Rationale of the Week | How to Prep for Surgery

For our June 29th Question of the Week, 56% of respondents chose the best answer. Since people with diabetes will often need to undergo a procedure or surgery that requires they be NPO, we wanted to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: AR is living with type 2 diabetes, has an A1c of 7.4%, and takes metformin 1000 BID and 60 units of glargine at bedtime. AR is admitted to the hospital overnight for early morning surgery.
According to ADA Guidelines, what adjustment in his diabetes medications are needed to prepare for a safe surgery?
Answer Choices:
- Hold the evening metformin and glargine the night before surgery to prevent perioperative hypoglycemia.
- Hold morning metformin the day of surgery and give about 40 units of bedtime glargine the night before surgery.
- Hold metformin 3 days before surgery and give 60 units of bedtime glargine the night before surgery.
- Hold the metformin the day before surgery and give the glargine the morning of surgery to prevent perioperative hyperglycemia.
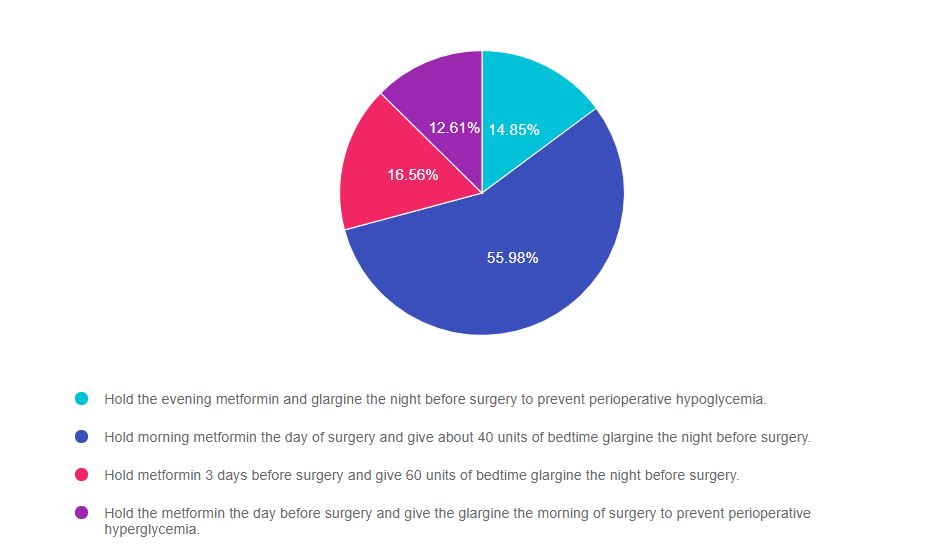
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 1, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with knowledge of preparation for surgery or other procedures that require the person with diabetes to be in a fasting state.
Answers & Rationale
Answer 1 is incorrect, 14.85% chose this answer, “Hold the evening metformin and glargine the night before surgery to prevent perioperative hypoglycemia.” Since AR has type 2 diabetes, even though AR is going to be NPO in preparation for surgery, AR can still take the evening metformin and most of the glargine. If AR holds both of these treatments, there is a high chance that AR will wake up with elevated morning blood sugars, which could delay surgery or lead to a hyperglycemic crisis.
Answer 2 is correct, 55.98% of you chose this answer, “Hold morning metformin the day of surgery and give about 40 units of bedtime glargine the night before surgery.” GREAT JOB. This is the BEST answer. According to the ADA, since AR has type 2 diabetes, even though AR is going to be NPO in preparation for surgery, AR can still take the evening metformin and 60-80% of the evening glargine. Since AR’s A1c is 7.4%, we give 60% of the usual 60 units of glargine (~40 units), so that AR wakes up with glucose close to the target, but not too low to cause hypoglycemia.
Answer 3 is incorrect, 16.56% of you chose this answer, “Hold metformin 3 days before surgery and give 60 units of bedtime glargine the night before surgery.” Since AR has type 2 diabetes, even though AR is going to be NPO in preparation for surgery, there is no reason for AR to hold the metformin for 3 days. AR can take metformin the day before surgery and resume metformin the evening after surgery if kidney function is stable. Since AR’s A1c is 7.4%, we give only 60% of the usual 60 units of glargine (~40 units), so that AR wakes up with glucose close to the target, but not too low to cause hypoglycemia.
Answer 4 is incorrect, 12.61% of you chose this answer “Hold the metformin the day before surgery and give the glargine the morning of surgery to prevent perioperative hyperglycemia.” Since AR has type 2 diabetes, even though AR is going to be NPO in preparation for surgery, there is no reason for AR to hold the metformin the day before surgery. AR can take metformin the day before surgery and resume metformin the evening after surgery if kidney function is stable. As far as changing glargine administration time to the morning to lower surgical glucose, this would not be advised since it would be a departure from AR’s usual routine and could cause unwanted glucose fluctuations.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | Hospitals & Hyperglycemia Standards | 1.5 CEs

Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control and outline practical strategies to achieve targets in the inpatient setting. We incorporate the latest ADA Standards and provide links to resources and inpatient management templates.
Topics include:
- The impact of hyperglycemia in the hospital setting.
- The importance of inpatient glucose control.
- Three strategies to get glucose to goal in the hospital setting.
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | How do Pregnancy Hormones affect Glucose?

For our June 22nd Question of the Week, 64% of respondents chose the best answer. Since many diabetes specialists aren’t exposed to the care of people with diabetes during pregnancy, we want to “take a closer look” at this question and determine strategies to choose the best response so test takers can be ready for these types of questions.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: ML has type 1 diabetes, her A1c is on target and she and is hoping to get pregnant in the upcoming year.
Which of the following statement best reflects the physiologic changes associated with pregnancy?
Answer Choices:
- A sharp increase in glucose levels in the first trimester due to placental hormones.
- A decrease in insulin needs during the second and third trimester.
- A minimal fluctuation in insulin needs until about 36 weeks.
- A decrease in insulin needs during the first 16 weeks.
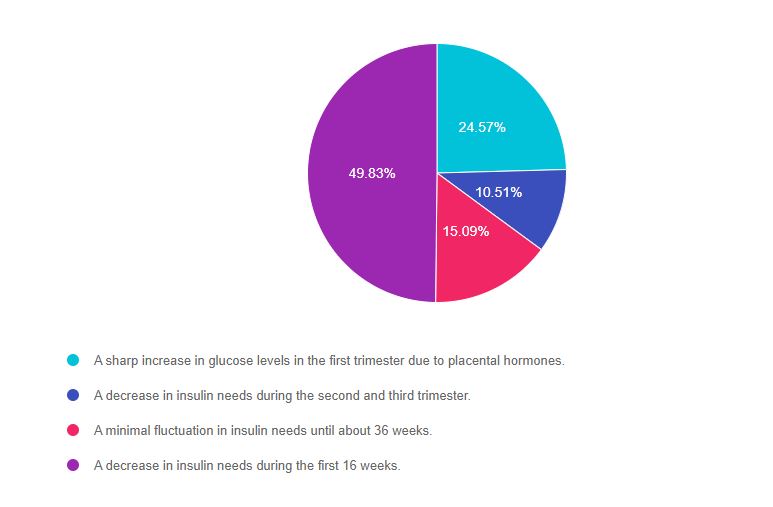
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 3, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with knowledge of diabetes during pregnancy,
Answers & Rationale
Answer 1 is incorrect, 24.57% chose this answer, “A sharp increase in glucose levels in the first trimester due to placental hormones.” This is not the best answer based on the pathophysiology of early pregnancy. According to ADA Standards of Care 14, “early pregnancy is a time of enhanced insulin sensitivity and lower glucose levels, many women with type 1 diabetes will have lower insulin requirements and increased risk for hypoglycemia.” Often, during the first trimester, insulin doses may need to be decreased to prevent hypoglycemia.
Answer 2 is incorrect, 10.51% of you chose this answer, “A decrease in insulin needs during the second and third trimester.” This is not the best answer based on the pathophysiology of mid and later pregnancy. According to ADA Standards of Care 14, “Around 16 weeks, insulin resistance begins to increase, and total daily insulin doses increase linearly ?5% per week through week 36. This usually results in a doubling of daily insulin dose compared with the prepregnancy requirement.”
Answer 3 is incorrect, 15.09% of you chose this answer, “A minimal fluctuation in insulin needs until about 36 weeks.” This is not the best answer based on the pathophysiology of pregnancy. Based on answers 1 and 2, blood sugars can plummet during early pregnancy and then glucose levels dramatically increase starting at 16 weeks, resulting in increasing insulin requirement of about 5% a week through week 36 of pregnancy.
Answer 4 is correct, 49.83% of you chose this answer “A decrease in insulin needs during the first 16 weeks.” GREAT JOB – Since there is increased glucose uptake by the fetus and placenta combined with enhanced insulin sensitivity in early pregnancy, blood sugars generally run lower and are associated with lower insulin requirements during the first 16 weeks.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | Pregnancy & Diabetes Standards | 1.5 CEs

People living with diabetes who are pregnant are confronted with a variety of issues that require special attention, education, and understanding.
This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Topics include:
- Three issues that affect pregnancy with diabetes
- The unique attributes of pre-existing diabetes in pregnancy and gestational diabetes
- Diagnostic criteria and management goals for gestational diabetes
- Potential short term and long term complications of fetal exposure to hypoglycemia
- Prevention measures to keep mother and baby healthy
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | JR worried about cancer; sorting fact from fiction

For our June 8th Question of the Week, only 64% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is taking Metformin 1000mg BID but is worried about getting cancer and is thinking about stopping the metformin.
Which of the following is an accurate statement regarding diabetes and cancer?
Answer Choices:
- People with diabetes have a slightly lower risk of liver and uterine cancers.
- Some brands of metformin were recalled because of an NDMA impurity, so it is best to hold metformin for now.
- There is research suggesting that metformin may be associated with a decreased risk of certain cancers.
- Metformin does not increase the risk of cancer, but it can negatively impact renal function.
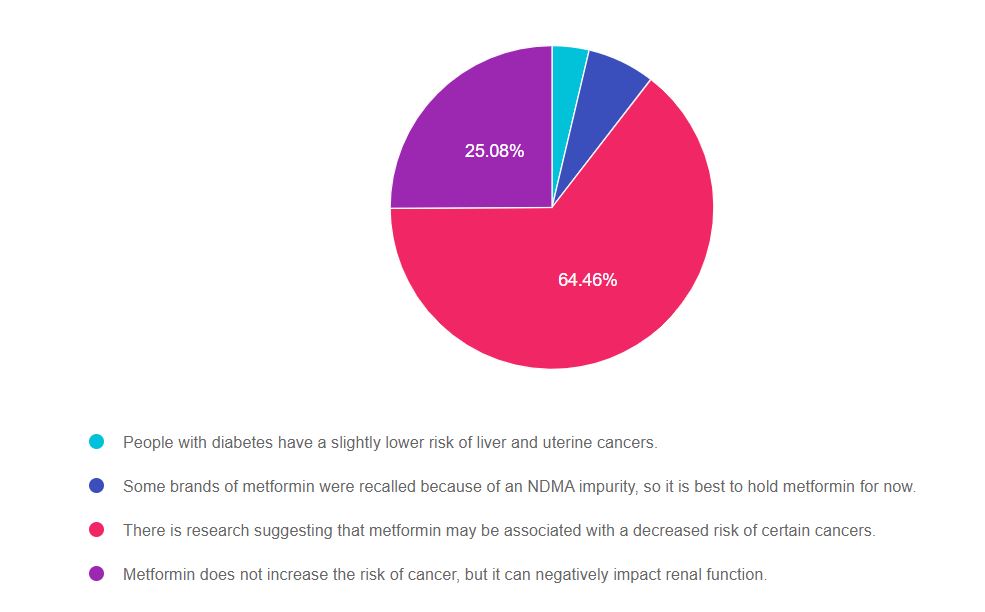
As shown above, the most common choice was option 3, the second most common answer was option 4, then option 2, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with knowledge of diabetes co-conditions plus prevention and screening guidelines.
Answers & Rationale
Answer 1 is incorrect, 3.69% chose this answer, “People with diabetes have a slightly lower risk of liver and uterine cancers.” People with type 2 diabetes have a higher risk of getting liver and endometrial cancers. There is an increased risk of diabetes and cancer in the same person due to an overlap of risk factors (age and weight) plus lifestyle factors (smoking, activity level, income and environmental factors).
Answer 2 is incorrect, 6.77% of you chose this answer, “Some brands of metformin were recalled because of an NDMA impurity, so it is best to hold metformin for now.” In 2020, some brands of Metformin were recalled because of above acceptable levels of NDMA due to the manufacturing process. The FDA recalled those brands and they were pulled from pharmacy shelves. Any dispensed metformin post recall should be safe.
Answer 3 is Correct, 64.46% of you chose this answer, “There is research suggesting that metformin may be associated with a decreased risk of certain cancers.” YES, you chose the BEST answer. Congratulations. Multiple studies have examined metformin for its potential tumor and cancer fighting ability and it looks very promising. Read more here >>
Answer 4 is incorrect, 25.08% of you chose this answer, “Metformin does not increase the risk of cancer, but it can negatively impact renal function.” This answer is NOT correct. Metformin appears to reduce the risk of some cancers but does NOT harm kidney function. There has been a increase of misinformation about metformin over the past year. Metformin is not recommended for anyone with a GFR less than 30 due to increase risk of lactic acidosis. But, metformin WON’T harm the kidneys and one could even argue that it protects them by lowering A1C by 1-2% points. You can download our Medication PocketCards for more information.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Level 4 | Cancer & Diabetes | 1.25 CEs

Patients with cancer often experience hyperglycemia secondary to treatment, which can increase risk of infection and compromise their nutritional status. In addition, recent research has identified the link between diabetes and cancer. Join us to learn more about this unexpected link and treatment strategies for steroid induced hyperglycemia using a case study approach.
Topics Include:
- Discuss the relationship between cancer, hyperglycemia and insulin resistance.
- State 3 benefits of normalizing glucose levels during chemotherapy.
- Using a case study approach, discuss strategies to improve glucose levels and quality of life.
2021 Live Webinar Events
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week – Less than 50% chose best answer | New Type 2, Action Needed?

For our June 1st Question of the Week, only 45% of respondents chose the best answer. We want to “take a closer look” at this question and figure out how to drill down to discover the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is 43 years old with newly discovered type 2 diabetes.
According to the ADA Standards, which of the following actions need to be taken with a new type 2 diabetes diagnosis?
Answer Choices:
- Hepatitis B Vaccine.
- Screening for prostate cancer.
- Referral to podiatry.
- Antibody testing to confirm the diagnosis.
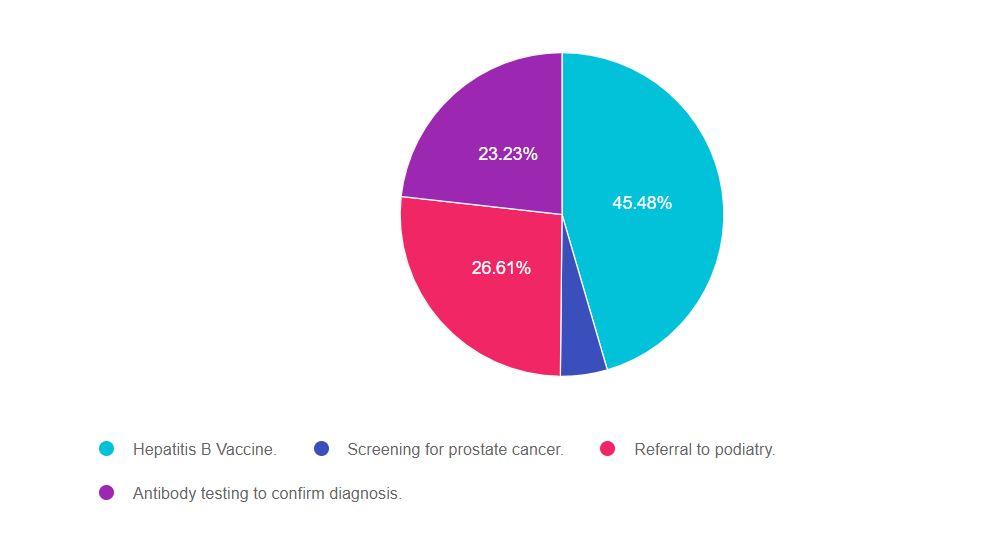
As shown above, the most common choice was option 1, the second most common answer was option 3, then option 4, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with preventive care measures, especially suggested vaccinations based on age and risk profile.
Answers & Rationale
Answer 1 is correct, 45.48% chose this answer, “Hepatitis B Vaccine.” CONGRATS, this is the BEST answer. According to the ADA Standards of Care (see below), people with diabetes who are 18-59 years of age need protection against hepatitis infection. Since people with diabetes may share glucose checking devices and may have less hearty immune systems, they are at higher risk of getting Hepatitis B. Getting the 2-3 dose series if not previously vaccinated, offers important protection.
Answer 2 is incorrect, 4.68% of you chose this answer, “Screening for prostate cancer.” According to the ADA Standards, a new diagnosis of type 2 diabetes does not require screening for prostate cancer. In addition, according to the consensus statement on Diabetes and Cancer, men with diabetes are not at higher risk of prostate cancer. However, people with diabetes are at higher risk of pancreas, liver and breast cancer, so regular screenings for these types of cancers is indicated.
Answer 3 is incorrect, 26.61% of you chose this answer, “Referral to podiatry.” This is answer is juicy, but we don’t have enough details in the question to support referral to a podiatrist. Not everyone with new diabetes is referred to podiatry for lower extremity care. Podiatry referral is based on a careful lower extremity assessment coupled with an indication that this person is at higher risk of complications (ie ulcerations, severe calluses, risk of injury when cutting toenails, loss of protective sensation, etc).
Answer 4 is incorrect, 23.23% of you chose this answer, “Antibody testing to confirm the diagnosis.” Another juicy answer. For most people with new type 2 diabetes, the clinical presentation coupled with family history and ketone status is usually enough to determine the type of diabetes. If the question hinted that this person might have type 1 (ie history of celiac or thyroid disease, positive ketones, BMI of 21 etc) then, the provider may want to evaluate for the presence of antibodies.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What are Pediatric Glucose Targets?

For our June 15th Question of the Week, only 54% of respondents chose the best answer. We want to “take a closer look” at this question with the aim for 100% correct responses the next to go around.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: RT is 12 years old and has a new diagnosis of type 1 diabetes.
Based on the ADA Standards of Care, what is the most accurate statement regarding glycemic goals?
Answer Choices:
- Glucose targets are based on the individual.
- Strive to achieve at least 80% time in range.
- A1C less than 6.5% for children under the age of 18.
- Pre-meal glucose of 80-130 and post-meal glucose less than 200 to prevent hypoglycemia.
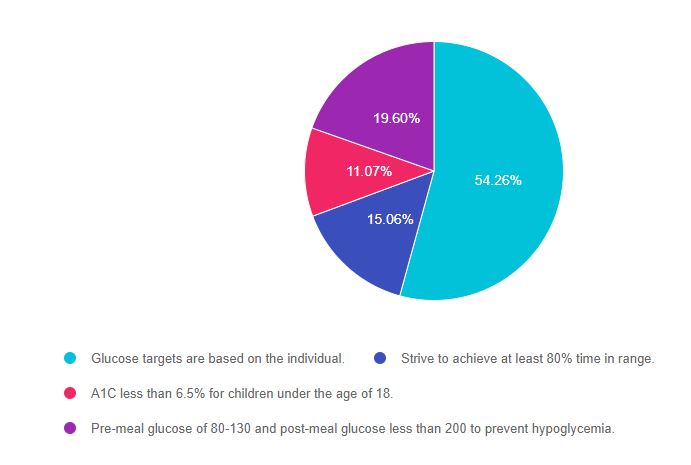
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with the goals of care for specialty populations, including pediatrics.
Answers & Rationale
Answer 1 is Correct, 54.26% chose this answer, “Glucose targets are based on the individual.” GREAT JOB. This is the best answer. The American Diabetes Association provides a general A1c target of 7% or less for pediatrics, but it encourages the person with diabetes and the care provider to determine glucose ranges that best match the individual based on their values, preferences, access to technology and safety.
Answer 2 is incorrect, 15.06% of you chose this answer, “Strive to achieve at least 80% time in range.” According the the ADA, the time in range target is 60% or an A1c of less than 7.5% for those under the age of 25. Of course, these goals are customized to match the individual.
Answer 3 is incorrect, 11.07% of you chose this answer, “A1C less than 6.5% for children under the age of 18..” This is a juicy answer. This target may be right for those who are using a CGM, pump and advanced technology features that help users avoid hypoglycemic events. But this is not the A1C target for all children with type 1 diabetes, so this is not the best answer. There is no A1C target that fits all.
Answer 4 is incorrect, 19.60% of you chose this answer, “Pre-meal glucose of 80-130 and post-meal glucose less than 200 to prevent hypoglycemia.” The American Diabetes Association provides a general A1c target of 7% or less for pediatrics, but it encourages the person with diabetes and the care provider to determine pre and post meal glucose ranges that best match the individual based on their values, preferences, access to technology and safety.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Level 2 | From Tots to Teens Diabetes Standards | 1.5 CEs

This course includes updated goals and guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes and their families.
We discuss the clinical presentation of diabetes, goals of care, and normal growth and development through the early years through adolescence. Strategies to prevent acute and long term complications are included with an emphasis on positive coping for family and child with diabetes.
Topics include:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes
- State Strategies to prevent acute and chronic complications
- Discuss the importance of positive psychosocial adjustment and resources
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | U-500 Insulin Still Causing Confusion

For our May 25th Question of the Week, 71% of respondents chose the best answer, which is awesome! However, for safety and teaching purposes, we still want to “take a closer look” at this question at aim for 100% correct responses the next go around.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Mr. J is started on 100 units U-500 twice a day.
Which of the following administration techniques would ensure he gets the right dose?
Answer Choices:
- Using a U-100 syringe, withdraw 100 units.
- Using a U-500 syringe, withdraw 20 units.
- Using a U-500 pen, dial to 100 units.
- Using a U-500 pen, covert to 20 units.
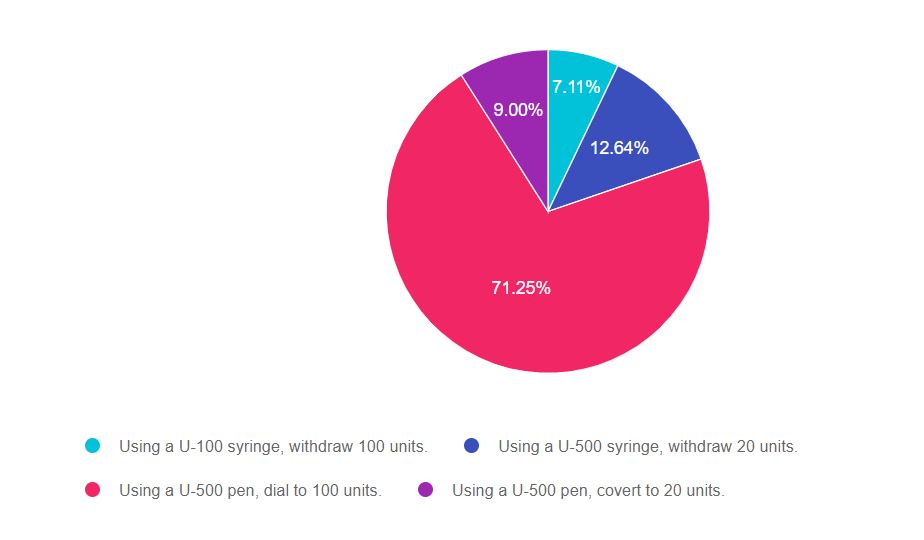
As shown above, the most common choice was option 3, the second most common answer was option 2, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with accurate dispensing of diabetes medications, injectables and insulins, including the concentrated versions.
Answers & Rationale
Answer 1 is incorrect, 7.11% chose this answer, “Using a U-100 syringe, withdraw 100 units.” This answer is wrong because when withdrawing U-500 insulin from a vial, a U-500 insulin syringe must be used (see image). Since U-500 insulin is 5x’s the concentration of U-100 insulin, drawing up 100 units of U-500 insulin in a U-100 syringe would deliver 500 units of insulin (or 5x’s too much and could be life threatening). See Concentrated insulin card below.
When using a U-500 syringe, no conversion is needed since the syringe automatically delivers the correct dose of U-500 insulin. No conversion, calculations or adjustments required.
Answer 2 is incorrect, 12.64% of you chose this answer, “Using a U-500 syringe, withdraw 20 units.” When using a U-500 syringe, no conversion is needed since the syringe automatically delivers the correct dose of U-500 insulin. No conversion, calculations or adjustments required. For example, if the order reads “100 units of U-500 concentrated insulin twice a day”, using a U-500 syringe, the person would withdraw 100 units of U-500 insulin.
Answer 3 is correct, 71.25% of you chose this answer, “Using a U-500 pen, dial to 100 units.” YES, GREAT JOB! If the order reads “100 units of U-500 concentrated insulin twice a day”, using a U-500 pen, the person would dial to 100 units of U-500 insulin. The pens automatically deliver the correct dose in less volume. No conversion, calculations or adjustments required.
Answer 4 is incorrect, 9.00% of you chose this answer, “Using a U-500 pen, covert to 20 units.” When using a U-500 pen, no conversion is needed since the U-500 pen is specifically created to deliver the correct dose of U-500 insulin. For example, if the order reads “100 units of U-500 concentrated insulin twice a day”, using a U-500 pen, the person would dial to 100 units of U-500 insulin.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more? Enroll in our
Brand New Online Advanced Courses | Level 4!
We are so excited to expand our Level 4 – Advanced Level & Specialty Topics Series!

Our Level 4 specialty courses are designed to address topics that not only enhance the clinical practice but also prepare participants to take the Board Certification in Advanced Diabetes Management (BC-ADM) exam. The fast-paced content is designed to fulfill curiosity, build on previous significant diabetes care experience and support your journey toward expanding your diabetes knowledge.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best next step?

For our May 18th Question of the Week, 76% of respondents chose the best answer, which is awesome! We still want to “take a closer look” at this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: CT was diagnosed with type 2 diabetes three years ago. The current medication regimen includes 1000 mg of metformin twice daily and 70 units of glargine at night. CT wears an intermittent sensor, and you look at the glucose trends together on CT’s phone app. You both agree that there are consistent postmeal spikes up to 250 almost every day after lunch and dinner. The lowest blood sugar readings are in the 100s. BMI is 33.8 and CT says, “I never feel full”. The most recent A1C is 8.2%, urinary albumin creatinine ratio less than 30.
Based on this information, what intervention would be most likely help CT get to recommended ADA targets?
Answer Choices:
- Add on low-dose sulfonylurea to prevent hypoglycemia.
- Suggest adding a GLP-1 Receptor Agonist.
- Hold metformin, and switch to basal-bolus therapy.
- Encourage CT to get more active, especially after meals.
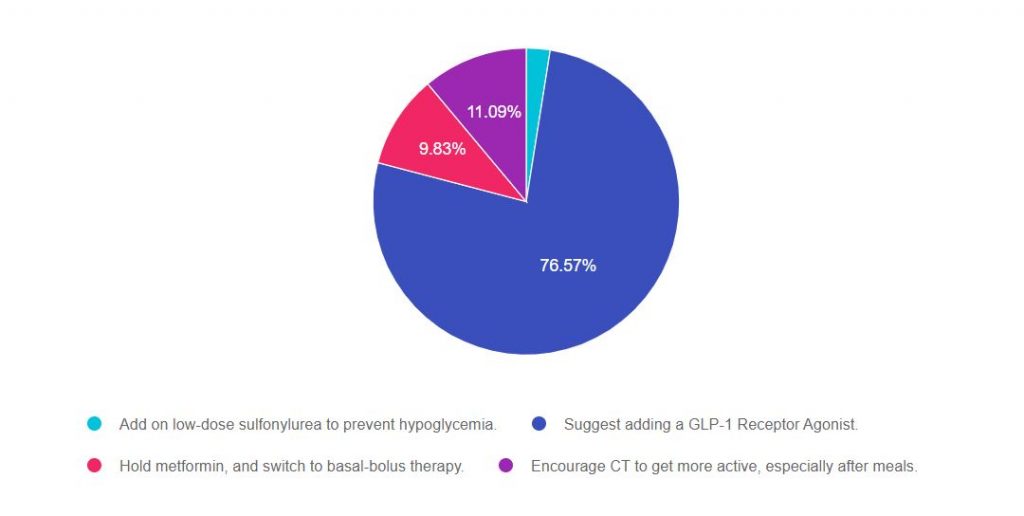
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with the stepwise approach to type 2 diabetes management in a variety of settings and situations.
For a complete listing of diabetes medications, please Download our Medication PocketCards.
Answers & Rationale
Answer 1 is incorrect, 2.51% chose this answer, “Add on low-dose sulfonylurea to prevent hypoglycemia.” Although we might consider this option, we can quickly identify a “tacked on” second half of the answer that makes it a wrong choice. One of the major side effects of sulfonylureas is hypoglycemia, so adding this class of medication wouldn’t prevent hypoglycemia, it would actually increase the risk of low blood sugars.
Answer 2 is correct, 76.57% of you chose this answer, “Suggest adding a GLP-1 Receptor Agonist.” GREAT JOB! Given the fact that CT is on 70 units of basal plus metformin and is experiencing postmeal spikes up to 250 almost every day after lunch and dinner and “never feels full”, adding a GLP-1 is the best choice. Adding a GLP-1 will decrease post meal hyperglycemia and postprandial glucose. In addition, GLP-1s can decrease appetite and increase feelings of satiation. Before suggesting addition of this medication class, it is important to consider insurance coverage and out of pocket cost, since cost could be a barrier.
Answer 3 is incorrect, 9.83% of you chose this answer, “Hold metformin, and switch to basal-bolus therapy.” According to the ADA, when initiating basal bolus insulin therapy for people with type 2 diabetes, they recommend continuing metformin to decrease insulin resistance. The ADA also suggests considering adding a GLP-1 RA or SGLT-2 Inhibitor before switching to basal bolus therapy.
Answer 4 is incorrect, 11.09% of you chose this answer, “Encourage CT to get more active, especially after meals.” While activity is important, this goal is very vague and not really actionable. In addition, “getting active after meals” will certainly improve health and is a great recommendation, but is not likely to drop the A1c to less than the goal of 7% or help with appetite.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Join us for our upcoming
Level 4 | Solving Glucose Mysteries for Type 2 | 1.5 CEs | Ready to Watch!

Why are glucose levels elevated in the morning? When should insulin be started? What is the next step to get A1c to target?
During this course Coach Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 2 diabetes.
By attending this webinar, you will gain confidence in evaluating glucose patterns and making recommendations for improvement.
Objectives
- Describe common glucose mysteries encountered by people with type 2 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Join us for our Live Webinars
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1 Needs Surgery

For our May 4th Question of the Week, 48% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: MS is 63, has type 1 diabetes, and will be having knee surgery. In addition to using an insulin pump and CGM to manage their type 1 diabetes, MS also takes empagliflozin (Jardiance) 25 mg daily to improve glucose levels.
In preparation for the upcoming surgery, which of the following is an accurate statement?
Answer Choices:
- Transition to insulin injections in preparation for surgery.
- Maintain perioperative glucose between 80-110.
- Stop empagliflozin (Jardiance) 3 days prior to surgery.
- Reduce basal insulin by half the night before surgery.
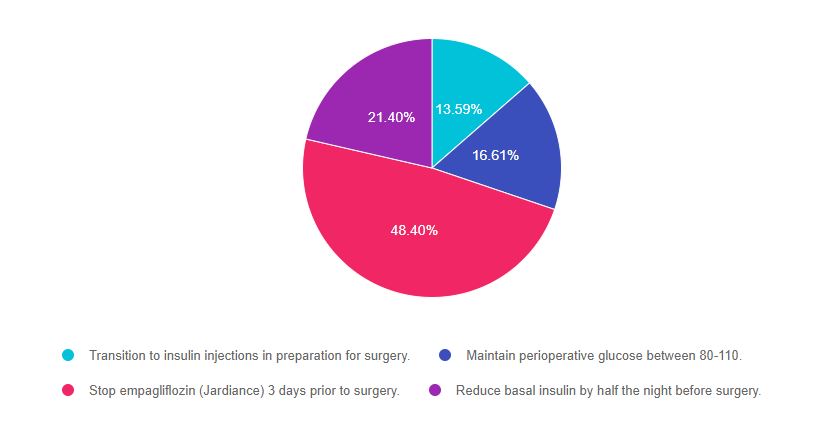
As shown above, the most common choice was option 3, the second most common answer was option 4, then option 2, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with type 1 and type 2 diabetes management in a variety of settings and situations.
Answers & Rationale
Answer 1 is incorrect, 13.59% chose this answer, “Transition to insulin injections in preparation for surgery.” Having glucose levels on target can help to improve surgical outcomes. For MS, staying on the insulin pump pre and post post-operatively will ensure best glucose management and allow MS to participate in care.
Answer 2 is incorrect, 16.61% of you chose this answer, “Maintain perioperative glucose between 80-110.” According to the ADA Standards, the perioperative glucose target is 80- 180. The goal of 80-110 is too narrow of a range and increases risk of intraoperative hypoglycemia.
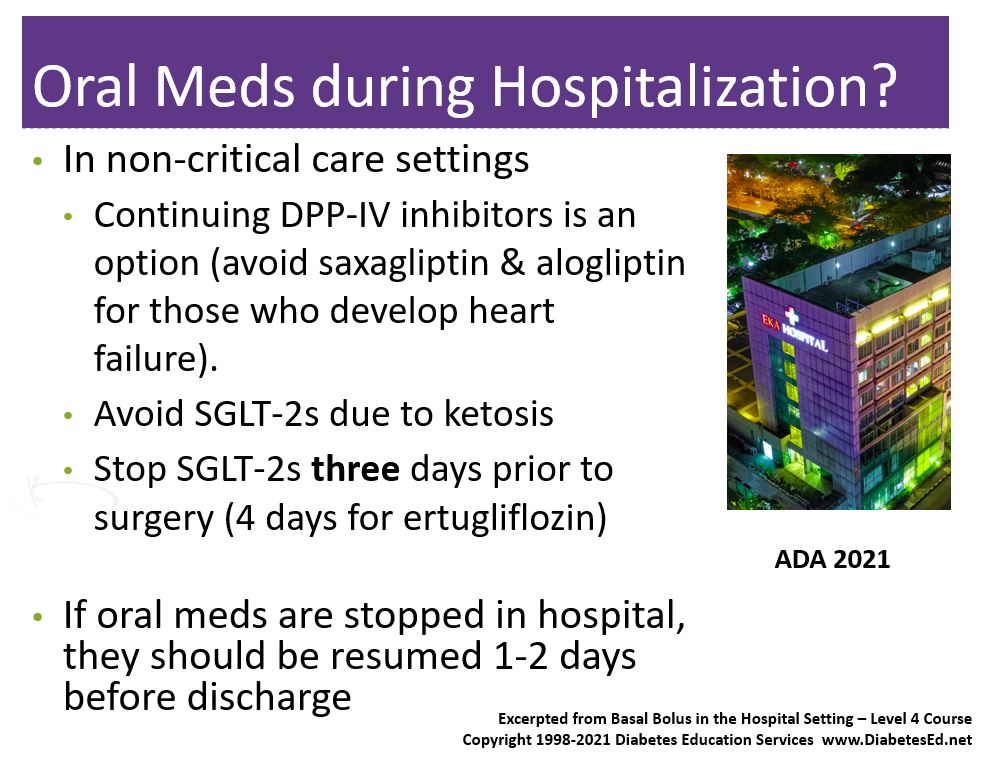
Answer 3 is correct, 48.40% of you chose this answer, “Stop empagliflozin (Jardiance) 3 days prior to surgery.” The new ADA 2021 Standards recommend stopping all SGLT-2s three days prior to surgery and ertugliflozin four days prior to surgery. In addition, SGLT-2s should be stopped with hospital admission. The reason behind this recommendation is to prevent DKA or ketoacidosis during hospitalization. (See slide below from our Basal Bolus in the Hospital Setting Level 4 Class).
Download Free Med PocketCards
Answer 4 is incorrect, 21.40% of you chose this answer, “Reduce basal insulin by half the night before surgery.” For someone with type 1 diabetes, if the basal rate is set correctly there is no basal dose reduction needed, even if someone is NPO. Reducing basal by 50% could actually put them at risk for hyperglycemia pre-operatively. If MS is at risk of hypoglycemia, we might consider making a 5-10% basal rate reduction, but not 50%.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
See ADA Standard 15 – Diabetes Care in the Hospital Setting
Want to learn more about this question and more?
Enroll on our
Basal/Bolus Therapy in Hospital Webinar 1.5 CEs
Recorded and Ready for viewing

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely and effectively implement Basal Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the individual’s clinical presentation and apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings and a discussion of solutions that will keep people safe and get glucose levels to goal. In addition, sample basal/bolus and insulin drip guidelines plus lots of resource articles are included.
Topics Include:
- Discussing appropriate insulin dosing based on the individual’s clinical presentation
- Applying dosing strategies to a variety of case studies
- Introduce hard-to-manage situations that commonly occur in hospital settings
- A discussion of solutions that will keep individuals safe and get glucose levels to goal
- Sample basal/bolus and insulin drip guidelines plus lots of resource articles are included
Join us for our Live Webinars
Including Brand New Specialty Courses!
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








