Rationale of the Week | Which diabetes meds safe during pregnancy?

For last week’s practice question, we quizzed test takers on pregnancy and diabetes. 63% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR says they just found out they are pregnant. AR has type 2 diabetes and polycystic ovary syndrome and takes metformin 1000mg BID, semaglutide (Ozempic) 1.0mg weekly, and 30 units glargine insulin for diabetes management. Her most recent A1C was 8.2%. What is the most important action to take?
Answer Choices:
- Add bolus insulin to get A1C less than 6.5%.
- Increase the semaglutide (Ozempic) to 2.0mg weekly.
- Add a SGLT-2 Inhibitor to get glucose to target.
- Instruct AR to stop the semaglutide (Ozempic).
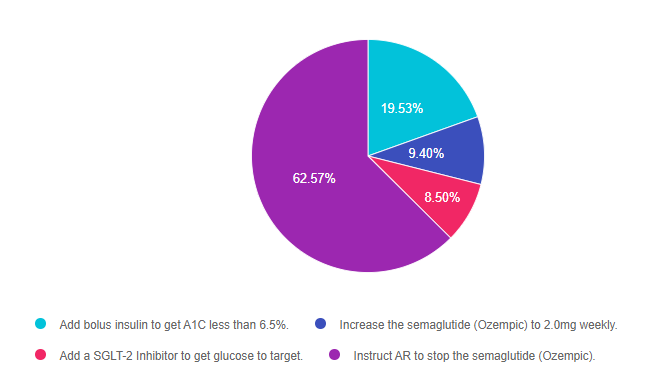
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally 3.
Getting to the Best Answer
Answer 1 is incorrect. 19.53% chose this answer, “Add bolus insulin to get A1C less than 6.5%.” This answer is accurate, but it is not the best answer. The A1C goal during pregnancy is less than 6.5% and in this case, AR will need to manage their diabetes using basal bolus insulin therapy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 2 is incorrect. 9.40% of you chose this answer, “Increase the semaglutide (Ozempic) to 2.0mg weekly.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 3 is incorrect. 8.50% of respondents chose this answer, “Add a SGLT-2 Inhibitor to get glucose to target.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, SGLT-2s are not approved for pregnancy and the GLP-1 RA, semaglutide would also need to be discontinued.
Finally, Answer 4 is correct. 62.57% chose this answer, “Instruct AR to stop the semaglutide (Ozempic).” YES, GREAT JOB! AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Basal bolus insulin therapy is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA. Metformin can be continued through the first trimester and the insulin would need to be intensified to get A1C to target.
Want to learn more about this question? Join us for our webinar
Pregnancy & Diabetes Standards | Level 2 | $29 for 1.5 CEs
Recorded & Ready to Watch!

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, and understanding. This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Objectives:
- Three issues that affect pregnancy with diabetes
- The unique attributes of pre-existing diabetes in pregnancy and gestational diabetes
- Diagnostic criteria and management goals for gestational diabetes
- Potential short term and long term complications of fetal exposure to hypoglycemia
- Prevention measures to keep parent and baby healthy
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Insulin safe for older adults?

For last week’s practice question, we quizzed test takers on if insulin is safe for older adults. 78% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: For older adults with diabetes using insulin therapy, which of the following is the most accurate statement?
Answer Choices:
- Due to cognitive decline, continuous glucose monitoring is not recommended for older adults.
- Older adults are at greater risk of hypoglycemia than younger adults.
- Divide basal insulin into two separate doses to enhance absorption.
- Give insulin after meals to prevent hypoglycemia.
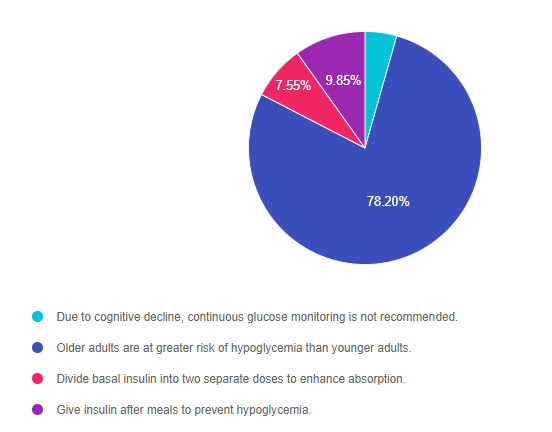
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally 1.
Getting to the Best Answer
Answer 1 is incorrect. 4.40% chose this answer, “Due to cognitive decline, continuous glucose monitoring is not recommended for older adults.” Many older adults on intensive insulin therapy with a history of hypoglycemia can benefit from CGM technology to prevent low blood sugars and fine tune carb intake and insulin dosing. Each older adult needs a individualized assessment to determine if a CGM is right for them. The rate of cognitive decline is complex and is a result of genetics, other chronic conditions and overall health combined with aging.
Answer 2 is correct. 78.20% of you chose this answer, “Older adults are at greater risk of hypoglycemia than younger adults. GREAT JOB, almost 80% of you chose this best answer. As people with diabetes age, they are at higher risk for low blood sugars for many reasons, especially if they are taking insulin or a secretagogue. Older individuals may have diminished renal function, which increases the duration of the action of insulin and secretagogues. Some can experience lower calorie intake due to decreasing appetite, trouble chewing, lack of resources, forgetfulness or depression and feelings of isolation. Others may have difficulty administering their insulin or medications accurately or may forget to eat after injections. For this reason, the ADA Standards recommends that older adults are assessed for hypoglycemia risk at each visit coupled with problem solving as needed.
Answer 3 is incorrect. 7.55% of respondents chose this answer, “Divide basal insulin into two separate doses to enhance absorption.” This is a juicy answer. For older adults at risk for hypoglycemia, the ADA does recommend scheduling the basal insulin for the morning instead of evening.
Finally, Answer 4 is incorrect. 9.85% chose this answer, “Give insulin after meals to prevent hypoglycemia.” Another juicy answer. This answer implies that all older people should take their insulin after meals. Some individuals might benefit from post-meal insulin, especially if they are not sure how much they are going to eat and they have a history of hypoglycemia. However, insulin works best when given before the meal so it peaks at the same time the post meal glucose is peaking.
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Diabetes and Earth Health interconnected?

For last week’s practice question, we quizzed test takers on how diabetes and earth health are interconnected. 78% of respondents chose the best answer, GREAT JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues. We can all take action to protect the earth and prepare for extreme climate events.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: According to a NIH systematic literature review, there is clear evidence that diabetes and climate change are interconnected. Which of the following situations are due to the impact of a changing climate?
Answer Choices:
- Lack of healthy food supply due to disrupted agricultural production.
- Shortages of medications, insulin and other diabetes supplies.
- Increased risk of cardiovascular events and death in people with diabetes due to extreme heat.
- All of the above
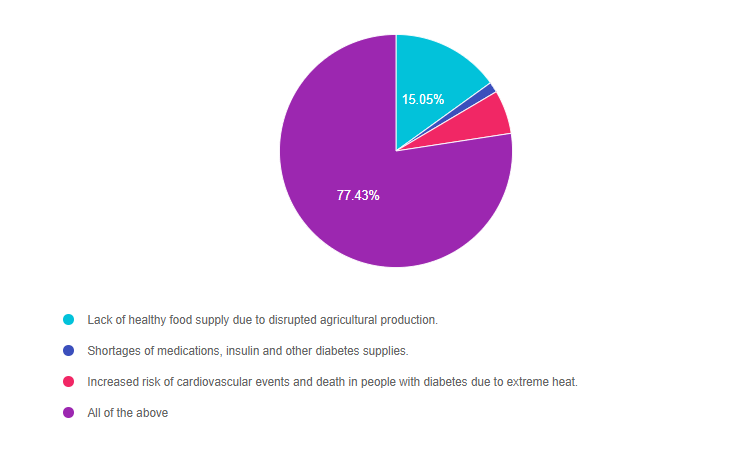
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 3, and finally 2.
Getting to the Best Answer
Answer one – 15.05% chose this answer, and it is accurate “Lack of healthy food supply due to disrupted agricultural production.” It is true that extreme weather can result in agricultural production disruptions. In our community, many fields that were once green with trees and crops, now are brown and barren. There is not enough water to keep crops alive and growing. When the healthy food supply is limited, people living with diabetes may turn to lower-cost, processed foods which are environmentally unfriendly and low in nutrients.
Answer two – 1.46% of you chose this answer and it is accurate, “Shortages of medications, insulin, and other diabetes supplies.” It is true that with recent climate disasters, like the Camp Fire, Hurricane Katrina in 2005, and Hurricane Harvey in 2017, resulted in people not being able to access, afford or safely store their medications, including insulin. In addition, we are experiencing supply chain disruptions in D50 (25 grams of glucose in a 50 ml prefilled syringe (50% glucose)) to treat hypoglycemia and certain intravenous fluids are in short supply. Other diabetes products and medications could be impacted in the future.
Answer three – 6.07% of respondents chose this answer and it is accurate, “Increased risk of cardiovascular events and death in people with diabetes due to extreme heat.” It is true that people with diabetes are at greater risk of experiencing dehydration and cardiovascular events during periods of extreme heat. With the increasing frequency of extreme heat episodes, there is an associated increased risk of heat-related death and cardiovascular events for people living with diabetes. Several studies reveal that people with diabetes have a higher risk of death on hot days, and are more likely to need emergency care and those with a history of heart disease are most vulnerable.
Finally, Answer four – 77.43% chose this answer, “All of the above.” YES. Great job, all of the answers are true, there is clear evidence that diabetes and climate changes are interconnected. As Diabetes Specialists, I believe we can make a difference by leaning into our unique blend of behavior change skills, advocacy, and scientific knowledge.
We can take a two-fold approach:
- Take action to help slow and reverse climate change – Read our blog on actions we can start taking today.
- Help people with diabetes to be prepared for natural disasters. Read our blog on How to Get Ready
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1 or Type 2 Diabetes?

For last week’s practice question, we quizzed test takers on which labs to order for JR. 57% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR’s mom has type 1 diabetes and JR’s dad has type 2 diabetes. JR is 21 years old and in the emergency room with a glucose of 482 mg/dl. Besides checking glucose, ketones and A1C levels, which of the following lab test can be used to determine if someone has autoimmune diabetes?
Answer Choices:
- Endogenous insulin titer
- Glutamic acid decarboxylase
- Beta cells autoantibodies
- Langerhan’s antibody titer
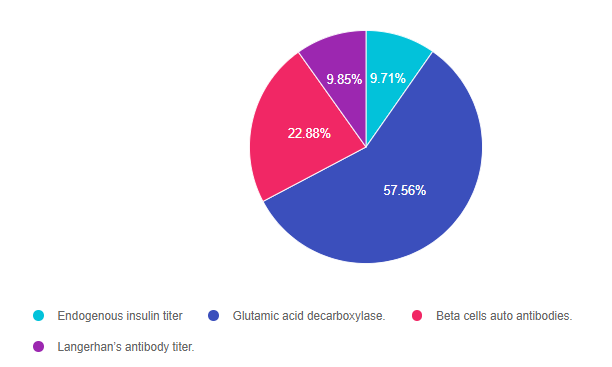
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally 1.
Getting to the Best Answer
Answer 1 is incorrect. 9.71% chose this answer, “Endogenous insulin titer.” This is a juicy answer. Evaluating endogenous insulin production is helpful since it reflects how much insulin the pancreas is secreting. However, it does not reveal if the beta cell loss is due to an immune-mediated response.
Answer 2 is correct. 57.56% of you chose this answer, “Glutamic acid decarboxylase (GAD)”, YES, this is the best answer. If the autoimmune blood test GAD comes back positive, it verifies that the pancreas is being destroyed through an immune-mediated attack of the beta cells. Autoantibodies against GAD are found in 80% of people with type 1 diabetes at clinical presentation.
Answer 3 is incorrect. 22.88% of respondents chose this answer, “Beta cells autoantibodies.” Another juicy answer that is very tempting. However, there is no blood test with this name. The three common antibodies tested are Islet Cell Autoantibodies (ICA), Insulin Autoantibodies (IAA), and Glutamic Acid Decarboxylase (GAD).
Finally, Answer 4 is incorrect. 9.85% chose this answer, “Langerhan’s antibody titer.” Another juicy answer that is very tempting. However, there is no blood test with this name. The three common antibodies tested are Islet Cell Autoantibodies (ICA), Insulin Autoantibodies (IAA), and Glutamic Acid Decarboxylase (GAD).
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Which Produce is listed in the”Dirty Dozen”?

For last week’s practice question, we quizzed test takers on which produce has the most pesticide residue. 82% of respondents chose the best answer, GREAT JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Each year, the Environmental Working Group (EWG) publishes the Shopper’s Guide to Pesticides in Produce™, which ranks the pesticide contamination of 46 popular fruits and vegetables based on test results by the Department of Agriculture and the Food and Drug Administration of around 45,000 samples of produce. Based on their 2022 analysis, which three fruits and vegetables listed are included in the “dirty dozen” (produce that is highest in pesticide residue)?
Answer Choices:
A. Strawberries, tomatoes, pears
B. Kale, asparagus, mangoes
C. Avocados, onions, sweet corn
D. Sweet potatoes, watermelon, cherries
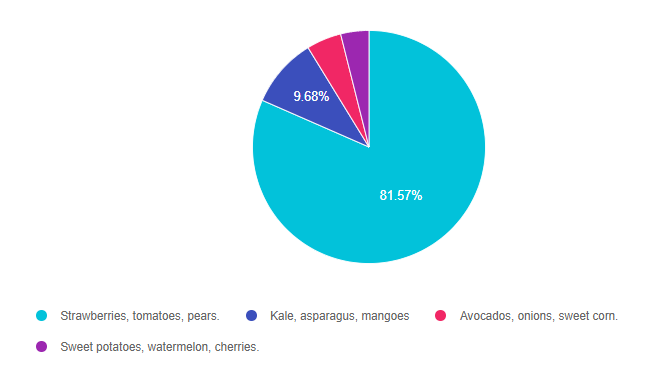
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 3, and finally 2.
Getting to the Best Answer
Answer 1 is correct. 81.57% chose this answer, “Strawberries, tomatoes, pears.” YES, this is the best answer. The complete list of fruits and vegetables with the highest pesticide levels include:
Dirty Dozen
These fruits and veggies are still healthy choices since they are packed with fiber and phytonutrients. However, given their higher amount of pesticide, try to purchase from the Organic Section of your local store or farmer’s market.

- Strawberries
- Spinach
- Kale, collard and mustard greens
- Nectarines
- Apples
- Grapes
- Bell and hot peppers
- Cherries
- Peaches
- Pears
- Celery
- Tomatoes
Answer 2 is incorrect. 9.68% of you chose this answer, “Kale, asparagus, mangoes.” Kale is included on the dirty dozen list, while asparagus and mangoes are part of the Clean 15.
Answer 3 is incorrect. 4.84% of respondents chose this answer, “Avocados, onions, sweet corn.” All of these vegetables and fruits have the lowest amount of pesticide and a part of the Clean 15.
Clean 15
These Clean 15 healthy fruits and veggies are safe to purchase in the non-organic or organic section. It’s always a good idea to wash fruit and veggies before eating.
- Avocados
- Sweet Corn
- Pineapple
- Onions
- Papaya
- Sweet peas (if frozen)
- Asparagus
- Honeydew melon
- Cabbage
- Kiwi
- Mangoes
- Mushrooms
- Watermelon
- Sweet potatoes
Finally, Answer 4 is incorrect. 3.92% chose this answer, “Sweet potatoes, watermelon, cherries.” Sweet potatoes and watermelon are part of the Clean 15 while cherries are included in the dirty dozen.
More info Here
Please visit the Environmental Working Groups Web page here
Dirty Dozen List
Clean 15 List
Info on how this list is created each year
We hope you appreciate this week’s rationale!
FREE PocketCard & Wildflower Seed PostCard for a Pledge

Free PocketCard and Wildflower Seed Postcard
We have created a list of 10 Actions to Celebrate Earth Day and printed these actions on wildflower seed postcards, that are ready for planting. To thank you for your pledge to commit to one or more actions that invest in the well-being of our planet, we will mail you a Free PocketCard and Wildflower Seed PostCard.
It’s easy! Just pick your action(s) on this survey and provide a mailing address where to send these gifts of appreciation. Each action, no matter how small, matters.
Want to learn more about this question? View our
Virtual DiabetesEd Specialist Conference
30+ CEs
Recorded & Ready to Watch!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $449: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | The “tooth” about diabetes & oral health

For last week’s practice question, we quizzed test takers on the link between oral health & hyperglycemia. 73% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Diabetes is associated with an increased risk of oral disease. Which of the following statements is true regarding people living with diabetes and hyperglycemia?
Answer Choices:
- Experience decreased salivary production.
- Benefit from vinegar gargles to decrease the bacterial load.
- At greater risk for oral cancers.
- More likely to experience tonsillitis.
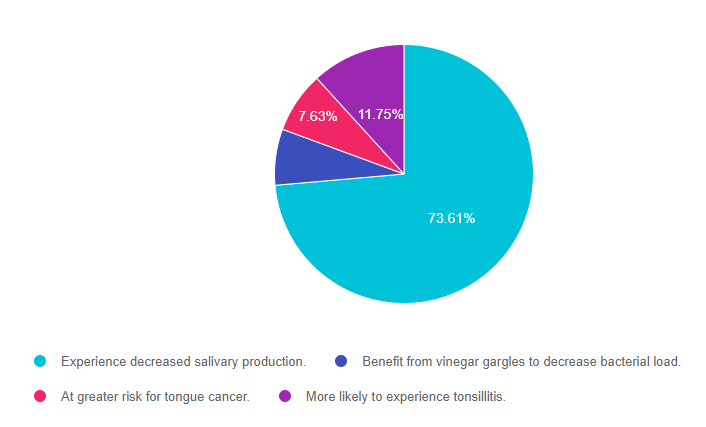
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 3, and finally 2.
Getting to the Best Answer
Answer 1 is correct. 73.61% chose this answer, “Experience decreased salivary production.” YES, GREAT JOB, this is the best answer. When a person is experiencing hyperglycemia, this leads to dehydration due to the chronic diuresis. When dehydrated, people with hyperglycemia produce less saliva and they saliva they do produce is laden with glucose. These 2 factors contribute to a higher risk of dental caries and can make mastication more difficult. There are products to increase salivary production, but the best treatment is to improve blood glucose levels.
Answer 2 is incorrect. 7.01% of you chose this answer, “Benefit from vinegar gargles to decrease the bacterial load.” Actually, gargling with vinegar can be harmful to your mouth if it is dry. Without the proper amount of saliva, the acid can break down enamel and decrease ability to fight off infection. There are products to increase salivary production, but the best treatment is to improve blood glucose levels.
Answer 3 is incorrect. 7.63% of respondents chose this answer, “At greater risk for oral cancers.” People with diabetes and chronic hyperglycemia have a higher risk for oral carries, gingivitis and periodontitis due to increased levels of sugar in the saliva that supports bacterial growth. However, do not have an increased risk of oral cancers.
Finally, Answer 4 is incorrect. 11.75% chose this answer, “More likely to experience tonsillitis.” People with diabetes and chronic hyperglycemia have a higher risk for oral carries, gingivitis and periodontitis due to increased levels of sugar in the saliva that supports bacterial growth. However, do not have an increased risk of tonsillitis.
More information from the American Dental Association.
We hope you appreciate this week’s rationale!
Want to learn more about this question? View our
Virtual DiabetesEd Specialist Conference
30+ CEs
Recorded & Ready to Watch!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Can you calculate LR’s Sensitivity Factor?

For last week’s practice question, we quizzed test takers on calculating LR’s sensitivity factor. 76% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: LR is a 30-year-old with type 1 diabetes. LS uses 25 units of basal insulin and 20 units of bolus insulin (about 6-7 units per meal) per day. Using the rule of 1700, what is LR’s insulin sensitivity factor?
Answer Choices:
- 23
- 85
- 50
- 38
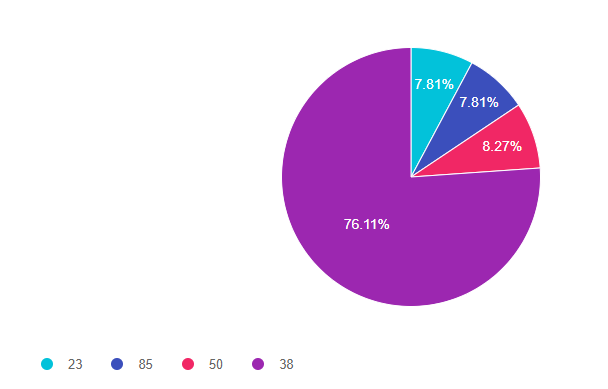
As shown above, the most common choice was option 4, the second most common answer was option 3, then a tie for options 1 and 2.
Getting to the Best Answer
Answer 1 is incorrect. 7.81% chose this answer, “23.” To figure out the sensitivity factor, we first have to determine the Total Daily Dose (TDD) that LR is taking. LR is taking 25 units of basal insulin and 20 units of bolus insulin, which equals a TDD of 45 units. If we are using 1700 as our insulin sensitivity factor (ISF), we divide the 1700 divided by 45 or 1700/45 or 37.7 which we round up to 38. In other words, 1 unit of insulin will drop LR’s blood sugar by 38 points.
Answer 2 is incorrect. 7.81% of you chose this answer, “85.” People who chose this answer, probably only included the bolus insulin dose in the calculation or 1700/20. To get to the accurate answer, add the basal plus bolus to get the total dose of 45, the divide as follows 1700/45 equals or 37.7 which we round up to 38. In other words, 1 unit of insulin will drop LR’s blood sugar by 38 points.
Answer 3 is incorrect. 8.27% of respondents chose this answer, “50.” To figure out the sensitivity factor, we first have to determine the Total Daily Dose (TDD) that LR is taking. LR is taking 25 units of basal insulin and 20 units of bolus insulin, which equals a TDD of 45 units. If we are using 1700 as our insulin sensitivity factor (ISF), we divide the 1700 divided by 45 or 1700/45 or 37.7 which we round up to 38. In other words, 1 unit of insulin will drop LR’s blood sugar by 38 points.
Finally, Answer 4 is correct. 76.11% chose this answer, “38.” YES, most of you chose the BEST answer. To figure out the sensitivity factor, we first have to determine the Total Daily Dose (TDD) that LR is taking. LR is taking 25 units of basal insulin and 20 units of bolus insulin, which equals a TDD of 45 units. If we are using 1700 as our insulin sensitivity factor (ISF), we divide the 1700 divided by 45 or 1700/45 or 37.7 which we round up to 38. In other words, 1 unit of insulin will drop LR’s blood sugar by 38 points.
Extra Credit info. What sensitivity factor should we use?
We use 1700 or 1800 insulin sensitivity factor (ISF) for people on insulin analogs and the 1500 ISF for people on regular insulin. But also, as you can see with the math below, a higher ISF number means less insulin. So, if we are working with a leaner more frail individual, we might choose to be more conservative and start with and ISF of 1800.
Example- A person’s Total Daily Dose (TDD) is 30 units a day. To figure out how much correction insulin they need to correct their hyperglycemia, we would consider the following options depending on their presentation.
1800/30 = 1 unit for every 60 points above target
1700/30 = 1 unit for every 56
1500 / 30 = 1 unit for every 50
We hope you appreciate this week’s rationale!
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Which Medications are needed?

For last week’s practice question, we quizzed test takers on which medications are needed. you all did great, since 81% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: LS is 43 with type 2 diabetes, with an A1C of 8.8%, UACR is 32 mg/g, GFR is 48, and blood pressure is 146/84 or greater on 2 different occasions. Current medications include metformin 1000mg BID, lovastatin 20mg, glipizide 20mg.
Based on the ADA standards of care, in addition to lifestyle encouragement, adding which medications would most improve outcomes?
Answer Choices:
- GLP-1 RA and low dose aspirin
- ACE and ARB for blood pressure management
- Basal insulin and a diuretic
- SGLT-2 and ACE or ARB
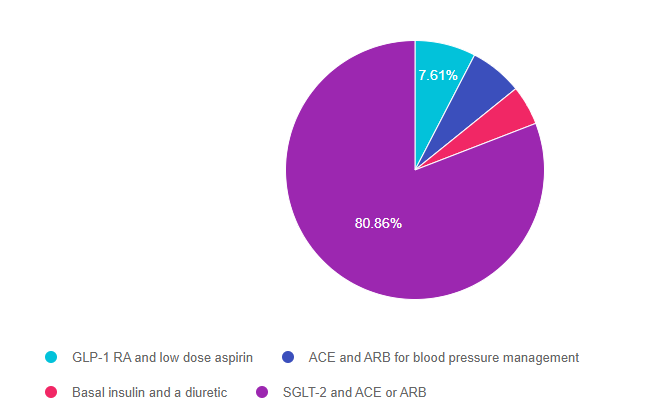
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and then finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 7.61% chose this answer, “GLP-1 RA and low dose aspirin.” Since LS is under the age of 50 and their CV risk status isn’t revealed in this case study, we don’t have enough information to start LS on aspirin. We could consider adding a GLP-1 RA, since it is known to lower glucose, decrease CV risk and offer some renal protection. However, since one part of the answer is wrong, the whole answer is wrong, even though adding a GLP-1 to LS’s plan would be helpful.
Answer 2 is incorrect. 6.58% of you chose this answer, “ACE and ARB for blood pressure management.” LS does have hypertension and elevated albumin levels and is not taking any medication for blood pressure. Given those two risk factors, LS needs to take EITHER an ACE Inhibitor or ARB for blood pressure management, but NOT both. We would recommend starting LS on an ACE or ARB first and adjusting the dose based on home blood pressure reading. If LS needs an additional blood pressure medication, we could add a diuretic, calcium channel blocker or beta-blocker, or another agent. See our Hypertension & Lipids, Cheat Sheet for more info.
Answer 3 is incorrect. 4.94% of respondents chose this answer, “Basal insulin and a diuretic.” With an A1c of 8.8%, LS isn’t quite ready for insulin since there are 2 other medications we could try first (SGLT-2 or GLP-1) to get glucose to goal. The ADS Standards recommend trying a GLP-1 before basal insulin if possible to avoid the risk of hypoglycemia and to decrease weight gain. In addition, because LS has hypertension and albuminuria, a diuretic would not be the medication of choice to lower blood pressure. The preferred medications for blood pressure in the presence of albuminuria include either an ACE or ARB.
Finally, Answer 4 is correct. 80.86% chose this answer, “SGLT-2 and ACE or ARB.” GREAT JOB! Most of you chose this BEST answer. In the presence of hyperglycemia, albuminuria, and diminishing renal function, adding a SGLT-2 Inhibitor is the best choice based on ADA Standards. SGLT-2s have been shown to not only lower glucose and protect kidneys, they can also lower blood pressure due to their “glucoretic” properties. To manage LS’s hypertension, the preferred medications for blood pressure in the presence of albuminuria include either an ACE or ARB.
We hope you appreciate this week’s rationale! For more information on this topic, check out the ADA Standards of Care. Or, join our 3 day DiabetesEd Specialist Virtual Conference next week. It’s not to late to register!
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








