
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | What Stage of Change?
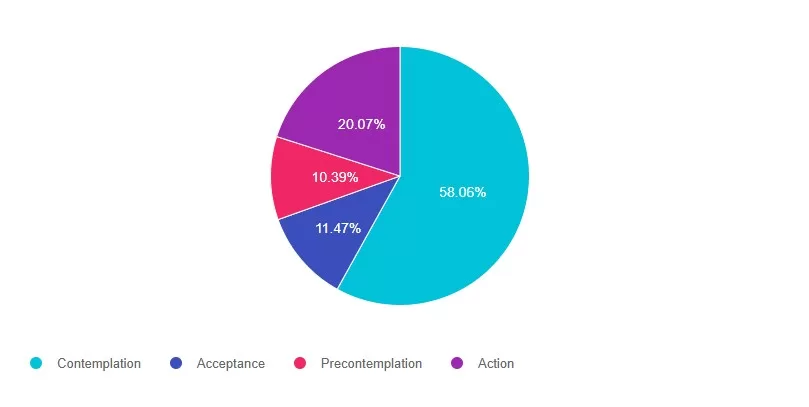
For last week’s practice question, we quizzed participants on What Stage of Change? 58% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

BT was started on a GLP-1 and is losing weight. BT has read articles about the importance of strength training to maintain muscle. They ask you questions about whether using weights or resistance bands is better.
According to the transtheoretical model, what stage of change is BT in?
Answer Choices:
- Contemplation
- Acceptance
- Precontemplation
- Action
Getting to the Best Answer
Answer 1 is correct. 58% chose this answer, “Contemplation.” GREAT JOB! When people are in contemplation stage, they are aware of the need for change and are actively considering making a change within the next six months. They are weighing the pros and cons of changing their behavior. In this situation BT is contemplating two different approaches to strengthening exercises,
Answer 2 is incorrect. 11% of you chose this answer, “Acceptance.” Even though BT may be accepting the need to get active, acceptance is not one of the stages in the transtheoretical model. This was one of those juicy answers.: -)
Answer 3 is incorrect. About 10% of respondents chose this, “Precontemplation.” This answer is tempting, but in precontemplation, individuals are not yet considering changing behavior. They may be unaware of the need for change or may have a resistant attitude toward it. BT wants to increase activity, but is choosing between two strength training options.
Finally, Answer 4 is incorrect. 20% chose this answer, “Action.” This person is not quite at the action stage. Action is when Individuals are actively modifying behavior, implementing plans, and making observable changes in their behavior, environment, or lifestyle.
Watch our FREE webinar, Behavior Change Made Easy. Register Here >>
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us for our upcoming Tech Data Toolkit Webinar!
Join us live on May 8th & May 15th!
Session 1 – May 8th
with Beverly Thomassian at 11:30am to 12:30pm PST
Session 2 – May 15th
with Dr. Diana Isaacs at 11:30am to 2:30pm PST
Gain confidence in interpreting Glucose Profile Report (AGP) & CGM data using a person-centered approach!
If you are preparing for certification exams or want to up your game using CGM data to improve outcomes, this course is for you.
We still have room available for the May 8th kick off date.
With diabetes technology entering all aspects of diabetes care, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience. Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Coach Beverly will build on Dr. Isaacss’ presentation. She will expand the focus to include steps to collaborate with the person with diabetes. Using a case study approach, she will provide strategies to integrate the AGP with person-centered care that empowers individuals to experience increased confidence in their diabetes self-management.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments with a person-centered approach.
Topics include:
Review CGM key metrics and individualize time in-range goals.
Learn how to recognize patterns with the AGP report efficiently.
Recommend lifestyle and medication adjustments based on CGM data.
Utilize the AGP report coupled with a person centered approach when meeting with a person with diabetes.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Sleep and ADA Recommendations
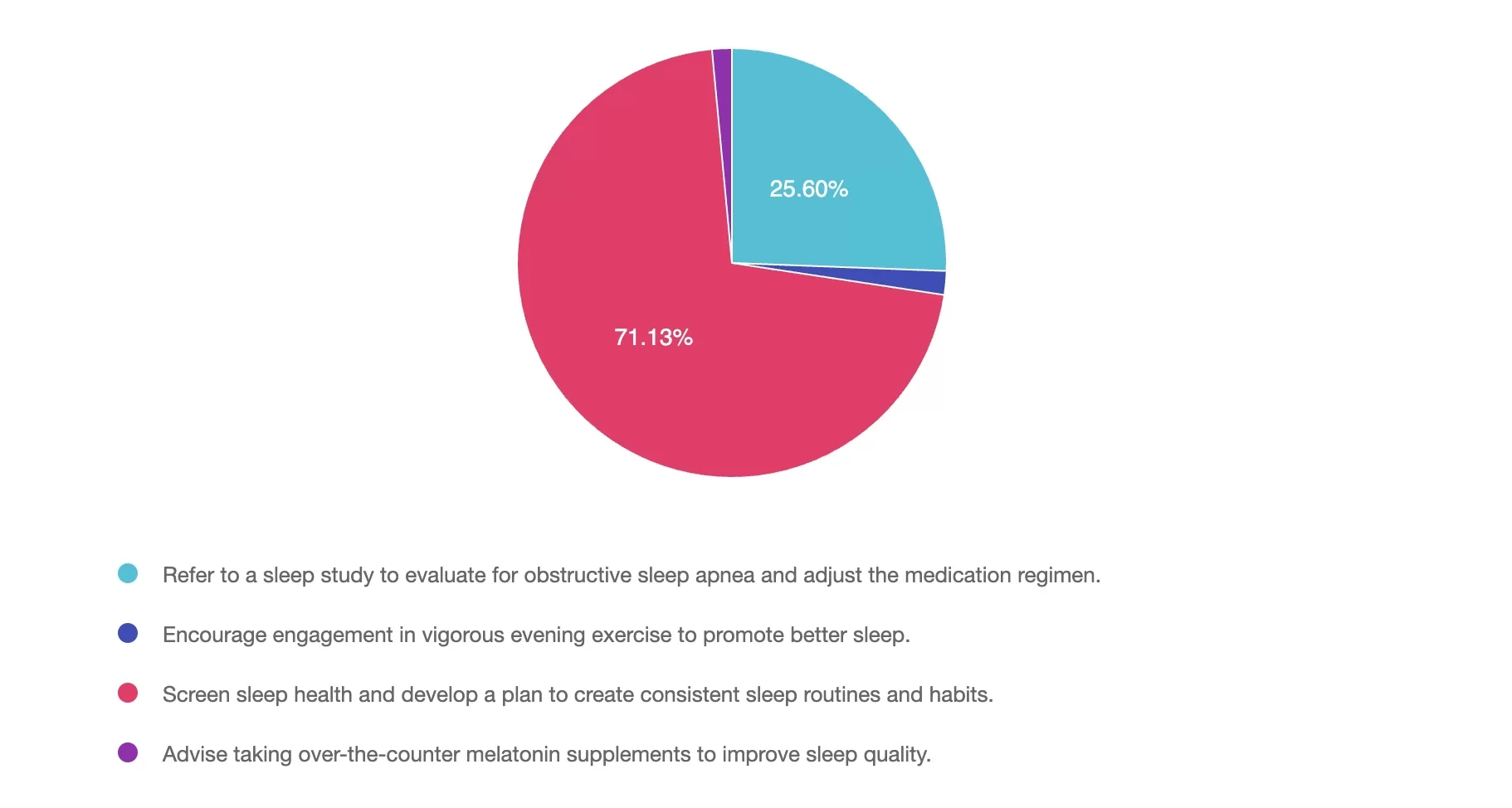
For last week’s practice question, we quizzed participants on Sleep and ADA Recommendations. 71% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
A 62-year-old with type 1 diabetes presents for their follow-up visit. They report struggling with fatigue, poor sleep quality, and difficulty with glucose management despite taking medications as prescribed. Upon review, you find their A1C is 7.6%, and their average nightly sleep duration is 4.5-6 hours per night.
Based on the 2025 ADA Standards of Care, which of the following interventions would be the most appropriate next step to address sleep and glucose management?
Answer Choices:
- Refer to a sleep study to evaluate for obstructive sleep apnea and adjust the medication regimen.
- Encourage engagement in vigorous evening exercise to promote better sleep.
- Screen sleep health and develop a plan to create consistent sleep routines and habits.
- Advise taking over-the-counter melatonin supplements to improve sleep quality.
Getting to the Best Answer
Answer 1 is incorrect. 25% chose this answer, “Refer to a sleep study to evaluate for obstructive sleep apnea and adjust the medication regimen.” While a sleep study may be recommended for suspected sleep disorders, such as sleep apnea (for example: loud snoring, daytime sleepiness), the first step should be a comprehensive sleep health screening. This screening helps identify potential causes of poor sleep, including symptoms of sleep disorders, disruptions from diabetes management (for example: nocturnal hypoglycemia, frequent urination), or anxiety about sleep. Based on the findings, appropriate treatment modifications and referrals can then be made.
Answer 2 is incorrect. 1% of you chose this answer, “Encourage engagement in vigorous evening exercise to promote better sleep.” Although exercise can improve sleep quality, vigorous evening exercise may increase alertness, making it harder to fall asleep. In individuals with type 1 diabetes, this timing of exercise can also increase the risk of nighttime hypoglycemia, further disrupting sleep. Before recommending vigorous exercise, it’s important to first assess sleep habits to better understand the underlying causes of poor sleep quality.
Answer 3 is correct. About 71% of respondents chose the BEST ANSWER – GREAT JOB! “Screen sleep health and develop a plan to create consistent sleep routines and habits.” The 2025 ADA Standards emphasize the importance of screening for sleep health and providing guidance on sleep-promoting routines and habits. Based on screening results, referrals to sleep medicine programs, adjustment in medications or behavioral therapy programs are a few that may be appropriate. Prioritizing improved sleep duration and consistency can support better glucose management, reduce fatigue, and enhance overall well-being.
Finally, Answer 4 is incorrect. 1% chose this answer, “Advise taking over-the-counter melatonin supplements to improve sleep quality.” While melatonin may be helpful for certain sleep disorders, its use should be evaluated on a case-by-case basis and is not recommended within the ADA 2025 Standards of Care. The first-line recommendation should focus on screening to better determine appropriate actions.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to Prepare for Exam Certification?
Join our Behavior Change Theories Made Easy FREE Webinar on April 22nd at 11:30am PST.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Remote Eye Screening Precautions
For last week’s practice question, we quizzed participants on Remote Eye Screening Precautions. 84% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Retinal photography with remote reading by experts has great potential to provide screening services in areas where qualified eye care professionals are not readily available.
However, in person exams are still necessary in which of the following scenarios?
Answer Choices:
- If the retinal photos are of optimal quality.
- If abnormalities are detected.
- Immediately after diagnosis of type 1 diabetes.
- For those on long term aspirin therapy.
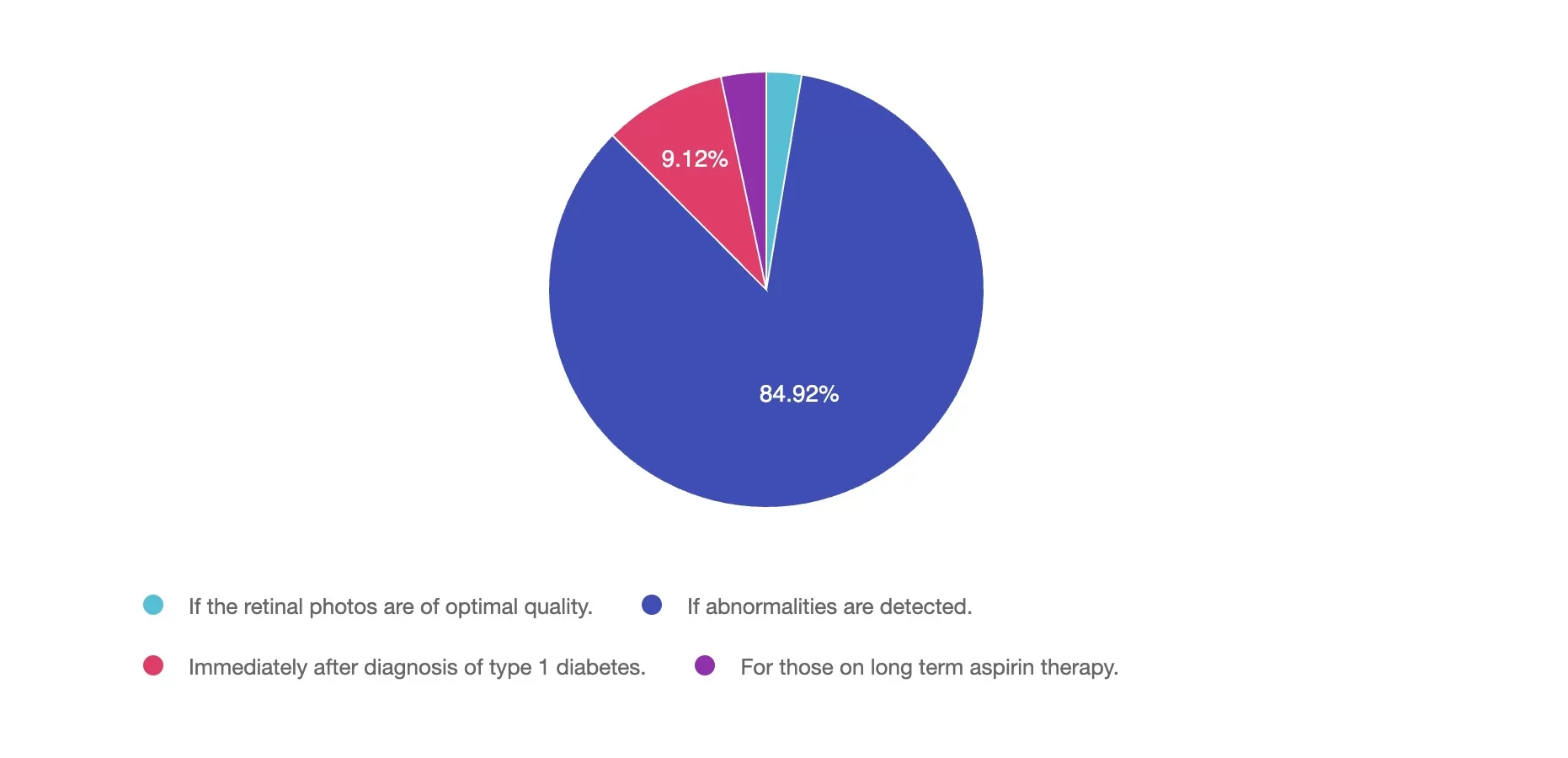
Getting to the Best Answer
Answer 1 is incorrect. 2% chose this answer, “If the retinal photos are of optimal quality.” If retinal photos of are of high quality and there are no detected abnormalities, the retinal photo is sufficient.
Answer 2 is correct. 84% of you chose this answer, “If abnormalities are detected.” YES, GREAT JOB. If the retinal photos detect any abnormalities, an in-person comprehensive eye exam is necessary.
Answer 3 is incorrect. About 9% of respondents chose this, “Immediately after diagnosis of type 1 diabetes.” People diagnosed with type 1 diabetes are not required to get an immediate eye exam. The ADA Standards state that people with new type 1 diabetes need an eye exam within 5 years.
Finally, Answer 4 is incorrect. 3% chose this answer, “For those on long term aspirin therapy.” Since aspirin therapy does not elevate the risk of eye disease, individuals taking aspirin can safely participate in remote eye exams without concern.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
It’s not too late to sign up and join us!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Who Benefits Most from Mindful Eating as a Primary Strategy?
For last week’s practice question, we quizzed participants on Who Benefits Most from Mindful Eating as a Primary Strategy? 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Mindful eating can support diabetes management in various ways.
For which of the following individuals would mindful eating be most effective as a primary strategy rather than a complementary approach?
Answer Choices:
- A 46-year-old male with type 1 diabetes on a fixed carbohydrate meal plan.
- A 30-year-old pregnant female recently diagnosed with gestational diabetes.
- A clinically underweight 77-year-old female with prediabetes and osteoporosis on a high-protein, high-calcium diet.
- A 28-year-old female with type 2 diabetes, a BMI of 35, and a history of disordered eating
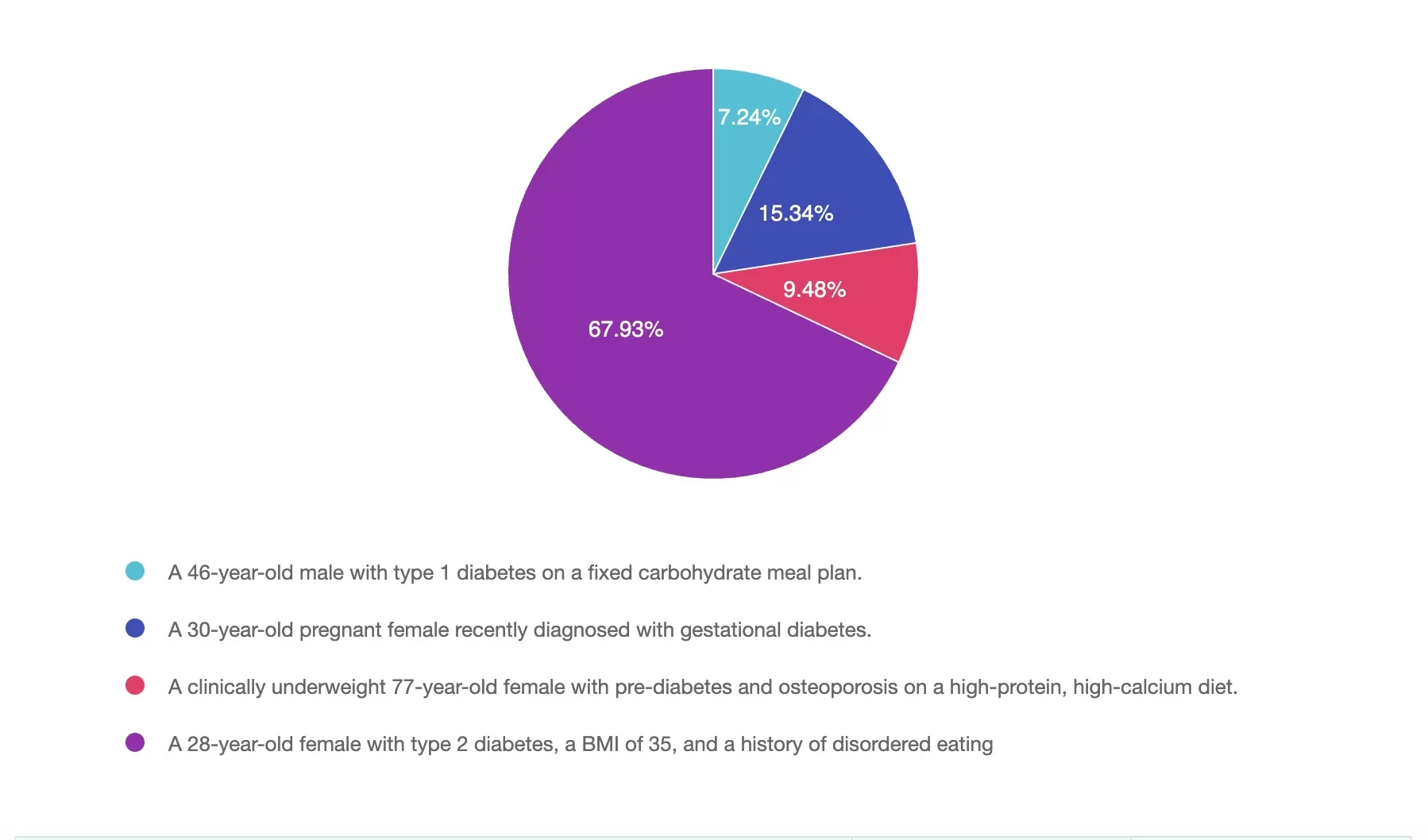
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Mindful eating is a flexible, non-restrictive approach that promotes awareness, self-regulation, and a healthier relationship with food. While many people with diabetes can benefit from mindful eating, individuals with a history of disordered eating often find it to be the most transformative strategy (Kristeller & Hallett, 1999; Miller et al., 2012; Mercado et al., 2021).
Answer 1 is incorrect. 7% chose this answer, “A 46-year-old male with type 1 diabetes on a fixed carbohydrate meal plan:
- Fixed-carb meal plans are essential for stabilizing blood sugar and matching insulin dosages.
- While mindful eating can support self-awareness and reduce mealtime stress, structured meal timing, and portioning remain the primary strategy.”
Answer 2 is incorrect. 15% of you chose this answer, “30-year-old pregnant female recently diagnosed with gestational diabetes:
- Gestational diabetes requires careful carbohydrate distribution and nutrient timing for optimal maternal and fetal health.
- Mindful eating may help reduce stress and support portion awareness, but medical nutrition therapy (MNT) takes priority for managing blood sugar levels during pregnancy.”
Answer 3 is incorrect. About 9% of respondents chose this, “A clinically underweight 77-year-old female with prediabetes and osteoporosis on a high-protein, high-calcium diet:
- While mindful eating can help this individual enhance food enjoyment and reduce mealtime stress, her primary concern is nutritional adequacy and weight gain.
- A structured, high-protein, high-calcium diet supports bone health, prevents muscle loss, and maintains energy balance.
- Encouraging mindful eating without ensuring sufficient caloric intake may not address the underlying need for increased nutrition.”
Finally, Answer 4 is correct. 67% chose this answer, “A 28-year-old female with type 2 diabetes, BMI 35, and a history of disordered eating:
- Mindful eating is particularly effective as a primary strategy for individuals with a history of emotional eating, binge eating, or restrictive dieting.
- It reduces anxiety around food, promotes a nonjudgmental approach to eating, and fosters long-term self-regulation (Miller et al., 2012; Kristeller et al., 2014).
- Studies show mindful eating lowers binge-eating episodes, improves self-efficacy, and helps individuals develop a positive relationship with food (Harvard T.H. Chan School of Public Health, 2024; Mercado et al., 2021).”
Why is #4 the correct answer?
Mindful eating is most beneficial as a primary approach for individuals who have struggled with disordered eating patterns. Unlike restrictive diets, it provides a structured yet flexible way to reconnect with hunger cues, reduce emotional eating, and develop sustainable habits.
We hope this week’s rationale clarifies the diverse applications of mindful eating. Thank you for engaging with this question, and we look forward to more learning opportunities together!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
by Evgenia Evans, MS, RDN, CDCES
References
Aikens, J. E. (2012). Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care, 35(12), 2472–2478. https://doi.org/10.2337/dc12-0181
Forman, E. M., Shaw, J. A., Goldstein, S. P., Butryn, M. L., Martin, L. M., Meiran, N., Crosby, R. D., & Manasse, S. M. (2016). Mindful decision making and inhibitory control training as complementary means to decrease snack consumption. Appetite, 103, 176-183. https://doi.org/10.1016/j.appet.2016.04.014
Framson, C., Kristal, A. R., Schenk, J. M., Littman, A. J., Zeliadt, S., & Benitez, D. (2009). Development and validation of the Mindful Eating Questionnaire. Journal of the American Dietetic Association, 109(8), 1439–1444. https://doi.org/10.1016/j.jada.2009.05.006
Fredrickson, B. L. (2004). The broaden-and-build theory of positive emotions. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 359(1449), 1367–1377. https://doi.org/10.1098/rstb.2004.1512
Garland, E. L., Fredrickson, B. L., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. https://doi.org/10.1016/j.cpr.2010.03.002
Harvard T.H. Chan School of Public Health. (2024, November 7). Mindful Eating. The Nutrition Source. https://nutritionsource.hsph.harvard.edu/mindful-eating/
Kabat-Zinn, J. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Random House Publishing Group.
Kristeller, J. L., & Hallett, C. B. (1999). An exploratory study of a meditation-based intervention for binge eating disorder. Journal of Health Psychology, 4(3), 357–363. https://doi.org/10.1177/135910539900400305
Kristeller, J. L., Wolever, R. Q., & Sheets, V. (2014). Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial. Mindfulness, 5(3), 282–297. https://doi.org/10.1007/s12671-012-0179-1
Mercado, C., Marasigan, K., Cardona, J., & Ko, E. (2021). Mindfulness-based interventions for emotional eating and binge eating in adults: A meta-analysis. Appetite, 164, 105265. https://pmc.ncbi.nlm.nih.gov/articles/PMC11893636/
Miller, C. K. (2017). Mindful eating with diabetes. Diabetes Spectrum, 30(2), 89–94. https://doi.org/10.2337/ds16-0040
Miller, C. K., Kristeller, J. L., Headings, A., Nagaraja, H., & Miser, W. F. (2012). Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A pilot study. Journal of the Academy of Nutrition and Dietetics, 112(11), 1835–1842. https://doi.org/10.1016/j.jand.2012.07.036
Miller, C. K., Kristeller, J. L., Headings, A., & Nagaraja, H. (2014). Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Education & Behavior, 41(2), 145–154. https://doi.org/10.1177/1090198113493092
Nicolucci, A., Kovacs Burns, K., Holt, R. I. G., Comaschi, M., Hermanns, N., Ishii, H., Kokoszka, A., Pouwer, F., Skovlund, S. E., Stuckey, H., Tarkun, I., Vallis, M., Wens, J., & Peyrot, M. (2013). Diabetes Attitudes, Wishes and Needs second study (DAWN2™): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabetic Medicine, 30(7), 767–777. https://doi.org/10.1111/dme.12245
Nelson, J. B. (2017). Mindful eating: The art of presence while you eat. Diabetes Spectrum, 30(3), 171–174. https://doi.org/10.2337/ds17-0015
Want to learn more about this question?
Enroll in our upcoming webinar led by Evgeniya Evans, MS, RDN, CDCES
Mindful Eating for Successful Diabetes Management
Join us live on June 11, 2025, at 11:30 am PST
This engaging and practical webinar, developed by Evgeniya Evans, MS, RDN, CDCES, a positive psychology practitioner, is tailored explicitly for healthcare professionals including dietitians, diabetes care specialists, and providers.
Using evidence-based strategies, participants will gain a deeper understanding of the benefits of incorporating mindfulness into the eating experience, including enhanced glycemic management, improved emotional well-being, and healthier eating behaviors. The webinar includes an overview of mindfulness and mindful eating strategies, such as engaging all five senses, recognizing hunger cues, addressing cravings, and using practical tools to create supportive eating environments.

Participants will also learn how to adapt these approaches to diverse populations and the unique needs of individuals. Join us to deepen your expertise, participate in insightful discussions, and empower individuals to cultivate sustainable, positive relationships with food while achieving long-term health goals.
Course topics:
- Introduction to the concept and benefits of mindful eating for individuals with diabetes
- Overview of key strategies for mindful eating
- Practical tools for incorporating mindful eating into professional practice (of Diabetes Educators)
- Cultural and individual adaptations of the mindful eating approach
Instructor: Evgeniya Evans, MS, RDN, CDCES

Evgeniya Evans, MAPP, RDN, LDN, CDCES, specializes in chronic disease prevention, diabetes management, and women’s health. Her unique approach integrates mindfulness-based nutrition and positive psychology, creating transformative impacts on her patients’ health and well-being.
Evgeniya’s academic journey reflects her dedication to lifelong learning and her holistic understanding of nutrition and health. She began with four years of Sociology studies at Omsk State University in Russia, followed by earning a Bachelor of Science in Nutrition and Dietetics from the University of Illinois Chicago. She furthered her expertise with a master’s degree in Applied Positive Psychology from the University of Pennsylvania. This diverse educational foundation allows her to address the socio-psychological factors that influence dietary behaviors and deliver a well-rounded approach to patient care.
At Cook County Health’s Diabetes Clinic within the Endocrinology Department, Evgeniya provides medically tailored nutrition therapy and culturally sensitive counseling. She works with individuals from various socio-economic backgrounds, guiding them through their unique health challenges with compassion and precision. Her dedication to creating personalized, sustainable dietary strategies highlights her commitment to promoting long-term health and vitality for her patients.
In addition to her clinical practice, Evgeniya is a passionate educator. She teaches several classes at her clinic, including Pillars of Diabetes Management with Lifestyle, Nutrition for Health and Vitality, and The Art of Mindful Eating. Her emphasis on education underscores her belief in the transformative power of fostering a healthy, enjoyable lifestyle supported by mindful eating and a positive mindset.
Evgeniya envisions a world where individuals are free from the struggles of dieting and food-related shame. She dreams of a future where no one feels deprecated by their appearance or food choices, and everyone enjoys the vitality and health to pursue their dreams. She is devoted to fostering vibrant, authentic lives where cooking, eating, and sharing meals with loved ones are sources of joy, love, and positive connection.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Weight-Inclusive Diabetes Care
For last week’s practice question, we quizzed participants on weight inclusive diabetes care. 85% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
How does weight-inclusive care improve clinical outcomes in diabetes management?
Answer Choices:
- It eliminates weight stigma, leading to enhanced engagement and collaboration.
- It reduces A1c only in those who experience weight loss.
- It leads to greater weight loss, which is the key factor in diabetes management.
- It removes the need for lifestyle modifications and focuses only on medication.
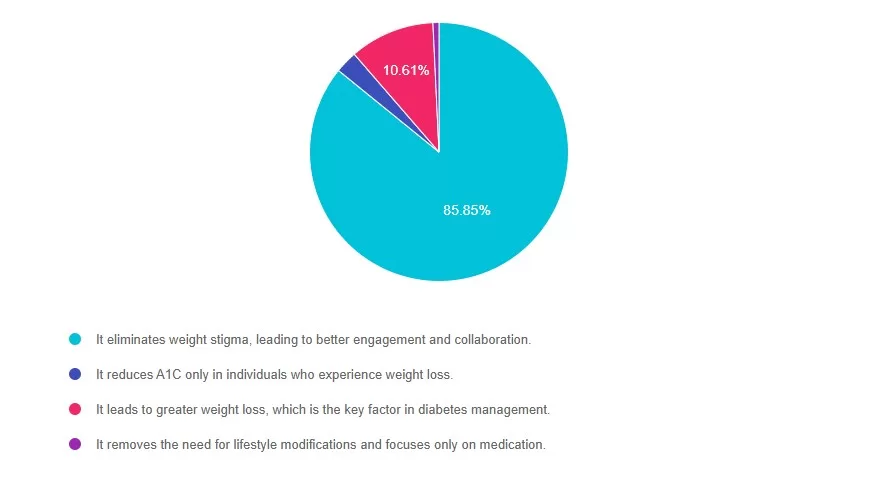
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 85% chose this answer, “It eliminates weight stigma, leading to better patient engagement and adherence to treatment.” Studies suggest that weight stigma in healthcare leads to worse health outcomes, as patients in larger bodies are more likely to delay care or avoid medical visits altogether due to fear of judgment. A weight-inclusive approach fosters trust and encourages long-term behavior change, which ultimately improves glycemic control and patient well-being.
Answer 2 is incorrect. 2% of you chose this answer, “It reduces A1c only in patients who experience weight loss.” Research has consistently shown that health-promoting behaviors—like increasing fiber intake and engaging in regular movement—can improve blood sugar levels independent of weight loss.
Answer 3 is incorrect. About 10% of respondents chose this, “It leads to greater weight loss, which is the key factor in diabetes management.” While weight loss is often associated with improved health markers, the key drivers of better outcomes in diabetes care are sustainable habits, not weight change itself. Many individuals improve their metabolic health and blood sugar levels through consistent health behaviors, regardless of changes in body size. The focus should be on sustainable, evidence-based interventions rather than weight as an outcome.
Finally, Answer 4 is incorrect. 1% chose this answer, “It removes the need for lifestyle modifications and focuses only on medication.” Medications like metformin and GLP-1 receptor agonists are valuable tools in diabetes management, but they work best when combined with behavior-based interventions. A weight-inclusive model does not dismiss the role of medication; rather, it ensures that patients receive comprehensive, stigma-free care that includes sustainable lifestyle adjustments.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
by Jessica Jones, MS, RD, CDCES, CEO and Co-founder of Diabetes Digital, a virtual nutrition counseling platform for people with diabetes and prediabetes
Want to learn more about this question?
Weight-Inclusive Diabetes Care: Turning Compassion into Practical Tools
by Jessica Jones, MS, RD, CDCES
This session provides healthcare providers with actionable strategies to integrate weight-inclusive care into diabetes management practices, focusing on improving outcomes through respect for body diversity and individual autonomy. Weight stigma is a well-documented barrier to effective care, contributing to poorer glycemic control, disordered eating, and care avoidance. By shifting from a weight-focused approach to one aligned with Health at Every Size (HAES®), providers can foster trust, enhance participant engagement, and support sustainable health behaviors.

Jessica Jones, MS, RD, CDCES, will share evidence-based insights on mitigating weight stigma and applying HAES-aligned strategies in practice. Participants will learn how to build rapport, set realistic nutrition goals, and implement interventions that prioritize blood sugar management, joyful movement, and intuitive eating. This session equips providers with tools to deliver compassionate, person-centered care, improving both clinical outcomes and the provider-participant relationship..
Course topics:
- Foundations of weight-inclusive diabetes care: overview and evidence
- Shifting perspectives: building trust and redefining success
- Practical tools for sustainable blood sugar management
Instructor: Jessica Jones, MS, RD, CDCES, CEO and Co-founder of Diabetes Digital

Jessica Jones, MS, RDN, CDCES, is a nationally recognized Registered Dietitian Nutritionist and Certified Diabetes Care & Education Specialist committed to making nutrition education accessible to everyone. As the CEO and co-founder of Diabetes Digital, Jessica has been pivotal in developing an innovative telehealth platform that provides tailored nutrition counseling for individuals with diabetes and prediabetes. Additionally, she co-hosts the Diabetes Digital Podcast, engaging listeners with thoughtful conversations on managing diabetes.
With over a decade of clinical experience, Jessica has contributed significantly to the field through her co-authorship of the “28-Day Plant-Powered Health Reboot” cookbook and “A Diabetes Guide to Enjoying the Foods of the World.” She also wrote the Diabetes Chapter for the Food and Nutrition Care Manual Textbook and regularly shares her insights as a columnist for SELF magazine.
As a co-founder of Food Heaven, an online platform and podcast with more than 5 million downloads, she offers essential resources on cooking, intuitive eating, and embracing body respect. Jessica’s contributions have been celebrated in prominent publications, including Oprah Magazine, Women’s Health, The Food Network Magazine, SELF Magazine, the Huffington Post, and Bon Appetit. She lives in Sacramento, CA with her husband and “spirited” Maltese Shih Tzu puppy, Poppy.
Rationale of the Week | Triglyceride Management
For last week’s practice question, we quizzed participants on Triglyceride Management. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
JT is 58-years-old and has type 2 diabetes, hypertension, and BMI is 32 kg/m². Medications include metformin, lisinopril, and atorvastatin. Diet intake includes frequent highly processed foods, sugary beverages, no alcohol consumption, and minimal physical activity. Recent lab work indicates A1c: 7.2%, LDL:82 mg/dL, HDL: 38 mg/dL, triglycerides: 345 mg/dL, AST/ALT were both normal.
Given these findings, what is the recommended first-line intervention for managing his elevated triglycerides according to the 2025 ADA Standards of Care?
Answer Choices:
- Omega-3 fatty acids
- Lifestyle modification (nutrition, physical activity, and weight management)
- Start a Statin
- Start a Fenofibrate
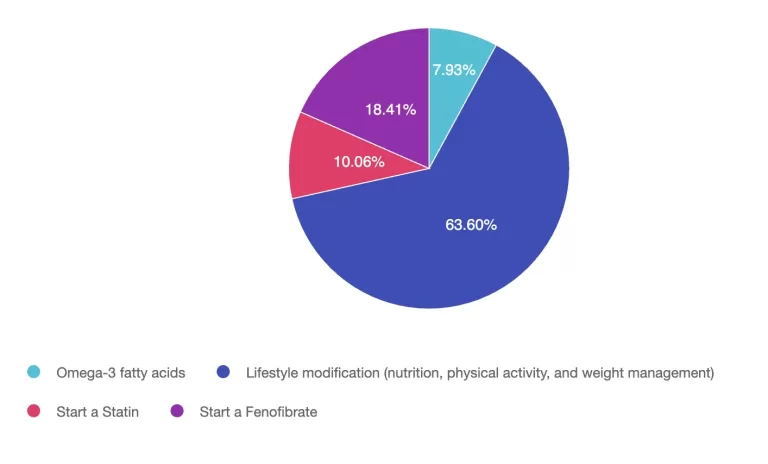

Getting to the Best Answer
Answer 1 is incorrect. 7.93% chose this answer, “Omega-3 fatty acid.” Icosapent ethyl, a refined omega-3 fatty acid, is typically considered when triglycerides ≥ 500 mg/dL to help lower levels and reduce pancreatitis risk, but they are not typically first-line for triglycerides at 345 mg/dL. For individuals with known cardiovascular risk consideration of additional of Icosapent ethyl could be added after maximizing statin therapy.
Answer 2 is correct. 63% of you chose this answer, “Lifestyle modification (nutrition, physical activity, and weight management.” The first-line recommendation for triglycerides 150-499 mg/dL is lifestyle modification. This may include dietary modifications (types of fats, reducing added sugars, refined carbohydrates, and alcohol), increasing physical activity, and weight loss, if applicable. If triglycerides remain elevated or reach ≥ 500 mg/dL, pharmacologic treatment such as icosapent ethyl or fibrates may be considered to reduce the risk of pancreatitis.
Answer 3 is incorrect. About 10% of respondents chose this, “Start a Statin.” JT is already taking a statin, atorvastatin. Although we can consider maximizing statin therapy as LDL is above 70 mg/dl, this is not the best answer. Statins may have a modest triglyceride-lowering effect, they are not the primary treatment for hypertriglyceridemia at this level.
Finally, Answer 4 is incorrect. 18.41% chose this answer, “Start a Fenofibrate.” Fenofibrate are typically recommended when triglycerides elevate greater than 500 mg/dL to reduce pancreatitis risk and addition could be
considered if lifestyle therapy does not indicate benefit.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | Best approach: Fasting During Ramadan
For last week’s practice question, we quizzed participants on best approach: fasting during Ramadan . 74% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JL observes Ramadan and fasts from sunrise to sunset. JL has type 2 diabetes and usually takes 4 units of bolus insulin three times a day with meals and 10 units of glargine (Rezvoglar) at bedtime.
What would be the best recommendation for JL?
Answer Choices:
- See if JL can get a note from your doctor to allow eating during the day.
- Take bolus insulin when JL eats a meal.
- Monitor urine ketones at least twice a day.
- Switch glargine to degludec to decrease risk of hypoglycemia.
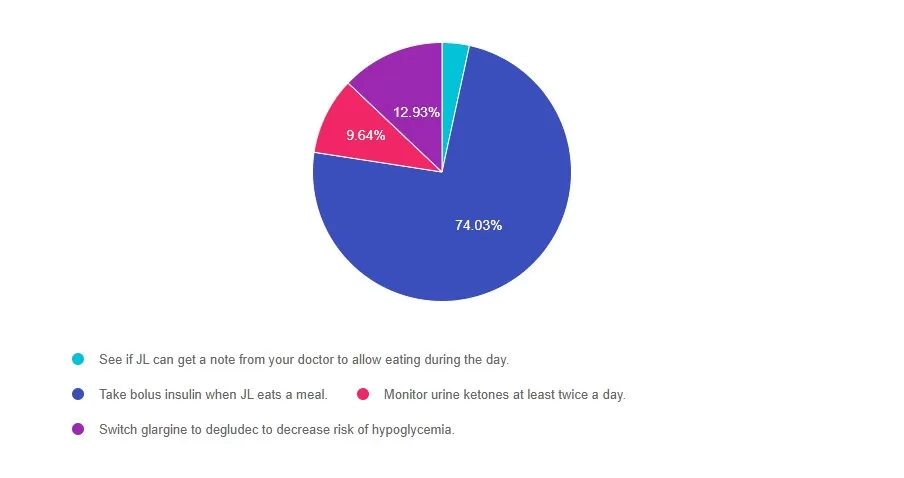
Getting to the Best Answer
Answer 1 is incorrect. 3% chose this answer, See if JL can get a note from your doctor to allow eating during the day. With careful planning and insulin adjustments, we can honor JL’s religious fast and cultural beliefs.
Answer 2 is correct. 76% of you chose this answer, Take bolus insulin when JL eats a meal. Yes, this is the BEST answer. If the basal insulin is dosed correctly, it won’t cause hypoglycemia while fasting. JL can hold bolus insulin during fasting, and take bolus insulin when eating.
Answer 3 is incorrect. About 9% of respondents chose this, Monitor urine ketones at least twice a day. There is no need to monitor ketones, since JL will be taking basal insulin daily and bolus insulin with meals, which will prevent ketosis.
Finally, Answer 4 is incorrect. 12% chose this answer, Switch glargine to degludec to decrease risk of hypoglycemia. There is no need to switch basal insulins. JL can stay on glargine, recognizing that it may need to be adjusted.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | Based on ADA Standards, what is next med addition?
For last week’s practice question, we quizzed participants on ADA Standards & what is next med addition? 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has type 2 diabetes and takes Metformin 1000mg BID and sitagliptin (Januvia), A1C 8.1%. GFR 47, UACR 158mg/g. Recent diagnosis of congestive heart failure. These are the medications their insurance covers.
Of the following medications, which addition would most benefit JR?
Answer Choices:
- glipizide (Glucotrol)
- pioglitazone (Actos)
- semaglutide (Ozempic)
- dapagliflozin (Farxiga)
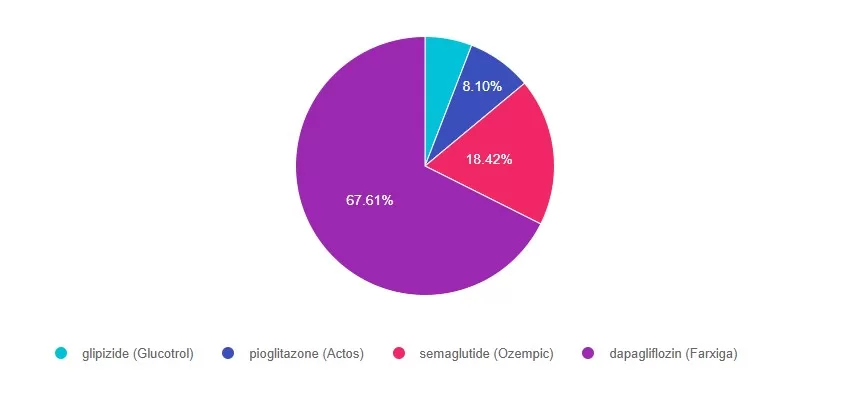
Getting to the Best Answer
For a helpful reference, please see our PocketCards for more information.
Answer 1 is incorrect. 5% chose this answer, “Glipizide (Glucotrol)”. Even though glipizide would help lower blood glucose, considering JL’s CHF and worsening kidney function, it is not the best choice.
Answer 2 is incorrect. 8% of you chose this answer, “pioglitazone (Actos)”. Even though pioglitazone would help lower blood glucose, considering JL’s CHF and worsening kidney function, it is not the best choice.
Answer 3 is incorrect. About 18% of respondents chose this, “Semaglutide (Ozempic)”. Even though semaglutide would help lower blood glucose and would address worsening kidney function, considering JL’s CHF and worsening kidney function, it is not the best choice.
Finally, Answer 4 is correct. 67% chose this answer, “Dapagliflozin (Farxiga)”. YES, GREAT JOB. Dapagliflozin is a SGLT-2i that will help lower blood glucose, address worsening kidney function and CHF. Plus, it is covered by insurance. Considering JL’s health profile, it is the best choice.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over






