Rationale of the Week | New Standards for Kidney Disease
We quizzed test takers on the new ADA Standards of Care for Kidney Disease. 56% of respondents chose the best answer. We want to share this important info so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Based on the 2022 ADA Standards of Care, which of the following is the most accurate statement regarding chronic kidney disease and risk management?
Answer Choices:
- Monitor kidney function twice yearly if urinary albumin is 300 or greater and/or if GFR is 30-60.
- For people with GFR less than 60, relax glucose target to prevent hypoglycemia.
- If GFR is less than 30 in an individual with diabetes, avoid use of SGLT-2 Inhibitors.
- For individuals with GFR less than 60, refer to RD to encourage low protein diet.
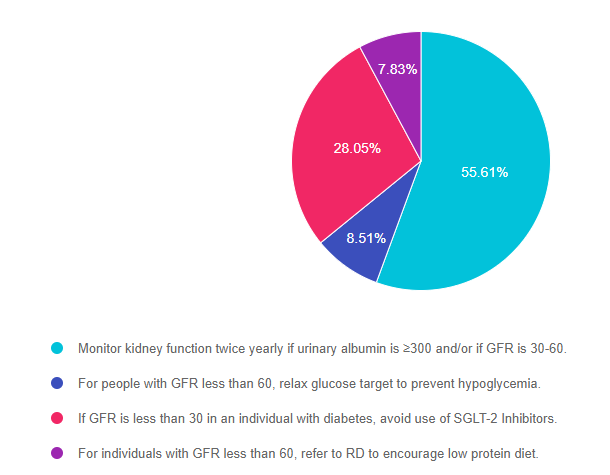
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 2, and then finally option 4.
Getting to the Best Answer
Answer 1 is correct. 55.61% chose this answer, “Monitor kidney function twice yearly if urinary albumin is 300 or greater and/or if GFR is 30-60.” YES, GREAT JOB. Most of you chose the best answer for this new recommendation. Catching renal failure early can be life saving. Two big indicators of serious renal issues include proteinuria and a diminished GFR. Early interventions (including getting BG and BP to goal) and regular monitoring can protect kidneys for the long run.
Answer 2 is incorrect. 8.51% of you chose this answer, “If GFR is less than 30 in an individual with diabetes, avoid use of SGLT-2 Inhibitors.” This is a juicy answer. The GFR cut-offs for the SGLT-2s have been changing a lot over the past year. More research is showing that, in some cases, even with a GFR less than 30 (especially in the presence of proteinuria) SGLT-2s are indicated since they have a renal protective effect. See ADA Standard 11 on Chronic Kidney Disease for more info.
Answer 3 is incorrect. 28.05% of respondents chose this answer, “People with type 2 are less likely to experience diabetes complications than those with type 1 diabetes.” According the the National Kidney Foundation, “About 30 percent of people with Type 1 diabetes and 10 to 40 percent of those with Type 2 diabetes eventually experience kidney failure.” The most important message is to encourage people with diabetes to be actively involved in their treatment plan and advocate for best medical care to protect renal function.
Finally, Answer 4 is incorrect. 7.83% chose this answer, “For individuals with GFR less than 60, refer to RD to encourage low protein diet.” This is an outdated recommendation for over the past five years. The ADA recognized that the science does not support low protein diets as a protective intervention for those with renal disease. For people with nondialysis-dependent stage 3 or higher chronic kidney disease, dietary protein intake recommendation is 0.8 g/kg body weight per day.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Enroll in Our Standards of Care Intensive | Level 2
This bundle is specifically designed for healthcare professionals who want to learn more about the ADA Standards of Diabetes Care for their clinical practice or for those who are studying for the BC-ADM or the CDCES certification exam.
2022 Live Webinar Updates
- Recorded December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- Recorded December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1 vs Type 2 Diabetes?
We quizzed test takers on the difference between Type 1 & Type 2 Diabetes. 87% of respondents chose the best answer. We want to share this important info so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JS has newly diagnosed type 1, yet their parent has type 2 diabetes. They ask you the difference between the two types of diabetes.
What is your best response?
Answer Choices:
- Type 1 and Type 2 are both autoimmune conditions, but people with type 2 don’t need insulin at first.
- Type 1 is due to a progressive destruction of the alpha cells of the pancreas.
- People with type 2 are less likely to experience diabetes complications than those with type 1 diabetes.
- Type 1 diabetes is an immune mediated condition that requires insulin from the start.
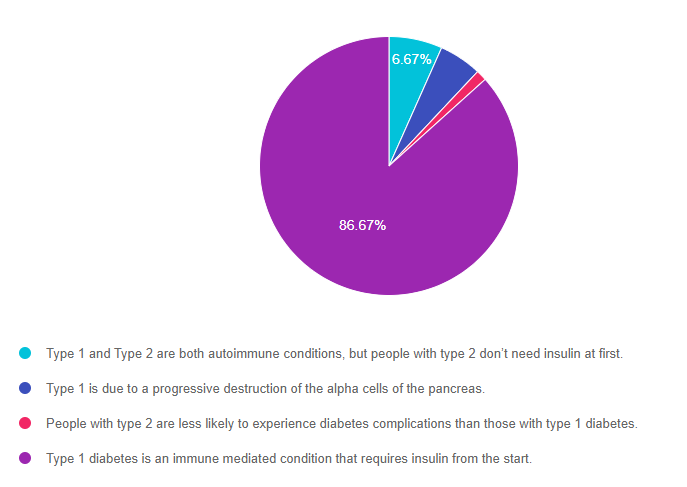
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and then finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 6.67% chose this answer, “Type 1 and Type 2 are both autoimmune conditions, but people with type 2 don’t need insulin at first.” Only type 1 diabetes is considered an immune mediated condition where there is autoimmune destruction of the beta cells. About 30% of people with type 2 will eventually require insulin due to gradual loss of beta cells.
Answer 2 is incorrect. 5.33% of you chose this answer, “Type 1 is due to a progressive destruction of the alpha cells of the pancreas.” In type 1 diabetes, there is destruction of the beta cells that produce insulin, not the alpha cells. Alpha cells produce glucagon, an important hormone that increases glucose levels.
Answer 3 is incorrect. 1.33% of respondents chose this answer, “People with type 2 are less likely to experience diabetes complications than those with type 1 diabetes.” Complications are a result of a complex interplay of genetics, lifestyle and duration plus severity of hyperglycemia. Many people with type 2 diabetes already have complications at diagnosis due to unknowingly having diabetes for an average of six years.
Finally, Answer 4 is correct. 86.67% chose this answer, “Type 1 diabetes is an immune mediated condition that requires insulin from the start.” YES, This is best answer. All people diagnosed with type 1 diabetes immediately need exogenous insulin since their beta cells have been destroyed and they are at risk for hyperglycemic crisis due to insulinopenia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more about this topic?
Enroll in our Diabetes Fundamentals | Level 1
Airs Live Jan 11th – Jan 27th, 2022 at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
2022 Live Webinar Updates
- January 11, 2022 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 13, 2022 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 18, 2022 – Class 3 – Insulin Therapy & Pattern Management 1.5 CEs
- January 20, 2022 – Class 4 – Meds Overview for Type 2 – 1.5 CEs
- January 25, 2022 – Class 5 – Goals of Care – 1.5 CEs
- January 27, 2022 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | The truth about NPH Insulin?
We quizzed test takers on NPH insulin. 57% of respondents, chose the best answer. We want to share this important info so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
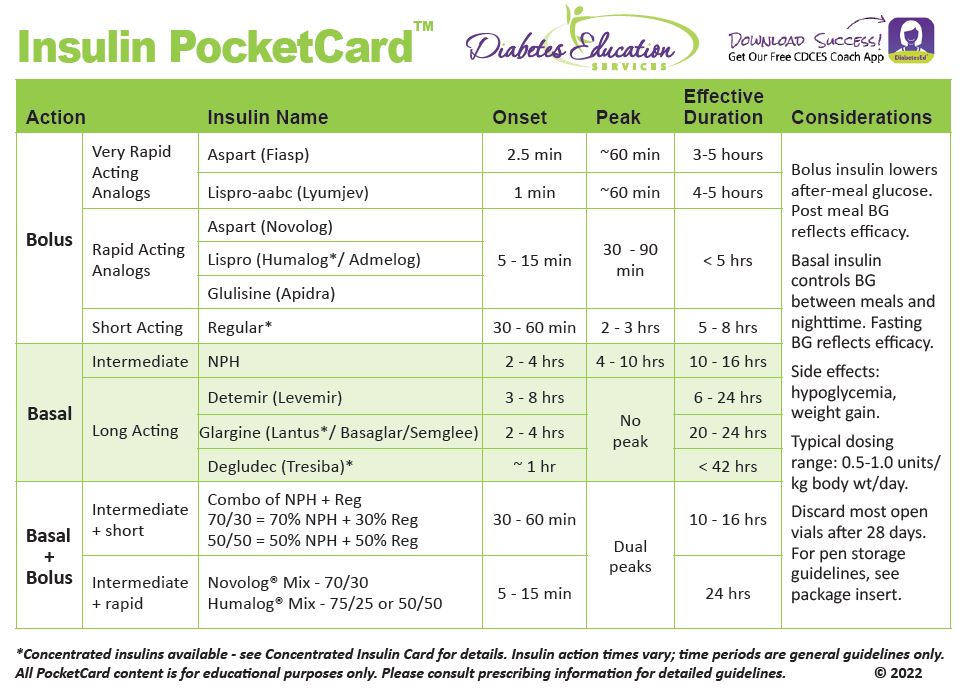
Question: NPH insulin, introduced in 1946 was one of the first basal insulins. It is considered intermediate-acting basal insulin since the duration of action is about a half-day. Given its effectiveness and affordability, it is on the World Health Organization’s List of Essential Medicines.
Which of the following is a true statement regarding NPH insulin?
Answer Choices:
- In most states, it can be purchased over the counter without a prescription
- Instructions include to gently shake before injection to adequately mix the particles
- NPH stands for Natural Proinsulin Hagedorn
- Due to its high rates of hypoglycemia, NPH is no longer recommended.
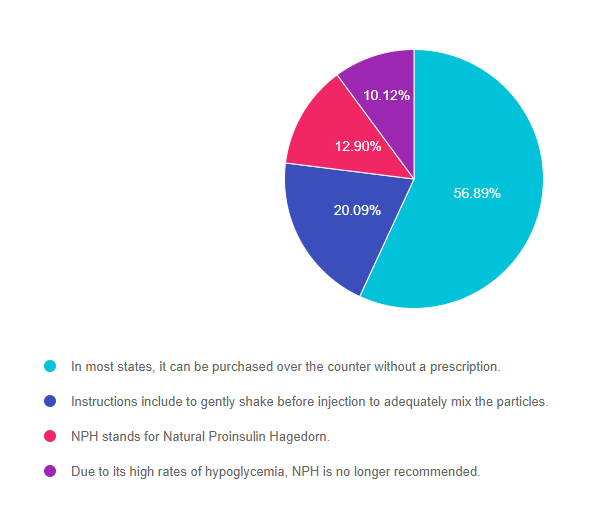
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 3, and then finally option 4.
Getting to the Best Answer
Answer 1 is correct. 56.89% chose this answer, “In most states, it can be purchased over the counter without a prescription.” YES, GREAT JOB. Actually, there are three over-the-counter insulins that are available for purchase without a prescription. They include regular insulin, NPH (intermediate-acting), and 70/30 insulin, a premixed combination of NPH and regular.
People might be interested in purchasing these older insulins because of their lower cost. Walmart sells all three types under the ReliOn brand umbrella for roughly $25 a vial. Chain pharmacies can also sell regular, NPH, and 70-30 insulin. However, OTC insulin is more frequently sold at Walmart than other chain pharmacies, likely due to the considerably lower price point.
– For more info on the different types of insulins, download our FREE PocketCards.
– For Info on affordable insulin, please visit our Insulin Cost Savings Resource page.
Answer 2 is incorrect. 20.09% of you chose this answer, “Instructions include to gently shake before injection to adequately mix the particles.” Shaking NPH insulin can cause clumping and is not recommended. According to the package insert, the most accurate instruction is to gently roll NPH insulin or invert it repeatedly until the particles are evenly distributed. NPH looks milky and homogeneous when properly mixed.
Answer 3 is incorrect. 12.90% of respondents chose this answer, “NPH stands for Natural Proinsulin Hagedorn.” So close. The name refers to N for neutral, P for protamine (a protein), and H for its creator scientist name Hans Christian Hagedorn. NPH insulin is FDA-approved in the adult and pediatric population to manage type 1 and type 2 diabetes. It is also useful in gestational diabetes. More info.
Finally, Answer 4 is incorrect. 10.12% chose this answer, “Due to its high rates of hypoglycemia, NPH is no longer recommended.” NPH insulin does have a somewhat higher risk of hypoglycemia. One way to decrease the risk of hypoglycemia and high day-to-day variability is to thoroughly re-suspend NPH until it is uniformly cloudy before injecting. This will improve the pharmacodynamic and pharmacokinetic profile of NPH insulin, leading to less hypoglycemia. NPH insulin onset of action is 2 to 4 hours, time to peak effect is 4 to 10 hours, and total duration 10-16 hours. The newer basal insulins don’t have a peak, so there is slightly less hypoglycemia. However, with careful dosing and education, NPH insulin can provide a lower cost and effective alternative to the newer analog insulins, especially for those living with type 2 diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more? Join our Webinar on Hyperglycemic Crisis, which is ready for viewing!
Want to learn more about this topic?
Enroll in our Diabetes Fundamentals | Level 1
Airs Live Jan 11th – Jan 27th, 2022 at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
2022 Live Webinar Updates
- January 11, 2022 – Class 1 – Getting to the Nitty Gritty 1.5 CEs
- January 13, 2022 – Class 2 – Nutrition and Exercise 1.5 CEs
- January 18, 2022 – Class 3 – Insulin Therapy & Pattern Management 1.5 CEs
- January 20, 2022 – Class 4 – Meds Overview for Type 2 – 1.5 CEs
- January 25, 2022 – Class 5 – Goals of Care – 1.5 CEs
- January 27, 2022 – Class 6 – Hypoglycemia, Sick Days, Monitoring, Foot Care 1.5 CEs
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | “I take insulin when I feel like it”
We quizzed test takers on identifying why a teenager with type 1 is only taking insulin “when they feel like it”. 73% of respondents, chose the best answer. We want to share this important info so you can pass it on to people living with diabetes, your colleagues and prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is a 15-year-old admitted to the hospital with DKA for the second time this month. JR says they are tired of their parents always telling them how to manage their diabetes. They just stopped wearing their continuous glucose monitor and tell you they “take insulin when they feel like it”.
What best describes what this teenager is experiencing?
Answer Choices:
- Diabetes distress.
- Diabetes burnout.
- Severe anxiety.
- Fear of hypoglycemia.
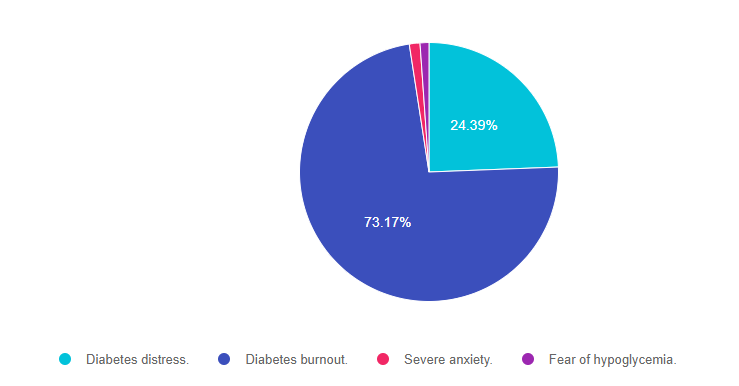
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 3, and then finally option 4.
Getting to the Best Answer
Answer 1 is incorrect. 24.39% chose this answer, “Diabetes distress.” JR certainly is dealing with aspects of diabetes distress, which is described as feeling like it’s too much or that things are out of control. However, the fact that “JR just stopped wearing their continuous glucose monitor and is only “taking insulin when they feel like it”, gives us a more complete understanding that JR is experiencing more than distress. Please see our blog on How to Identify Diabetes Distress and Burnout.
Answer 2 is correct. 73.17% of you chose this answer, “Diabetes burnout.” YES, this is the BEST ANSWER. Great job! Diabetes burnout is an emotional reaction that is usually more intense than diabetes distress. A person in the state of burnout is someone with diabetes who has grown tired of managing their condition, then simply ignores it for a period of time. The fact that JR stopped wearing their CGM and only takes insulin when they feel like it, are strong indicators that JR is on a diabetes vacation and is burned out. This might mistakenly be perceived as non-compliance, but these behaviors indicate that JR is really struggling and needs the support of the health care team. Visit our page on Diabetes Burnout or Distress? 12 Reframes that can HELP for ideas to support people struggling with their diabetes self care.
Answer 3 is incorrect. 1.33% of respondents chose this answer, “Severe anxiety.” Hardly any of you chose this because in this vignette, JR is not exhibiting any signs of anxiety. Good job.
Finally, Answer 4 is incorrect. 1.11% chose this answer, “Fear of hypoglycemia.” Since this vignette does not mention that JR has experienced lows or that JR lets blood sugars run high to prevent lows, this is not the best answer. Good job.
Learn more about Diabetes Distress in our December Newsletter.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more? Join our Webinar on Hyperglycemic Crisis, which is ready for viewing!
Want to learn more about this topic?
Enroll in our Level 2 | Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
Updated for the new 2022 ADA Standards of Care

This presentation will include the latest information on Social Determinants of health, assessment strategies, and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers. Life studies are used to apply theory to real-life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Objectives:
- State strategies to assess and address social determinants of health
- Discuss health care delivery systems using a person-centered approach
- List screening tools that can help detect distress, depression, trauma, and cognitive decline
- Describe psycho-social and emotional barriers to diabetes self-management
- Provide strategies for healthcare professionals to identify and overcome barriers to self-care
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below 2022 Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- Recorded December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- Recorded December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of Week | What is the Truth about Hyperglycemic Crisis?
We quizzed test takers on hyperglycemic crisis. 61% of respondents, chose the best answer. We want to share this important info so you can pass it on to people living with diabetes and your colleagues and prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: People with type 1 or type 2 diabetes can experience hyperglycemic crises.
Which of the following is true about Diabetes Ketoacidosis (DKA)?
Answer Choices:
- People with Latent Autoimmune Diabetes (LADA) are not at risk of DKA.
- DKA is associated with hyperkalemia and elevated pH.
- DKA can be managed with IV or Sub-Q insulin therapy.
- People with type 1 on SGLT-2s have lower risk of DKA than those with type 2.
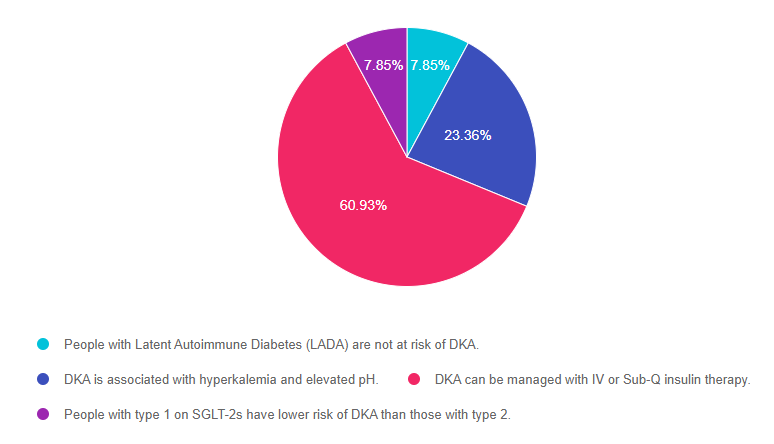
As shown above, the most common choice was option 3, the second most common answer was option 2, then a tie for option 1 and option 4.
Getting to the Best Answer
Answer 1 is incorrect. 7.85% chose this answer, “People with Latent Autoimmune Diabetes (LADA) are not at risk of DKA.” Any person with a substantial insulin deficiency (including type 1, type 2 and people with LADA) are at risk of ketoacidosis. The risk increases during periods of illness, inadequate calorie intake or when an individual is not injecting adequate insulin. Most individuals with LADA need insulin within 6 months of diagnosis to maintain glucose levels. Without insulin injections, people with LADA can’t use glucose for fuel and will start burning fat for energy, which leads to excess circulating ketones and potentially DKA.
Answer 2 is incorrect. 23.36% of you chose this answer, “DKA is associated with hyperkalemia and elevated pH.” Part of this answer is correct, which makes it a juicy answer. This common test taking pitfall is easy to fall into. It is true that people in DKA can become hyperkalemic, but they also always experience acidosis, which causes the pH to fall, not elevate.
Answer 3 is correct. 60.93% of respondents chose this answer, “DKA can be managed with IV or Sub-Q insulin therapy.” Yes, GREAT job, this is the BEST answer. Mild or moderate DKA can be treated using SubQ insulin and all levels of DKA can be treated with IV insulin. The treatment choice is based on health care setting, provider preference, and the patient’s presentation.
Finally, Answer 4 is incorrect. 7.85% chose this answer, “People with type 1 on SGLT-2s have lower risk of DKA than those with type 2.” Some people living with Type 1 may be started on an SGLT-2 (which is OFF-LABEL) by their provider to help with glucose management and lower insulin needs. People with type 2 diabetes, may also be started on an SLGT-2. Both groups are at increased risk for experiencing DKA on a SGLT-2. However, the person with type 1 is at HIGHER risk of experiencing DKA, because they have an absolute insulin deficiency and if they reduce their insulin dose too much, they might need to convert from using glucose for fuel to fat for fuel, leading to DKA.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Want to learn more? Join our Webinar on Hyperglycemic Crisis, which is ready for viewing!
Want to learn more about this topic?
Level 2 | Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
Annual Webinar Recorded on December 15th
This course discusses common causes of hyperglycemia crises. Topics include hyperglycemia secondary to medications and insulin deprivation. The difference and similarities between Diabetes Ketoacidosis and Hyperosmolar Hyperglycemic Syndrome are also covered. Treatment strategies for all situations are included.
Objectives:
- Common causes of hyperglycemic crises.
- The difference and similarities between DKA and HHS and treatment strategies
- Causes and treatment of hyperglycemic crises.
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below Annual Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | I am non-binary. Will having diabetes impact my sexual health?
We quizzed test takers on diabetes and sexual health. 73% of respondents, chose the best answer. Since we are addressing diabetes distress in our December newsletter, we thought this would be the right time to explore this topic in more depth. As we all know, sexual health and well being are interrelated. We want to share this important info on discussing sexual well being, so you can pass it on to people living with diabetes and your colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is a 33-year-old who is non-binary and was recently diagnosed with type 2 diabetes. During your assessment, JR asks if diabetes can affect their sexual health.
What is the best response?
Answer Choices:
- That is a complicated question that is best discussed with your provider
- Here is a pamphlet on LGBTQ+ issues and sexuality that explains the most frequently asked questions.
- According to the data, there is a higher rate of erectile dysfunction in people living with diabetes.
- There is a relationship between elevated blood sugars and sexual health.
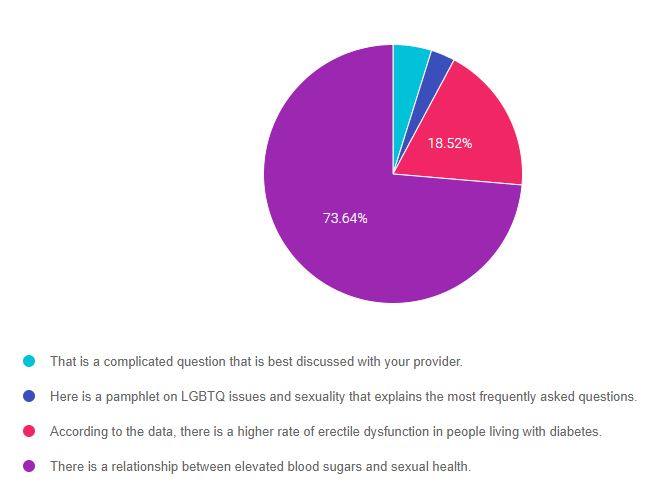
As shown above, the most common choice was option 4, the second most common answer was option 3, then option 1, and finally option 2.
Getting to the Best Answer and Providing Inclusive Care
If you are thinking about taking the certification exam, providing person-centered care is at the heart of the exam. Being familiar with diabetes care across the lifespan and for diverse populations is also really important. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer based on the person’s characteristics.
Inclusive Care and Gender Identity
In this Question of the week, we are working with JR who identifies as non-binary. Let’s take a moment and address how this might impact our approach to care.
First, since JR let’s us know that they are non-binary, what does that mean?
Nonbinary describes someone whose gender doesn’t fit within the gender binary of a man or a woman. “Nonbinary” is an umbrella term that expresses a wide range of gender identities; other terms someone may use to describe themselves is genderqueer or gender non-conforming, among others. It is important to check in with each person and ask them how they identify. One way of doing this is to introduce yourself, along with your pronouns, and then ask what pronouns the other person uses, as in the example below.
“Hello, my name is Beverly and I go by ‘she, her’ pronouns. What pronouns do you use?”
or
“How would you like me to refer to you?”
By paying careful attention to each person’s experience from the moment they walk in the door until we say goodbye, we can find ways to create a more inclusive environment. This awareness of the details, such as inclusive gender questions on intake forms or gender-neutral signage on the bathrooms, are great first steps to show your care and respect for those you work with.
Next, what do we know about providing care to members of the lesbian, gay, bisexual, transgender, and queer (LGBTQ+) community with diabetes?
Studies have shown that those who are LGBTQ+ are subject to unique health disparities and worse health outcomes than their heterosexual counterparts, which has clinical relevance in the delivery of diabetes care and education. Diabetes care and education specialists are in a pivotal position to advocate for this medically underserved and vulnerable population, to make sure they get the best possible care.
Lastly, JR wants to know how diabetes will affect their sexual health.
At this juncture, we may provide a general overview of how elevated blood sugars can affect blood vessel health and cause nerve damage, that may impact their sexual function over time (such as difficulty feeling pleasure or achieving an orgasm). Then we might ask if they have any particular questions. Our willingness to explore this sensitive topic free of judgment will be very meaningful. And, it’s okay if this feels new and uncomfortable.
“We all have our own personal experiences and internalized biases which impact the care we deliver. Our job is to practice cultural humility by checking in with our biases so they do not interfere with helping someone find a path to thriving with diabetes. It can feel uncomfortable at first, but as we take the time to expand our knowledge about others, it will feel more comfortable”
And just know, it takes time to get up to speed. I’d encourage readers to check out the ADCES handout below and watch this funny video clip that a colleague sent me, “What “The Sex Talk” Looks Like Now, by Alternatino. This video made me crack up and appreciate the nuance of all the terms. Thanks so much, for your willingness to consider this topic. I truly hope you find it helpful in improving in delivery of care.
Getting to the Best Answer
Answer 1 is incorrect. 4.82% chose this answer, “That is a complicated question that is best discussed with your provider.” Even though sexual health may not be our area of expertise, we can certainly provide a general answer and explore their particular questions. Of course, if a question is beyond our knowledge, referring back to the provider would be best.
Answer 2 is incorrect. 3.01% of you chose this answer, “Here is a pamphlet on LGBTQ+ issues and sexuality that explains the most frequently asked questions.” This is not the best answer, because it doesn’t address the question the person is asking. JR wants to know how diabetes can affect their sexual health, not the relationship between LGBTQ+ and sexuality.
Answer 3 is incorrect. 18.52% of respondents chose this answer, “According to the data, there is a higher rate of erectile dysfunction in people living with diabetes.” It is true that up to 50% of men with diabetes experience erectile dysfunction. However, we are not sure of JR’s sex assigned at birth, so this answer may not apply to JR. Instead, we could provide a general overview of how elevated blood sugars can affect blood vessel health and cause nerve damage, that may impact their sexual function over time (such as difficulty feeling pleasure or achieving an orgasm).
Finally, Answer 4 is correct. 73.64% chose this answer, “There is a relationship between elevated blood sugars and sexual health.” YES. This is the BEST answer. And, we might then ask if they have any particular questions.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this important learning activity!
Resources for Inclusive Care
ADCES Inclusive Care for LGBTQ+ People with Diabetes Handout – this handout provides definitions, terms to avoid, and a cultural competency checklist to help you move towards improving inclusivity within your practice.
All Gender Restroom Sign PDF
A Guide To Gender Identity Terms by NPR – A glossary for gender identity terms to use more inclusive language.
Diabetes Prevention and Management for LGBTQ+ People Handout – this handout includes research of diabetes within the LGBTQ+ community, along with clinical considerations, programs, and resources for diabetes educators to use within their practice.
Policies on Lesbian, Gay, Bisexual, Transgender & Queer (LGBTQ+) issues – this resource by the American Medical Association lists all the current healthcare policies in place for the LGBTQ+ community.
Helio’s LGBTQ+ Health Updates Resource Center – this is a “collection of news articles and features that provide the latest information on the unique health needs of individuals in the LGBTQ+ community.”
Want to learn more about this topic?
Enroll in our Level 2 | Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
Annual Update Airs Live on December 21st at 11:30 am PST
This presentation will include the latest information on Social Determinants of health, assessment strategies, and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers. Life studies are used to apply theory to real-life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Objectives:
- State strategies to assess and address social determinants of health
- Discuss health care delivery systems using a person-centered approach
- List screening tools that can help detect distress, depression, trauma, and cognitive decline
- Describe psycho-social and emotional barriers to diabetes self-management
- Provide strategies for healthcare professionals to identify and overcome barriers to self-care
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below 2022 Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Who is struggling with Diabetes Distress?
Our November 30th Question of the week quizzed test takers on Diabetes Distress. 75% of respondents, chose the best answer, which is awesome. Providing person centered care and assessing for diabetes distress are both critically important knowledge points for clinical practice and also for the certification exams.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
About 30% of people living with type 1 diabetes experience diabetes distress.
Which of the following statements reflects someone struggling with diabetes distress?
Answer Choices:
- I just can’t keep up with all this diabetes self-care stuff.
- I am having trouble with carbohydrate counting.
- I just don’t want to get out of bed in the morning.
- I don’t want to wear a diabetes bracelet or necklace.
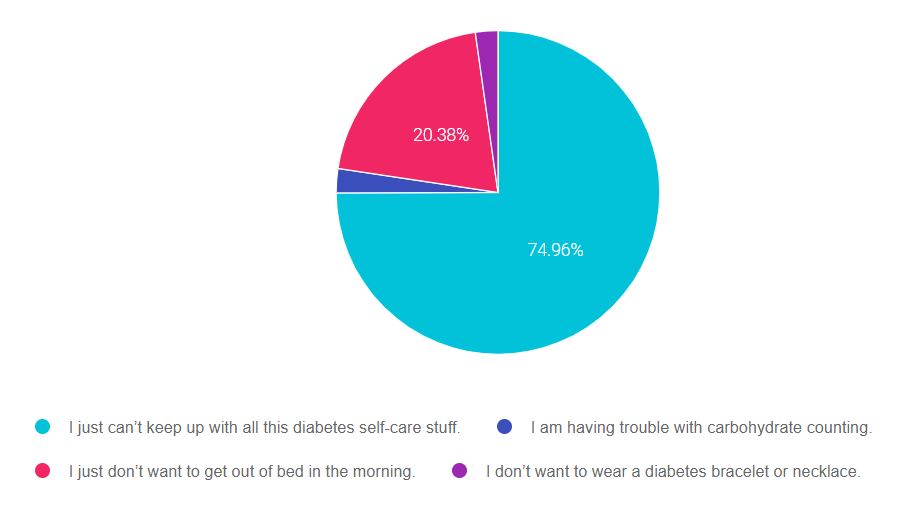
As shown above, the most common choice was option 3, the second most common answer was option 2, then option 4, and finally option 1.
Getting to the Best Answer
Answer 1 is correct. 74.96% chose this answer, “I just can’t keep up with all this diabetes self-care stuff.” Yes, GREAT JOB. When diabetes self-care all starts feeling like it’s too much or like it’s out of control, that’s when we might say a person is experiencing diabetes distress. Regimen distress is the most common area that people with diabetes come up against. Please see our blog on How to Identify Diabetes Distress and Burnout for information on how to help with diabetes distress.
Answer 2 is incorrect. 2.42% of you chose this answer, “I am having trouble with carbohydrate counting.” This comment indicates a common knowledge gap that can be addressed through providing resources and carb counting information and does not indicate distress.
Answer 3 is incorrect. 20.38% of respondents chose this answer, “I just don’t want to get out of bed in the morning.” If a person with diabetes makes this statement, we would be concerned that they are grappling with more than distress. This comment would prompt us to screen for depression. Please see this link to download the Diabetes Distress Scale and other psychosocial screening tools.
Finally, Answer 4 is incorrect. 2.25% chose this answer, “I don’t want to wear a diabetes bracelet or necklace.” Although we recommend that people taking insulin wear diabetes identification in case of emergency, it is not mandatory and they can chose not to wear one. This comment alone does not indicate diabetes distress.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Please see our blog on How to Identify Diabetes Distress and Burnout for more information.
Please see this link to download the Diabetes Distress Scale and other psychosocial screening tools.
Want to learn more about this topic?
Enroll in our Level 2 | Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
Annual Update Airs Live on December 21st at 11:30 am PST
This presentation will include the latest information on Social Determinants of health, assessment strategies, and approaches. We will explore the psychosocial issues that can discourage individuals from adopting healthier behaviors and provides strategies to identify and overcome these barriers. Life studies are used to apply theory to real-life situations. A great course for anyone in the field of diabetes education or for those looking for a new perspective on assessment and coping strategies.
Objectives:
- State strategies to assess and address social determinants of health
- Discuss health care delivery systems using a person-centered approach
- List screening tools that can help detect distress, depression, trauma, and cognitive decline
- Describe psycho-social and emotional barriers to diabetes self-management
- Provide strategies for healthcare professionals to identify and overcome barriers to self-care
Intended Audience: A great course for healthcare professionals in the field of diabetes education looking for a straightforward explanation of identification and treatment of hyperglycemic crises.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Enroll in our entire Level 2 – Standards of Care to join us for the below 2022 Live Webinar Updates. All courses air at 11:30 a.m. (PST)
- December 15, 2021 – Hyperglycemic Crises, DKA & HHS Standards | 1.0 CE
- December 21, 2021 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach Standards | 1.5 CEs
- February 3, 2022 – ADA Standards of Care | 2.0 CEs
- March 24, 2022 – Meds Management for Type 2 – 1.5 CEs
- March 29, 2022 – Lower Extremity Assessment 1.5 CEs
- April 26, 2022 – Microvascular Complications, Eye, Kidney Nerve Disease 1.5 CEs
- April 28, 2022 – Critical Assessment of Diabetes Patient 2.0 CEs
- May 10, 2022 – Cardiovascular Disease and Diabetes Standards 1.5 CEs
- May 12, 2022 – Older Adults and DIabetes 1.5 CEs
- May 17, 2022 – Tots to Teens – Diabetes Standards 1.5 CEs
- May 19, 2022 – Pregnancy and Diabetes 1.5 CEs
- May 26, 2022 – Hospital and Hyperglycemia 1.5 CEs
- July 21, 2022 – Setting up a Successful Diabetes Program 1.5 CEs
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | 1923 Noble Recipients for Discovery of Insulin?
Our November 23rd Question of the week quizzed test takers on the Nobel Prize insulin. 34% of respondents, chose the best answer. We are excited to share this info about the discovery of insulin with you.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
In 1923, the Nobel Prize in Physiology or Medicine was awarded for the discovery of insulin.
Which group of scientists were the recipients of the award?
Answer Choices:
- Dr. Banting and Dr. Best
- Dr. Collip, Dr. Banting and Dr. Best
- Dr. Banting, Dr. Collip, Dr. Macleod, Dr. Best
- Dr. Banting and Dr. Macleod
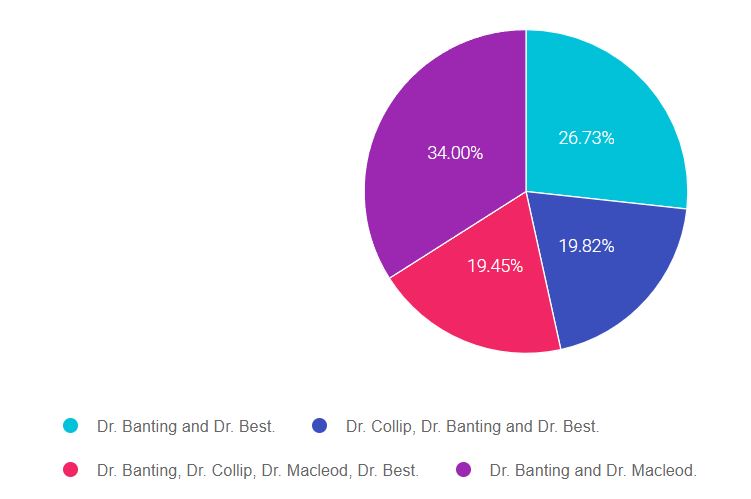
As shown above, the most common choice was option 3, the second most common answer was option 2, then option 4, and finally option 1.
Discovery of Insulin Nobel Prize 1923

The Nobel Prize in Physiology or Medicine 1923 was awarded jointly to Frederick Grant Banting and John James Rickard Macleod “for the discovery of insulin.”
According to the summary at the Nobel Prize Website – Previous doctors realized that diabetes is caused by a lack of insulin, which is formed in parts of the pancreas but could not prove it. Frederick Banting suspected that another substance formed in the pancreas, trypsin, broke down the insulin.
In John MacLeod’s laboratory in 1921, Frederick Banting and Charles Best treated dogs so that they no longer produced trypsin. Insulin could then be extracted and used to treat diabetes. A short while later, Dr. Collip made a breakthrough in purifying the extract, using alcohol in slightly over 90 percent concentration to precipitate out the active ingredient (insulin).
Although Dr. Banting, Dr. Collip, Dr. Macleod, and Dr. Best were all involved in the discovery of insulin, only Dr. Banting and the lab director, Dr. Macleod received the official Nobel prize for Medicine.
Getting to the Best Answer
Answer 1 is incorrect. 26.73% chose this answer, “Dr. Banting and Dr. Best.” Credited for their experiments on dogs at the University of Toronto in 1921 that eventually led to the discovery of insulin.
Answer 2 is incorrect. 19.82% of you chose this answer, “Dr. Collip, Dr. Banting, and Dr. Best”. Although Dr. Collip made a breakthrough in purifying the extract, using alcohol in slightly over 90 percent concentration to precipitate out the active ingredient (insulin), he, along with Best, was not recognized with a Nobel Prize.
Answer 3 is incorrect. 19.45% of respondents chose this answer, “Dr. Banting, Dr. Collip, Dr. Macleod, Dr. Best” All four of these physicians played a major part in the discovery and availability of insulin, but only Dr. Banting and Dr. Maccleod were awarded the Nobel prize.
Finally, Answer 4 is correct. 34% chose this answer, “Dr. Banting and Dr. Macleod” YES, GREAT JOB.
The Nobel Prize in Physiology or Medicine 1923 was awarded jointly to Frederick Grant Banting and John James Rickard Macleod “for the discovery of insulin.” According to the summary at the Nobel Prize Website – In John MacLeod’s laboratory in 1921, Frederick Banting and Charles Best treated dogs so that they no longer produced trypsin. Insulin could then be extracted and used to treat diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want more practice questions? Enroll in our
Test Taking Practice Exam Toolkit Webinar
20 Sample Practice Questions
You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
For many of us, taking the certification exam is a nerve-wracking process.
During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
2 Ways to Join Test Taking Webinar
Watch Webinar for FREE
This includes a review of 20 sample test questions with test-taking strategies. This does not include access to the recorded webinar or the practice questions.
Purchase for $49
This includes access to the recorded version of this webinar on your Online University Student Portal.
Plus, the Test Taking Toolkit provides you with over 220 sample online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test-taking confidence.
Don’t worry if you can’t make it live.
Your registration guarantees access to the recorded version.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.