Rationale of the Week | The First Person to Receive Insulin?

This month, we are quizzing test takers on the history of diabetes and the discovery of insulin. Our November 2nd Question of the week quizzed test takers on the first insulin injections in humans. 47% of respondents, chose the best answer. We are excited to share this info with you in celebration of National Diabetes Month.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question:
Which of the following statements is true regarding the first experiments using insulin in humans?
Answer Choices:
- Since insulin worked successfully on dogs, no experimentation was needed on humans to gain approval.
- Leonard Thompson, a 14-year-old received the first successful insulin injection in January 1922.
- The initial insulin was derived from the exocrine cells of ligated canine and porcine pancreases.
- Elizabeth Hughes was the first insulin recipient in 1921 but the insulin formulation didn’t work to lower her glucose until 1922.
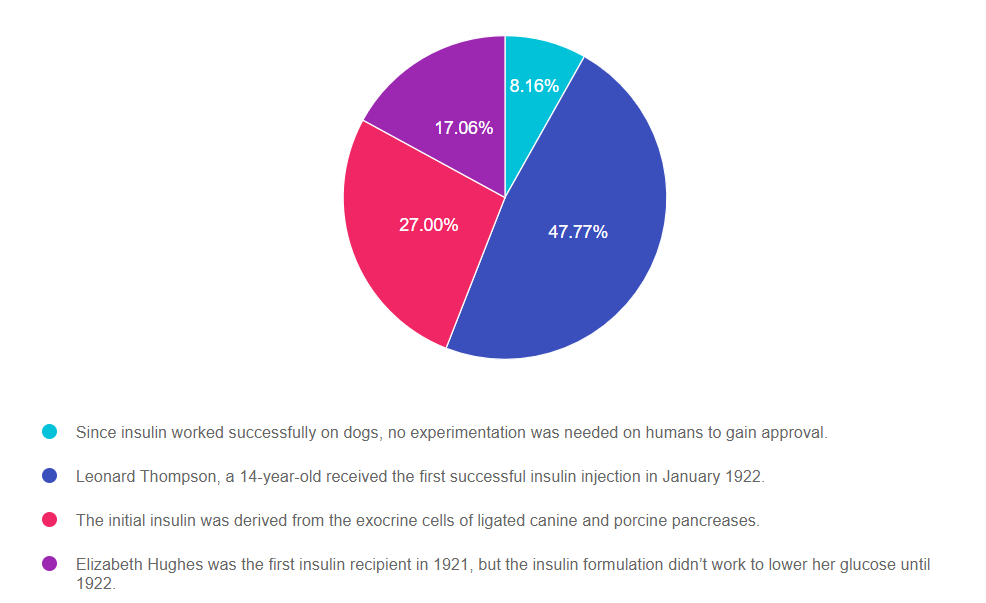
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through, eliminate FALSE answers and then choose the BEST answer.
Answer 1 is incorrect. 8.16% chose this answer, “Since insulin worked successfully on dogs, no experimentation was needed on humans to gain approval.” Insulin’s approval was certainly fast tracked, but experiments were conducted on animals first, than humans, before releasing for widespread use and saving the lives of millions.
Answer 2 is correct. 47.77% of you chose this answer, “Leonard Thompson, a 14-year-old received the first successful insulin injection in January 1922.” YES, great job. On January 11, 1922, Leonard Thompson was the first person to receive insulin when he was only 14 years of age. The first injection caused an allergic reaction due to impurities. After James Collip improved the insulin refinement process, the second dose of canine pancreas extract was delivered to the young patient twelve days after the first. Thompson’s health rapidly improved and he lived another 13 years on insulin injections, dying at the young age of 26 due to pneumonia.
Answer 3 is incorrect. 27% of respondents chose this answer, “The initial insulin was derived from the exocrine cells of ligated canine and porcine pancreases.” This is a juicy sounding answer! However, insulin was derived from the endocrine cells of dogs, ox and porcine, to produce insulin; not the exocrine cells that produce digestive enzymes.
Finally, Answer 4 is incorrect. 17.06% chose this answer, “Elizabeth Hughes was the first insulin recipient in 1921 but the insulin formulation didn’t work to lower her glucose until 1922.” Another juicy answer since it has some elements of truth, however Elizabeth was not the first person to receive insulin therapy. Elizabeth developed diabetes in 1918 at age 11 and by the fall of 1922, she weighed only 45 pounds, due to her body’s inability to store energy and the strict 800 calorie diet she followed to prevent ketosis. Elizabeth arrived in Toronto in August 15, 1922 and received insulin injections from Dr. Banting and she recovered rapidly. She returned home to Washington D.C . Thanksgiving Day 1922 on a 2200 calorie meal plan and insulin injections. She lived to the age of 73, and received over 42,000 insulin injections over her lifetime. You can read more in the book, Breakthrough, which chronicles Elizabeth Hughes, the discovery of insulin and the Making of a Medical Miracle.
More Reading on the Discovery of Insulin
The Discovery of Insulin – Vecchio I, Tornali C, Bragazzi NL, Martini M. The Discovery of Insulin: An Important Milestone in the History of Medicine. Front Endocrinol (Lausanne). 2018;9:613. Published 2018 Oct 23. doi:10.3389/fendo.2018.00613
Breakthrough, which chronicles Elizabeth Hughes, the discovery of insulin and the Making of a Medical Miracle.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries!
You can register now to watch on-demand
Click here to learn more and get started!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Virtual DiabetesEd Specialist Conference Deluxe | Recorded & Ready for Viewing! | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best strategy to Prevent Hypo in Hospital?

Our September 28th Question of the week quizzed test takers on the best strategy to prevent hypo in the hospital. 64% of respondents, chose the best answer. We are excited to share info so you can pass on helpful info to people living with diabetes and your hospital colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: As a diabetes specialist at a local hospital, one of your quality improvement goals is to prevent nocturnal hypoglycemia.
Which of the of following policy changes would most likely lower rates of overnight and morning hypoglycemia?
Answer Choices:
- Make sure the medication carts are stocked with glucagon rescue kits.
- Eliminate insulin sliding scale and encourage basal insulin therapy.
- Collaborate with dietary to make sure all people with diabetes get protein plus carb snack.
- Implement a plan to decrease basal insulin dose if morning glucose is less than 100 mg/dl.
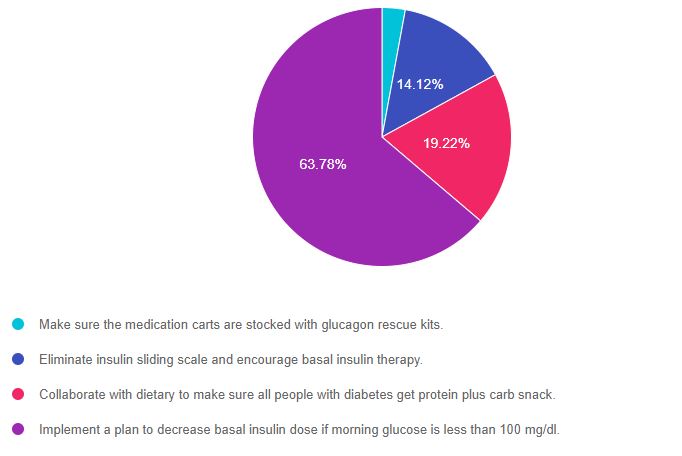
As shown above, the most common choice was option 4, the second most common answer was option 3, then option 2, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and considerations for people with diabetes in the acute care setting. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 2.88% chose this answer, “Make sure the medication carts are stocked with glucagon rescue kits.” Since the question is asking “what policy changes would most likely lower rates of overnight and morning hypoglycemia“, this is answer does not address the problem in the question; what policy change would PREVENT hypoglycemia. Having glucagon rescue meds would treat hypoglycemia, but not prevent it.
Answer 2 is incorrect. 14.12% of you chose this answer, “Eliminate insulin sliding scale and encourage basal insulin therapy.” It is true that the ADA does not recommend insulin sliding scale for inpatient management of diabetes since it is not an effective way to manage hyperglycemia. In addition, since sliding scale is usually administered with meals, it is not the most likely culprit causing morning hypoglycemia. Generally speaking, too much basal insulin is usually the cause of morning hypoglycemia. So stopping the sliding scale and encouraging basal insulin, is not the BEST answer to address the question and reduce morning hypoglycemia.
Answer 3 is incorrect. 19.22% of respondents chose this answer, “Collaborate with dietary to make sure all people with diabetes get protein plus carb snack.” Studies have shown that providing a carb snack at bedtime can decrease risk of nocturnal and morning hypoglycemia. But, if the basal insulin dose is too much, the person could still experience hypoglycemia, even with a carb snack. P.S, adding protein has not been shown to sustain the action of the carb and enhance hypoglycemia prevention. We never want to “feed” the insulin. We always want to give the least amount of insulin to get glucose to target and keep people safe.
Finally, Answer 4 is correct. 63.78% chose this answer, “Implement a plan to decrease basal insulin dose if morning glucose is less than 100 mg/dl.” YES, this is the BEST Answer. GREAT JOB. To keep inpatients safe, creating a policy that notifies the medical team when the morning glucose level is less than 100 mg/dL coupled with a reduction of basal insulin dose, would be an effective strategy to prevent morning hypoglycemia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries!
You can register now to watch on-demand
Click here to learn more and get started!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Virtual DiabetesEd Specialist Conference Deluxe | Recorded & Ready for Viewing! | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | “My life is a mess”

Our October 19th Question of the week quizzed test takers on a person who is clearly in crisis. 36% of respondents, chose the best answer. We feel it is important to share this rationale of the week, so you can advocate for people struggling with mental health while trying to manage their diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is 26 years old with newly diagnosed diabetes. JR keeps missing appointments and when you finally get a hold of them on the phone, they start crying and say “my life is a mess”. JR is struggling with addiction, periods of houselessness and extra weight in addition to diabetes.
Based on this information, what is the most likely barrier to JR engaging in self-care?
Answer Choices:
- Adverse Childhood experiences (ACEs)
- JR is struggling with depression
- Diabetes distress is at the core of the listed behaviors
- Grieving and denial of diabetes diagnosis
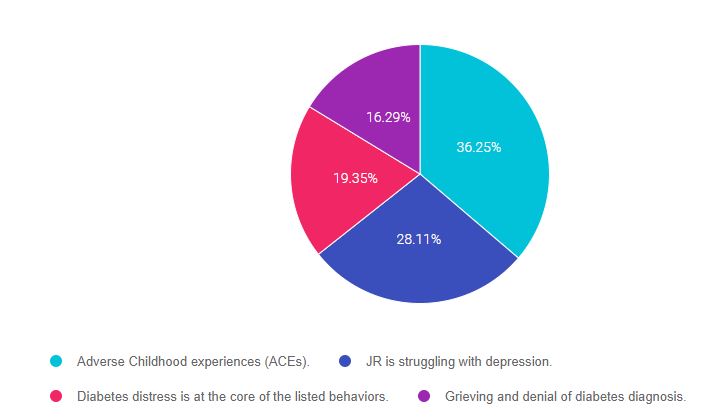
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and mental health considerations for people with diabetes . This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is correct. 36.25% chose this answer, “Adverse Childhood Experiences (ACEs).” YES, Good job, this is the BEST Answer. JR is missing appointments and when you finally get a hold of them, they say, “my life is a mess”. In addition, we know that JR is struggling with addiction, periods of houselessness and extra weight in addition to diabetes. These are all signs that JR has lived through adverse childhood experiences and toxic stress. By addressing this and providing resources, we can help JR move toward healing. See our ACE Resource page for more info.
Answer 2 is incorrect. 28.11% of you chose this answer, “JR is struggling with depression.” Is this situation, depression can be considered, but we don’t hear the hallmark statements associated with depression – “Loss of pleasure in things that used to bring them joy or feeling down or hopeless”. ACE’s are a better match for what JR is describing. See our Psychosocial Care Resource Page– for articles and screening tools.
Answer 3 is incorrect. 19.35% of respondents chose this answer, “Diabetes distress is at the core of the listed behaviors.” Is this situation, diabetes distress certainly can be considered, but it doesn’t seem to be the driving force behind JR’s struggle with addiction, periods of houselessness and extra weight. Diabetes distress is more heavily associated with diabetes specific related behaviors (fear of hypo, provider doesn’t understand my diabetes, etc.). See our Psychosocial Care Resource Page– for articles and the diabetes distress screening tool.
Finally, Answer 4 is incorrect. 16.29% chose this answer, “Grieving and denial of diabetes diagnosis.” Is this situation, grieving and denial can certainly can be considered, but it doesn’t seem to be the driving force behind JR’s struggle with addiction, periods of houselessness and extra weight. Diabetes denial is more heavily associated with lack of self-care; not checking blood glucose, avoiding medications, eating “whatever”. We don’t hear any of that from this person. The best explanation is that JR has lived through adverse childhood experiences and toxic stress. By addressing this and providing resources, we can help JR move toward healing. See our ACE Resource page for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn about this important topic?
Join Coach Bev for an honest conversation on
The Impact of Adverse Childhood Experiences on Health
Adverse childhood experiences (ACE) are associated with an increased risk of diabetes, heart disease, cancer and a variety of other health consequences for adults. This session reviews how diabetes care and education specialists can provide screening, assessment, and trauma-informed care to individuals who experienced ACEs and are living with toxic stress. We will explore strategies to address ACES and improve outcomes for individuals and communities. Throughout, we will focus on supporting self-care with a focus on recognizing and promoting resilience.
Topics include:
- Discuss the benefits of assessing Adverse Childhood Experiences (ACE) in individuals with diabetes.
- State the relationship between ACE Scores and risk of future health complications.
- Describe a person-centered approach to fostering resilience and self-care for individuals with toxic stress.
- Identify two strategies to provide trauma-informed care in your work setting.
2 Ways to Join the Webinar
This includes access to the recorded version of this webinar on your Online University Student Portal and 1.0 CE.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in enhancing their diabetes medication knowledge.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of Week | 90 years old and hungry. Best action?

Our October 12th Question of the week quizzed test takers on the best strategy for a 90-year-old who states “they feel hungry” all the time. 76% of respondents, chose the best answer. We are excited to share this rationale of the week, so you can advocate for people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: HM is living with type 2 diabetes and is 90 years old with a BMI of 32. HM’s most recent A1c was 9.6% and their GFR is 16. The provider stopped the metformin due to the diminished kidney function and HM is currently on no diabetes medications. To manage HM’s blood sugar, the provider ordered a low-calorie restrictive meal plan for HM. HM was a chef for 40 years and tells you, “they feel hungry” all the time. Based on this assessment, you decide to contact the provider.
Which of the following would be the best suggestion?
Answer Choices:
- Ask provider to add a bedtime snack to reduce hunger.
- Encourage HM to take a short walk after meals to reduce post prandial hyperglycemia.
- Reassure HM that limiting calories is the best plan to keep blood glucose on target.
- Contact provider with suggestion to start HM on once daily basal insulin.
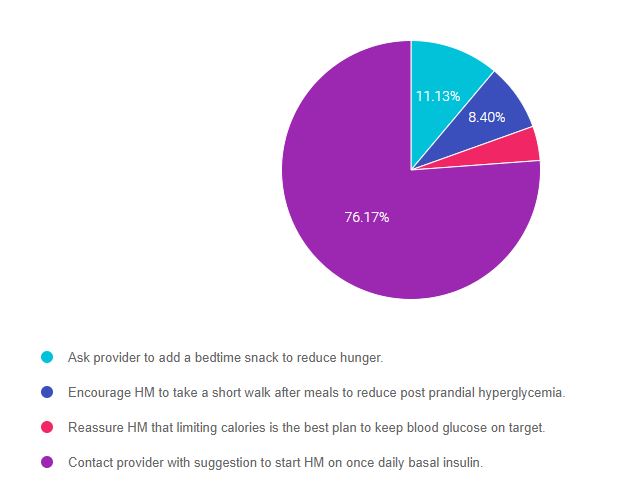
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and considerations for people with diabetes across the lifespan. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 11.13% chose this answer, “Ask provider to add a bedtime snack to reduce hunger.” While it is true that HM is hungry, a bedtime snack is not the best solution since it might contribute to already elevated blood sugars. We need to figure out a way to get blood glucose levels to goal while providing adequate nutrition.
Answer 2 is incorrect. 8.40% of you chose this answer, “Encourage HM to take a short walk after meals to reduce post prandial hyperglycemia.” Post meal walks are an excellent way to decrease post meal blood sugars, but they most likely won’t be enough to get HM out of glucose toxicity. Given that HM’s A1c is 9.6%, the average blood sugars are around 230 mg/dl. HM will need more than post meal jaunts to get blood glucose to target.
Answer 3 is incorrect. 4.30% of respondents chose this answer, “Reassure HM that limiting calories is the best plan to keep blood glucose on target.” In this situation, we need to consider quality of life issues. Given that HM is 90 years old and they were a chef, limiting calories to the point of hunger is not a strategy that considers HM’s needs, values and wants. A better approach would be to create a person-centered solution.
Finally, Answer 4 is correct. 76.17% chose this answer, “Contact provider with suggestion to start HM on once daily basal insulin.” YES, GREAT JOB. In this situation we requested that the provider start HM on 10 units of 70/30 insulin in the morning. This simple intervention will help HM in numerous ways:
- allows more food flexibility
- renal protection due to lower glucose levels
- decreased nerve pain
- increase HM’s energy
- improve HM’s quality of life.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn about this question and more as you’re studying for the CDCES Exam?
Enroll in our CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 43 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Intensive Insulin Therapy with A1c 6.2%

Our September 21st Question of the week quizzed test takers on Intensive Insulin Therapy with A1c 6.2%. Three quarters (74%) of respondents, chose the best answer. We are excited to share info so you can pass on correct info to people living with diabetes and your colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: HR is a 78-year-old with a stroke and limited cognition with diabetes for 8 years and is on intensive insulin therapy: HR takes bolus insulin at meals and basaglar at night. HR has an A1c is 6.2% and employs a part time caretaker.
What is the best response in this situation?
Answer Choices:
- Start HR on an insulin pump and CGM to prevent hypoglycemia.
- Discuss de-intensifying insulin regimen.
- Using a strength-based approach, reinforce the importance of keeping the A1c less than 7%.
- Evaluate for diabetes related distress.
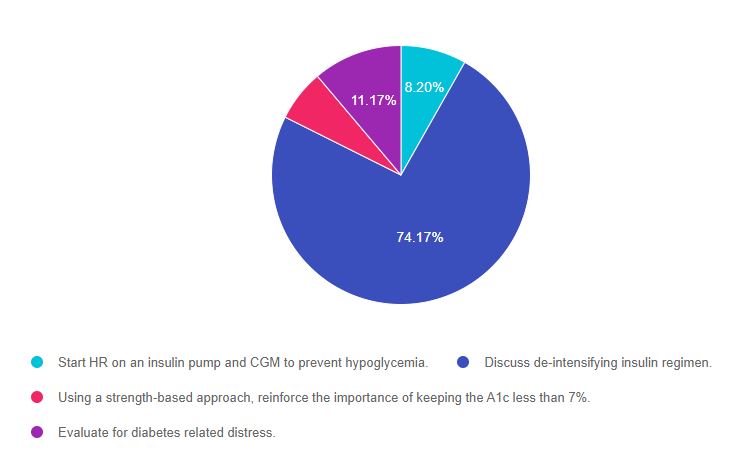
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 1, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and considerations for people with diabetes across the lifespan. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 8.20% chose this answer, “Start HR on an insulin pump and CGM to prevent hypoglycemia.” This is not the best answer because we want to provide person-centered care based on the unique situation of this individual. HR has a history of a stroke, limited cognition and relies on a part time caregiver. It doesn’t seem realistic to provide pump and CGM training to HR given the cognitive limitations and the caregiver is only part-time. It is unlikely that the two of them would be comfortable enough or have the skill level to help oversee this complex technology and changing insertion sites.
Answer 2 is correct. 74.17% of you chose this answer, “Discuss de-intensifying insulin regimen.” YES. This is the best answer. Since HR is on multiple daily injections and has an A1c in the low 6% range, we know they are most likely experiencing episodes of hypoglycemia. To address this, we would need to discuss goals of care with HR and their caregivers and share our concerns about the risk and danger of hypoglycemia. We need to de-intensify this management plan. Based on the outcome of the discussion with HR, this could be accomplished by: reducing the overall insulin dose, switching to twice a day 70/30 insulin, or evaluating if oral medications could be trialed to reduce the need for insulin.
Answer 3 is incorrect. 6.46% of respondents chose this answer, “Using a strength-based approach, reinforce the importance of keeping the A1c less than 7%.” Using a strength-based approach is always a good idea, but the main issue in this question is that HR’s A1c is only 6.2%. According to the ADA Standards of Care, the A1c target in this situation would be individualized based on safety considerations, quality of life, and the goals and values of the person living with diabetes. For older, frail individuals at risk of hypoglycemia, a safer A1c target would be 7% – 8%.
Finally, Answer 4 is incorrect. 11.17% chose this answer, “Evaluate for diabetes-related distress.” Even though it is always important to consider people’s emotional response to diabetes, this answer does not address the key issue presented in this question. The first priority would be to make sure HR is safe, with a reduced risk of hypoglycemia and a realistic insulin regimen.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What Teaching Tip for New Med – finerenone?

Our September 14th Question of the week quizzed test takers on a new med. Less than half, 47% of respondents, chose the correct answer. This was a hard question since this finerenone was only recently FDA approved. We are excited to share info about this med along to you, so you can pass on correct info to people living with diabetes and kidney disease.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR has a GFR of 43 and lives with type 2 diabetes. JR excitedly brings you an article that talks about finerenone (Kerendia), a newly approved non-steroidal mineralocorticoid receptor antagonist which is indicated for people with chronic kidney disease (CKD) associated with Type 2 diabetes.
If JR is started on this medication, what instruction would you provide?
Answer Choices:
- Make sure to take this medication on an empty stomach
- Contact the provider if you notice ankle swelling
- Notify your provider if you experience a non-productive cough
- Avoid taking medication with grapefruit or grapefruit juice.
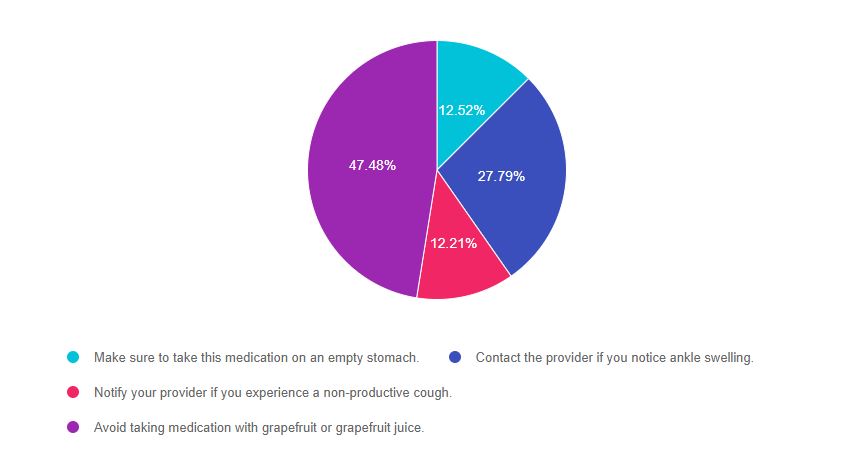
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 4, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know about newly approved diabetes medications, although it may take at least a year to appear in exams. However, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 12.5% chose this answer, “Make sure to take this medication on an empty stomach.” If you don’t know anything about a particular medication and are forced to guess, this answer is pretty unlikely to be the best answer, for one reason. Most meds don’t need to be taken on an empty stomach. Two diabetes related meds, levothyroxine and oral semaglutide DO need to be taken on an empty stomach, but an empty stomach is not required for most other meds. Finerenone can be taken with or without food.
Answer 2 is incorrect. 27.8% of you chose this answer, “Contact the provider if you notice ankle swelling.” This was another juicy answer that we purposefully included. There is a class of diabetes medications, the TZDs (pioglitazone and rosiglitazone) that can cause ankle swelling, so this answer might have seemed familiar to you. Also when trying to find false answers, you may want to consider that it seems unlikely that a medication that slows kidney failure would have edema as a side effect.
Answer 3 is incorrect. 12.2% chose this answer, “Notify your provider if you experience a non-productive cough.” This juicy answer goes with a common blood pressure medication class, ACE Inhibitors, that people with diabetes are often prescribed to manage hypertension. With finerenone, the major consideration is monitoring the potassium in the first month of initiation.
Answer 4 is correct. 47.5% of respondents chose this answer, “Avoid taking medication with grapefruit or grapefruit juice.” GREAT JOB, this is the best answer. Since finerenone is a CYP3A4 substrate, the package insert recommends to avoid taking finerenone with other strong cype3A4 inhibitors. It also advises to avoid taking finerenone with grapefruit or grapefruit juice. Great job!
Want to learn more about finerenone?
Check out our New Updated Med Cheat Sheets 2021 (page 2) and consider attending our Virtual Conference with Dr. Diana Isaacs, who will speak more to this topic. You can also check out our Blog Post on New Meds for Diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Getting to the Right Carb Count

Our September 7th Question of the week quizzed test takers on carb counting. 55% of respondents chose the correct answer. This was a hard question. Figuring out how much insulin to cover carbs is an important topic to review, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: LS uses an insulin pump and CGM. Most recent report reveals LS is running 56% time in range and 44% above target range. LS asks for help with carb counting. A typical breakfast includes: ½ cup of milk, 2 tablespoons peanut butter and 1 piece whole grain bread, 3 oz’s of grapes and one cup of black coffee with Splenda. LS’s insulin to carb ratio for breakfast is 1:12, for lunch and dinner is 1:15.
Based on this, how much insulin does LS need for breakfast?
Answer Choices:
- 3.1 units
- 2.4 units
- 3.0 units
- 2.5 units
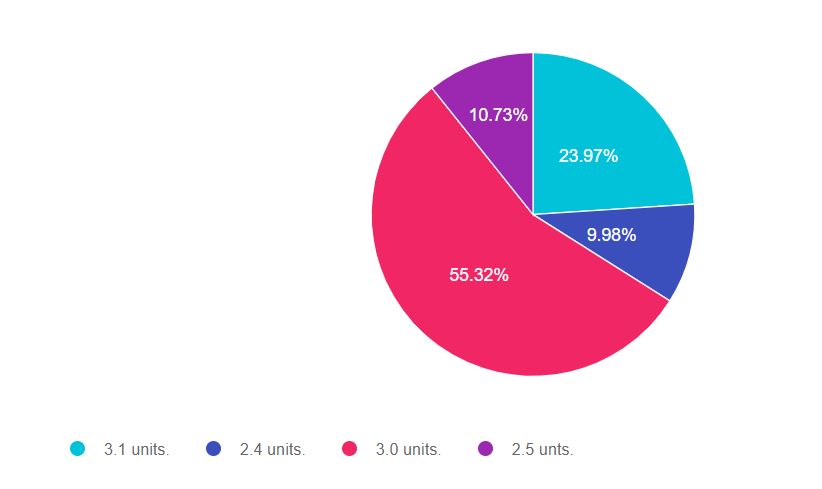
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 4, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, do careful math, be familiar with the exchange list and choose the BEST answer.
Diabetes Exchange List – a brief summary of serving size and carbohydrate counts for common foods. Excellent study tool for the exam.
Here are the carb counts of the foods listed:
- ½ cup of milk = 6gms
- 2 tablespoons peanut butter = 0
- 1 piece whole grain bread = 15gms
- 3 oz’s of grapes = 15gms
- one cup of black coffee with Splend = 0 carbs
- Total carbs for this meal =36gms
LS’s insulin to carb ratio:
- breakfast is 1:12
- lunch and dinner is 1:15
Answer 1 is incorrect. 23.97% chose this answer, “3.1 units.” If you chose this answer you are so close. For the exam, remember that one cup of milk has 12gms of carbohydrate (not 15gms). Please see the link to the exchange list for the carb counts of common foods.
Answer 2 is incorrect. 9.98% of you chose this answer, “2.4 units.” If you chose this answer, you may have used the lunch/dinner insulin to carb ratio of 1:15 instead of the breakfast ratio of 1:12. This is an easy mistake to make, so make sure to read the question carefully and take your time doing the math. You got this.
Answer 3 is correct. 55.32% of respondents chose this answer, “3.0 units.” GREAT JOB. This is the best answer. The total carb intake for LS is 36 gms. Since the Insulin to Carb (I:CR) ratio for breakfast is 1:12, to find out how much insulin LS needs for breakfast, just divide gms of carb by the I:CR or 36 / 12 = 3 units.
Finally, Answer 4 is incorrect. 10.73% chose this answer, “2.5 units.” If you chose this answer. there are 2 things to be aware of: one cup of milk has 12gms of carbohydrate (not 15gms) and you may have used the lunch/dinner insulin to carb ratio of 1:15 instead of the breakfast ratio of 1:12. These are easy mistakes to make, so make sure to read the question carefully, be familiar with common carbs and take your time doing the math. You got this.
Diabetes Exchange List a brief summary of serving size and carbohydrate counts for common foods. Excellent study tool for the exam.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about carb counting and more?
We address this topic from many different angles during our Virtual Course!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best intervention for JR?

Our August 31st Question of the week quizzed test takers on interventions. Over 90% of respondents chose the correct answer. Great job! We thought that this was an important topic to review, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is 43 with type 2 diabetes who shows up for their usual visit and happens to mention that they have had moments of feeling dizzy over the past few months. A few times, they have checked their blood sugars during these spells, and they were 121 and 136. JRs medications include glipizide 10mg BID, metformin 1000mg BID, lisinopril 20mg, atorvastatin 20mg. JR has lost about 10 lbs since their last visit by eating more whole foods and grains and less fast foods.
Based on this assessment, what is the next best action?
Answer Choices:
- Suggest that JR starts on aspirin given their cardiovascular risk profile.
- Recommend JR get a home blood pressure monitor.
- Assess if JR might need a sleep study to evaluate for sleep disorders.
- Encourage JR to increase activity level, to decrease cardiovascular risk.
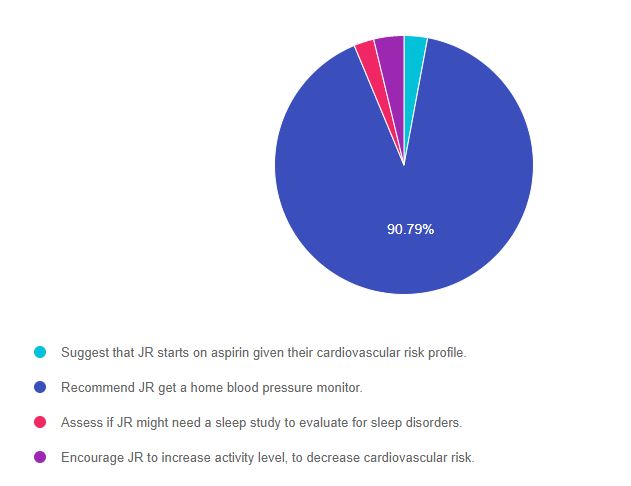
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 2, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 2.93% chose this answer, “Suggest that JR starts on aspirin given their cardiovascular risk profile.” Aspirin therapy is recommended for those 50 and older with existing or at risk for a cardiovascular event. Since JR is younger than 50, this is not the best answer.
Answer 2 is correct. 90.79% of you chose this answer, “Recommend JR get a home blood pressure monitor.” Yes, GREAT JOB. Most of you chose this best answer. Most likely, the dizziness is a result of lower blood pressure secondary to weight loss and treatment with an ACE Inhibitor (lisinopril). The ADA Standards recommend that people on blood pressure medications self-monitor their blood pressure at home to detect changes in pressure that warrant a reduction or intensification of anti-hypertensive therapy.
Answer 3 is incorrect. 2.51% of respondents chose this answer, “Assess if JR might need a sleep study to evaluate for sleep disorders.” While it is true that many people with diabetes have sleep disorders, in this case study there is not enough supporting clinical symptoms to support a sleep study. For example if JR was complaining of waking up tired or waking up gasping for air, plus they exhibit other risk factors, then further sleep evaluation might be warranted.
Finally, Answer 4 is incorrect. 3.77% chose this answer, “Encourage JR to increase activity level, to decrease cardiovascular risk.” Encouraging activity to improve health is an important part of self-care coaching. However, in this case, since JR is complaining of “dizziness”, for safety, we might even back off a little from recommending activity until we determine the cause of JRs dizziness.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








