Rationale of the Week | Thick calluses coupled with leg pain?

Our August 24th Question of the week quizzed test takers on thick calluses coupled with leg pain. 61% of respondents chose the correct answer. We thought that this was an important topic to discuss further, so we can pass on correct info to people living with diabetes.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR has lived with type 1 diabetes for over twenty years. JR arrived in the clinic with thick calluses on both feet and complaints of calf pain when walking for more than 10 minutes. JR’s pulses are difficult to palpate.
What diagnosis best matches JR’s presentation?
Answer Choices:
- Peripheral polyneuropathy.
- Diabetes venous stasis syndrome.
- Peripheral arterial disease.
- Charcot foot.
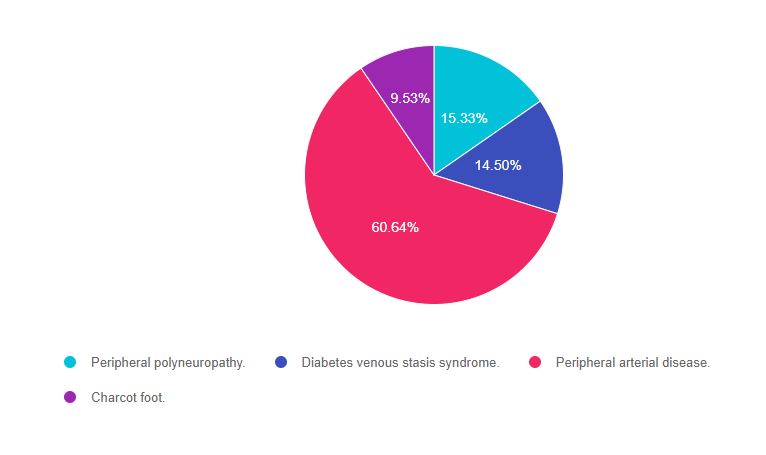
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 2, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer. If you want to learn more about lower extremities, we invite you to join our Virtual Course or check out our Level 2 Online Courses.
Answer 1 is incorrect. 15.33% chose this answer, “Peripheral polyneuropathy.” This juicy answer is tempting, however it does not match the symptoms detailed by JR. A person with peripheral polyneuropathy will typically complain of numbness, tingling and leg pain at night. They may also have thick calluses. However, there are two clues that indicate a mismatch between question and answer. JR is “complaining of calf pain when walking for more than 10 minutes with difficulty locating pulses.” These chief complaints indicate a different pathology. Keep reading to find out more.
Answer 2 is incorrect. 14.50% of you chose this answer, “Diabetes venous stasis syndrome.” This is another juicy answer with a made up condition that is designed to sound familiar. In general, with venous disease, pulses are still palpable since there is adequate blood flow to lower extremities. There are two clues that indicate a mismatch between question and answer. “JR is complaining of calf pain when walking for more than 10 minutes with difficulty locating pulses.” These chief complaints indicate a different pathology. Keep reading to find out more.
Answer 3 is correct. 60.64% of respondents chose this answer, “Peripheral arterial disease.” YES, this is the BEST answer. Great job. JR is exhibiting the classic signs of inadequate arterial blood flow to the lower extremities, or peripheral arterial disease. JR’s complaints of “calf pain when walking for more than 10 minutes with difficulty locating pulses” indicate poor arterial circulation and warrant referral to a provider for complete CV risk assessment.
Finally, Answer 4 is incorrect. 9.53% chose this answer, “Charcot foot.” This answer is tempting. Charcot foot is characterized by severe foot inflammation and structural collapse. Since JR is “complaining of calf pain when walking for more than 10 minutes with difficulty locating pulses”, these symptoms do not match the usual complaints associated with Charcot foot. Good try, see answer 3 for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of Week – | Which One is Autonomic Neuropathy? We made an oops!

For our August 17th Question of the Week, 39% of respondents chose the best answer. This is due in part to our error. We mis-keyed the best answer for the first 96 respondents (we quickly fixed it as soon as we discovered the error). So, you may want to retake this question before you read on to discover the answer. Coach Bev sincerely apologizes if this caused any of you distress! But today, we are making it right. Thanks for your patience and ongoing participation!
Before we start, if you don’t want any spoilers and you tried the question on Tuesday morning, you can answer below: Answer Question
Question 1: Which of the following are considered diabetes autonomic neuropathies?
- Decreased sexual arousal, pins and needles sensations in lower extremities.
- Loss of protective sensation and urinary incontinence.
- Resting tachycardia and esophageal dysmotility.
- Hypoglycemia unawareness and insensate feet.
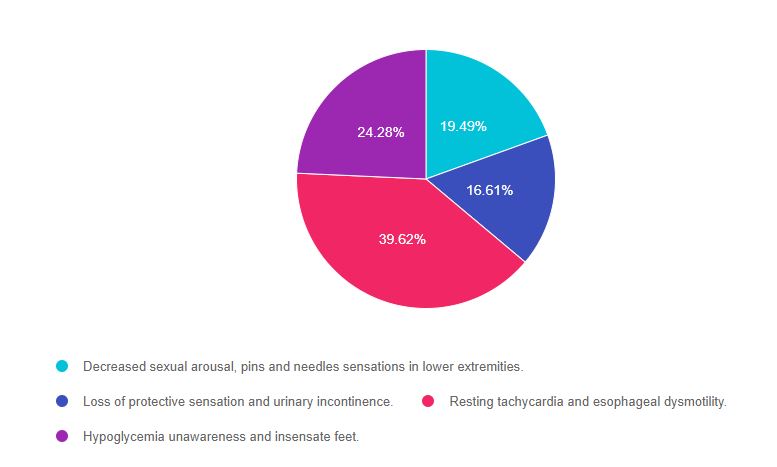
As shown above, the most common choice was option 3, the second most common answer was option 4, then option 1, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for specialty topics like microvascular disease. Be familiar with nerve disease presentation and screening as listed in the ADA Standards of Care on Microvascular health and treatment options. We also invite you to join our webinar (see below). Also, the tests will often provide a 2 part answer, one part being correct and the other part incorrect. Of course, if any part of the answer is incorrect, it is not the best answer. A great test taking tip to hold onto to when your sympathetic nervous system is in full gear. You got this, Coach Beverly
A note on Autonomic Neuropathy. This condition causes nerve damage to the autonomic nervous system which is in charge of digestion, sexual function, heart rate, and the adrenergic flight or fight response. The autonomic nervous system also “oversees” the energy-conserving parasympathetic response including bladder control, heart rate slowing, eye pupil constriction, and more.
Answers & Rationale
Answer 1 is incorrect, 19.49% chose this answer, “Decreased sexual arousal, pins and needles sensations in lower extremities.” This is a juicy answer. Autonomic dysfunction can affect sexual function, but it doesn’t affect libido or sexual desire. In addition, the pins and needles sensation is due to the nerve damage associated with peripheral neuropathy. Since both parts of this answer aren’t correct, this answer is false.
Answer 2 is incorrect, 16.61% of you chose this answer, “Loss of protective sensation and urinary incontinence.” Loss of protective sensation is associated with peripheral neuropathy. However, urinary incontinence is often a result of autonomic neuropathy. Since both parts of this answer aren’t correct, this answer is false.
Answer 3 is correct, 39.62% of you chose this answer, GREAT JOB! “Resting tachycardia and esophageal dysmotility.” Elevated heart rate while resting is a concerning sign and is often associated with cardiac autonomic neuropathy and increased risk of a cardiac event. Autonomic neuropathy can affect the motility of the entire GI track, including the esophagus. The more commonly recognized GI autonomic neuropathy is gastroparesis. Since both conditions, resting tachycardia and esophageal dysmotility, are associated with autonomic neuropathy, this is the best answer.
Answer 4 is incorrect, 24.28% of you chose this juicy answer “Hypoglycemia unawareness and insensate feet.” Since hypoglycemia unawareness is associated with a diminished adrenergic response to low blood glucose levels, it is considered an autonomic neuropathy. However, insensate feet are due to peripheral nerve damage associated with ongoing hyperglycemia. Since both parts aren’t correct, this answer is false.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic?
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Eye Check Necessary?

For our August 10th Question of the Week, 37% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: AL is 24 with newly diagnosed type 1 diabetes. AL is very worried about going blind because an Aunt with Type 1 diabetes lost her vision due to living with type 1 diabetes.
Which of the following matches the ADA guidelines for diabetes eye care?
- An eye examination is recommended before pregnancy.
- Get eye exam immediately at type 1 diabetes diagnosis, then yearly thereafter.
- If no retinopathy found on initial exam, refer to trained retinal expert for thorough exam.
- Only trained ophthalmologist can screen for type 1 diabetes eye disease.
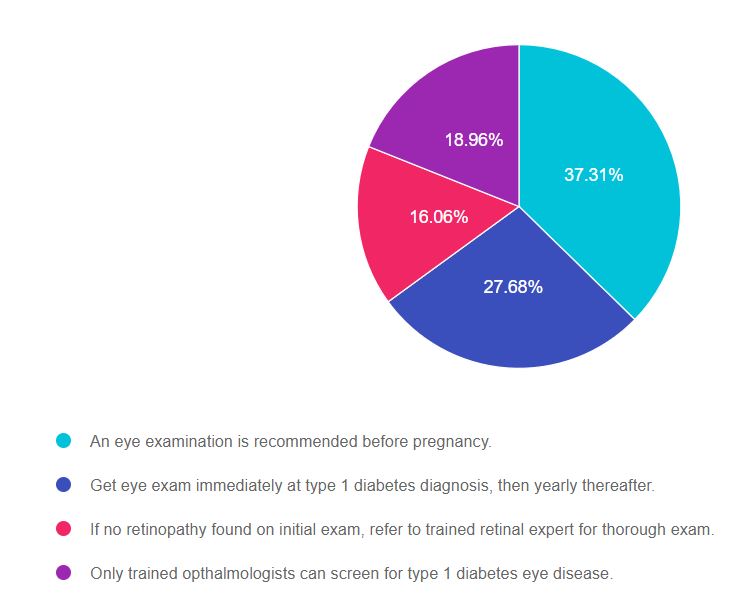
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 4, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for specialty topics like microvascular disease. Be familiar with screening guidelines for eye disease as listed in the ADA Standards of Care on Microvascular health and treatment options. We also invite you to join our webinar (see below). You got this, Coach Beverly
Answers & Rationale
Answer 1 is correct, 37.31% chose this answer, “An eye examination is recommended before pregnancy.” Great Job! Yes, this is the best answer. All people living with diabetes considering pregnancy need to get a baseline eye exam to evaluate retinal health. In addition, the ADA Standards recommend eye exams each trimester of pregnancy and after birth to monitor retinal changes.
Answer 2 is incorrect, 27.68% of you chose this answer, “Get eye exam immediately at type 1 diabetes diagnosis, then yearly thereafter.” This is the juicy answer. According to the ADA Standards for people with type 1 diabetes, they need an eye exam within in 5 years of diagnosis, then an eye exam every 1-2 years. The reason they don’t require an immediate eye exam is because type 1 diabetes is quickly identified and this short span of hyperglycemia does not increase risk of retinopathy. The reason we check people with type 2 eyes immediately, is because they could have had diabetes for an average of 6 years before diagnosis, allowing for the possibility of undetected eye damage.
Answer 3 is incorrect, 16.06% of you chose this answer, “If no retinopathy found on initial exam, refer to trained retinal expert for thorough exam.” ‘All people with diabetes do not need to be referred to a retinal expert. An ophthalmologist or optometrist can screen for type 1 diabetes eye disease. If retinopathy is discovered, depending on the severity, they may advise referral to a retinal specialist as needed.
Answer 4 is incorrect, 18.96% of you chose this answer “Only a trained ophthalmologists can screen for type 1 diabetes eye disease.” An ophthalmologist or optometrist can screen for type 1 diabetes eye disease. Programs that use retinal photography (with remote reading or use of a validated assessment tool) are also appropriate screening strategies for diabetes retinopathy. Such programs need to provide pathways for timely referral for a comprehensive eye examination when indicated.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic?
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
Enroll Now | 1.5 CEs | $29
Join us for our
Level 2 | Setting up a Successful DSME Program Standards | 1.5 CEs

This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking the CDCES Exam or considering setting up a DSME program, this program is designed for you. We review the 10 standards and provide strategies on implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- The steps involved in setting up a Diabetes Program
- List program essentials
- Discuss marketing strategies for success
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Protecting Kidney Function, Best Strategy?

For our August 3rd Question of the Week, 53% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: JR is 53 years old with type 2 diabetes for the past 7 years. JR’s BMI is 32, GFR is more than 60, blood pressure is 128/76, Urinary Albumin Creatinine Ratio (UACR) is 17mg/g.
According to the ADA Standards, which of the following is the most accurate recommendation to continue to protect JR’s kidney function?
Answer Choices:
- Initiate low dose ACE Inhibitor or ARB
- Focus on lifestyle changes
- Maintain protein intake to ~0.7 g/kg
- Reduce sodium intake to 1000 mg per day
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for these specialty topics like diabetes kidney disease. Be familiar with MNT guidelines and guidelines for best therapeutic intervention based on careful assessment of microvascular health. You got this, Coach Beverly
Answers & Rationale
Answer 1 is incorrect, 32% chose this answer, “Initiate low dose ACE Inhibitor or ARB.” This is a juicy answer, however, based on the ADA Standards on Microvascular Complications, medication is not required.
Here are 3 reasons why JR does not need an ACE or ARB:
- JRs GFR is more than 60, indicating acceptable kidney function.
- His B/P is below the most stringent target of 130/80.
- His UACR is normal, at less than 30.
Since all three of these indicators are below target range, blood pressure medication is not warranted and could even cause unwanted side effects like orthostatic hypotension. About a decade ago, there was a recommendation to start people with type 1 on an ACE or ARB to protect the kidney function, but it is NO longer recommended because it did not improve outcomes.
Answer 2 is correct, 53% of you chose this answer, “Focus on lifestyle changes.” YES, GREAT job. To help JR to keep his vessels healthy and improve his overall nutrition, we are going to encourage regular activity and an evidence based nutrition approach (DASH diet, Mediterranean, Plant Based eating etc.). We will make sure JR has an appointment with a diabetes care and education specialist and RD/RDN. No medications needed for JR, just ongoing self-care support and encouragement.
Answer 3 is incorrect, 9% of you chose this answer, “Maintain protein intake to ~0.7 g/kg.” In the old days, we used to recommend restricting protein intake to less than 0.8g/kg for people with diabetes kidney disease. We no longer make this recommendation since it didn’t improve outcomes! Plus, JR’s kidney function is fine and there is no diabetes kidney disease based on the information provided.
Answer 4 is incorrect, 6% of you chose this answer “Reduce sodium intake to 1000 mg per day.” For people with diabetes, the sodium recommendation is 2,300 mg per day, regardless of their blood pressure, since there is no evidence that a lower sodium intake reduces risk of complications.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
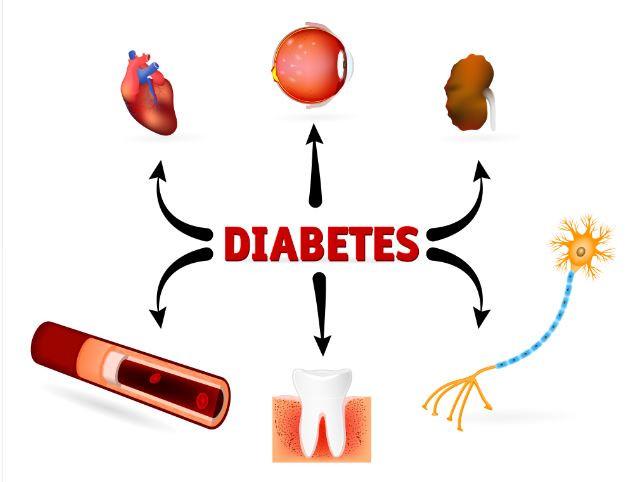
Rationale of the Week | Are diet sodas good for me?

For our July 27th Question of the Week, 72% of respondents chose the best answer. GREAT JOB! We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: JR has type 2 diabetes and is trying to lose weight by eating less and moving more. JR asks your advice about drinking diet sodas.
Based on the recommendations in the ADA Standards of Care, what is the best response?
Answer Choices:
- Sodas that contain non-nutritive sweeteners help with weight loss and increase sugar cravings.
- Try to decrease intake of beverages with non-nutritive sweeteners and increase water intake.
- Drinking beverages with non-nutritive sweeteners is better than drinking sugary beverages.
- Research has found that drinking beverages with nonnutritive sweeteners decreases diabetes risk.
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Since medical nutrition therapy (MNT) is an integral part of providing diabetes care, regardless of profession, it will be helpful to be familiar with the MNT guidelines in the ADA Standards of Care 5. Thanks much, Coach Beverly
Answers & Rationale
Answer 1 is incorrect, 4.29% chose this answer, “Sodas that contain non-nutritive sweeteners help with weight loss and increase sugar cravings.” According to the ADA “The addition of nonnutritive sweeteners to diets poses no benefit for weight loss or reduced weight gain without energy restriction.” The ADA Standards makes no comment on sugar cravings associated with non-nutritive sweeteners, so the first and second part of this answer are not based on evidence, which makes this answer false.
Answer 2 is correct, 72.39% of you chose this answer, “Try to decrease intake of beverages with non-nutritive sweeteners and increase water intake.” Yes, this is the best evidence based recommendation for fluid intake, health and diabetes management. I recommend flavored sparkly waters or adding a slice of cucumber, lemon or a fresh strawberry to your glass of H2O and calling it spa water.
Answer 3 is incorrect, 15.86% of you chose this juicy answer, “Drinking beverages with non-nutritive sweeteners is better than drinking sugary beverages.” According to the ADA Standards, “some people with diabetes who are accustomed to regularly consuming sugar-sweetened products, nonnutritive sweeteners (containing few or no calories) may be an acceptable substitute for nutritive sweeteners (those containing calories, such as sugar, honey, and agave syrup) when consumed in moderation.” Clearly, the ADA Standards do not say that beverages with non-nutritive sweeteners are better than sugary beverages, so this answer is juicy answer is false.
Answer 4 is incorrect, 7.46% of you chose this answer “Research has found that drinking beverages with nonnutritive sweeteners decreases diabetes risk.” According to the ADA, some research has found that higher nonnutritive-sweetened beverage and sugar-sweetened beverage consumption may be positively associated with the development of type 2 diabetes.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic?
Enroll in our Virtual DiabetesEd Specialist Program!
Medical Nutrition Therapy + Meal Planning + Exercise with Guest Speaker Ashley LaBrier | 4 CEs

These courses with Ashley LaBrier, MS, RD, CDCES who is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
These courses review the latest national nutrition guidelines and provide strategies to translate this information to an individual living with diabetes. Included is a discussion on different approaches to meal planning and the benefits and limitations of each, meal planning, and the importance of activity with nutrition.
Topics include:
- Medical Nutrition Therapy Updates and Critical Content
- Describe person-centered nutrition issues based on assessment and clinic data.
- Explore national guidelines for medical nutrition therapy and how to individualize interventions from a person-centered perspective.
- State how to customize nutritional approaches in people living with complications of diabetes.
- How to Eat by the Numbers and Meal Planning Approaches
- Describe the impact of micro and macronutrients on health.
- List different meal planning approaches and the pros and cons of each.
- Describe how to help people with diabetes to read labels and be thoughtful consumers.
- Keeping Well Through Activity and Nutrition
- Describe activity benefits, precautions, and recommendations
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
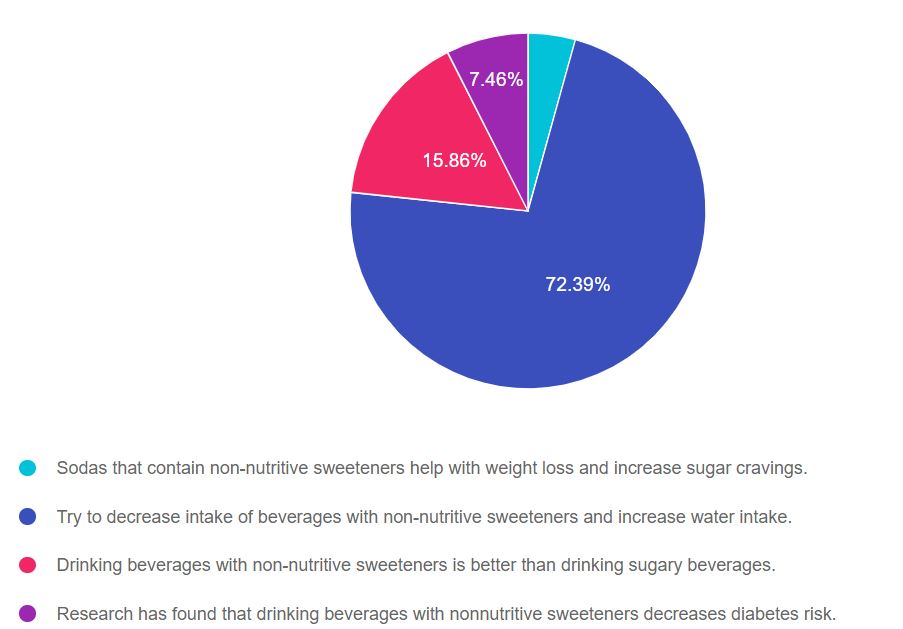
Rationale of the Week | Best meal planning approach with GDM

For our July 20th Question of the Week, 78% of respondents chose the best answer. GREAT JOB! We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: LS is 26 weeks pregnant and just discovered she has gestational diabetes. LS asks you what type of meal planning approach will help keep her and the baby healthy.
According to the ADA Standards of Care, what is the most accurate response?
Answer Choices:
- To promote healthy fetal development, consume about 175 gms of carb a day.
- Try to eliminate simple carbohydrates to decrease risk of reactive hypoglycemia.
- Consume the majority of carbs in the morning when you are most insulin resistant.
- Eat no more than one serving of fruit a day to prevent hepatic fructose toxicity.
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 3, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Being familiar with diabetes self-management guidelines and considerations during pregnancy is critical for exam success. If you don’t work with people with diabetes during pregnancy, I encourage you to be familiar with the ADA Standard on Diabetes and Pregnancy and to consider joining our online course for a 1.5 hour painless summary of this standard (see below). Lastly, don’t forget to leverage your common sense and vast health care knowledge to get to the best answer for these specialty topics. Coach Beverly
Answers & Rationale
Answer 1 is correct, 78.69% chose this answer, “To promote healthy fetal development, consume about 175 gms of carb a day.” GREAT JOB. According to the ADA Standard on Diabetes and Pregnancy, the food plan during pregnancy is individualized based on a nutrition assessment with guidance from the Dietary Reference Intakes (DRI). The DRI during pregnancy recommends a minimum of 175 g of carbohydrate, a minimum of 71 g of protein, and 28 g of fiber, with an emphasis on monounsaturated and polyunsaturated fats while limiting saturated fats and avoiding trans fats. All people with diabetes during pregnancy need to meet with a RD/RDN for specific guidance and recommendations.
Answer 2 is incorrect, 15.99% of you chose this answer, “Try to eliminate simple carbohydrates to decrease the risk of reactive hypoglycemia.” This is a juicy answer. It is true that eating less simple carbs, including processed foods and beverages, is a good idea before, during and after pregnancy. However, the second part of the answer makes this response incorrect for two reasons; the term “reactive hypoglycemia” is not a generally accepted diabetes term in this context and eliminating simple carbs would potentially increase the risk of hypoglycemia.
Answer 3 is incorrect, 3.02% of you chose this answer, “Consume the majority of carbs in the morning when you are most insulin resistant.” Part of this answer is correct. During pregnancy, many people are more insulin resistant in the morning. But, if a person is more insulin resistant in the morning, they would decrease the consumption of morning carbs to prevent post breakfast spikes.
Answer 4 is incorrect, 2.31% of you chose this answer “Eat no more than one serving of fruit a day to prevent hepatic fructose toxicity.” During pregnancy, incorporating a variety of fruits in the meal plan is a great idea, since they are packed with micronutrients, vitamins and fiber. They are carbohydrates and will increase blood sugars, so portion size and timing are important to consider when working them into the meal plan.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | Pregnancy & Diabetes Standards | 1.5 CE

People living with diabetes who are pregnant are confronted with a variety of issues that require special attention, education, and understanding.
This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Topics include:
- Three issues that affect pregnancy with diabetes
- The unique attributes of pre-existing diabetes in pregnancy and gestational diabetes
- Diagnostic criteria and management goals for gestational diabetes
- Potential short term and long term complications of fetal exposure to hypoglycemia
- Prevention measures to keep mother and baby healthy
See Full Calendar for upcoming webinars.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Why is JR missing insulin dose?

For our July 13th Question of the Week, 80% of respondents chose the best answer. GREAT JOB! We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: JR is 78, lives alone, and manages their diabetes with bolus insulin at breakfast and dinner and basal insulin at night. For the past few months, JR has had trouble remembering to take insulin with meals and JR’s most recent A1c is above 9%.
Which of the following is most likely contributing to this change of behavior for JR?
Answer Choices:
- Increased frequency of hypoglycemia.
- Nonalcoholic fatty liver disease.
- Alzheimer dementia.
- Adjustment of statin dose.
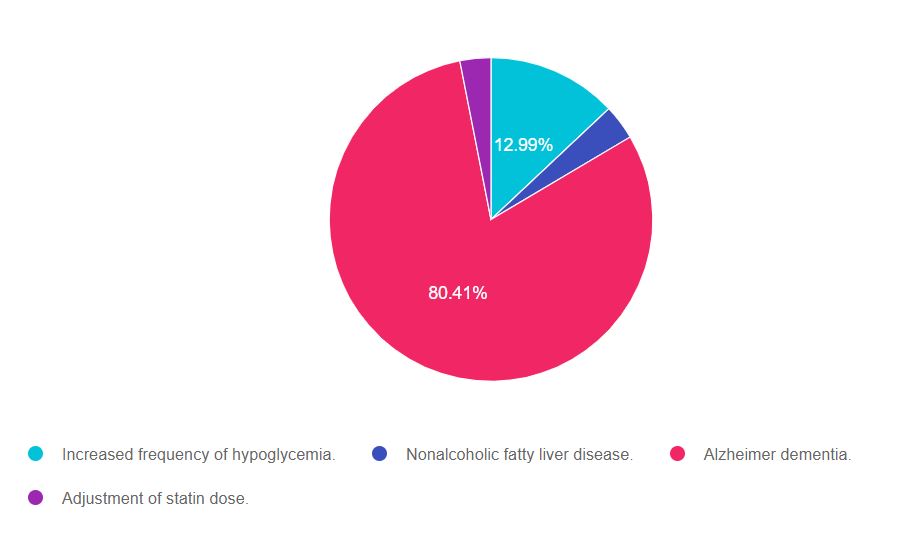
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 2, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Being familiar with the experiences and co-conditions that impact older people’s ability to self-manage diabetes will be helpful for the exams.
Answers & Rationale
Answer 1 is incorrect, 12.99% chose this answer, “Increased frequency of hypoglycemia.” This is the juicy answer, but not the best one. Since JRs A1c is elevated, we don’t suspect hypoglycemia is causing the missed bolus doses of insulin. However, it is important to assess for hypoglycemic events for older individuals taking insulin.
Answer 2 is incorrect, 3.51% of you chose this answer, “Nonalcoholic fatty liver disease.” It is true that more people with diabetes are experiencing fatty liver disease. However, we get no indication from the question that JR has visceral adiposity, jaundice skin color or elevated liver enzymes. And fatty liver disease in the early stages is not commonly associated with forgetfulness.
Answer 3 is correct, 80.41% of you chose this answer, “Alzheimer dementia.” GREAT JOB, this is the best answer. People with diabetes and hyperglycemia are at higher risk of Alzheimer and vascular dementia. Dementia can decrease the ability to remember to take insulin and other medications which can then lead to hyperglycemia which can worsen dementia. If you suspect that someone is forgetting to take insulin due to dementia, reaching out to the referring provider for a cognitive assessment and evaluation is warranted. See screening tools here.
Answer 4 is incorrect, 3.09% of you chose this answer “Adjustment of statin dose.” A few years back, there was a social media buzz that statin therapy is associated with decreased cognition and memory loss. According to the ADA Standards of Care, multiple well designed studies have found no association between statins and memory loss.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | Older Adults & Diabetes | 1.5 CEs

We have updated this content based on the ADA 2021 Standards of Care.
We are living longer and more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering reduction of medication and insulin therapy intensity. The older population has unique issues and special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Objectives:
- Self-management considerations for older individuals
- Strategies to prevent complications and maintain optimal quality of life
- The role of the Diabetes Educator as advocate
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What Diabetes Meds approved for Peds?

For our July 6th Question of the Week, 80% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
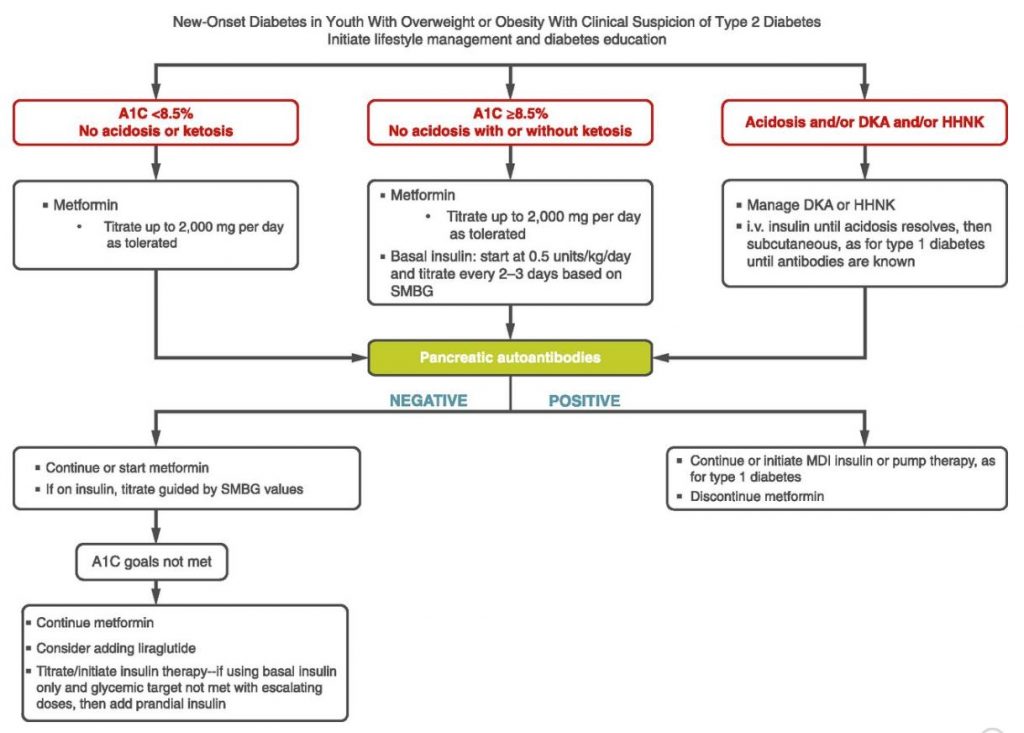
Question 1: JR is a 15-year-old with newly diagnosed type 2 diabetes, with an A1c of 8.3% and elevated lipids.
In addition to nutrition and activity coaching, which of the following medications are FDA approved for pediatrics?
Answer Choices:
- Glipizide and Sitagliptin
- SGLT-2 Inhibitors and GLP-1 Receptor Agonists
- Glimepiride and Empagliflozin
- Liraglutide and Metformin
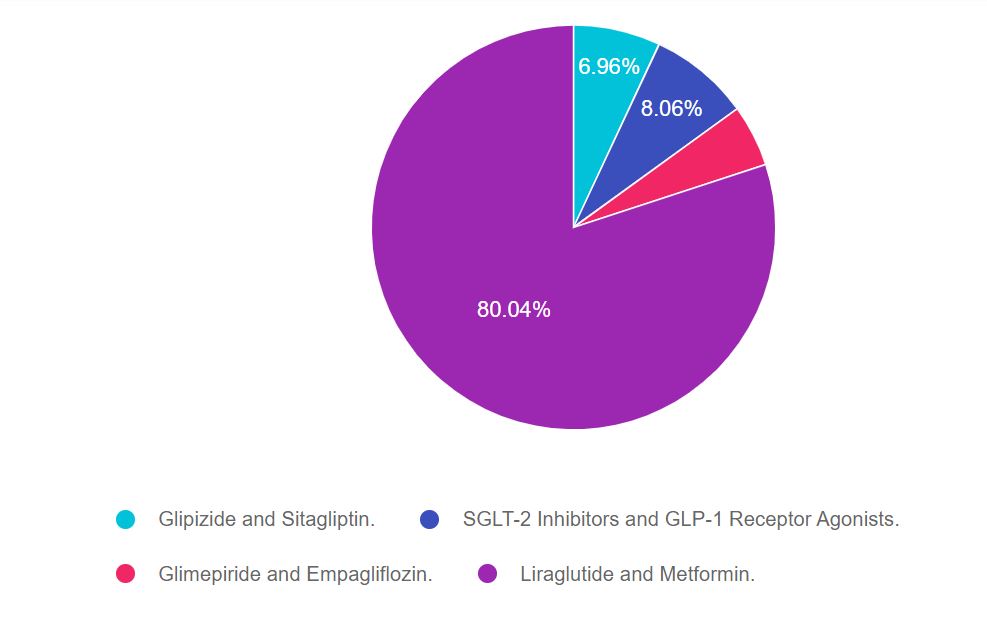
As shown above, the most common choice was option 4, the second most common answer was option 2, then option 1, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with knowledge of special populations like pediatrics, older folks and management of diabetes during pregnancy. According to the ADA Standards of Care, Section 13 of Children and Adolescents, here is the best answer.
Answers & Rationale
Answer 1 is incorrect, 6.96% chose this answer, “Glipizide and Sitagliptin.” Although commonly used in adults, sulfonylureas, including glipizide and DPP-IV’s including Sitagliptin, are not FDA approved for people under the age of 18.
Answer 2 is incorrect, 8.06% of you chose this answer, “SGLT-2 Inhibitors and GLP-1 Receptor Agonists.” Although commonly used in adults, SGLT-2s are not FDA approved for people under the age of 18. There is one GLP-1 Receptor Agonists, liraglutide (Victoza) approved for use in pediatrics over the age of 10. However, none of the other GLP-1 RAs are FDA approved for pediatrics.
Answer 3 is incorrect, 4.95% of you chose this answer, “Glimepiride and Empagliflozin.” Although commonly used in adults, sulfonylureas, including glimepiride and SGLT-2 Inhibitors, including empagliflozin, are not FDA approved for people under the age of 18.
Answer 4 is Correct, 80.04% of you chose this answer “Liraglutide and Metformin.” Great Job! For children under the age of 18, the only FDA approved pharmacologic interventions include metformin, liraglutide and insulin.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | From Tots to Teens Diabetes Standards | 1.5 CEs

This course includes updated goals and guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes and their families.
We discuss the clinical presentation of diabetes, goals of care, and normal growth and development through the early years through adolescence. Strategies to prevent acute and long term complications are included with an emphasis on positive coping for family and child with diabetes.
Topics include:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes
- State Strategies to prevent acute and chronic complications
- Discuss the importance of positive psychosocial adjustment and resources
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








