
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
For last week’s practice question, we quizzed participants on Best example of Person-Centered Question. 93% of respondents chose the best answer – GREAT JOB! We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: RJ is entering the field of diabetes care and education and has heard about the new language movement but isn’t sure how to apply it to their clinical practice. Which of the following is the best example of using person-centered language when speaking to someone with diabetes?
Answer Choices:
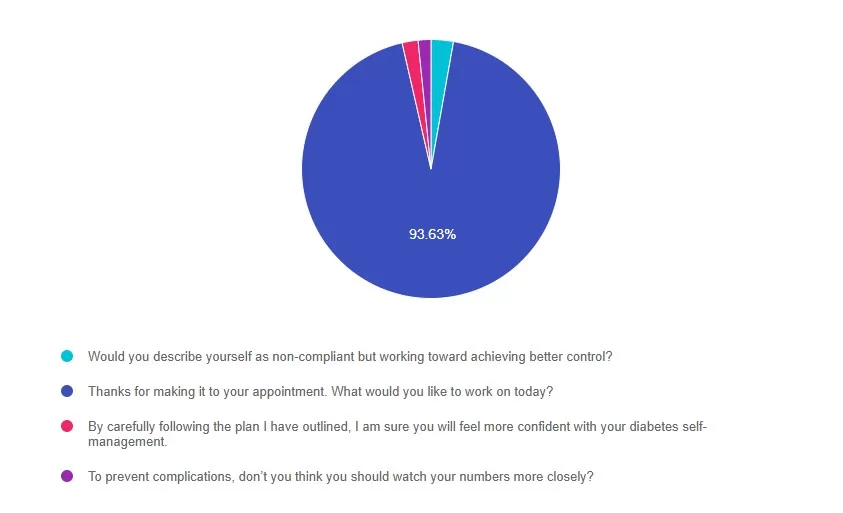
Answer 1 is incorrect. 2% chose this answer, “Would you describe yourself as non-compliant but working toward achieving better control?” This response uses outdated judgmental terms like “non-compliant” and “control”.
Answer 2 is correct. 93% of you chose this answer, “Thanks for making it to your appointment. What would you like to work on today?” This uses respectful, person-first language and invites collaboration by focusing on the individual’s goals.
Answer 3 is incorrect. About 1% of respondents chose this, “By carefully following the plan I have outlined, I am sure you will feel more confident with your diabetes self-management.” This non-collaborative approach doesn’t include the individual in creating a plan.
Finally, Answer 4 is incorrect. 1% chose this answer, “To prevent complications, don’t you think you should watch your numbers more closely?” This uses a negative tone and the outdated “should” word. It can lead to shame or resistance.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on What best describes the action of GLP-1 Receptor Agonists? 54% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which of the following is accurate statement regarding Glucagon Like Peptides (GLP-1)?
Answer Choices:
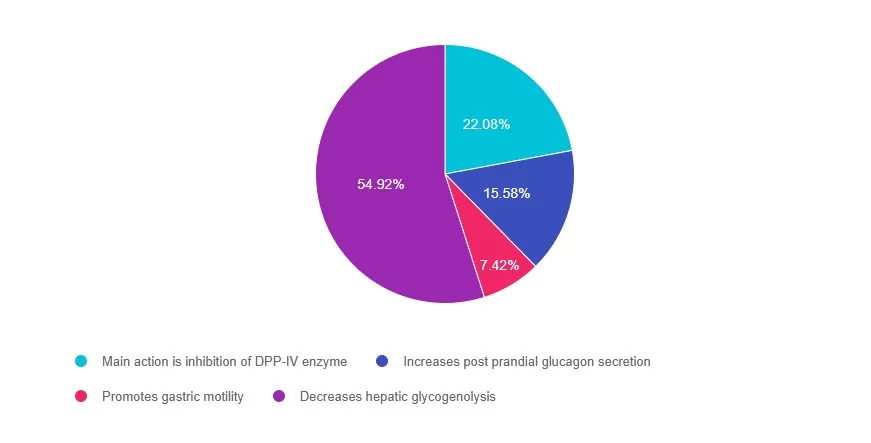
Answer 1 is incorrect. 22% chose this answer, “Main action is inhibition of DPP-IV enzyme.” The GLP-1’s do not inhibit the action of the DPP-IV enzyme (that is the DPP-IV inhibitor class). GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 2 is incorrect. 15% of you chose this answer, “Increases post prandial glucagon secretion.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon, slow gastric emptying and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 3 is incorrect. About 7% of respondents chose this, “Promotes gastric motility.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Finally, Answer 4 is correct. 54% chose this answer, “Decreases hepatic glycogenolysis.” YES – GREAT JOB! GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon which decreases hepatic glycogenolysis. They also slow gastric emptying, stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on What Helps Manage Gastroparesis in Type 1 Diabetes? 80% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: VC has been living with type 1 diabetes for 43 years and was recently diagnosed with gastroparesis. Symptoms have included early satiety, nausea, bloating and intestinal pain. VC has an A1c of 6.7% but is experiencing frequent hypoglycemia. What general nutrition modifications would VC benefit from?
Answer Choices:
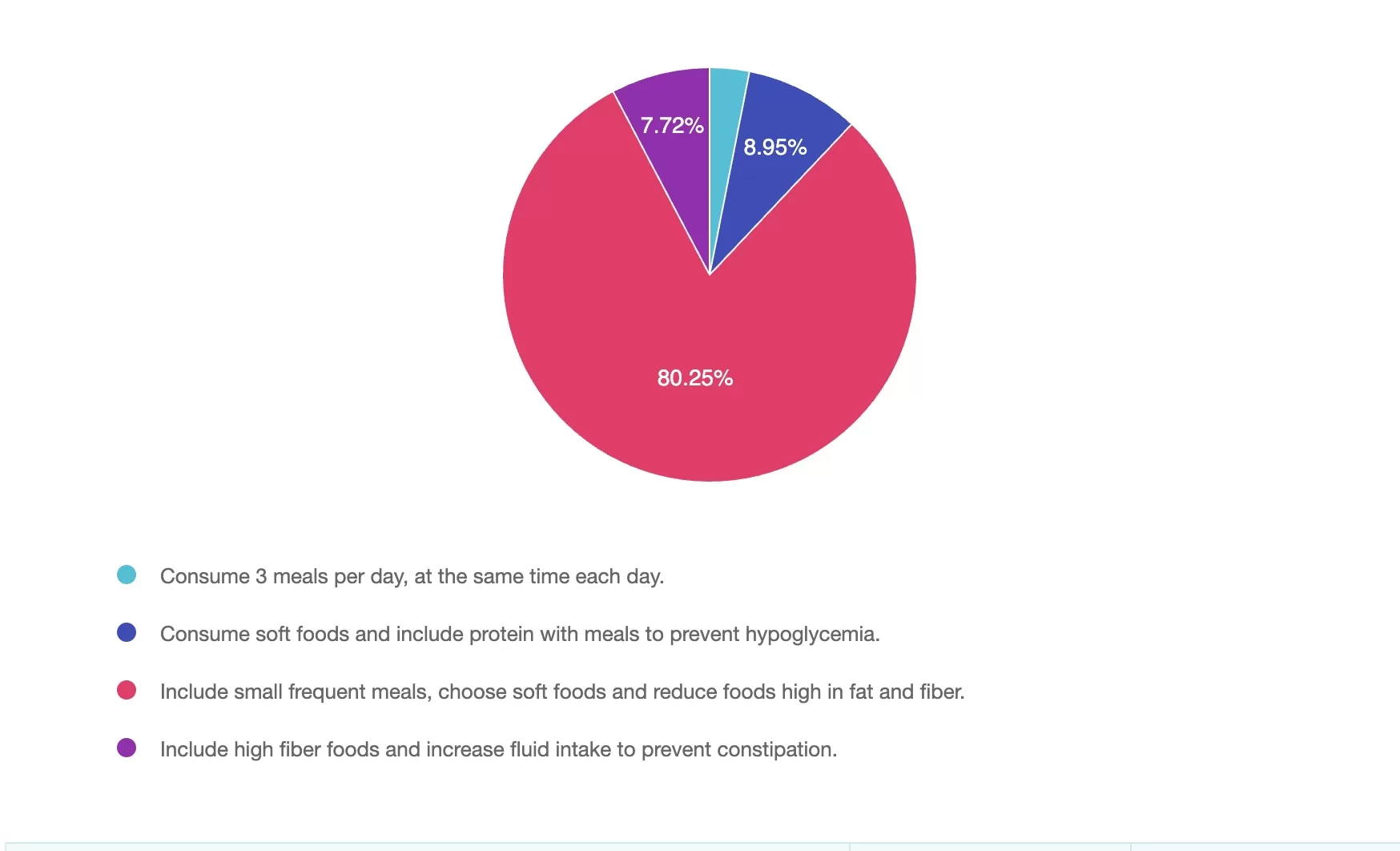
Answer 1 is incorrect. 3% chose this answer, “Consume 3 meals per day, at the same time each day.” This approach can be helpful to manage glucose for some individuals with diabetes, however in gastroparesis timing, meal size, type of foods, and food textures are key.
Answer 2 is incorrect. 8% of you chose this answer, “Consume soft foods and include protein with meals to prevent hypoglycemia.” While soft foods and adequate protein is important, this doesn’t address the need to reduce fat and fiber and shift to smaller, more frequent meals.
Answer 3 is correct. About 80% of respondents chose this, “Include small frequent meals, choose soft foods and reduce foods high in fat and fiber.” Small frequent meals can improve rate of motility through the stomach to small intestine, low fat and low fiber whole foods also tend to move more quickly from the stomach (liquid sources may be tolerated better), and soft foods such as well-cooked vegetables to tender proteins may help reduce nausea, bloating and can ease the digestive process. Individual assessment of rate of digestion and insulin administration timing should also be considered to reduce the risk of post-prandial hypoglycemia.
Finally, Answer 4 is incorrect. 7% chose this answer, “Include high fiber foods and increase fluid intake to prevent constipation.” A high fiber diet can often worsen symptoms in gastroparesis by slowing gastric emptying further. Fluids are important, but fiber from whole foods is typically reduced.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Managing Overnight Hypoglycemia: Best Plan? 86% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Your client wants to discuss a concern about overnight hypoglycemia alerts on the CGM. These hypoglycemia alerts have been happening intermittently and only in the overnight hours. The client reports no changes in diet, activity, or insulin doses over the past 2 weeks. These events are asymptomatic, and the client reports that these episodes resolve rapidly before they can get to the kitchen to treat the hypoglycemic event. What is the best plan of action for this client?
Answer Choices:
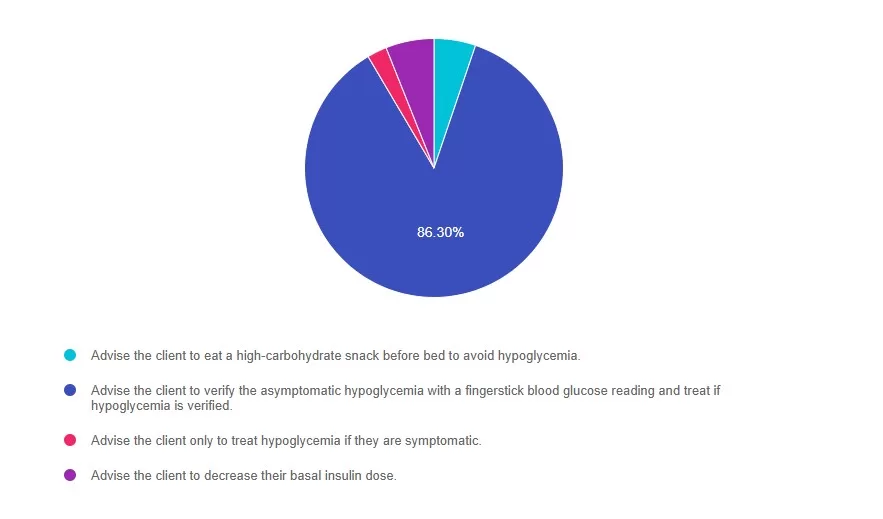
Answer 1 is incorrect. 4% chose this answer, “Advise the client to eat a high-carbohydrate snack before bed to avoid hypoglycemia.” Although tempting, eating a high-carbohydrate snack before bed doesn’t address the need to verify an asymptomatic and unexpected low blood glucose.
Answer 2 is correct. 86% of you chose this answer, “Advise the client to verify the asymptomatic hypoglycemia with a fingerstick blood glucose reading and treat if hypoglycemia is verified.” GREAT JOB! Continuous glucose monitors are susceptible to compression lows. These lows occur when pressure is applied to the sensor/transmitter, which can occur during sleep. This can result in hypoglycemia alerts. Diabetes care and education specialists can help recognize this pattern and coach clients using CGM technology to verify any asymptomatic or unexpected hypoglycemia with a fingerstick blood glucose reading before making a treatment decision.
Answer 3 is incorrect. About 2% of respondents chose this, “Advise the client only to treat hypoglycemia if they are symptomatic.” All clients need to be encouraged to verify any unexpected glucose readings, particularly if they have asymptomatic hypoglycemia, with a fingerstick blood glucose reading before treating.”
Finally, Answer 4 is incorrect. About 5% of you chose this answer, “Advise the client to decrease their basal insulin dose.” The blood glucose readings need to be verified before adjusting the basal insulin dose.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live on July 15th and July 22nd, 2025 at 9:00 am PST
6+ CEs with Expanded Accreditation!
Join experts Larry Fisher, Ph.D., ABPP, Susan Guzman, Ph.D., and Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, for this transformative two-part training on the ReVive 5 framework—an evidence-based approach that integrates emotional well-being and glucose data into person-centered diabetes care.
Grounded in the results of the EMBARK Trial, this program emphasizes the urgent need to assess and address diabetes distress, now recognized in the ADA Standards of Care as a critical component of care. You’ll gain practical tools and strategies used in the trial to support emotional well-being, meet clinical standards, and empower individuals on their diabetes journey.
Upon completion of this activity, participants will be able to:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:



Lawrence Fisher, Ph.D., ABPP
Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
CEO of DiabetesEd Services
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Speaker Interview:
Bio:
Dr. Fisher has been a professor in the Department of Family & Community Medicine at the University of California, San Francisco for over 25 years, and he is the Director of The Behavioral Diabetes Research Group at UCSF.
He has a Diplomate in Clinical Psychology from the American Board of Professional Psychology and is a former Associate Editor of Diabetes Care. He has conducted multiple cross-sectional and longitudinal NIH- and ADA-supported clinical research with adults with diabetes and their families.
His recent work focuses on diabetes distress and depression, disease management, and how adults and families struggle over time to manage chronic health conditions. He has won two major UCSF School of Medicine teaching awards, was nominated for the UCSF Postdoctoral Scholars Association Outstanding Mentorship Award, and has received a certificate from the American Psychological Association in “Recognition for Substantial Contributions to the Field of Family Psychology and Health.”
In 2012 he received the Richard Rubin Award from the American Diabetes Association. He maintains an active clinical practice at UCSF, has published over 190 peer-reviewed articles on diabetes and related topics, and frequently speaks to both professional and lay groups at local, national, and international meetings and workshops.
 Susan Guzman, PhD
Susan Guzman, PhD
Dr. Guzman is a clinical psychologist specializing in diabetes. In 2003, Dr. Guzman co-founded the Behavioral Diabetes Institute (BDI), the first non-profit organization devoted to the emotional and behavioral aspects of living with diabetes.
At BDI, she serves as the Director of Clinical Education, developing and leading programs for people with diabetes and healthcare professionals. She has helped develop and facilitate diabetes distress group interventions for two NIH-funded research studies for adults with type 1 diabetes.
Dr. Guzman is passionate about helping to change the conversations in diabetes away from shame, blame, and judgment to those based on facts, empathy, and engagement. She has been part of a joint ADA/ADCES effort to address problematic language and messages in diabetes.
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADMBeverly Thomassian has no financial disclosures
Speaker Interview:
Bio:
Activity Start and End Date: 7/15/2025 to 7/22/2027
Estimated time to complete the activity: 6 hours and 15 minutes
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 6.25 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 6.25 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 6.25 contact hour(s) (.625] CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – UAN JA4008073-9999-25-198-H01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 6.25 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 6.25 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 6.25 Interprofessional Continuing Education (IPCE) credit for learning and change.
Disclosure of Unlabeled Use:
This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings.
Disclaimer:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
Instructions for Credit
Participation in this self-study activity should be completed in approximately 6 hours and 15 minutes. To successfully complete this activity and receive CE credit, learners must follow these steps during the period from 7/15/2025 to 7/22/2027.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Diabetes Burnout Despite Control. 94% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question.

Question: Jada, a 29-year-old with type 1 diabetes, tells you she’s feeling burned out and emotionally drained, despite maintaining a time in range above 70% for the past several months. She says, “I’m doing everything right, but I’m exhausted and don’t feel like myself lately.” You review her CGM data and see no major red flags. She denies any recent illnesses or major changes in insulin needs. What is the most appropriate next step?
Answer Choices:
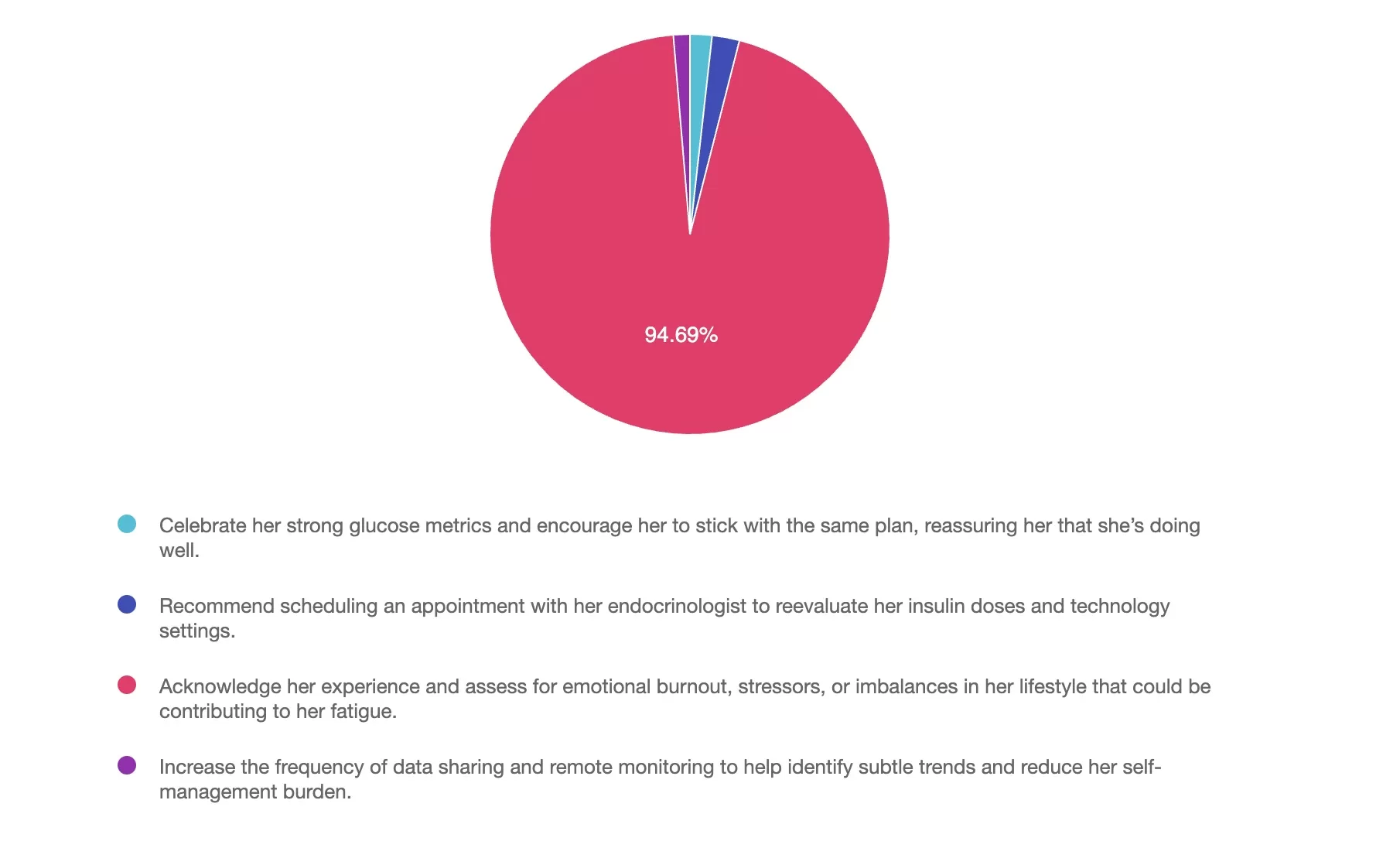
Answer 1 is incorrect. 1% chose this answer, “Celebrate her strong glucose metrics and encourage her to stick with the same plan, reassuring her that she’s doing well.” While it’s important to acknowledge the hard work it takes to stay in range, this answer misses the bigger picture. Jada is telling us she’s struggling emotionally — this is not the time to brush past her experience. High time in range does not always equal high quality of life. When someone shares they’re feeling burned out, it’s our cue to pause and dig deeper, not simply pat them on the back and move on.
Answer 2 is incorrect. 2% of you chose this answer, “Recommend scheduling an appointment with her endocrinologist to reevaluate her insulin doses and technology settings.” Jada isn’t expressing concerns about her insulin needs — she’s talking about emotional exhaustion. Jumping to insulin or tech adjustments may send the message that we’re not really listening. Yes, there’s always room to optimize settings, but that’s not the priority here. This response may unintentionally medicalize a problem that’s likely rooted in something else.
Answer 3 is correct. About 94% of respondents chose this, “Acknowledge her experience and assess for emotional burnout, stressors, or imbalances in her lifestyle that could be contributing to her fatigue.” YES — this is the best answer. Jada is doing a great job with her glucose, but she’s telling us she’s tired. Diabetes burnout is real, even when the data looks “perfect.” This is our opportunity to normalize her feelings, offer support, and explore what might be out of balance — whether it’s stress, sleep, relationships, or unrealistic expectations around self-management. Holistic care means seeing the person, not just the numbers.
Finally, Answer 4 is incorrect. 1% chose this answer, “Increase the frequency of data sharing and remote monitoring to help identify subtle trends and reduce her self-management burden.” While that might sound helpful, more data is not necessarily the answer here. In fact, increasing monitoring could add to Jada’s mental load — and she’s already telling us she’s exhausted. If anything, now might be a time to consider reducing the burden, simplifying routines, or talking about boundaries with diabetes tech.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live on July 24th, 2025, at 11:30 am PST to watch our brand new webinar, Beyond Blood Glucose: Empowering Health Through a Holistic Lens by Nick Kundrat, BS, CEP, CDCES, LMT
Despite the rise of cutting-edge diabetes technologies and therapeutics, many people with diabetes still struggle with fatigue, blood glucose swings, and burnout. Why? Because we’re often so focused on managing diabetes itself that we often forget to take care of the human being who lives with it.
Join Nick Kundrat, BS, CEP, CDCES, LMT and Integrative Health Practitioner, for an engaging webinar where he simplifies the often-misunderstood world of holistic health. You’ll learn practical, accessible strategies to begin thinking more holistically and discover simple, effective tools that enhance conventional care and empower people with diabetes to thrive—physically, emotionally, and spiritually.
Drawing from over two decades of lived experience with type 1 diabetes and years of supporting clients in both clinical and holistic settings, Nick offers a unique perspective on diabetes care focused on the whole person. Through reconnecting with the foundational elements of health, which are often overlooked in conventional diabetes care, Nick aims to equip you with actionable strategies to help people with diabetes restore their energy, support their bodies, and thrive beyond diabetes.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, our special guest expert Jill Schramm, DNP, FNP-C, BC-ADM, CDCES quizzed us on Current Hormone Therapy Guidance for people with T2D. 57% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which statement accurately reflects current guidelines on hormone therapy (HT) in postmenopausal women with type 2 diabetes?
Answer Choices:
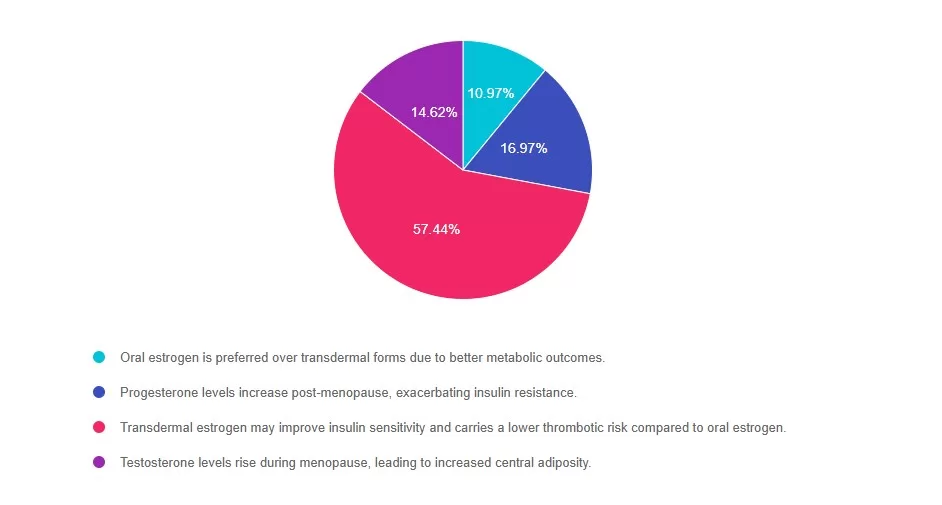
Answer 1 is incorrect. 10% chose this answer, “Oral estrogen is preferred over transdermal forms due to better metabolic outcomes.” Oral estrogen undergoes first-pass hepatic metabolism, which can negatively influence clotting factors. Transdermal estrogen bypasses the liver and is generally favored in women with cardiometabolic risk, such as those with type 2 diabetes.
Reference: The Menopause Society, 2022; American Diabetes Association (ADA) Standards of Care in Diabetes; 2025.
Answer 2 is incorrect. 16% of you chose this answer, “Progesterone levels increase post-menopause, exacerbating insulin resistance.” Progesterone levels actually decrease after menopause due to ovarian senescence. There is no physiological increase in progesterone levels that would worsen insulin resistance during the postmenopausal years.
Reference: The Menopause Society, 2022.
Answer 3 is correct. About 57% of respondents chose this, “Transdermal estrogen may improve insulin sensitivity and carries a lower thrombotic risk compared to oral estrogen.” GREAT JOB. This is the best answer and aligns with current guidelines. Transdermal estrogen has been shown to improve insulin sensitivity and does not increase hepatic production of clotting factors the way oral estrogen does. As a result, it is associated with a lower risk of venous thromboembolism, making it a safer option for postmenopausal women with metabolic concerns such as type 2 diabetes.
Reference: The Menopause Society (formerly NAMS), 2022 Position Statement
Finally, Answer 4 is incorrect. 14% chose this answer, “Testosterone levels rise during menopause, leading to increased central adiposity.“Testosterone levels generally decline with age and menopause, although the ratio of testosterone to estrogen may shift due to declining estrogen. While visceral adiposity does tend to increase in menopause, it is more directly related to estrogen deficiency rather than a surge in testosterone.
Reference: The Menopause Society, 2022.
Thanks to Jill Schramm, DNP, FNP-C, BC-ADM, CDCES for her providing us with these terrific insights into menopause. Join her presentation on August 27th to learn more! See info below. Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live on August 27th, 2025, at 11:30 am PST to watch our brand new webinar, Hot Flashes & Hyperglycemia: What Clinicians Need to Know by Dr. Jill Schramm, DNP, FNP-C, BC-ADM, CDCES
The intersection of menopause and diabetes is often underrecognized in clinical care, yet people with diabetes in menopausal transition face unique metabolic, hormonal, and lifestyle changes that can significantly impact glycemic control. This session explores the physiological shifts of menopause, the implications for insulin resistance, and evidence-based strategies for individualized care. Attendees will leave with practical guidance on hormone therapy, lifestyle management, and education tools to improve outcomes for people with diabetes navigating both diabetes and the menopausal transition.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on T1D and Artificial Sweeteners: Safe Limits. 95% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Sam is a 28-year-old with type 1 diabetes who reports drinking six diet sodas per day, believing they help manage blood sugar. Sam asks if this is safe or if they should reduce consumption. What would be an appropriate response based on the 2025 ADA Standards of Care?
Answer Choices:
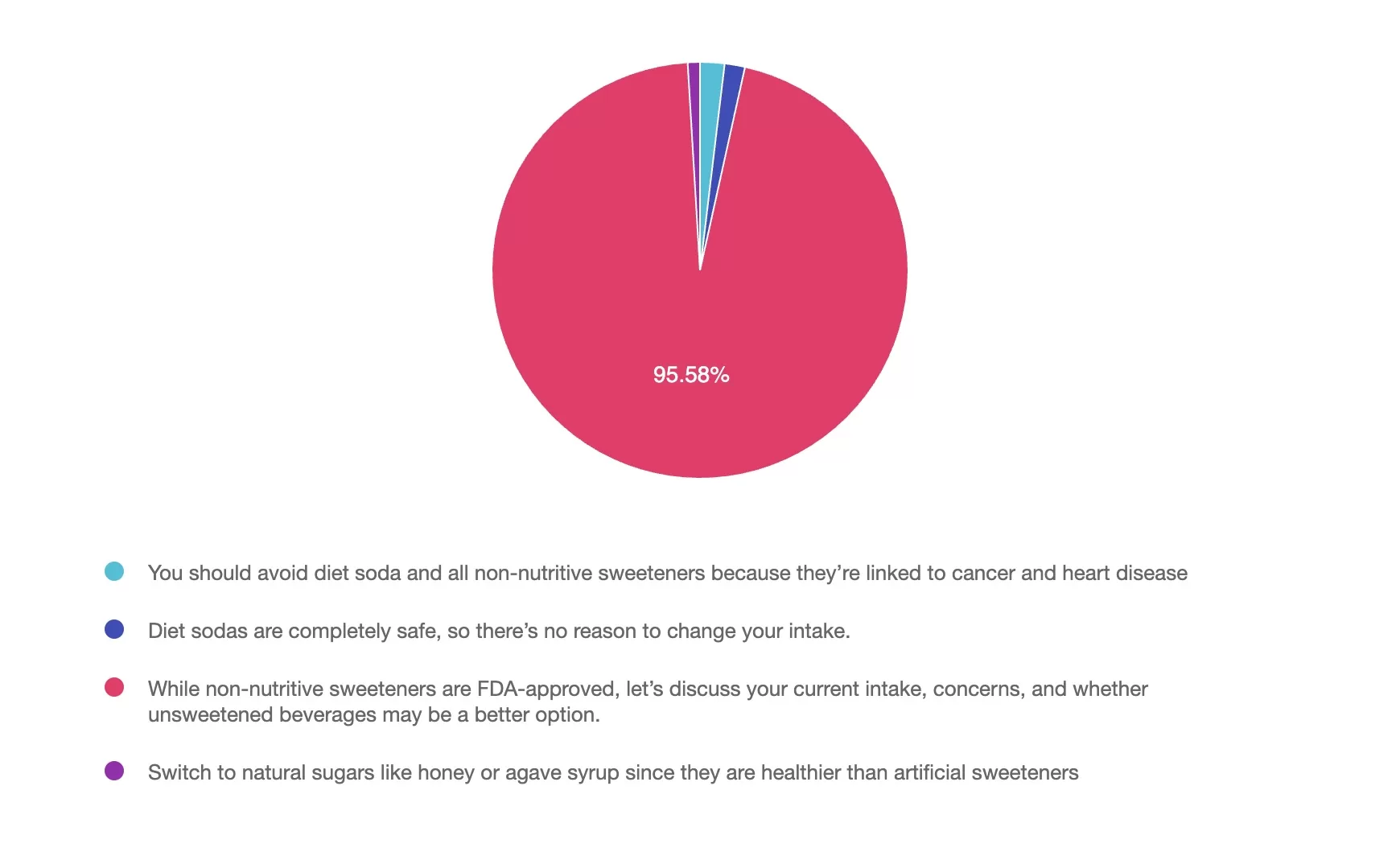
Answer 1 is incorrect. 1% chose this answer, “You should avoid diet soda and all non-nutritive sweeteners because they’re linked to cancer and heart disease.” While concerns about non-nutritive sweeteners (NNS) exist, especially aspartame and erythritol, the ADA and FDA consider approved sweeteners safe and within acceptable daily intake levels. Blanket avoidance is not person-centered nor based on current evidence.
Answer 2 is incorrect. 1% of you chose this answer, “Diet sodas are completely safe, so there’s no reason to change your intake.” Although NNS are considered safe by the FDA, the ADA recommends moderation. It supports reducing the total intake of sweetened beverages and those with NNS, encouraging water and unsweetened options where possible.
Answer 3 is correct. About 95% of respondents chose this – GREAT JOB! “While non-nutritive sweeteners are FDA-approved, let’s discuss your current intake, concerns, and whether unsweetened beverages may be a better option.” The 2025 ADA Standards of Care support a person-centered approach and recognize that FDA-approved non-nutritive sweeteners (NNS) are safe when used in moderation. This answer allows for a discussion tailored to Sam’s health goals, type of sweetener consumed and specific concerns. While water is the preferred beverage, using NNS to replace sugar-sweetened drinks may be an option to reduce overall calorie and carbohydrate intake.
Finally, Answer 4 is incorrect. 1% chose this answer, “Switch to natural sugars like honey or agave syrup since they are healthier than artificial sweeteners.” Natural sugars like honey and agave, although considered natural, are a form of added sugar that can negatively affect blood glucose. There is no specific guidance for the amount of added sugar within the diet, but the ADA Standards of Care recommends minimizing all forms of added sugar while also considering an individual’s nutrition plan.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live on July 24th, 2025, at 11:30 am PST to watch our brand new webinar, Beyond Blood Glucose: Empowering Health Through a Holistic Lens by Nick Kundrat, BS, CEP, CDCES, LMT
Despite the rise of cutting-edge diabetes technologies and therapeutics, many people with diabetes still struggle with fatigue, blood glucose swings, and burnout. Why? Because we’re often so focused on managing diabetes itself that we often forget to take care of the human being who lives with it.
Join Nick Kundrat, BS, CEP, CDCES, LMT and Integrative Health Practitioner, for an engaging webinar where he simplifies the often-misunderstood world of holistic health. You’ll learn practical, accessible strategies to begin thinking more holistically and discover simple, effective tools that enhance conventional care and empower people with diabetes to thrive—physically, emotionally, and spiritually.
Drawing from over two decades of lived experience with type 1 diabetes and years of supporting clients in both clinical and holistic settings, Nick offers a unique perspective on diabetes care focused on the whole person. Through reconnecting with the foundational elements of health, which are often overlooked in conventional diabetes care, Nick aims to equip you with actionable strategies to help people with diabetes restore their energy, support their bodies, and thrive beyond diabetes.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on CGM Timing Post-T1D Diagnosis: ADA 2025. 95% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JT, a 17-year-old recently hospitalized with a new diagnosis of type 1 diabetes, is using
Multiple Daily Injections (MDI) therapy. JT uses fingerstick blood glucose monitoring but
wants to move to a CGM. JT’s mother wants to know how long fingerstick monitoring must
be used before a CGM can be started. According to the ADA 2025 Standards of Care, when
can a CGM be initiated after a type 1 diabetes diagnosis?
Answer Choices:
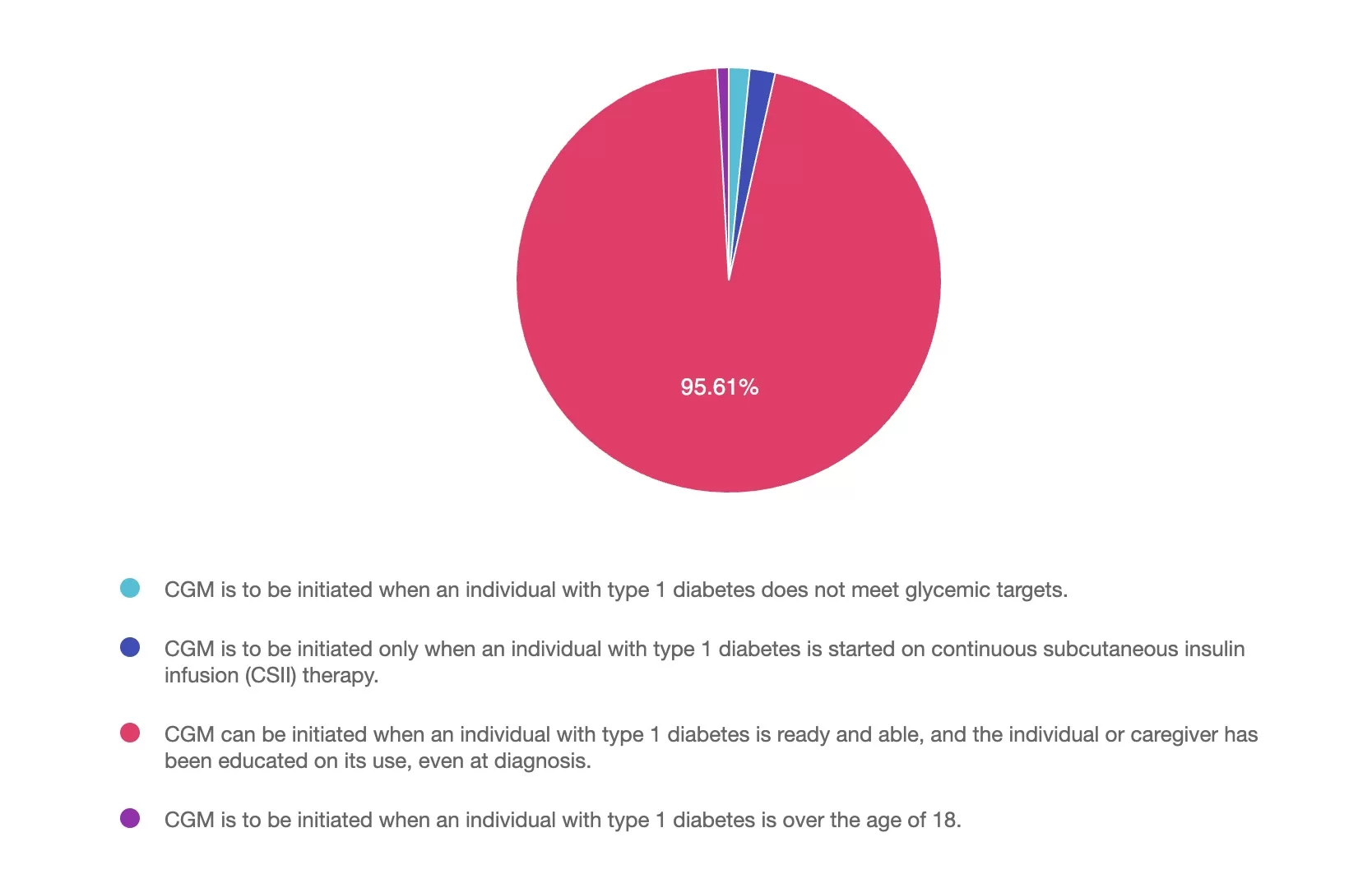
Answer 1 is incorrect. 1% chose this answer, “CGM is to be initiated when an individual with type 1 diabetes does not meet glycemic targets”. Since CGM is not used only for those with elevated glucose levels, this is not the best answer.
Answer 2 is incorrect. 1% of you chose this answer, “CGM is to be initiated only when an individual with type 1 diabetes is started on continuous subcutaneous insulin infusion (CSII) therapy”. Actually, CGM technology can be used with or without CSII (either standard pump or AID systems).
Answer 3 is correct. About 95% of respondents chose this, “CGM can be initiated when an individual with type 1 diabetes is ready and able, and the individual or caregiver has been educated on its use, even at diagnosis.” GREAT JOB! According to the American Diabetes Association 2025 Standards of Care, CGM technology can be initiated in any person living with diabetes on insulin therapy as early as diagnosis. The diabetes education specialist will use an individualized approach in choosing the most appropriate CGM technology and educating the individual and caregiver on how to use it. “
Finally, Answer 4 is incorrect. 1% chose this answer, “CGM is to be initiated when an individual with type 1 diabetes is over the age of 18.” According to the ADA 2025 Standards of Care, CGM technology should be offered to any adult or youth using insulin therapy. Some CGM devices are approved for use in the pediatric population (refer to each specific CGM for approval for use in children).
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Course Overview:
This course covers updated care goals and guidelines for children with type 1 or type 2 diabetes. Topics include clinical presentation, developmentally appropriate care, complication prevention, and family support.
Learn anytime, anywhere with 1-year access. Each course includes a video, podcast, practice test, and resources.
Objectives:
Identify care goals for kids with Type 1 and Type 2 diabetes
Outline strategies to prevent complications
Emphasize positive psychosocial support
Learning Outcome:
Gain a thorough understanding of individualized care and standards for pediatric diabetes management.
Buy individually for or get the full Level 2 Bundle and save 45% (discount applied). Don’t worry if you cannot attend, the course includes access to the recording for one year!
All hours earned count toward your CDCES Accreditation Information