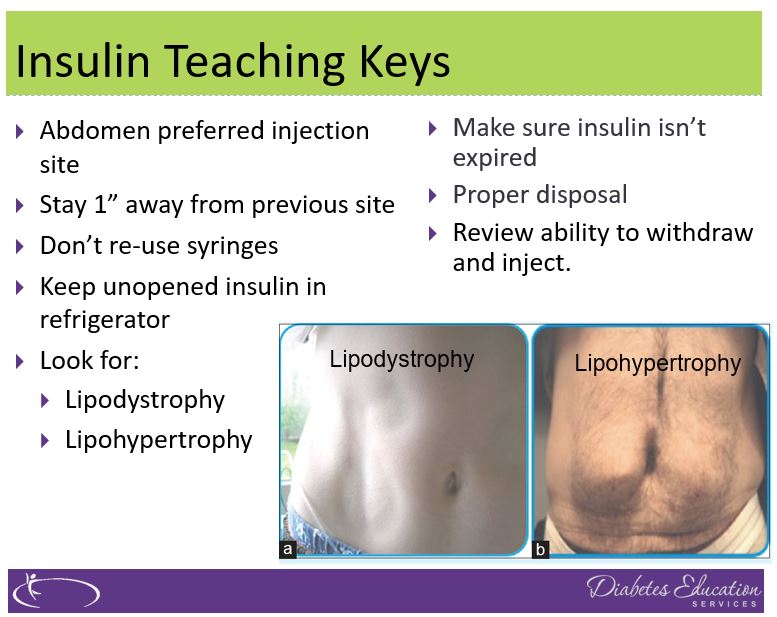
JL is 67 years old, with a BMI of 23 and A1C of 7.6% and injects insulin 4 times a day to manage their type 1 diabetes. On visual inspection, you notice that there are many areas of lipohypertrophy on JL’s abdominal region.
Which of the following interventions would be the best recommendation?
Answer Choices:
- Switch to 50/50 insulin twice daily.
- Stop bolus insulin and switch to a GLP-1 RA.
- Switch bolus injections to inhaled insulin.
- Use a higher gauge needles to enhance absorption.
Getting to the Best Answer
Answer 1 is incorrect. 18.54% chose this answer, “Switch to 50/50 insulin twice daily.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to 50/50 insulin may even lead to worsening blood sugars since it is a premixed basal bolus insulin that would be difficult to fine tune for people with type 1 diabetes. (See photo of lipohypertrophy below)
Answer 2 is incorrect. 7.85% of you chose this answer, “Stop bolus insulin and switch to a GLP-1 RA.” This is not the best answer since GLP-1 RA’s are not FDA approved to treat people with type 1 diabetes*. If a person with type 1 diabetes stopped their bolus insulin, they would become very insulin deprived and likely experience severe blood glucose elevations and hyperglycemic crisis. Plus, this answer doesn’t address the core issue of injection site overuse and fat accumulation. *Footnote: some people with type 1 are prescribed a GLP-1 RA (off label) in ADDITION to basal bolus insulin to lower glucose levels and help with weight management. (See photo of lipohypertrophy below)
Answer 3 is correct. 45.93% of respondents chose this answer, “Switch bolus injections to inhaled insulin.” YES, GREAT JOB. Lipohypertrophy, a lump of fat accumulation due to frequent injections, has been shown to affect ?50% of people injecting insulin and results from lack of injection site rotation and needle. Injecting into these “lumps” reduces insulin absorption and action, raises postprandial glucose, and greatly increases insulin uptake variability. Despite this, inspection of injection sites is not routinely performed by health care professionals or people with diabetes, which reveals the “unexplained” nature of many blood glucose fluctuations. (Excerpted from this Article on Insulin Injection Technique- Clinical Diabetes, 2019).
To avoid lipohypertrophy, we can transition people to boluses of inhaled insulin to cover for food and hyperglycemia and still provide one basal injection a day, using sites free of fatty lumps. This reduction of the injection frequency allows time for tissue healing and reduces creation of new lipohypertrophy sites. Download our FREE Insulin PocketCards here.
If a person decides to stay on injections, encourage them to systematically space them at least 1 cm (about the width of an adult finger) from each other; this helps to avoid repeat tissue trauma. One approach involves dividing sites into quadrants (or halves when using the buttocks or thighs), using one quadrant per week and moving from quadrant to quadrant in a consistent direction (e.g., clockwise). Encourage people to rotate injections between sites, as well as within a site. Use needles once and toss, since excessive reuse of needles can traumatize the skin and underlying structures. (See photo of lipohypertrophy below)
Finally, Answer 4 is incorrect. 27.67% chose this answer, “Use a higher gauge needles to enhance absorption.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to a higher gauge needle just means the barrel of the needle is thinner and hurts less when passing through the skin. Improper injection site rotation and needle reuse are the most common factors associated with lipohypertrophy. (See photo of lipohypertrophy below)
Read more great info here, The Injection Technique Factor: What You Don’t Know or Teach Can Make a Difference – Article from Clinical Diabetes, 2019. You are also invited to join our Virtual Conference where we tackle this topic and many more factors that affect diabetes self-care.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
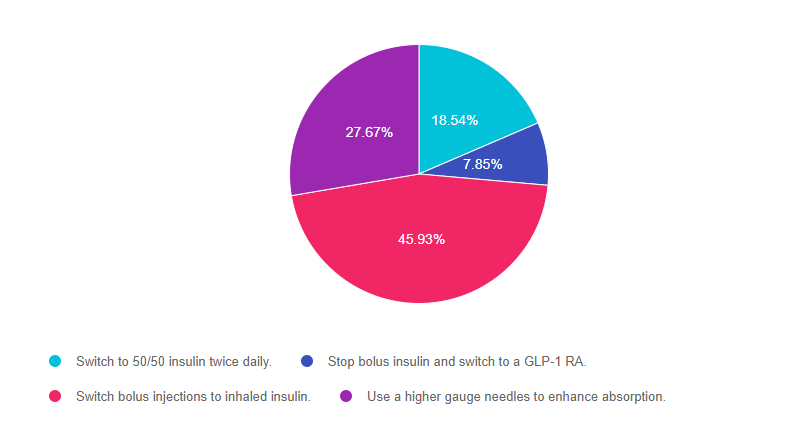
Rationale of the Week | Right amount of insulin for 83 year old?

For last week’s practice question, we quizzed test takers on the right amount of insulin for an 83 year old. Only 50% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
MS is an 83-year-old admitted to the hospital for a broken hip. MS has a BMI of 22.4, A1C of 6.9% on metformin 500mg twice daily. UACR is less than 30 and GFR is 48. The MD writes to stop oral meds in prep for surgery and start on basal-bolus insulin therapy.
Based on MS’s profile, what would be the most accurate formula to calculate their total daily insulin dose?
Answer Choices:
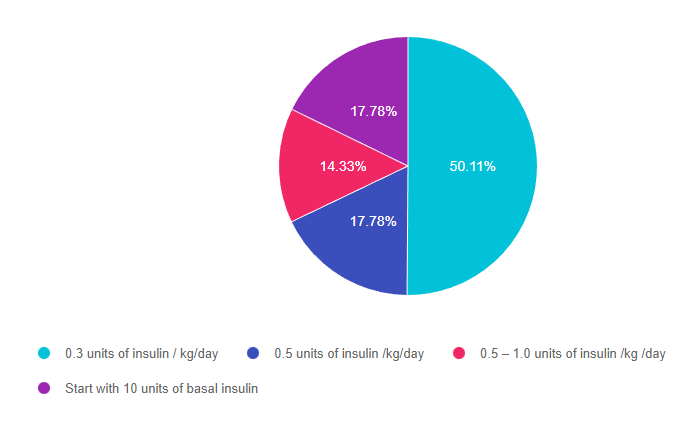
- 0.3 units of insulin / kg/day
- 0.5 units of insulin /kg/day
- 0.5 – 1.0 units of insulin /kg /day
- Start with 10 units of basal insulin
Getting to the Best Answer
Answer 1 is correct. 50.11% chose this answer, 0.3 units of insulin / kg/day.” YES, GREAT JOB. This is the best answer for several reasons. We can tell from the case study that MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting on a VERY conservative total daily insulin dose is the best and safest approach.
Answer 2 is incorrect. 17.78% of you chose this answer, “0.5 units of insulin /kg/day.” This is a juicy answer However MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting MS on 0.5 units/kg total daily insulin might be too much and might put MS at risk of hypoglycemia due to over insulinization.
Answer 3 is incorrect. 14.33% of respondents chose this answer, “0.5 – 1.0 units of insulin /kg /day.” This is another juicy answer However MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting MS on 0.5 – 1.0 units/kg total daily insulin might be too much and might put MS at risk of hypoglycemia due to over insulinization.
Finally, Answer 4 is incorrect. 17.78 chose this answer, “Start with 10 units of basal insulin.” This answer is appealing, since we often start people on 10 units of basal insulin. However, in this case study, we don’t have MS’s body weight to calculate their total daily insulin needs. Since we don’t have their weight in kgs, we don’t know what the right starting basal dose. For this reason, this is not the best answer.
Want to learn more about this question? Join us for our
Level 4 | Basal Bolus Therapy in Hospitals | 1.5 CEs
Recently updated and ready to watch!

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely and effectively implement Basal Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the patient’s clinical presentation and apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings and a discussion of solutions that will keep patients safe and get glucose levels to goal. In addition, sample basal/bolus and insulin drip guidelines plus lots of resource articles are included.
Objectives:
- Discussing appropriate insulin dosing based on the patient’s clinical presentation
- Applying dosing strategies to a variety of case studies
- Introduce hard-to-manage situations that commonly occur in hospital settings
- A discussion of solutions that will keep patients safe and get glucose levels to goal
- Sample basal/bolus and insulin drip guidelines plus lots of resource articles are included
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Should I toss food if it’s past the date?

For last week’s practice question, we quizzed test takers on if you should toss food if it is past the expiration date. Only 35% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
A person comes into the clinic for a diabetes education appointment. They are on a budget and ask you if they should throw away food if it is older than the date on the package.
What is the most accurate response?
Answer Choices:
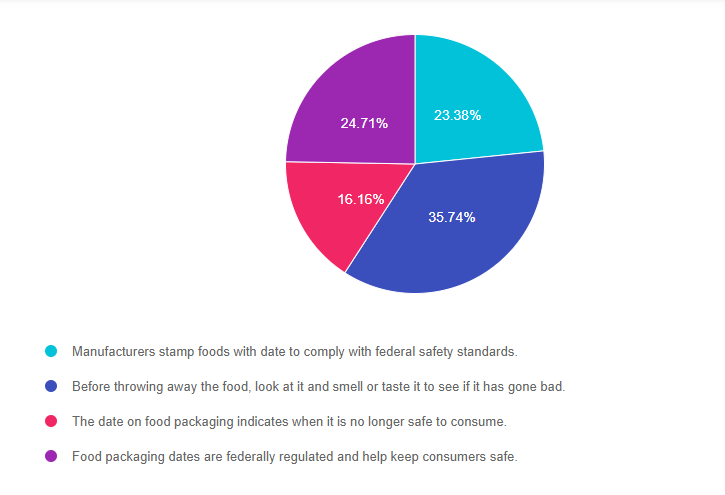
- Manufacturers stamp foods with a date to comply with federal safety standards.
- Before throwing away the food, look at it and smell or taste it to see if it has gone bad.
- The date on food packaging indicates when it is no longer safe to consume.
- Food packaging dates are federally regulated and help keep consumers safe..
Getting to the Best Answer
Answer 1 is incorrect. 23.38% chose this answer, “Manufacturer’s stamp foods with a date to comply with federal safety standards.” This is a juicy answer, but it is not the best answer. Except for infant formula, dates are not an indicator of the product’s safety and are not required by Federal law. Since the federal government doesn’t require the dates, the “sell by” or “enjoy by” dates are determined mostly by the manufacturers. Manufacturers put the date on the package to encourage consumers to eat the food product when it tastes best, not when the food will go “bad”. They want to protect their brand and encourage the consumer to purchase their product again.
Answer 2 is correct. 35.74% of you chose this answer, “Before throwing away the food, look at it and smell or taste it to see if it has gone bad.” Research shows that one in three bags of groceries purchased will end up in the trash due to dates stamped on food items. According to the United States Department of Agriculture (USDA), foods are still safe for consumption after these expiration dates pass, but make sure to look out for an off odor, flavor, or texture that mean the food has spoiled and should not be eaten.
The FDA says the dates on food aren’t serving a safety role. A food and law expert, Broad Leib says, “however, you do want to pay attention to dates on food in the prepared food section, including deli meat, raw fish, unpasteurized milk and cheese.” But for most foods, like a box of mushrooms or a bottle of ketchup, Broad Leib suggests we take a pause to look at the food. Smell and taste it to determine if it seems okay to eat. We can tell if something went bad.
Answer 3 is incorrect. 16.16% of respondents chose this answer, “The date on food packaging indicates when it is no longer safe to consume. ” This is a juicy answer, but it is not the best answer. Except for infant formula, dates are not an indicator of the product’s safety and are not required by Federal law. Since the federal government doesn’t require the dates, the “sell by” or “enjoy by” dates are determined mostly by the manufacturers. Manufacturers put the date on the package to encourage consumers to eat the food product when it tastes best, not when the food will go “bad”. They want to protect their brand and encourage the consumer to purchase their product again.
Finally, Answer 4 is incorrect. 24.71% chose this answer, “Food packaging dates are federally regulated and help keep consumers safe.” This is a juicy answer, but it is not the best answer. Except for infant formula, dates are not an indicator of the product’s safety and are not required by Federal law. Since the federal government doesn’t require the dates, the “sell by” or “enjoy by” dates are determined mostly by the manufacturers. Manufacturers put the date on the package to encourage consumers to eat the food product when it tastes best, not when the food will go “bad”. They want to protect their brand and encourage the consumer to purchase their product again.
Read more in our blog
Food Dates Can Lead to Unnecessary Waste

Have you inspected a food product that you bought last week and wondered if you should toss it because it expired yesterday? If you said yes, you are not alone.
About 40% of food waste happens in the kitchen, when consumers throw away foods that have passed the expiration date.
Are we throwing away perfectly good food based on the date stamped on the package?
Dates are confusing and they are often not associated with safety concerns. Learn why food and legal experts are asking consumers to reconsider their thinking.
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Training Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Training Conference and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best Action for Glucagon Rescue after too many beers?

For last week’s practice question, we quizzed test takers on the best action for glucagon rescue medicine with beer. 70% of respondents chose the best answer. Great JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
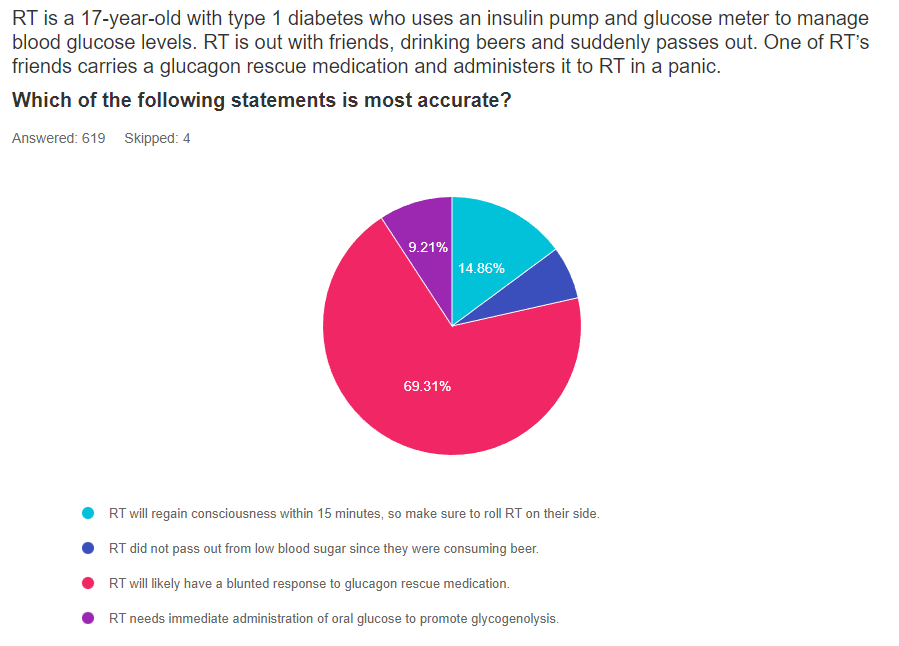
RT is a 17-year-old with type 1 diabetes who uses an insulin pump and glucose meter to manage blood glucose levels. RT is out with friends, drinking beers and suddenly passes out. One of RT’s friends carries a glucagon rescue medication and administers it to RT in a panic.
Which of the following statements is most accurate?
Answer Choices:
- RT will regain consciousness within 15 minutes, so make sure to roll RT on their side.
- RT did not pass out from low blood sugar since they were consuming beer.
- RT will likely have a blunted response to the glucagon rescue medication.
- RT needs immediate administration of oral glucose to promote glycogenolysis.
Getting to the Best Answer
Answer 1 is incorrect. 15% chose this answer, “RT will regain consciousness within 15 minutes, so make sure to roll RT on their side.” Since alcohol consumption slows glycogen breakdown in the liver, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications. While we hope the RT regains consciousness quickly, there is a real possibility that it will take longer than 15 minutes. However, the second half of the answer offers sound advice. Since people often get nauseated and may vomit after receiving glucagon, it is a good idea to roll RT on their side. See our Blog for more info – Warning Alcohol can Blunt Impact of Glucagon
Answer 2 is incorrect. 5% of you chose this answer, “RT did not pass out from low blood sugar since they were consuming beer.” Although beer may contain some carbohydrate, the body considers alcohol a toxin and as soon as it reaches the bloodstream, the liver prioritizes metabolizing the alcohol and breaking it down. During this clean-up process, the liver is distracted from hormone signals that direct the liver to break down glycogen for energy and liberate glucose into the bloodstream. This clean-up can last for up to 8 hours, making delayed hypoglycemia a real possibility. See our Blog for more info – Warning Alcohol can Blunt Impact of Glucagon
Answer 3 is correct. 70% of respondents chose this answer, “RT will likely have a blunted response to the glucagon rescue medication.” YES, this is the best answer. Alcohol consumption slows glycogen breakdown in the liver, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications. When a person with type 1 diabetes drink alcohol, they at increased risk of hypoglycemia because the liver is less capable of breaking down stored glycogen.
Having a conversation with people with type 1 about the suppressive nature of alcohol on glycogen release for many hours after consuming alcohol is very important.
As a general rule of thumb, encouraging people with type 1 to eat 15gms of carbs with each drink and have a glass of water in between, may help make sure they have enough circulating carbs and slow the pace of alcohol consumption to help the liver with processing. They may also consider decreasing their insulin dose in association with alcohol intake to prevent this serious side effect. See our Blog for more info- Warning Alcohol can Blunt Impact of Glucagon
Finally, Answer 4 is correct. 9% chose this answer, “RT needs immediate administration of oral glucose to promote glycogenolysis.” This is a juicy answer. AFTER RT regains consciousness, they will certainly need to consume an oral form of energy to replete their glycogen stores and stabilize glucose levels. Of course, it isn’t safe to administer oral glucose when a person loses consciousness. Instead, emergency responders would administer glucagon or dextrose through an IV. See our Blog for more info- Warning Alcohol can Blunt Impact of Glucagon
Read more in our blog
Does Alcohol Intake Blunt Impact of Glucagon?
LS tells you that they frequently attend company mixers where they feel compelled to have at “least a few drinks”, to fit in and network.
The tricky part is that LS lives with type 1 diabetes. Since they don’t have a working pancreas, their circulating levels of insulin and glucagon are often mismatched to their body’s needs.
If LS has several drinks, then loses consciousness from hypoglycemia, will emergency treatment be effective?
There is emerging evidence that glucagon rescue medications may have a blunted response when ingesting alcohol.
Want to learn more about this question?
Enroll in our upcoming webinar series updates
Level 4 | Advanced Level & Specialty Topic Courses | 13+ CEs
Join us live beginning August 9th through November 9th at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about Specialty Topics for their clinical practice or for those who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) certification exam.
2022 Live Webinar Updates
Previously recorded & available for on-demand viewing
- The Impact of Adverse Childhood Experiences on Health | 1.0 CE
- 3 Steps to Save Feet; Assess, Screen, and Report | 1.0 CEs
- Solving Glucose Mysteries for Type 1 | 1.5 CEs
- Solving Glucose Mysteries for Type 2 | 1.5 CEs
All courses air at 11:30 a.m. (PST)
- August 23, 2022 | Insulin Calculation Workshop – From Pumps & Beyond | 1.5 CEs
- August 25, 2022 | Basal Bolus Therapy in Hospital |1.5 CEs
- September 15, 2022 | Type 2 Diabetes Intensive | 2 CEs
- October 26, 2022 | Cancer & Diabetes | 1.25 CEs
- November 9, 2022 | Getting to the Gut (& Skin) | 1.0 CEs
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.

Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Premeal Glucose is Too Low

For last week’s practice question, we quizzed test takers on what to do when premeal glucose is too low. 49% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: RL carb counts and takes 1 unit of insulin for every 10 gms of carbohydrate. RL also uses a correction ratio and takes 1 unit for every 40 points above their glucose target of 120. RL’s asks you what to do if their premeal glucose is less than 70 before their lunch meal at work. RL often has blood sugar drops right before lunch and usually eats a sandwich, chips, berries and some sparkling water for lunch.
Given the situation, what is the best recommendation for JL to do if their pre-lunch glucose is less than 70 mg/g?
Answer Choices:
- Immediately eat 15gms of berries and recheck glucose in 15 minutes.
- Decrease usual insulin carb coverage for this meal by 1 or 2 units.
- Encourage RL to eat lunch immediately and give insulin afterward.
- Discuss which strategies would work best for RL in this situation.
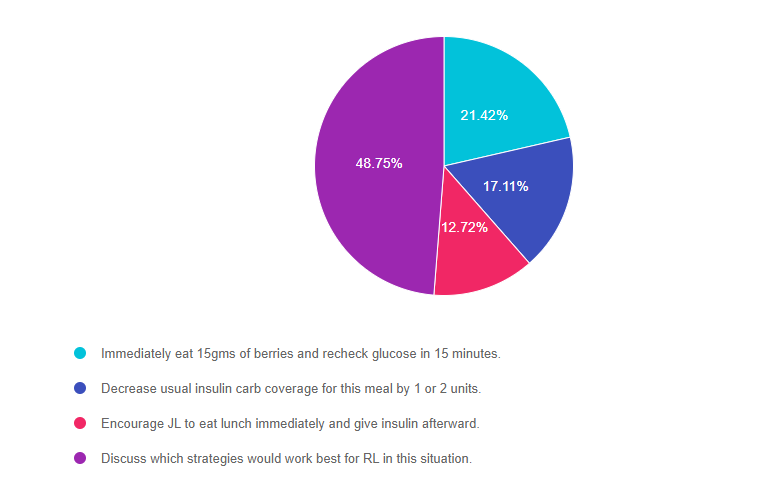
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 21.42% chose this answer, “Immediately eat 15gms of berries and recheck glucose in 15 minutes.” This answer is a right answer, but it is not the BEST answer. Yes, we recommend treating low blood sugar with 15 gms of carbohydrate, but is this the preferred treatment strategy for RL? Would RL choose this option?
Answer 2 is incorrect. 17.11% of you chose this answer, “Decrease usual insulin carb coverage for this meal by 1 or 2 units.” This also could be a right answer, but it is not the BEST answer. When faced with a premeal low blood sugar, some people may choose to decrease their bolus insulin dose by 1-2 units, but is this the preferred treatment strategy for RL?
Answer 3 is incorrect. 12.72% of respondents chose this answer, “Encourage RL to eat lunch immediately and give insulin afterward.” This also could be a right answer, but it is not the BEST answer. When faced with a premeal low blood sugar, some people may choose to eat first then give their insulin afterward, based on glucose levels, but is this the preferred treatment strategy for RL?
Finally, Answer 4 is correct. 48.75% chose this answer, “Discuss which strategies would work best for RL in this situation.” YES, this is the BEST answer. RL may choose any of the above mentioned strategies, or RL may have some other ideas on how to manage this situation. Our goal is to keep it person centered and recognize the expertise of the individual who lives with diabetes everyday.
Level 4 | Advanced Level & Specialty Topic Courses | 13+ CEs
Join us live beginning August 9th through November 9th at 11:30 am PST

This bundle is specifically designed for healthcare professionals who want to learn more about Specialty Topics for their clinical practice or for those who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) certification exam.
2022 Live Webinar Updates
Previously recorded & available for on-demand viewing
- The Impact of Adverse Childhood Experiences on Health | 1.0 CE
- 3 Steps to Save Feet; Assess, Screen, and Report | 1.0 CEs
- Solving Glucose Mysteries for Type 1 | 1.5 CEs
All courses air at 11:30 a.m. (PST)
- August 11, 2022 | Solving Glucose Mysteries for Type 2 | 1.5 CEs
- August 23, 2022 | Insulin Calculation Workshop – From Pumps & Beyond | 1.5 CEs
- August 25, 2022 | Basal Bolus Therapy in Hospital |1.5 CEs
- September 15, 2022 | Type 2 Diabetes Intensive | 2 CEs
- October 26, 2022 | Cancer & Diabetes | 1.25 CEs
- November 9, 2022 | Getting to the Gut (& Skin) | 1.0 CEs
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best treatment for abrasion?

For last week’s practice question, we quizzed test takers on the best treatment for abrasions 65% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 38 years old and takes insulin twice a day. They mention they went to the bathroom at night, lost their balance, and scraped their shin. They put a band-aid on it, but want you to take a look.
What is the best approach to treat the abrasion?
Answer Choices:
- Clean carefully with sanitizing gel, apply topical antibiotic and observe for signs of infection.
- Discuss creating a safe path to the bathroom at night and assess the abrasion for severity.
- Replace the band-aid with gauze and suggest they make an appointment with podiatry.
- Take a photo of the abrasion, wash with soap and water, and apply iodine around the perimeter.
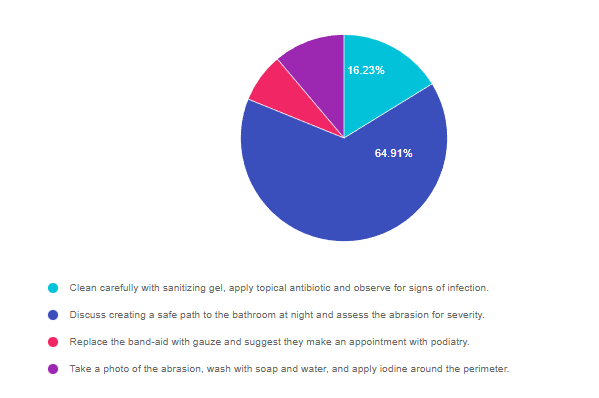
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 4, and finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 16.23% chose this answer, “Clean carefully with sanitizing gel, apply topical antibiotic and observe for signs of infection.” This is a juicy answer, but not the best answer for this situation for two main reasons. Applying topical antibiotic is a great idea, but generally, abrasions are cleansed with soap and water instead of sanitizing gel. In addition, this answer did not address the core issue, of improving safety when going to the bathroom at night.
Answer 2 is correct. 64.91% of you chose this answer, “Discuss creating a safe path to the bathroom at night and assess the abrasion for severity.” YES, GREAT JOB, this is the best answer. Many lower extremity falls, scrapes and injuries happen on the way to the bathroom when it is dark. It is important to make sure people have a safe path, including night lights and removal of any potential fall risks, especially for older people with balance issues.
Answer 3 is incorrect. 7.71% of respondents chose this answer, “Replace the band-aid with gauze and suggest they make an appointment with podiatry.” It is important to evaluate and treat the abrasion, but it does not warrant an automatic referral to the podiatrist, especially since it is on the shin. Also, this question does not provide enough details about the severity of the wound to determine if further treatment is required.
Finally, Answer 4 is incorrect. 11.16% chose this answer, “Take a photo of the abrasion, wash with soap and water, and apply iodine around the perimeter.” Of course it is a great idea to evaluate an abrasion, but iodine can cause skin irritation and not usually recommended as an antiseptic. In addition, this answer did not address the core issue, of improving safety when going to the bathroom at night.