Rationale of the Week | Best next step?

For our May 18th Question of the Week, 76% of respondents chose the best answer, which is awesome! We still want to “take a closer look” at this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: CT was diagnosed with type 2 diabetes three years ago. The current medication regimen includes 1000 mg of metformin twice daily and 70 units of glargine at night. CT wears an intermittent sensor, and you look at the glucose trends together on CT’s phone app. You both agree that there are consistent postmeal spikes up to 250 almost every day after lunch and dinner. The lowest blood sugar readings are in the 100s. BMI is 33.8 and CT says, “I never feel full”. The most recent A1C is 8.2%, urinary albumin creatinine ratio less than 30.
Based on this information, what intervention would be most likely help CT get to recommended ADA targets?
Answer Choices:
- Add on low-dose sulfonylurea to prevent hypoglycemia.
- Suggest adding a GLP-1 Receptor Agonist.
- Hold metformin, and switch to basal-bolus therapy.
- Encourage CT to get more active, especially after meals.
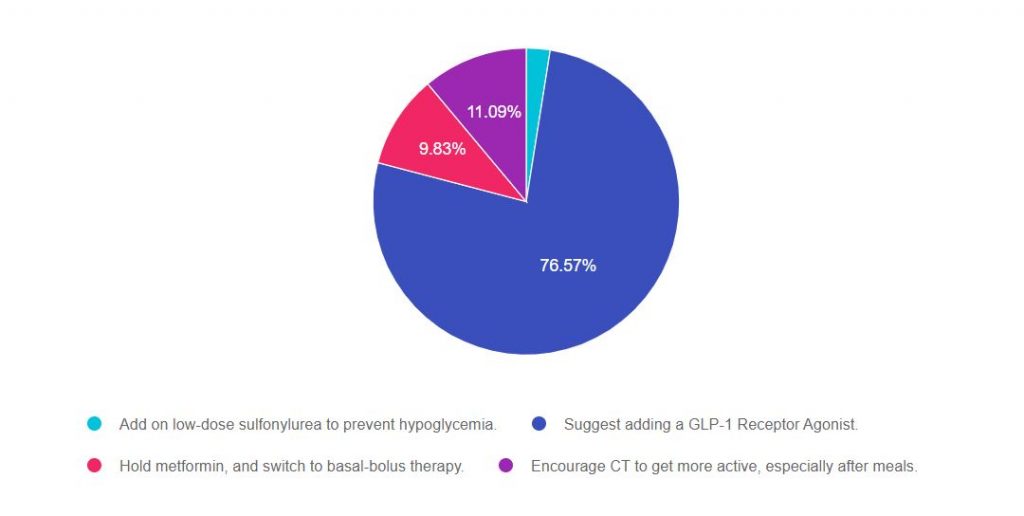
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with the stepwise approach to type 2 diabetes management in a variety of settings and situations.
For a complete listing of diabetes medications, please Download our Medication PocketCards.
Answers & Rationale
Answer 1 is incorrect, 2.51% chose this answer, “Add on low-dose sulfonylurea to prevent hypoglycemia.” Although we might consider this option, we can quickly identify a “tacked on” second half of the answer that makes it a wrong choice. One of the major side effects of sulfonylureas is hypoglycemia, so adding this class of medication wouldn’t prevent hypoglycemia, it would actually increase the risk of low blood sugars.
Answer 2 is correct, 76.57% of you chose this answer, “Suggest adding a GLP-1 Receptor Agonist.” GREAT JOB! Given the fact that CT is on 70 units of basal plus metformin and is experiencing postmeal spikes up to 250 almost every day after lunch and dinner and “never feels full”, adding a GLP-1 is the best choice. Adding a GLP-1 will decrease post meal hyperglycemia and postprandial glucose. In addition, GLP-1s can decrease appetite and increase feelings of satiation. Before suggesting addition of this medication class, it is important to consider insurance coverage and out of pocket cost, since cost could be a barrier.
Answer 3 is incorrect, 9.83% of you chose this answer, “Hold metformin, and switch to basal-bolus therapy.” According to the ADA, when initiating basal bolus insulin therapy for people with type 2 diabetes, they recommend continuing metformin to decrease insulin resistance. The ADA also suggests considering adding a GLP-1 RA or SGLT-2 Inhibitor before switching to basal bolus therapy.
Answer 4 is incorrect, 11.09% of you chose this answer, “Encourage CT to get more active, especially after meals.” While activity is important, this goal is very vague and not really actionable. In addition, “getting active after meals” will certainly improve health and is a great recommendation, but is not likely to drop the A1c to less than the goal of 7% or help with appetite.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Join us for our upcoming
Level 4 | Solving Glucose Mysteries for Type 2 | 1.5 CEs | Ready to Watch!

Why are glucose levels elevated in the morning? When should insulin be started? What is the next step to get A1c to target?
During this course Coach Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 2 diabetes.
By attending this webinar, you will gain confidence in evaluating glucose patterns and making recommendations for improvement.
Objectives
- Describe common glucose mysteries encountered by people with type 2 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Join us for our Live Webinars
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1 Needs Surgery

For our May 4th Question of the Week, 48% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: MS is 63, has type 1 diabetes, and will be having knee surgery. In addition to using an insulin pump and CGM to manage their type 1 diabetes, MS also takes empagliflozin (Jardiance) 25 mg daily to improve glucose levels.
In preparation for the upcoming surgery, which of the following is an accurate statement?
Answer Choices:
- Transition to insulin injections in preparation for surgery.
- Maintain perioperative glucose between 80-110.
- Stop empagliflozin (Jardiance) 3 days prior to surgery.
- Reduce basal insulin by half the night before surgery.
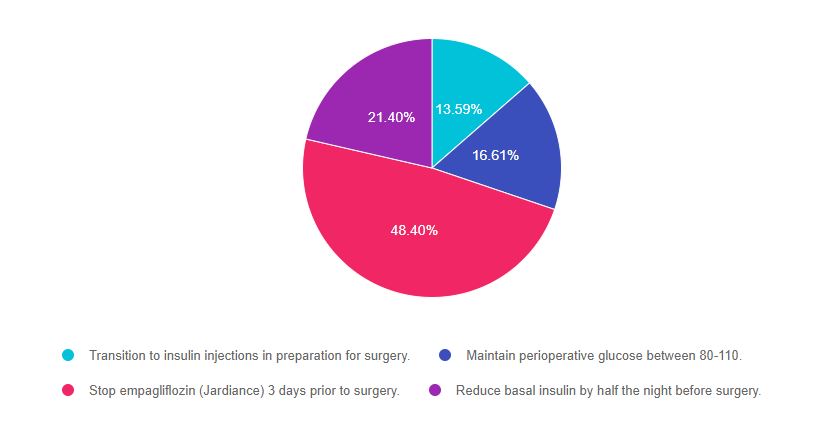
As shown above, the most common choice was option 3, the second most common answer was option 4, then option 2, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with type 1 and type 2 diabetes management in a variety of settings and situations.
Answers & Rationale
Answer 1 is incorrect, 13.59% chose this answer, “Transition to insulin injections in preparation for surgery.” Having glucose levels on target can help to improve surgical outcomes. For MS, staying on the insulin pump pre and post post-operatively will ensure best glucose management and allow MS to participate in care.
Answer 2 is incorrect, 16.61% of you chose this answer, “Maintain perioperative glucose between 80-110.” According to the ADA Standards, the perioperative glucose target is 80- 180. The goal of 80-110 is too narrow of a range and increases risk of intraoperative hypoglycemia.
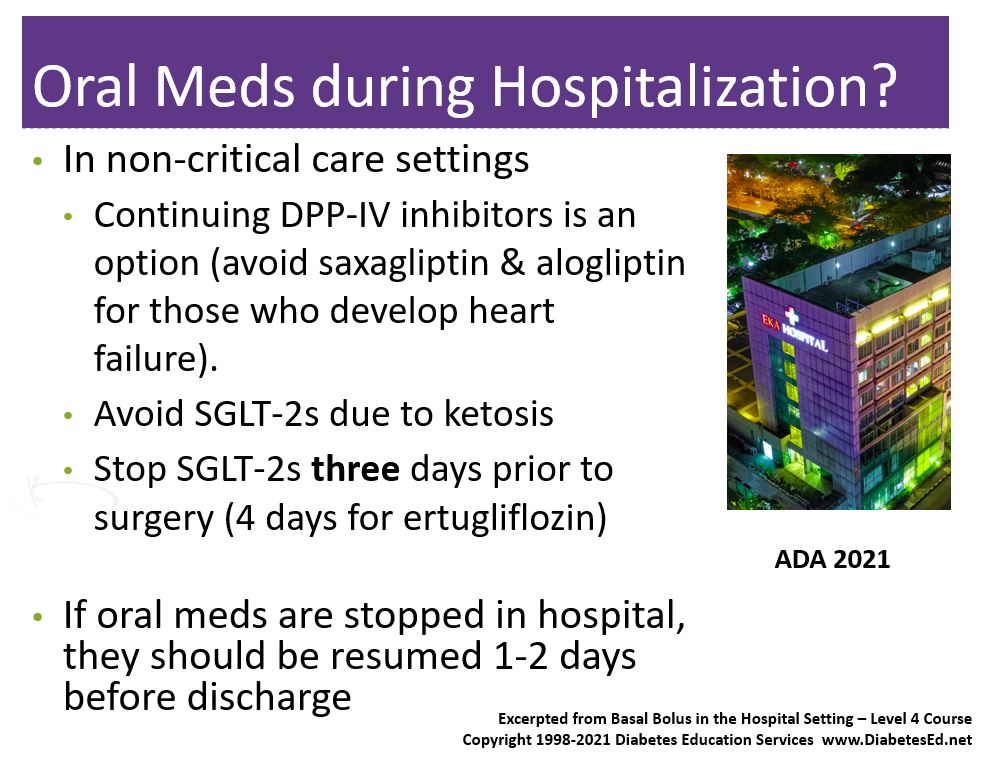
Answer 3 is correct, 48.40% of you chose this answer, “Stop empagliflozin (Jardiance) 3 days prior to surgery.” The new ADA 2021 Standards recommend stopping all SGLT-2s three days prior to surgery and ertugliflozin four days prior to surgery. In addition, SGLT-2s should be stopped with hospital admission. The reason behind this recommendation is to prevent DKA or ketoacidosis during hospitalization. (See slide below from our Basal Bolus in the Hospital Setting Level 4 Class).
Download Free Med PocketCards
Answer 4 is incorrect, 21.40% of you chose this answer, “Reduce basal insulin by half the night before surgery.” For someone with type 1 diabetes, if the basal rate is set correctly there is no basal dose reduction needed, even if someone is NPO. Reducing basal by 50% could actually put them at risk for hyperglycemia pre-operatively. If MS is at risk of hypoglycemia, we might consider making a 5-10% basal rate reduction, but not 50%.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
See ADA Standard 15 – Diabetes Care in the Hospital Setting
Want to learn more about this question and more?
Enroll on our
Basal/Bolus Therapy in Hospital Webinar 1.5 CEs
Recorded and Ready for viewing

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely and effectively implement Basal Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the individual’s clinical presentation and apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings and a discussion of solutions that will keep people safe and get glucose levels to goal. In addition, sample basal/bolus and insulin drip guidelines plus lots of resource articles are included.
Topics Include:
- Discussing appropriate insulin dosing based on the individual’s clinical presentation
- Applying dosing strategies to a variety of case studies
- Introduce hard-to-manage situations that commonly occur in hospital settings
- A discussion of solutions that will keep individuals safe and get glucose levels to goal
- Sample basal/bolus and insulin drip guidelines plus lots of resource articles are included
Join us for our Live Webinars
Including Brand New Specialty Courses!
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Why is A1c on the Rise?

Most of you, 69%, chose the best answer for our May 11th Question of the Week. Great job! We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: RT is 33 years old and has had diabetes for the past 20 years. RT uses an insulin pump and CGM and works hard to keep A1cs less than 7%. Their most recent A1c increased to 7.9% and RT sets up an appointment with the diabetes specialist for help. After downloading the report, the specialist thinks they have discovered the reason behind the increasing A1c.
Which of the following would most likely explain the A1c increase?
Answer Choices:
- Carbohydrate bolus insulin omissions
- Basal insulin rate set too high
- Bolus insulin given 15 minutes before meal
- CGM sensor malfunction
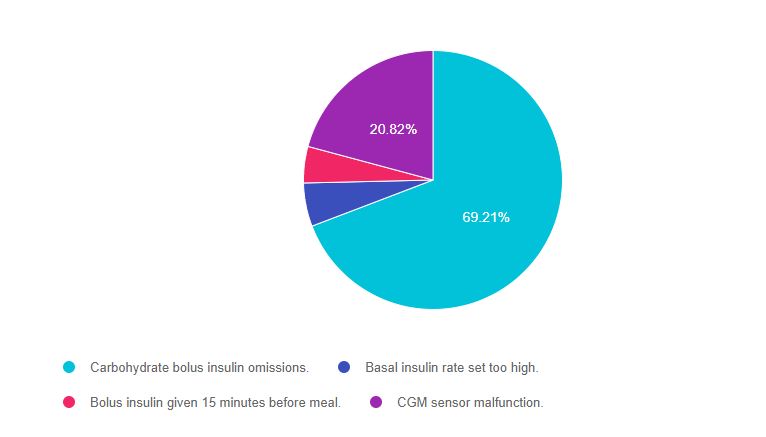
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with diabetes technology and helping people with problem solving and getting glucose to target.
Answers & Rationale
Answer 1 is correct, 69.21% chose this answer, “Carbohydrate bolus insulin omissions.” GREAT JOB! Skipping coverage for carbs, even once a day, can lead to a 1% increase in A1c. When discussing the data download with RT, the diabetes specialist will recognize all the actions that RT is doing correctly. Then, the specialist will share their observations that it seems RT sometimes skips bolusing for carb intake. The specialist can pause and see what RT says or the specialist could say something like, “can you tell me more about what is happening around these meals?”
Answer 2 is incorrect, 5.43% of you chose this answer, “Basal insulin rate set too high.” Getting to the correct basal rate is important to maintain glucose levels on target. If the basal rate is set too high, this means that RT would be getting too much insulin. This would result in hypoglycemia and a drop in A1c.
Answer 3 is incorrect, 4.55% of you chose this answer, “Bolus insulin given 15 minutes before meal.” The timing of bolus insulin before meals can make a big difference in getting glucose to target. Giving bolus insulin 15 minutes before meals can actually improve glucose levels since it allows the insulin peak to more closely match the post meal glucose elevation.
Answer 4 is incorrect, 20.82% of you chose this answer, “CGM sensor malfunction.” This is a juicy answer, but it doesn’t match the intent of the question. If the question said, “according to the CGM download the estimated A1c is 7.0% and the lab A1c is 7.9%” then we might consider this answer. However, we have no indication that the CGM sensor wasn’t working, nor do we have any data from the CGM to consider. That’s why this juicy answer is not the best one.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question and more?
Enroll in our Level 4 | Insulin Calculation Workshop – From Injections to Pumps Course | 1.5 CEs

Determining basal and bolus rates for multiple daily injections or insulin pumps can seem overwhelming. This 90-minute course provides participants with a step-by-step approach to determine basal rates, bolus ratios and how to problem solve when blood glucose levels aren’t on target. During this 90-minute course, Coach Beverly will provide abundant case studies to give participants hands-on practice and build confidence when calculating insulin doses for a variety of situations.
Objectives:
- Describe using formulas to determine appropriate insulin dosing.
- Discuss strategies to determine and fine-tune basal insulin dose
- Describe how to determine and fine-tune bolus rates including coverage for carbs and hyperglycemia.
- Using a case study approach, utilize calculations to determine the best insulin dosing strategy.
2021 Live Webinar Events
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of Week | Kidney Transplant and Hyperglycemia – Best Action?

Most of you, 73%, chose the best answer for our April 27th Question of the Week. Great job! We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is a 38 yr old who received a kidney transplant 3 months ago and has a GFR >60 and creatinine of 0.9. JR takes prednisone 10mg daily as part of the post-transplant protocol. JR’s most recent A1c came back at 7.9% and the provider asks the Diabetes Specialist what intervention is recommended.
Which of the following is the best response?
Answer Choices:
- Refer to a kidney specialist for a thorough workup.
- Encourage referral for medical nutrition therapy.
- Evaluate if JR can cut the prednisone dose in half.
- Instruct JR to start a very low-calorie diet to reverse hyperglycemia.
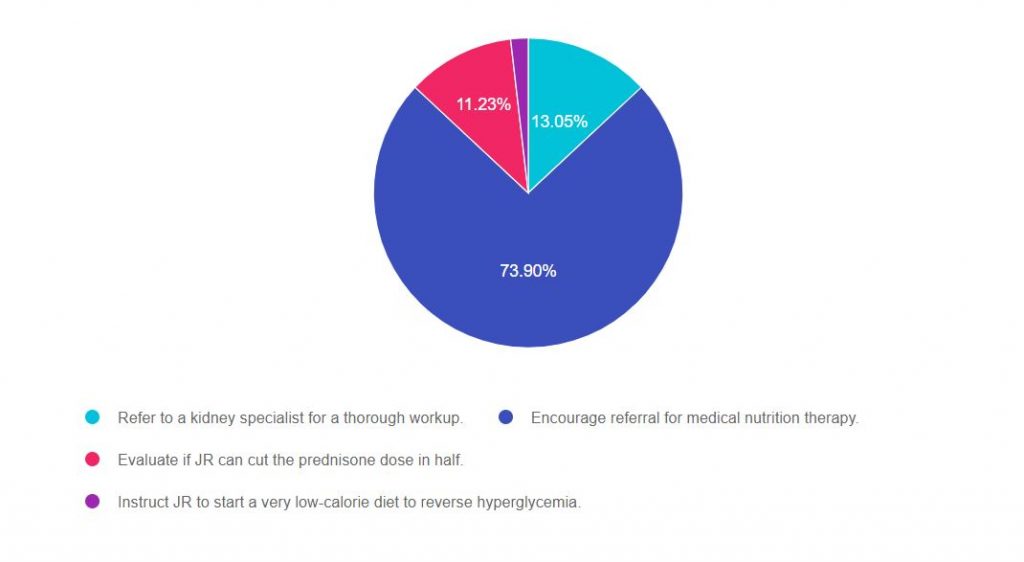
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 3, and finally option 4.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with identifying common diabetes co-conditions, screening guidelines and interventions.
Answers & Rationale
Answer 1 is incorrect, 13.05% chose this answer, “Refer to a kidney specialist for a thorough workup.” As many as 10-40% of solid organ transplant recipients develop post-transplant diabetes (PTDM). This is due to a combination of genetic susceptibility plus the anti-rejection medications, including steroid therapy (see slide below). Since JRs kidney function is terrific based on his GFR and creatinine, referring to a kidney specialist is not warranted. However, referring to DSME is high on the list of priorities.
Answer 2 is correct, 73.90% of you chose this answer, “Encourage referral for medical nutrition therapy.” YES, this is the BEST answer. For any person experiencing post-transplant diabetes, they will need a referral to an RD/RDN and DSME program to learn diabetes self-management strategies. They will also need medication therapy, but there is currently no standard treatment approach due to the complexities of mixing transplant medications with diabetes therapies. However, insulin therapy is a safe and effective option for those experiencing post-transplant hyperglycemia.
Answer 3 is incorrect, 11.23% of you chose this answer, “Evaluate if JR can cut the prednisone dose in half.” Prednisone therapy is a critical intervention to prevent post-transplant rejection. For this reason, maintaining prednisone therapy is a priority. Diabetes specialists can help determine strategies to keep glucose on target to prevent infection, support graft health and limit other complications.
Answer 4 is incorrect, 1.82% of you chose this answer, “Instruct JR to start a very low-calorie diet to reverse hyperglycemia.” To maintain graft function and quality of life post-transplant, a very low-calorie diet is not recommended. To address this JR’s treatment plan will include a combination of healthy eating, activity plus diabetes medications.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question and more?
Enroll in our Level 2 – Critical Assessment – Fine-Tuning your Diabetes Detective Skills – 2.0 CEs

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: 90-minute video presentation, podcast, practice test, and additional resources.
This course integrates the ADA Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies and real-life situations, we discover often hidden causes of hyperglycemia and other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, and more. We delve into therapy for complicated situations and discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, and Transplants. Join us for this unique and interesting approach to assessing and evaluating the hidden complications of diabetes.
Topics Include:
- Identify common yet often underdiagnosed complications associated with type 1 and type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia and other conditions including, transplant, cystic fibrosis and liver disease.
Intended Audience: A great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Mystery Condition

For our April 20th Question of the Week, 44% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: ML has had type two diabetes for 12 years, a BMI of 33.7, an A1 C of 8.3%, and elevated triglycerides and LDL cholesterol levels. You notice ML’s palms are deeply red.
Which of the following conditions is ML most likely experiencing in addition to diabetes?
Answer Choices:
- Non-alcoholic fatty liver disease
- Dermatomyositis secondary to inflammation
- Auto immune renal hypertension
- Acanthosis Nigricans of the palmar surface
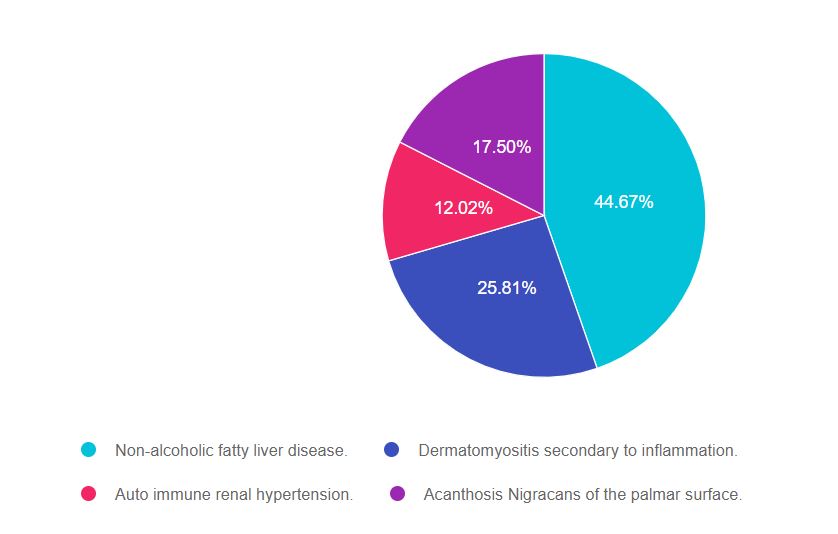
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 4, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to be familiar with identifying common diabetes co-conditions, screening guidelines and interventions.
Answers & Rationale
Answer 1 is correct, 44.67% chose this answer, “Non-alcoholic fatty liver disease.” Good job! Up to 20% of people with diabetes are living with non alcoholic steatohepatitis (NASH) which can lead to cirrhosis, liver failure and cancer. Risk factors associated with NASH include hyperlipidemia, hyperglycemia, and a BMI of 30 or greater. People with NASH may have elevated liver enzymes including ALT and AST. Physical symptoms include acanthosis nigricans, abdominal pain, sense of fullness, facial spider angiomas and red palms.
The major focus of treatment includes weight loss, increased activity, aggressive management of lipids and glucose. Some research also indicates that Actos, Vitamin E and liraglutide may improve liver histology. Join our Critical Assessment Course to learn more about NASH and other diabetes co-conditions.
Answer 2 is incorrect, 25.81% of you chose this answer, “Dermatomyositis secondary to inflammation.” This rare autoimmune condition is usually associated with type 1 diabetes. Signs of dermatomyositis include a dusky red rash on the face and eyelids, and in areas around the nails, knuckles, elbows, knees, chest, and back. Muscle weakness is frequent.
ML’s profile doesn’t match the clinical manifestations of this condition.
Answer 3 is incorrect, 12.02% of you chose this answer, “Auto immune renal hypertension.” This juicy answer with a fancy name suggests that ML has this rare condition. However, since ML has type 2 diabetes, test takers would be suspicious of any answer that points to autoimmune conditions. Type 2 is not an immune mediated condition, but a condition of inflammation.
ML’s profile doesn’t match the clinical manifestations of this condition.
Answer 4 is incorrect, 17.50% of you chose this answer, “Acanthosis Nigricans of the palmar surface.” Acanthosis nigricans (AN) is a dermatologic indicator of insulin resistance. However, it does not present on the palms, nor is it red in color. AN is a darkening and thickening of the skin often coupled with the appearance of skin tags. Common locations for AN include folds of skin in the neck, axilla, groin, elbows, knees and ankles.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more? Join Coach Beverly and the Critical Assessment Course. It is ready for viewing!
Level 2 – Critical Assessment – Fine-Tuning your Diabetes Detective Skills – 2.0 CEs.

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: 90-minute video presentation, podcast, practice test, and additional resources.
This course integrates the ADA Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies and real-life situations, we discover often hidden causes of hyperglycemia and other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, and more. We delve into therapy for complicated situations and discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, and Transplants. Join us for this unique and interesting approach to assessing and evaluating the hidden complications of diabetes.
Topics Include:
- Identify common yet often underdiagnosed complications associated with type 1 and type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia and other conditions including, transplant, cystic fibrosis and liver disease.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in enhancing their diabetes assessment skills.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Exercise & Heart Rate Mystery

For our April 13th Question of the Week, 62% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: LR loves going to the gym 3 times a week. LR is 78, with Latent Autoimmune Diabetes (LADA) and is on basal bolus insulin. LR also takes a statin and ACE Inhibitor. LR has a history of retinopathy and peripheral neuropathy. During your assessment, LR proudly shares that when on the treadmill, their heart rate never goes above 100 beats per minute.
What best explains this heart rate?
Answer Choices:
- Excellent cardiovascular health from regular exercise
- Cardiac autonomic neuropathy
- Stiff heart syndrome
- ACE Inhibitors can contribute to lower heart rates
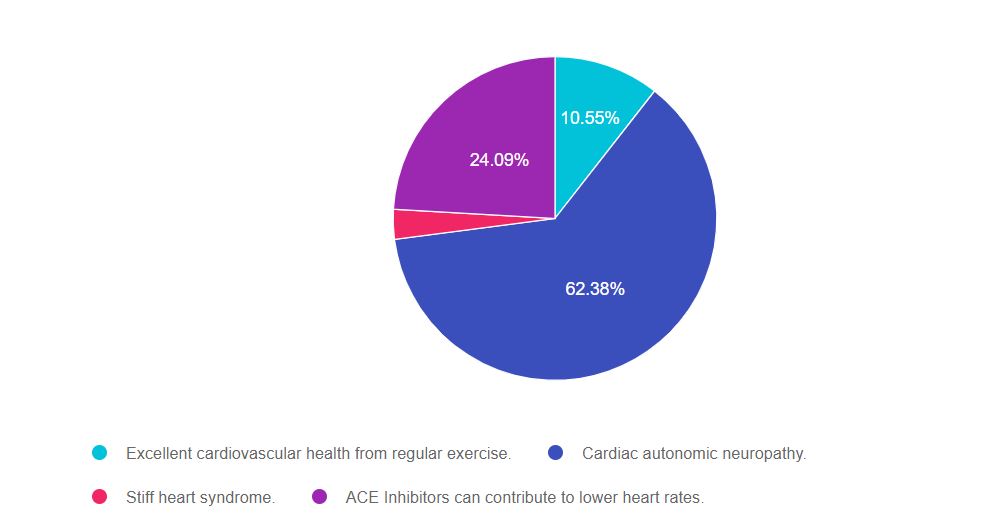
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 1, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 10.55% chose this answer, “Excellent cardiovascular health from regular exercise .” On first blush, this answer is tempting, yet it doesn’t consider in all the factors described in the case study. If we look at his age and the presence of microvascular disease and neuropathy, we are correct to suspect that he may also have autonomic neuropathy. Therefore, his low heart rate isn’t an indication of robust health but a sign of autonomic dysfunction.
Answer 2 is correct, 62.38% of you chose this answer, “Cardiac autonomic neuropathy.” Good job! When we look at his age and the presence of microvascular disease and neuropathy, we are right to suspect he also has cardiac autonomic neuropathy. As a result of nerve disease, his heart rate isn’t able to respond to the cardiac demand of intense exercise and never exceeds 100. This “fixed heart rate” is a sign of autonomic dysfunction that warrants further investigation.
Answer 3 is incorrect, 2.98% of you chose this answer, “Stiff heart syndrome.” People with diabetes are more likely to have stiff fibrotic hearts and this can lead to increased risk of heart failure. However, there is no such condition as a “stiff heart syndrome”. This answer was a distractor.
Answer 4 is incorrect, 24.09% of you chose this answer, “ACE Inhibitors can contribute to lower heart rates.” This was our juicy answer. The blood pressure class of ACE Inhibitors does not lower heart rates but does lower blood pressure. The blood pressure class Beta Blockers, can lower heart rate, but it was not included in this question. See our Med Cheat Sheets 2021 | Hypertension, Lipids, and Neuropathy for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more?
Join us for our Level 2 – Critical Assessment – Fine-Tuning your Diabetes Detective Skills – 2.0 CEs.

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: 90-minute video presentation, podcast, practice test, and additional resources.
This course integrates the ADA Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies and real-life situations, we discover often hidden causes of hyperglycemia and other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, and more. We delve into therapy for complicated situations and discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, and Transplants. Join us for this unique and interesting approach to assessing and evaluating the hidden complications of diabetes.
Topics Include:
- Identify common yet often underdiagnosed complications associated with type 1 and type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia and other conditions including, transplant, cystic fibrosis and liver disease.
Intended Audience: A great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1, Ramadan & Fasting

For our April 6th Question of the Week, 47% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: RS observes Ramadan and fasts from sunrise to sunset. RS is 13 years old, has type 1 diabetes, uses an insulin pump and CGM. RS’s insulin-to-carb ratio is 1:12 and correction is 1:45. Basal settings range from 0.5 -1.2 units an hour.
What would be the best recommendation for RS to keep blood sugars in the target range during Ramadan?
Answer Choices:
- See if RS can get a note from their doctor to allow eating during the day.
- Take bolus insulin when RS eats a meal or snack.
- Decrease basal insulin rate by 50% during periods of fasting.
- Monitor urine ketones at least twice a day.
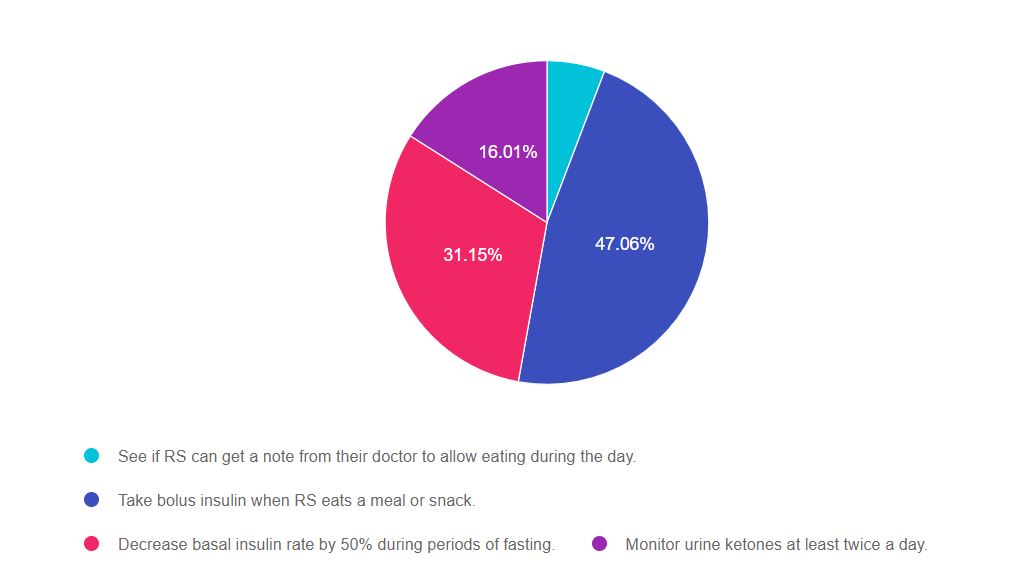
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 5.79% chose this answer, “See if RS can get a note from their doctor to allow eating during the day.” As diabetes specialists, we are at our best when we tap into our cultural humility. We may not be familiar with the customs and celebrations of other cultures, but we can honor these traditions and express sincere interest in learning more about them. In this situation, we would respect their tradition, explore potential issues surrounding fasting and help with problem solving and creating a back up plan in case an issue arises.
Answer 2 is correct, 47.06% of you chose this answer, “Take bolus insulin when RS eats a meal or snack.” Good Job! When the basal rates of an insulin pump are set correctly, a person with type 1 diabetes can fast and still keep glucose on target. This background or basal insulin works to manage glucose levels in between meals and through the night. Actually, this period of fasting will provide an opportunity to evaluate if basal settings need adjustment or if they are set correctly. When RS breaks the fast at sunset, they will just need to dose for carbohydrates and cover for hyperglycemia if needed.
Answer 3 is incorrect, 31.15% of you chose this answer, “Decrease basal insulin rate by 50% during periods of fasting.” When the basal rates of an insulin pump are set correctly, a person with type 1 diabetes can fast and still keep glucose on target. This background or basal insulin works to manage glucose levels in between meals and through the night. If RS is receiving too much basal insulin and experiences low blood sugars during periods of fasting, they will need to fine tune their basal rates. However, we would not suggest to automatically decrease basal rate by 50% in preparation for fasting.
Answer 4 is correct, 16.01% of you chose this answer, “Monitor urine ketones at least twice a day.” Since RS has an insulin pump that delivers basal insulin 24 hours a day, they are at low risk for ketosis. Ketosis is usually a result of insufficient insulin administration. Without adequate insulin, fats are utilized as an alternate energy source, leading to positive ketones. In this situation, RS is receiving adequate insulin through the pump and is not at increased risk of significant ketosis.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
On Sale | Now just $24.95
ADA 2021 Standards of Medical Care in Diabetes Book
The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
One of the most important pieces of literature to read prior to becoming a Diabetes Care and Education Specialist and for clinical practice, the Standards of Care book is a study must!
The book includes:
- ADA’s standards for diagnosing and treating diabetes
- Nutrition recommendations and principles
- Position statements on managing diabetes and its complications in various settings
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Black Spots in Eyes

For our March 30th Question of the Week, 79% of respondents chose the best answer. We wanted to “take a closer look” into this question. What is the best action to take for some one who is experiencing eye issues?
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR was recently diagnosed with type two diabetes. JR‘s A1 C was 13.9%, but now blood sugars are running in the 100 to 180 range. JR mentions that they have been noticing “black spots” floating in their eyes.
What is the best response by the diabetes specialist?
Answer Choices:
- This is an expected finding when blood sugars drop rapidly.
- On a scale of 1 to 10, how much are these spots affecting your daily quality of life?
- That must be really scary. Make sure to mention this at your next provider visit.
- Let’s get you scheduled in to see ophthalmology.
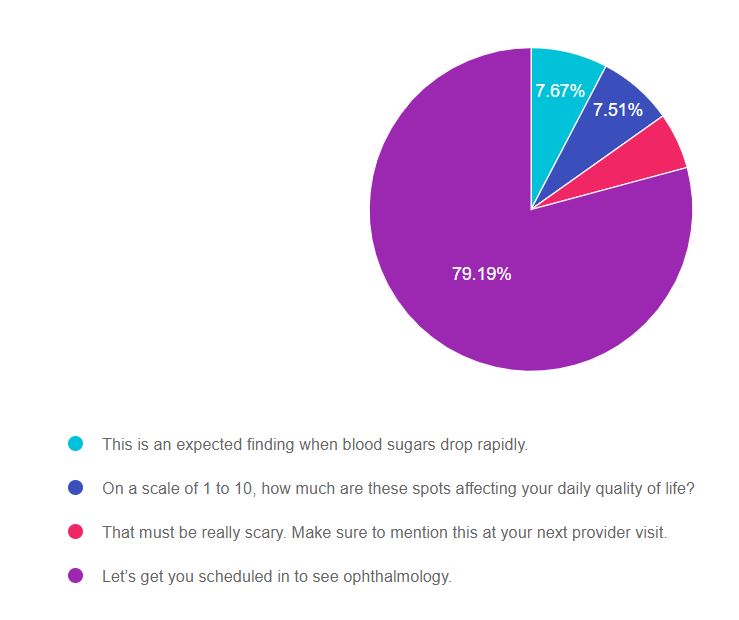
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 7.67% chose this answer, “This is an expected finding when blood sugars drop rapidly.” Actually, this is not an expected finding and warrants immediate investigation.
When people with diabetes experience fluctuations in blood sugars, they may complain of blurry vision and their glasses not working due to fluid shifts. However, a rapid drop in glucose can intensify the risk of retinal bleeds. “Black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 2 is incorrect, 7.51% of you chose this answer, “On a scale of 1 to 10, how much are these spots affecting your daily quality of life?” This assessment question would be appropriate if the person was receiving treatment for eye problems already and we are evaluating the impact on daily life. However, this is not the case.
This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 3 is incorrect, 5.63% of you chose this answer, “That must be really scary. Make sure to mention this at your next provider visit.” Yes, it is important to notify the provider, IMMEDIATELY. What if the next provider visit is in 6 months or a year? What if JR misses that appointment and gets lost to follow-up?
This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 4 is correct, 79.19% of you chose this answer, “Let’s get you scheduled in to see ophthalmology.” GREAT JOB. Most of you chose this answer. This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems and many people with diabetes don’t receive regular eye care. Let’s help break down barriers and make sure people with diabetes get the eye care they deserve.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








