Rationale of the Week | What is the cause of JR’s leg pain?

For last week’s practice question, we quizzed test takers on the cause of JR’s leg pain. 67% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is experiencing lower extremity pain and asks to get their gabapentin (Neurontin) renewed? When asked, JR says the pain is so bad in their calf muscles when walking, that they have to sit down and rest. What best describes the cause of JR’s pain?
Answer Choices:
- Loss of protective sensation (LOPS).
- Peripheral arterial disease (PAD).
- Autonomic neuropathy.
- Small nerve fiber neuropathy.
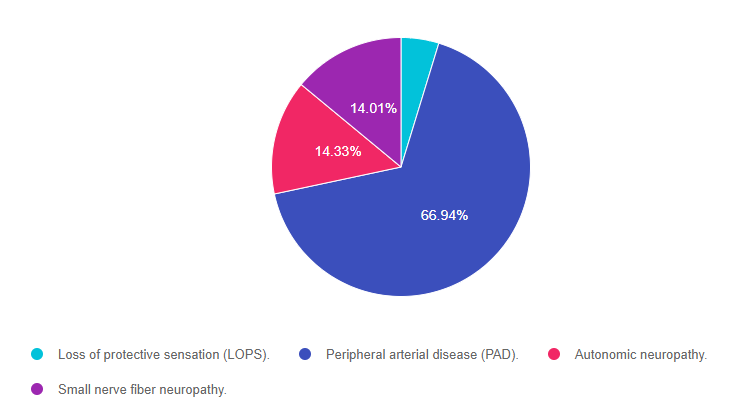
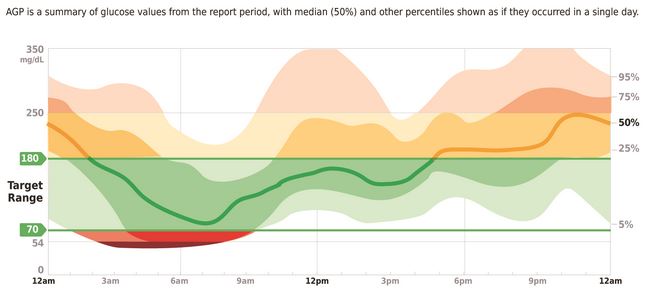
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and then finally option 1.
Getting to the Best Answer
Answer 1 is incorrect. 4.72% chose this answer, “Loss of protective sensation (LOPS).” This is a juicy answer because people with neuropathy and loss of protective sensation are often prescribed gabapentin to treat nerve pain. However, when we learn that JR’s calf pain only occurs when walking, we experience an “ah-ha” moment. The cause of JR’s pain is lack of arterial blood flow to the lower extremities, also known as peripheral arterial disease (PAD). The classic symptom of PAD is pain in calf muscles or buttocks when walking that is relieved by stopping. Neuropathy is most often described as burning pain in lower extremities that is often worse at night.
Answer 2 is correct. 66.94% of you chose this answer, “Peripheral arterial disease (PAD).” JR is experiencing lack of arterial blood flow to the lower extremities, also known as peripheral arterial disease (PAD). A classic symptom of PAD is pain in calf muscles or buttocks when walking that is relieved by stopping. Perhaps JR was prescribed gabapentin due to an incomplete medical assessment. With this new information, we can collaborate with the provider to see if referral to a vascular specialist is warranted to evaluate if further intervention is needed.
Answer 3 is incorrect. 14.33% of respondents chose this answer, “Autonomic neuropathy.” Autonomic neuropathy in people with diabetes does not cause lower extremity pain. Lower extremity pain is due to small and large nerve fiber destruction or peripheral arterial disease (PAD). People with autonomic neuropathy and diabetes are at higher risk of gastroparesis, sexual dysfunction, resting tachycardia and a myriad of other conditions.
Finally, Answer 4 is incorrect. 14.01% chose this answer, “Small nerve fiber neuropathy.” This answer is tempting because people with small nerve fiber neuropathy are often prescribed gabapentin to treat nerve pain. However, when we learn that JR’s calf pain only occurs when walking, we experience an “ah-ha” moment. The cause of JR’s pain is lack of arterial blood flow to the lower extremities, also known as peripheral arterial disease (PAD). The classic symptom of PAD is pain in calf muscles or buttocks when walking that is relieved by stopping. Small nerve fiber neuropathy is most often described as burning pain that is often worse at night.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this question?
Watch our Lower Extremity Assessment Standards | Level 2
$29 for 1.5 CEs
Recorded & Ready to Watch!
People with diabetes are at increased risk of Lower Extremity Complications. This course reviews the steps involved in performing a detailed assessment of the lower extremities, including how to use a monofilament and tuning fork to detect neuropathy. We also discuss the significance of Ankle Brachial Index and strategies to prevent lower extremity complications.
Objectives:
- Describe the risk factors for lower extremity complications
- Discuss prevention strategies
- Demonstrate steps involved in a lower extremity assessment
Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Schedule | Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What Changed with the New DSME Standard?

For last week’s practice question, we quizzed test takers on the most accurate statement based on the new ADA Standards of Care on DSME Programs. 60% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Which of the following best represents the 2022 update to the National Standards for Diabetes Self-Management Education and Support (DSMES)?
Answer Choices:
- Due to the complexity of delivering DSME in today’s health care environment, 2 new standards have been added for a total of 12 Standards.
- About 20 – 30% of people with Medicare or private insurance currently utilize DSMES services.
- To maintain quality, at least one of the DSMES team members needs to have either a CDCES or BC-ADM.
- Less focus on “checking the box” when delivering curriculum and more focus on the individual needs.
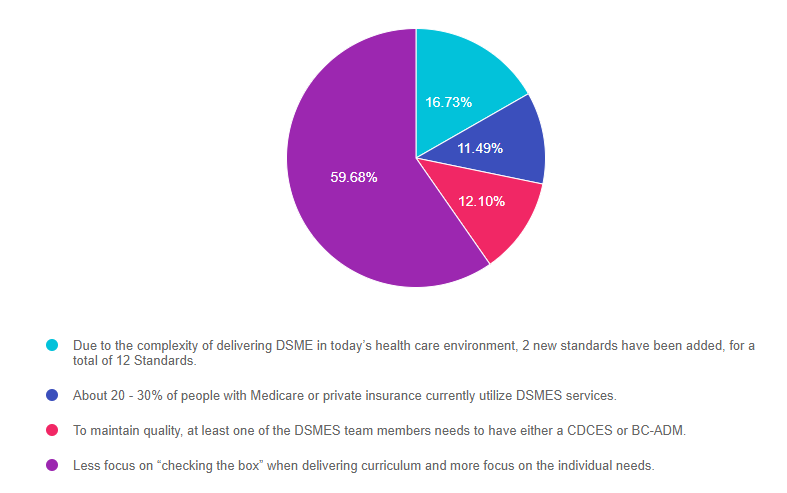
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 2, and then finally option 4.
Getting to the Best Answer
Answer 1 is incorrect. 16.73% chose this answer, “Due to the complexity of delivering DSME in today’s health care environment, 2 new standards have been added for a total of 12 Standards.” This was a juicy answer, but not the best one. The authors of this updated Standard of Practice for DSMES, decided that to INCREASE access to DSMES, there needed to be a DECREASE of bureaucracy and paperwork. They managed to maintain the essence of the original 10 Standards in this new streamlined version with only SIX standards. There was also a much needed intensive focus on recognizing and addressing Social Determinants of Health and breaking down barriers to DSMES access.
Answer 2 is incorrect. 11.49% of you chose this answer, “About 20 – 30% of people with Medicare or private insurance currently utilize DSMES services.” I wish this was the best answer. However, according to the ADA Standards, only 6-8% of Medicare recipients participate in DSMES. This lackluster level of participation is due to a multitude of factors and is best addressed by an interdisciplinary action committee, with stakeholders from the community and the health care team. Plus, creating a multi-pronged and thoughtful marketing plan is crucial to raise awareness of DSMES services.
Answer 3 is incorrect. 12.10% of respondents chose this answer, “To maintain quality, at least one of the DSMES team members needs to have either a CDCES or BC-ADM.” In the old days, this was a requirement. However, since many rural communities may not have access to a CDCES or BC-ADM, this requirement has been dropped for over 10 years. The good news is that a variety of health care professionals can make up the DSMES Team. Specifically, the new guidelines say that, “The DSMES team may include one or a variety of healthcare professionals. The evidence recommends the inclusion of dietitians, nurses, pharmacists, or all other disciplines with special certifications that demonstrate mastery of diabetes knowledge and training, such as BC-ADM and CDCES, can support all DSMES services, including clinical assessment.
Finally, Answer 4 is correct. 59.68% chose this answer, “Less focus on “checking the box” when delivering curriculum and more focus on the individual needs.” YES, this is the BEST Answer. The authors who gathered to write this paper, were from different parts of the country serving a wide variety of communities. I believe, by assembling this thoughtfully chosen and diverse group or diabetes advocates and educators, they created a fresh and more inclusive set of standards. The overall theme is more community engagement with a clearn focus on the individual needs versus completing check boxes of educational topics covered. I commend the authors and invite you to peruse this very important document that summarizes the delivery of effective and person centered DSMES.
2022 National Standards for Diabetes Self-Management Education and Support– A joint position statement of the American Diabetes Association, the American Association of Diabetes Educators, and the Academy of Nutrition and Dietetics.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic? You are invited to view our Setting Up a Successful DSMES Program.
Setting up a Successful DSME Program Standards | Level 2 $29 | 1.5 CEs
Recorded & Ready to Watch!
This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking certification exams or considering setting up a DSME program, this program is designed for you. We highlight the newly revised and simplified 2022 Standards and provide strategies on program implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- Describe DSME program examples from across the country.
- List the six standards for creating a successful DSME program
- Discuss marketing strategies for success
- Describe Medicare Reimbursement for diabetes care and education
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Most accurate MNT Statement based on New Standards?

For last week’s practice question, we quizzed test takers on the most accurate MNT statement based on the new ADA Standards of Care. 60% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Based on the 2022 ADA Standards of care on Medical Nutrition Therapy (MNT), which statement is most accurate?
Answer Choices:
- MNT provided by a RD/RDN is associated with A1c absolute decreases of 0.3 to 2.0 percent.
- A low carbohydrate, high protein diet is associated with increased risk of renal failure.
- With new type 2 diabetes, try to achieve A1c targets with MNT for 3 months before advancing to medication therapy.
- People with diabetes and hypertension have improved outcomes when they decrease sodium intake to less than 1,500 mg a day.
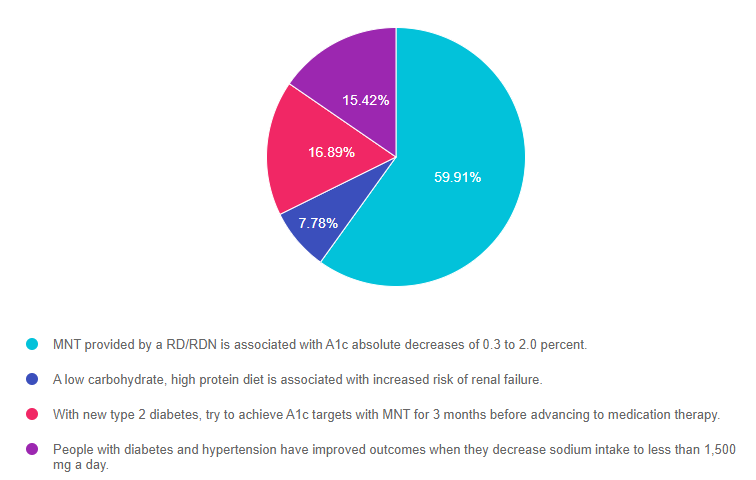
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 2, and then finally option 4.
Getting to the Best Answer
Answer 1 is correct. 59.91% chose this answer, “MNT provided by a RD/RDN is associated with A1c absolute decreases of 0.3 to 2.0 percent.” Yes, this is the best answer. When people with prediabetes or diabetes work with a registered dietitian/nutritionist to develop an individualized approach to meal planning, they are able to make significant changes in their food choices, portions and improve their overall nourishment – all resulting in significant A1C drops. The ADA Standards recommend that a person with new diabetes meet with an RD soon after diagnosis and at least annually thereafter.
Answer 2 is incorrect. 7.78% of you chose this answer, “A low carbohydrate, high protein diet is associated with increased risk of renal failure.” This juicy answer is tempting. However, there is not evidence to support the statement that high protein diets increase the risk of renal failure. The ADA does state that there is evidence to support limiting carbohydrates to improve blood glucose levels. But most important, all approaches need to be individualized.
Answer 3 is incorrect. 16.89% of respondents chose this answer, “With new type 2 diabetes, try to achieve A1c targets with MNT for 3 months before advancing to medication therapy.” For most people it can take over 5-6 years to discover diabetes and for many, there is already vessel damage and the beginnings of complications at diagnosis. For this reason and to slow the progression of complications, lifestyle and medication therapy are started simultaneously.
Finally, Answer 4 is incorrect. 15.42% chose this answer, “People with diabetes and hypertension have improved outcomes when they decrease sodium intake to less than 1,500 mg a day.” The standards recommend limiting sodium intake to about 2,300mgs a day for people with diabetes. However, they do not recommend going lower than 1,500mgs a day, because there isn’t enough data demonstrating that very low sodium intake improves heart health and it may even be harmful.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic- Our nutrition expert will review MNT for over 3 hours on April 15th.
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | High Fat & Protein Meals impact on post meal glucose?

For last week’s practice question, we quizzed test takers on the impact high-fat meals have on post-meal glucose. This was a tough one, since only 40% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: MJ is on an insulin pump and takes 1 unit of insulin for every 15 gms of carb. For a meal with 5 ounces of steak, medium baked potato with sour cream, asparagus, and salad, MJ bolused 3 units of insulin to cover carbs. What might MJ expect to happen 3 hours later?
Answer Choices:
- A glucose spike
- Hypoglycemia
- Blood glucose in target range
- Need to consume more carbs
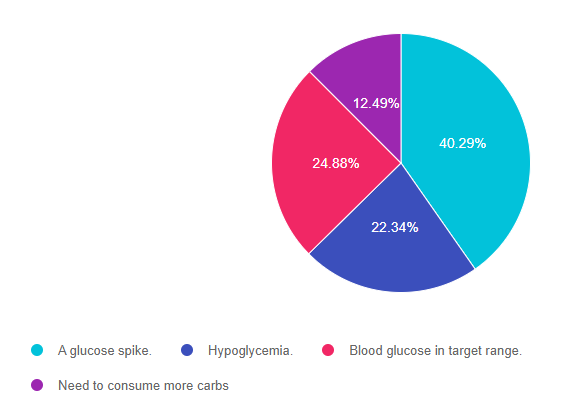
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 2, and then finally option 4.
Getting to the Best Answer
Answer 1 is correct. 40.29% chose this answer, “A glucose spike.” Great job, this is the best answer! Even though MJ gave 3 units of bolus insulin to cover the carbs from the potato, there will be a secondary glucose spike about 3 hours later from the meat protein and the sour cream. There is a growing understanding (as noted in ADA Standard 5) that people with type 1 diabetes need to not only cover for carbs in the meal, but many times they need to include a small amount of bolus insulin to cover for high fat and protein sources. The delayed post meal glucose elevation is secondary to gluconeogenesis as their body converts some of the digested fat and protein into glucose. For people using insulin pump, they can use dual wave bolus, so they get some of the bolus initially and the rest a few hours later to coincide with the second glucose spike. People on insulin injections could also inject a small amount as they see their secondary glucose rising as protein and fat impact blood sugar levels.
Answer 2 is incorrect. 22.34% of you chose this answer, “Hypoglycemia.” This is a juicy answer, but the 3 units is just the right amount to cover for the potato, veggies and salad. Plus, with the additional protein and fat consumption, MJ is unlikely to experience hypoglycemia.
Answer 3 is incorrect. 24.88% of respondents chose this answer, “Blood glucose in target range.” MJ blood sugar could be in target range one to two hours post meal, but given the additional consumption of 5 ounces of protein plus sour cream, it is likely that around hour three, MJ will experience a glucose spike.
Finally, Answer 4 is incorrect. 12.49% chose this answer, “Need to consume more carbs.” This is a juicy answer, but the 3 units is just the right amount to cover for the potato, veggies and salad. Plus, with the additional protein and fat consumption, MJ is not likely to see blood sugar drop to the point where they would need to consume more carbs.
Want to read more about his topic?
Beyond Carbohydrate Counting: Utilizing Nutrition Factors to Optimize Insulin Dosing | On the Cutting Edge| 2021 Volume 42 | No 4 – Subscription only
Benefit of supplementary fat plus protein counting as compared with conventional carbohydrate counting for insulin bolus calculation in children with pump therapy – Article
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | JR asks you; What is the Coefficient of Variation?

For last week’s practice question, we quizzed test takers on the coefficient of variation. 85% of respondents chose the best answer. We want to share this important updated information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: You are reviewing an ambulatory glucose profile with JR, a 27-year-old on an insulin pump. Time in range is 59% and the coefficient of variation is 46%. JR asks you to explain the coefficient of variation. What is the most helpful response?
Answer Choices:
- The amount of time blood glucose is at least one standard deviation below target.
- A statistic that summarizes if you are taking sufficient daily insulin based on basal rates.
- Great question that we can address later. Let’s focus on improving time in range first.
- It reflects how much your glucose levels fluctuate above and below target range.
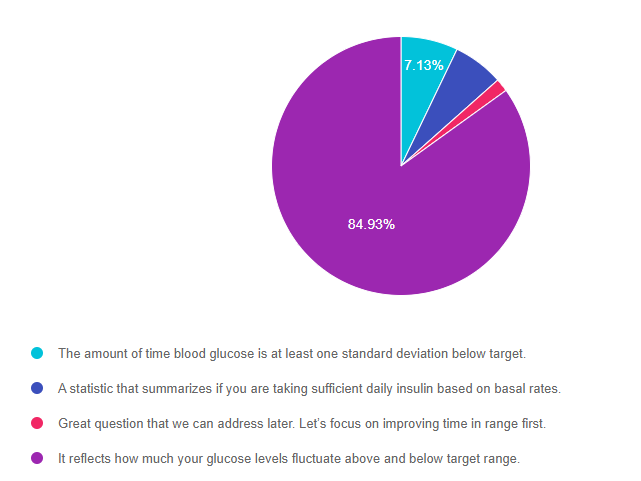
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and then finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 7.13% chose this answer, “The amount of time blood glucose is at least one standard deviation below target.” This is a juicy answer and is tempting. However, the coefficient of variation isn’t looking at only the below target blood glucose levels. It reflects how much glucose levels fluctuate above and below target range.
Answer 2 is incorrect. 6.31% of you chose this answer, “A statistic that summarizes if you are taking sufficient daily insulin based on basal rates.” Basal insulin dosing can affect glucose levels over night and between meals. But both the basal and bolus insulin affect the coefficient of variation which reflects how much the glucose levels are fluctuating above and below target range.
Answer 3 is incorrect. 1.63% of respondents chose this answer, “Great question that we can address later. Let’s focus on improving time in range first.” Time in range is important to discuss, however when using a person centered approach, we start with the topic that is most important to the person first.
Finally, Answer 4 is correct. 84.93% chose this answer, “It reflects how much your glucose levels fluctuate above and below target range.” GREAT JOB. 85% of you chose the best answer. When looking at the Ambulatory Glucose Profile, the shaded area reveals how much the glucose is fluctuating above and below target range. The goal for coefficient of variation (CV) is less than 36%, which is associated with a higher percentage of time in range.
CV is a fancy term for a simple calculation: dividing the SD by the mean glucose and multiplying by 100 to get a percentage. For example, if the SD is 50 mg/dl, and the average glucose is 150 mg/dl, then you divide 50 by 150, multiply by 100, and you get a CV of 33%.
Why use CV instead of SD? SD is highly influenced by the mean glucose – someone with a higher mean glucose will have a higher SD. This division helps “correct” and normalize glucose variability, allowing for a single variability goal (less than 36%) that applies to people with different mean glucose levels.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about diabetes technology?
Join our expert speaker, Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES, who will be delving into diabetes technology
Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | The new “F” Word

This year, the ADA Standards focused on the importance of fiber. Since fiber intake is so important to our health, we decided to deem it the new “F” word for 2022. To highlight this under-consumed nutrient, we quizzed test takers on the goal of fiber intake. 70% of respondents chose the best answer. We want to share this important updated information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: AR has type 2 diabetes, is on metformin 1000mg BID, has a UACR of 28 mg/g and a GFR of 62. AR is struggling with constipation. What are the ADA Fiber Intake Recommendations?
Answer Choices:
- 14 grams of fiber for every 1000 k/cal
- Goal is to consume about 55 grams of fiber a day
- Eat fiber at least three times a day
- Try to consume 16 oz’s legumes/ day
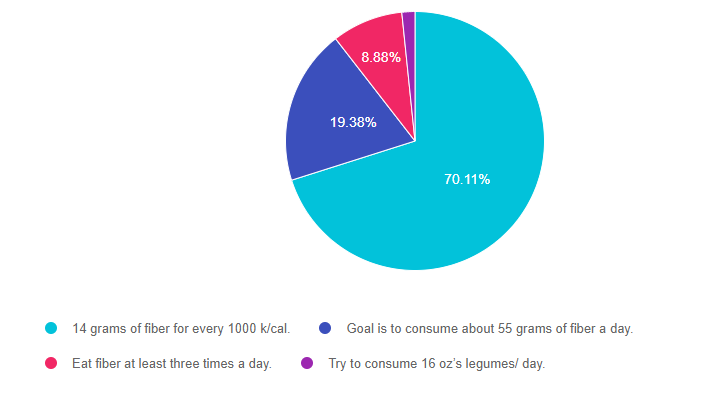
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 3, and then finally option 4.
Getting to the Best Answer
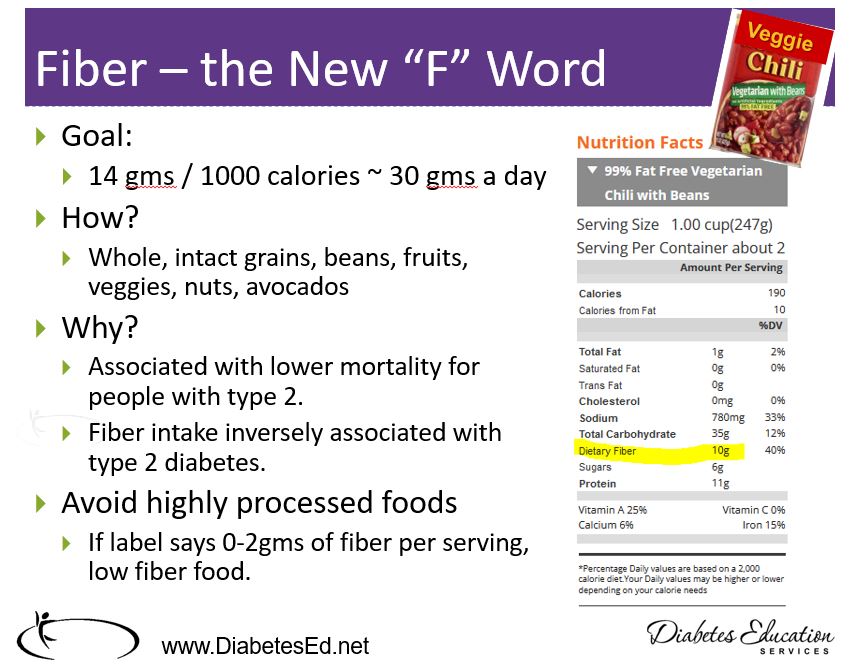
Answer 1 is correct. 70.11% chose this answer, “14 grams of fiber for every 1000 k/cal.” YES, GREAT JOB. This is the best answer based on the ADA Standards of Care and national nutrition guidelines. The daily goal is to consume about 30gms of fiber a day. Yet, most Americans only eat about half that amount. Approximately 70% of the food consumed in the U.S. is processed. Processed and fast foods are notorious for low fiber content. Fiber intake is associated with better overall health, improved longevity, and happier gut bacteria. By increasing intake of fresh fruit, legumes, vegetables, popcorn, avocados, whole grains, and nuts, we would all feel a little bit better.
Answer 2 is incorrect. 19.38% of you chose this answer, “Goal is to consume about 55 grams of fiber a day.” This is a juicy answer, but a little ambitious. The daily goal is to consume about 30gms of fiber a day. Yet, most Americans only eat about half that amount.
Answer 3 is incorrect. 8.88% of respondents chose this answer, “Eat fiber at least three times a day.” Eating fiber at each meal is a great idea, but the goal is to consume at least 30gms a day.
Finally, Answer 4 is incorrect. 1.63% chose this answer, “Try to consume 16 oz’s legumes/ day.” While legumes are very high in fiber (16 ounces of beans, packs 70gms of fiber), the goal is to consume 30gms from whatever sources of fiber the individual enjoys most.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Join our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Download Course Schedule | Download Course Flyer
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | How do they calculate UACR?

We quizzed test takers on the urinary albumin creatinine ratio. 59% of respondents chose the best answer. We want to share this important updated information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: What best describes how to measure urinary albumin creatinine ratio?
Answer Choices:
- Divide blood creatinine results with urinary albumin secretion rate.
- Collect 24-hour urine sample and add alkaline solution to determine albumin ratio quantity.
- Draw a fasting blood sample to determine ratio of creatinine in grams to albumin in milligrams.
- Divide urinary albumin concentration in milligrams by creatinine concentration in grams.
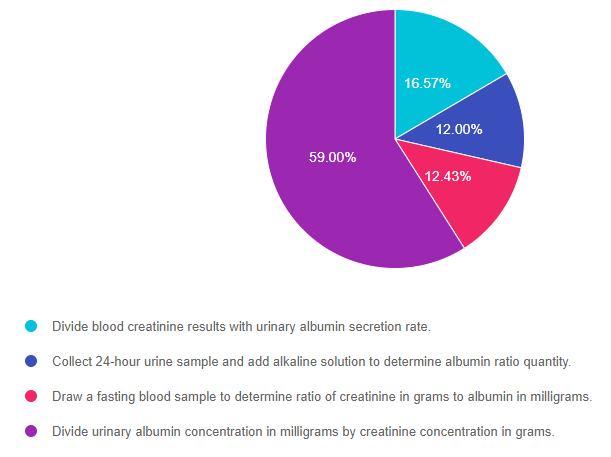
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 3, and then finally option 2.
Getting to the Best Answer
Answer 1 is incorrect. 16.57% chose this answer, “Divide blood creatinine results with urinary albumin secretion rate.” This is a juicy answer! To calculate UACR, the lab uses albumin and creatinine results from the urine only. And since it is a ratio, they divide the urine albumin levels by the urine creatinine to get the result. Please see our blog From Dipsticks to GFR – How to Evaluate Kidney Function for a detailed explanation.
Answer 2 is incorrect. 12.00%% of you chose this answer, “Collect 24-hour urine sample and add alkaline solution to determine albumin ratio quantity.” In the old days, we would collect a 24 urine samples to evaluate kidney health. However, since the spot urine albumin /creatinine ratio is so accurate, we don’t need to do the cumbersome 24-hour collection to determine UACR. Now we can evaluate UACR using a spot collection (dipstick) or lab evaluation of urine. Please see our blog From Dipsticks to GFR – How to Evaluate Kidney Function for a detailed explanation.
Answer 3 is incorrect. 12.43% of respondents chose this answer, “Draw a fasting blood sample to determine the ratio of creatinine in grams to albumin in milligrams.” To calculate UACR, the lab uses albumin and creatinine results from the urine only. And since it is a ratio, they divide the urine albumin levels by the urine creatinine to get the result. No fasting is required for this test. Please see our blog From Dipsticks to GFR – How to Evaluate Kidney Function for a detailed explanation.
Finally, Answer 4 is correct. 59.00% chose this answer, “Divide urinary albumin concentration in milligrams by creatinine concentration in grams.” GREAT JOB. You chose the best answer. Urinary Albumin Creatinine Ratio (UACR) is the ratio of urine albumin to urine creatinine. The UACR is usually already calculated on the lab report,
To determine the UACR, you divide urine albumin by creatinine, then convert it to mg/g. The reason this value is reported as a ratio as opposed to just urine albumin is to account for the concentration and hydration status of the individual which improves accuracy.
UACR is an important measure of kidney health and the goal is to measure it yearly and if elevated, more frequently.
Testing for UACR is fairly easy. The ADA has approved using a urine dipstick or a urine sample to calculate the UACR, However, according to the standards, two of three tests need to be positive to confirm diagnosis within a 3 to 6 month period before confirming a diagnosis of moderate or severe albuminuria. Exercise within 24 h, infection, fever, congestive heart failure, marked hyperglycemia, menstruation, and marked hypertension may elevate UACR independently of kidney damage. Please see our blog From Dipsticks to GFR – How to Evaluate Kidney Function for a detailed explanation.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Join our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Healthy Kidney Labs?

We quizzed test takers on kidney function. 81.64% of respondents chose the best answer. We want to share this important updated information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Evaluating kidney function is important to determine the most beneficial treatment interventions. Which of the following measurements would indicate that JR has healthy kidney function?
Answer Choices:
- Urinary albumin creatinine ratio of 30-299 mg/g with GFR of 45.
- GFR of 60 or greater and urinary albumin creatinine ratio of 2 mg/g.
- Urinary albumin creatinine ratio less than 30 mg/g and GFR of 30-45.
- Creatinine of 1.5 and urinary albumin creatinine ratio of 300 mg/g or greater.
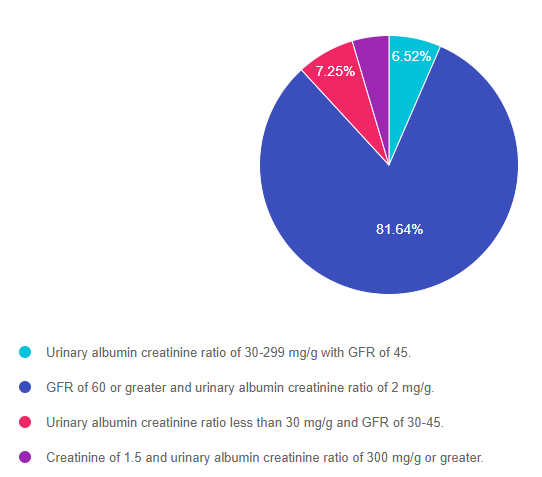
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 1, and then finally option 4.
Getting to the Best Answer
Answer 1 is incorrect. 6.52% chose this answer, “Urinary albumin creatinine ratio of 30-299 mg/g with GFR of 45.” There are two major indicators of kidney health for people with diabetes, Glomerular Filtration Rate (GFR) and Urinary Albumin Creatinine Ratio (UACR). According to the ADA Standards, to have a healthy kidney function, JR would need a GFR of 60 or greater and a UACR less than 30 mg/g. Give that JR’s UACR is elevated at 30 mg/g or greater and the GFR is sluggish at 45, this is not the best answer.
Answer 2 is correct. 81.64%% of you chose this answer, “GFR of 60 or greater and urinary albumin creatinine ratio of 2 mg/g.” YES, GREAT JOB choosing the BEST answer. There are two major indicators of kidney health for people with diabetes, Glomerular Filtration Rate (GFR) and Urinary Albumin Creatinine Ratio (UACR). According to the ADA Standards, to have a healthy kidney function, JR would need a GFR of 60 or greater and a UACR less than 30 mg/g. Since JR meets both of these criteria, we can rest well knowing JR’s kidneys are healthy and flowing.
Answer 3 is incorrect. 7.25% of respondents chose this answer, “Urinary albumin creatinine ratio less than 30 mg/g and GFR of 30-45.” There are two major indicators of kidney health for people with diabetes, Glomerular Filtration Rate (GFR) and Urinary Albumin Creatinine Ratio (UACR). According to the ADA Standards, to have a healthy kidney function, JR would need a GFR of 60 or greater and a UACR less than 30 mg/g. Even though JR’s UACR is less than 30mg/g, the GFR is sluggish at 30-45. For this reason, this is not the best answer.
Finally, Answer 4 is incorrect. 4.59% chose this answer, “Creatinine of 1.5 and urinary albumin creatinine ratio of 300 mg/g or greater.” There are two major indicators of kidney health for people with diabetes, Glomerular Filtration Rate (GFR) and Urinary Albumin Creatinine Ratio (UACR). According to the ADA Standards, to have a healthy kidney function, JR would need a GFR of 60 or greater and a UACR less than 30 mg/g. In this response, we only know the creatinine level (which is elevated), but no GFR is calculated. In addition, the UACR is very elevated at 300 mg/g. For these reasons, this is not the best answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Join our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022

Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Deluxe Version includes Syllabus, Standards and Swag*:
- Diabetes Educator Course 2022 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2022 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard, Tote Bag and Pen
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Deluxe Option for $499: Virtual Program includes:
- Q & A Session with the instructor after each webinar.
- LIVE Presentations by our team of experts.
- State of the art review of current diabetes care and technology.
- Resources for each session.
- Access to free podcasts and video recordings within a week of each live session for one year.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.