
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
For last week’s practice question, we quizzed participants on DKA Prevention After T1D Diagnosis. 52% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: A 10-year-old child with newly diagnosed type 1 diabetes is being discharged from the hospital. Which of the following components is most critical to include in the initial outpatient diabetes management plan to reduce the risk of diabetic ketoacidosis (DKA) and hospital readmission?
Answer Choices:
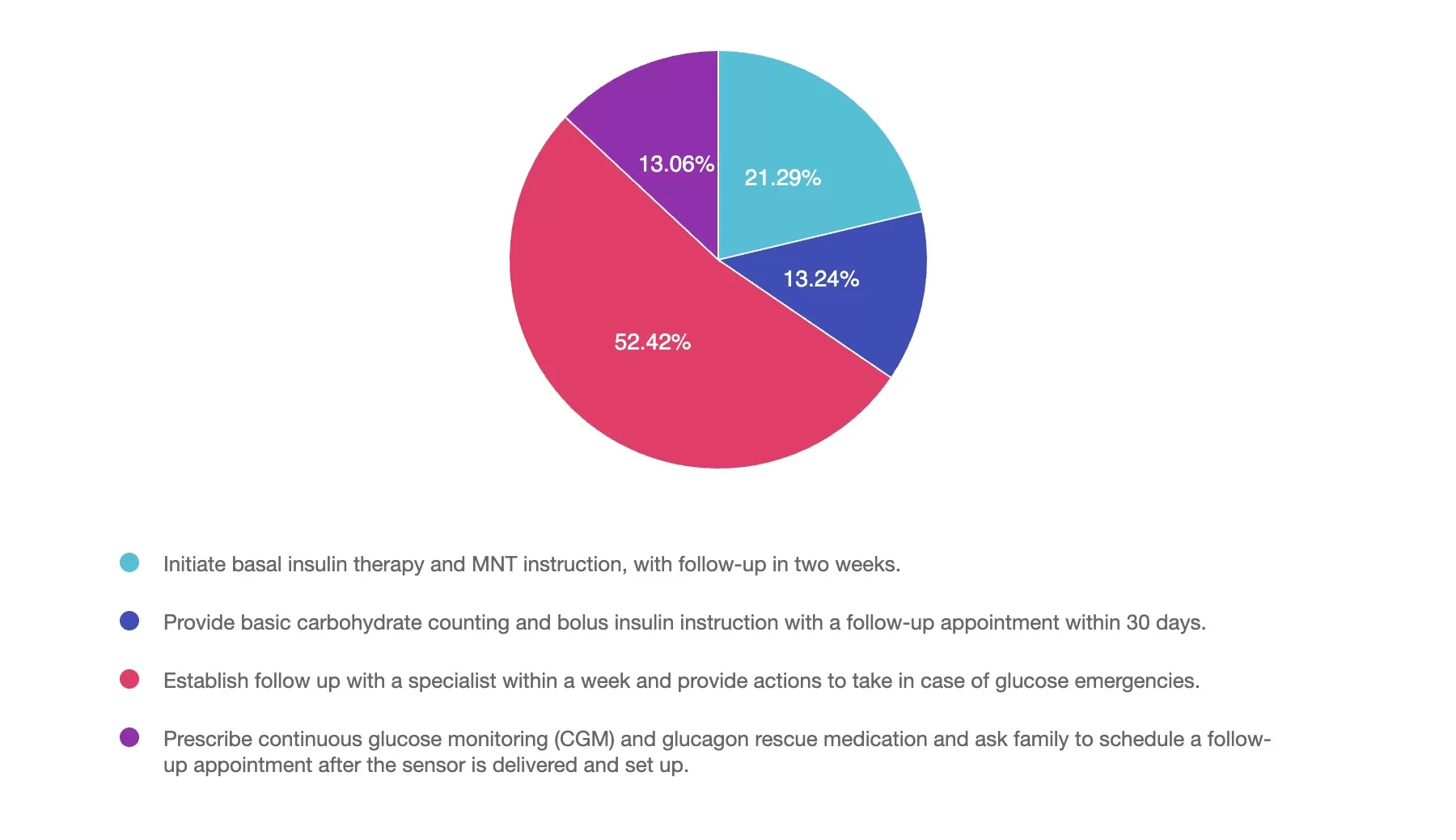
Answer 1 is incorrect. 21% chose this answer, “Initiate basal insulin therapy and MNT instruction, with follow-up in two weeks.” Basal insulin alone is insufficient; children require both basal and bolus insulin to mimic physiologic insulin needs and prevent DKA.
Answer 2 is incorrect. 13% of you chose this answer, “Provide basic carbohydrate counting and bolus insulin instruction with a follow-up appointment within 30 days.” Delayed follow-up increases the risk of complications. Carbohydrate counting and bolus insulin are important, but must be paired with timely, ongoing support.
Answer 3 is correct. About 52% of respondents chose this, “Establish follow up with a specialist within a week and provide actions to take in case of glucose emergencies.” Early involvement of a diabetes specialist and problem solving in case of glucose crises, significantly reduce the risk of DKA and readmission. Frequent follow-up in the first week is associated with better outcomes.
Finally, Answer 4 is incorrect. 13% chose this answer, “Prescribe continuous glucose monitoring (CGM) and glucagon rescue medication and ask family to schedule a follow-up appointment after the sensor is delivered and set up.” While CGM is valuable, delaying education and clinical engagement is risky; immediate education and care planning are essential.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Join us live on June 11, 2025, at 11:30 am PST to watch our brand new webinar, Mindful Eating for Successful Diabetes Management by Evgeniya Evans, MS, RDN, CDCES
This engaging and practical webinar, developed by Evgeniya Evans, MS, RDN, CDCES, a positive psychology practitioner, is tailored explicitly for healthcare professionals including dietitians, diabetes care specialists, and providers.
Using evidence-based strategies, participants will gain a deeper understanding of the benefits of incorporating mindfulness into the eating experience, including enhanced glycemic management, improved emotional well-being, and healthier eating behaviors. The webinar includes an overview of mindfulness and mindful eating strategies, such as engaging all five senses, recognizing hunger cues, addressing cravings, and using practical tools to create supportive eating environments.
Participants will also learn how to adapt these approaches to diverse populations and the unique needs of individuals. Join us to deepen your expertise, participate in insightful discussions, and empower individuals to cultivate sustainable, positive relationships with food while achieving long-term health goals.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on ADA 2025: Which MNT Statement Is False? 50% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: According to the 2025 ADA Standards of Care, which of the following statements about medical nutrition therapy (MNT) for adults with type 2 diabetes is NOT TRUE?
Answer Choices:
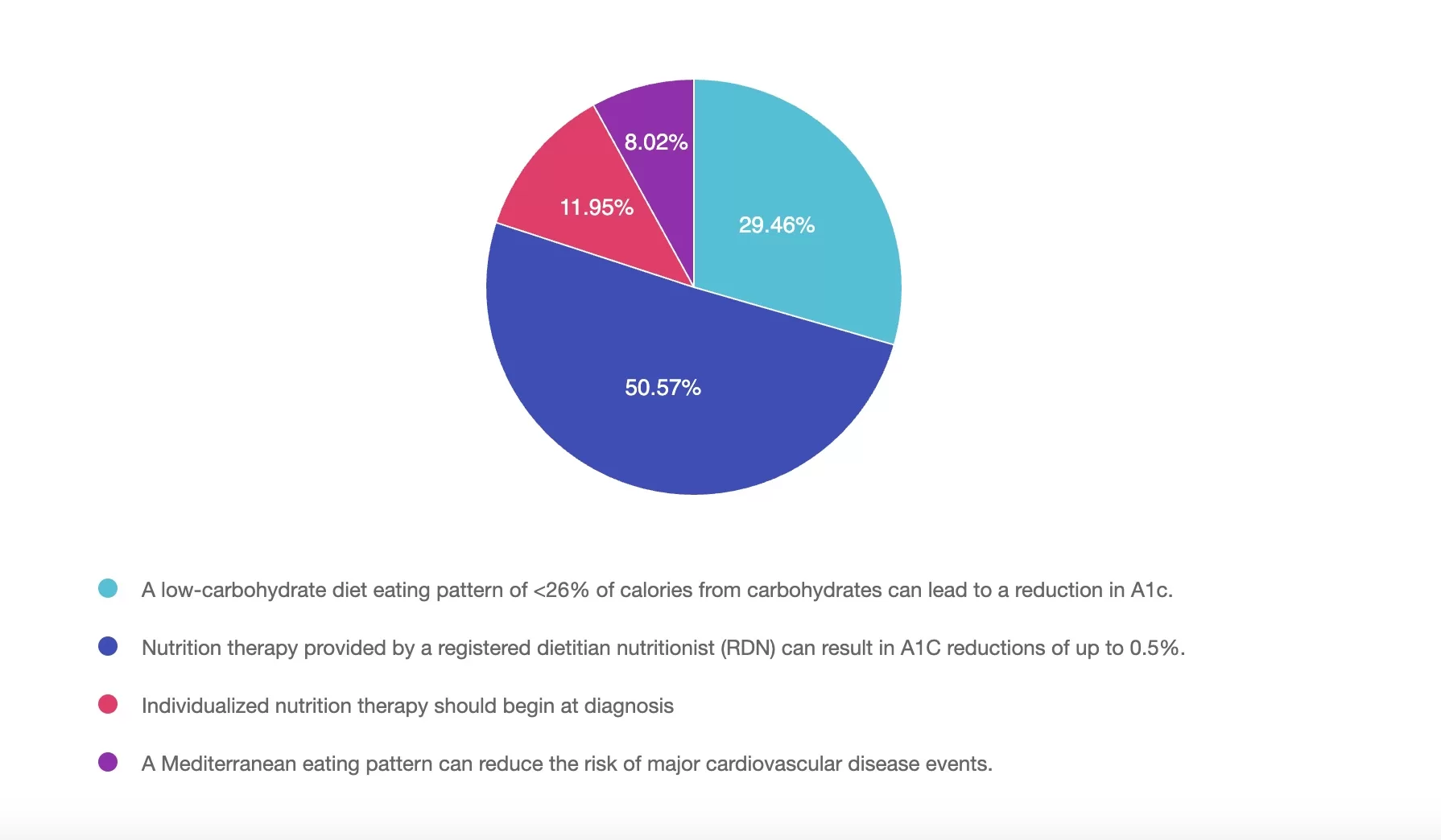
Answer 1 is incorrect. 29% chose this answer, “A low-carbohydrate diet eating pattern of <26% of calories from carbohydrates can lead to a reduction in A1c.” Low-carbohydrate eating patterns (defined as <26% of calories from carbohydrates) have been shown to lower A1C in adults with type 2 diabetes and are supported by the 2025 ADA Standards of Care as one of several individualized eating patterns.
Answer 2 is correct. 50% of you chose this answer, “Nutrition therapy provided by a registered dietitian nutritionist (RDN) can result in A1C reductions of up to 0.5%.” The 2025 ADA Standards of Care state that medical nutrition therapy (MNT) provided by an RDN can lead to A1C reductions of 0.3% to 2%, especially in individuals with type 2 diabetes. The answer is not true because a 0.5% reduction underestimates the potential benefit.
Answer 3 is incorrect. About 11% of respondents chose this, “Individualized nutrition therapy should begin at diagnosis.” The ADA recommends that individualized MNT should be initiated at the time of diagnosis. Additional times for referral include annually or when not meeting treatment goals, when complications occur or when transitions in life occur.
Finally, Answer 4 is incorrect. 8% chose this answer, “A Mediterranean eating pattern can reduce the risk of major cardiovascular disease events.” The Mediterranean eating pattern has been associated with improved glycemic control and a reduced risk of cardiovascular events, making it an eating pattern to consider for people with type 2 diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Join us live on June 5, 2025, at 11:30 am PST to watch our brand new webinar, Weight-Inclusive Diabetes Care: Turning Compassion into Practical Tools by Jessica Jones, MS, RDN, CDCES
This session provides healthcare providers with actionable strategies to integrate weight-inclusive care into diabetes management practices, focusing on improving outcomes through respect for body diversity and individual autonomy. Weight stigma is a well-documented barrier to effective care, contributing to poorer glycemic control, disordered eating, and care avoidance. By shifting from a weight-focused approach to one aligned with Health at Every Size (HAES®), providers can foster trust, enhance participant engagement, and support sustainable health behaviors.
Jessica Jones, MS, RD, CDCES, will share evidence-based insights on mitigating weight stigma and applying HAES-aligned strategies in practice. Participants will learn how to build rapport, set realistic nutrition goals, and implement interventions that prioritize blood sugar management, joyful movement, and intuitive eating. This session equips providers with tools to deliver compassionate, person-centered care, improving both clinical outcomes and the provider-participant relationship.
Course topics:
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on How Well Do You Know Coach Bev? 33% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which early job taught Coach Beverly the value of loving your work and providing excellent service?
Answer Choices:
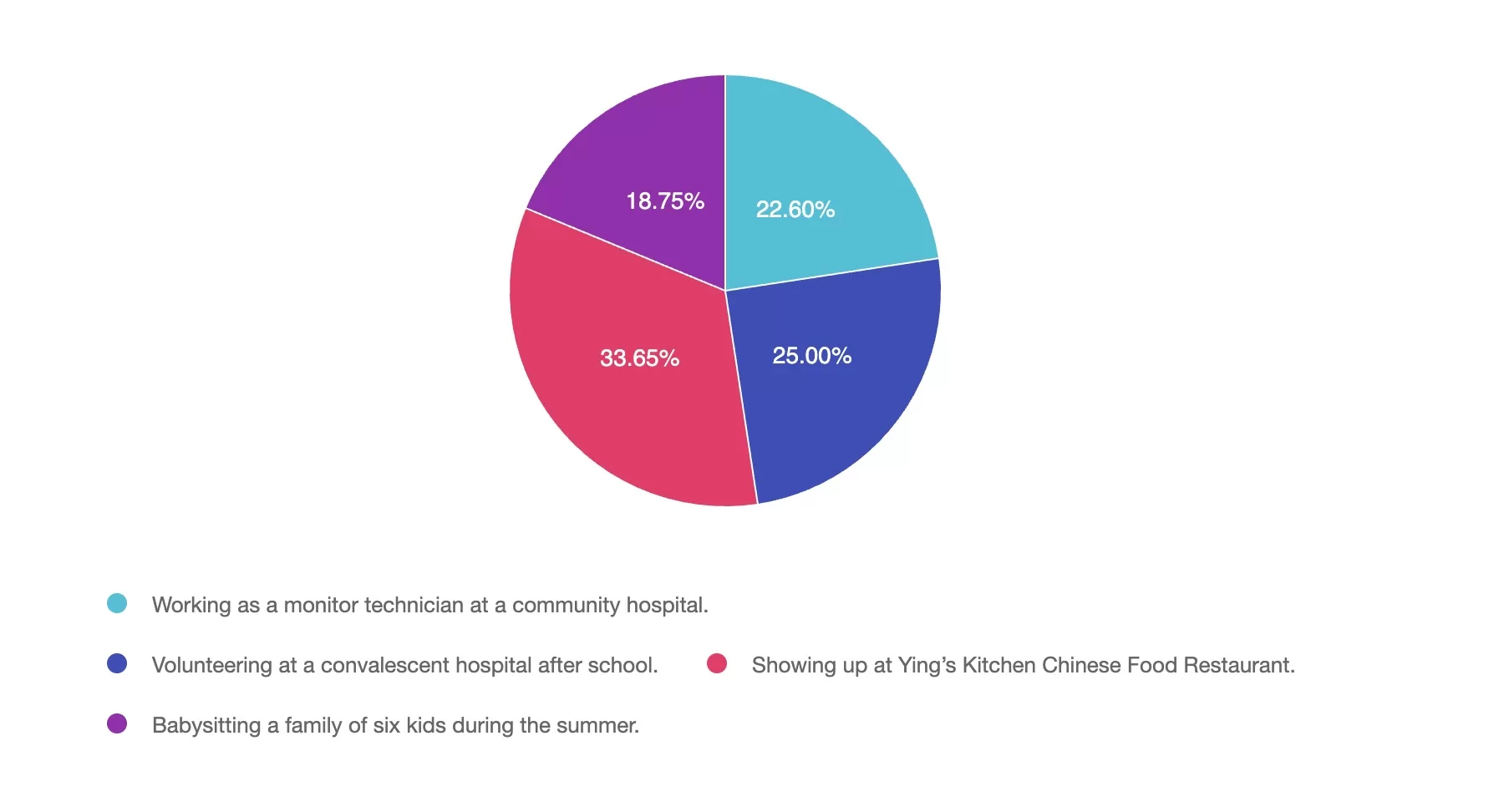
Answer 1 is incorrect. 22% chose this answer, “Working as a monitor technician at a community hospital.” Beverly worked as a monitor tech and nurses aide at a community hospital while attending nursing school. These experiences taught her about navigating medical terminology and hospital systems.
Answer 2 is incorrect. 25% of you chose this answer, “Volunteering at a convalescent hospital after school.” Coach Bev did lead Bingo games and play guitar at a convalesent home after school. She loved connecting with older adults and hearing their stories.
Answer 3 is correct. About 33% of respondents chose this, “Showing up at Ying’s Kitchen Chinese Food Restaurant.” This is the best answer. Her 8 years at Ying’s Kitchen taught her about hard work, attention to detail, and loving what you do.
Finally, Answer 4 is incorrect. 18% chose this answer, “Babysitting a family of six kids during the summer.” Watching 6 kids over the summer helped her recognize that being a parent has lots of perks, but she wasn’t ready.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Decoding AGP Report-Test Your Knowledge. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: AJ asks you why their blood glucose levels are “all over the place”. When you look at the AGP, you notice the coefficient of variation is 26%. What is the best response?
Answer Choices:
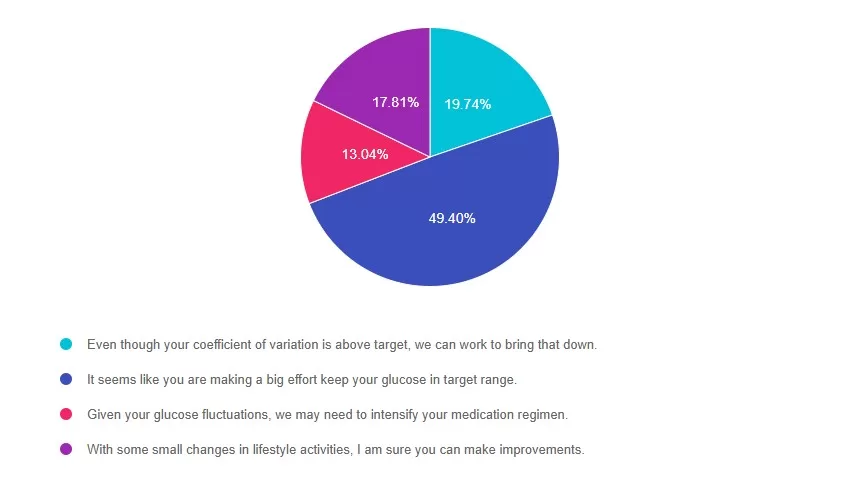
Answer 1 is incorrect. 19% chose this answer, “Even though your coefficient of variation is above target, we can work to bring that down.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Answer 2 is correct. 49% of you chose this answer, “It seems like you are making a big effort keep your glucose in target range.” YES, this is the BEST Answer. AJ has a coefficient of variation of 26%. That is 10% below the target of 36%. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Answer 3 is incorrect. About 13% of respondents chose this, “Given your glucose fluctuations, we may need to intensify your medication regimen.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Finally, Answer 4 is incorrect. 17% chose this answer, “With some small changes in lifestyle activities, I am sure you can make improvements.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Topics include:
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Best technique to assess Protective Sensation in feet? 44% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below:

Question: Best technique to assess Protective Sensation in feet? Which of the following best describes the proper technique for using a 10-gram monofilament to assess protective sensation in a person with diabetes?
Answer Choices:
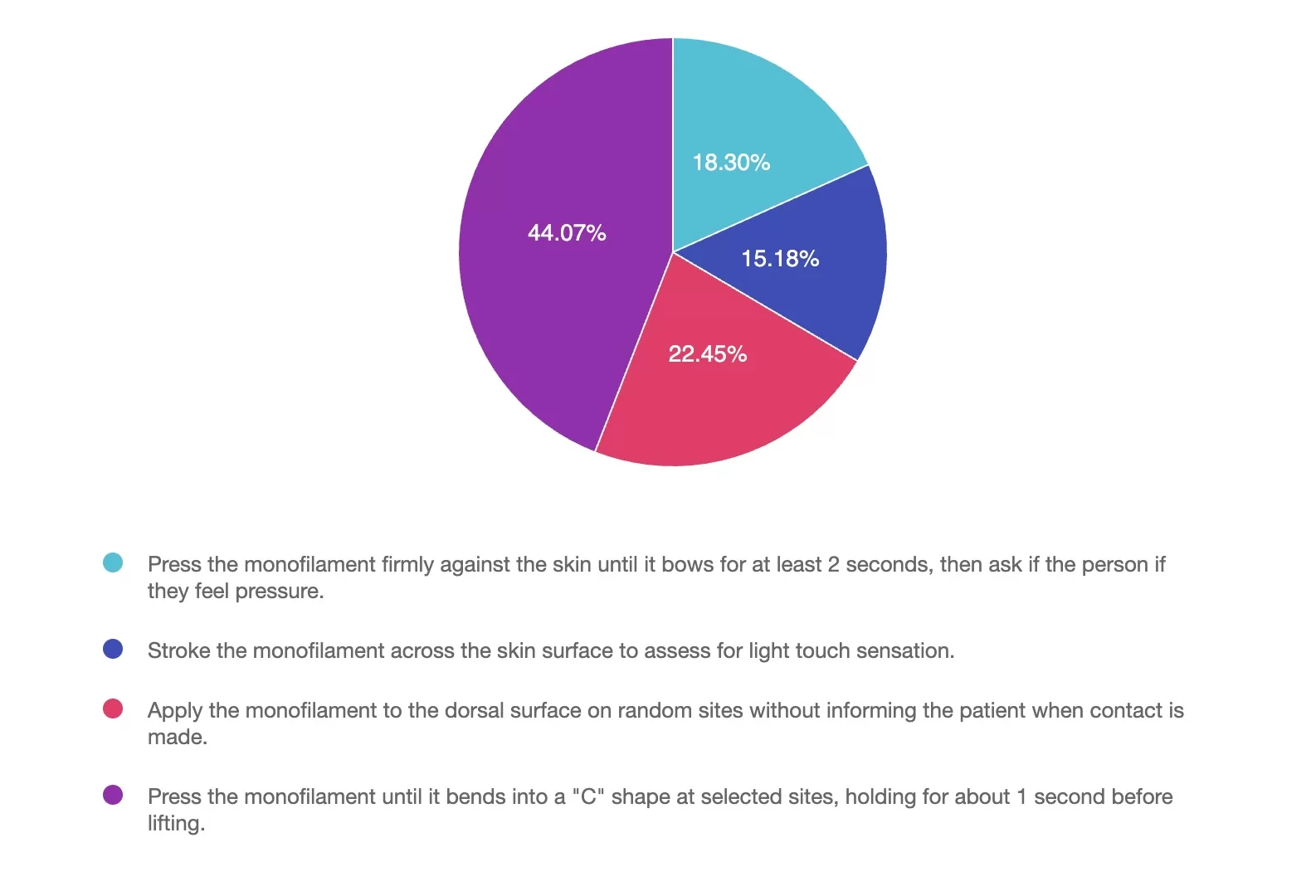
Answer 1 is incorrect. 18% chose this answer, “Press the monofilament firmly against the skin until it bows for at least 2 seconds, then ask if the person if they feel pressure.” This answer is tempting. You only need to apply the monofilament for one second and you don’t want to ask the person if they feel pressure when you are bending the monofilament into a C-shape on the plantar surface of four sites (as noted in the image below) . This could lead to them simply saying “yes” when you ask if “they feel it”.
Answer 2 is incorrect. 15% of you chose this answer, “Stroke the monofilament across the skin surface to assess for light touch sensation.” When using the monofilament, you only need to apply the monofilament for one second by bending it into a C-shape on the plantar surface of their feet on the four sites (as noted in the image below) to evaluate for sensation. This evaluation does not include stroking the monofilament.
Answer 3 is incorrect. About 22% of respondents chose this, “Apply the monofilament to the dorsal surface on random sites without informing the individual when contact is made.” You need to apply the monofilament for one second by bending it into a C-shape on the plantar surface of their feet on the four sites (as noted in the image below) to evaluate for sensation.
Finally, Answer 4 is correct. 44% chose this answer, “Press the monofilament until it bends into a “C” shape at selected sites, holding for about 1 second before lifting.” Yes, GREAT JOB. Simply apply the monofilament for one second to the sites on the image below, going above or below calluses. Ask the person to close their eyes and say yes when they feel the pressure as you bend the monofilament into a C-shape on the four plantar surfaces sites (as noted in the image below). If they can’t feel on one or more touch points, this is a sign they have “loss of protective sensation” and are at increased risk of foot injury.
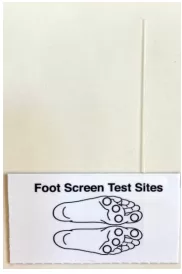 For more information on Lower Extremities – we have some great resources.
For more information on Lower Extremities – we have some great resources.
Free Assessing Lower Extremity Handout
Free Webinar: 3 Steps to DeFeet Amputations
Register for our Level 2 – Lower Extremity Assessment Course- Earn 1.5 CEs
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
We are living longer & more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering the reduction of medication & insulin therapy intensity. The older population has unique issues & special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
For last week’s practice question, we quizzed participants on Best treatment for Diabetes + Heart Disease? 70% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: BT has a history of stroke and new diagnosis of diabetes with an A1C of 6.9%.
Which of following treatment strategies is most appropriate for a person with new type 2 diabetes and established cardiovascular disease (CVD)?
Answer Choices:
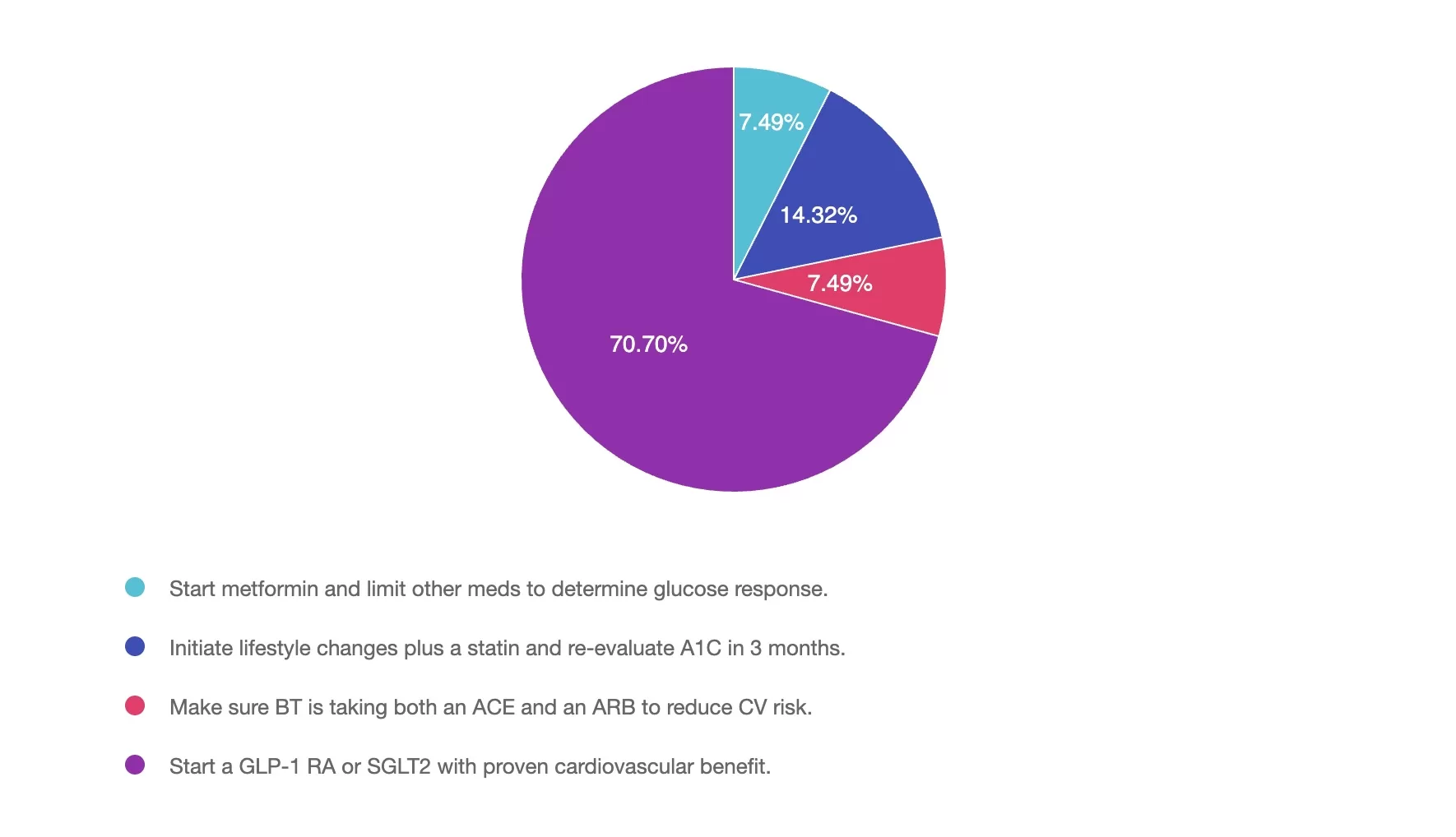
Answer 1 is incorrect. 7% chose this answer, “Start metformin and limit other meds to determine glucose response.” Based on ADA guidelines, we need to take a person’s CV and renal status into account when determining the most beneficial treatment for someone with newly diagnosed diabetes. Given the fact that BT has a history of a stroke, the MOST beneficial initial medication would be a SGLT-2 or a GLP-1 RA with proven CV benefit. Even though BT’s A1C is on target, starting either of these meds would lower their risk of another CV event. See Medication PocketCards
Answer 2 is incorrect. 14% of you chose this answer, “Initiate lifestyle changes plus a statin and re-evaluate A1C in 3 months.” Based on ADA guidelines, BT would absolutely need to be started on a statin with close monitoring of A1C coupled with lifestyle. However, we need to take a person’s CV risk status into account when determining the most beneficial treatment for someone with newly diagnosed diabetes. Given the fact that BT has a history of a stroke and new diabetes, the MOST beneficial initial medication would be a SGLT-2 or a GLP-1 RA with proven CV benefit. See Medication PocketCards
Answer 3 is incorrect. About 7% of respondents chose this, “Make sure BT is taking both an ACE and an ARB to reduce CV risk.” A person with diabetes plus hypertension and a history of stroke, would benefit from ONE of these. It is NOT recommended to take and ACE and ARB together, due the possibility of kidney complications. See HTN Med Cheat Sheets.
Finally, Answer 4 is correct. 70% chose this answer, “Start a GLP-1 RA or SGLT2 with proven cardiovascular benefit.” Based on ADA guidelines, we need to take a person’s CV risk status into account when determining the most beneficial treatment for someone with newly diagnosed diabetes. Given the fact that BT has a history of a stroke, the MOST beneficial initial medication would be a SGLT-2 or a GLP-1 RA with proven CV benefit. See Medication PocketCards.
Want to learn more about this topic? View our Level 2 Webinar – CV Disease and Decreasing Risk based on 2025 ADA Standards. Earn 1.5 CEs.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Session 1 – May 8th
with Beverly Thomassian at 11:30am to 12:30pm PST
Session 2 – May 15th
with Dr. Diana Isaacs at 11:30am to 2:30pm PST
Gain confidence in interpreting Glucose Profile Report (AGP) & CGM data using a person-centered approach!
We still have room available for the May 8th kick off date.
With diabetes technology entering all aspects of diabetes care, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience. Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Coach Beverly will build on Dr. Isaacs’ presentation. She will expand the focus to include steps to collaborate with the person with diabetes. Using a case study approach, she will provide strategies to integrate the AGP with person-centered care that empowers individuals to experience increased confidence in their diabetes self-management.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments with a person-centered approach.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on What Stage of Change? 58% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

BT was started on a GLP-1 and is losing weight. BT has read articles about the importance of strength training to maintain muscle. They ask you questions about whether using weights or resistance bands is better.
According to the transtheoretical model, what stage of change is BT in?
Answer Choices:
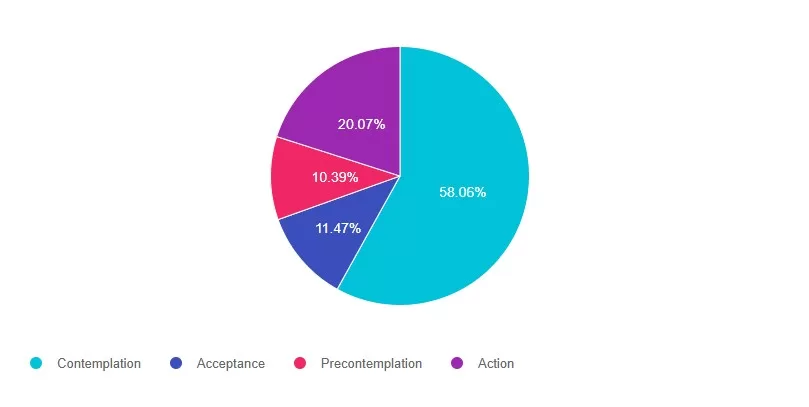
Answer 1 is correct. 58% chose this answer, “Contemplation.” GREAT JOB! When people are in contemplation stage, they are aware of the need for change and are actively considering making a change within the next six months. They are weighing the pros and cons of changing their behavior. In this situation BT is contemplating two different approaches to strengthening exercises,
Answer 2 is incorrect. 11% of you chose this answer, “Acceptance.” Even though BT may be accepting the need to get active, acceptance is not one of the stages in the transtheoretical model. This was one of those juicy answers.: -)
Answer 3 is incorrect. About 10% of respondents chose this, “Precontemplation.” This answer is tempting, but in precontemplation, individuals are not yet considering changing behavior. They may be unaware of the need for change or may have a resistant attitude toward it. BT wants to increase activity, but is choosing between two strength training options.
Finally, Answer 4 is incorrect. 20% chose this answer, “Action.” This person is not quite at the action stage. Action is when Individuals are actively modifying behavior, implementing plans, and making observable changes in their behavior, environment, or lifestyle.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Session 1 – May 8th
with Beverly Thomassian at 11:30am to 12:30pm PST
Session 2 – May 15th
with Dr. Diana Isaacs at 11:30am to 2:30pm PST
Gain confidence in interpreting Glucose Profile Report (AGP) & CGM data using a person-centered approach!
If you are preparing for certification exams or want to up your game using CGM data to improve outcomes, this course is for you.
We still have room available for the May 8th kick off date.
With diabetes technology entering all aspects of diabetes care, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience. Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Coach Beverly will build on Dr. Isaacss’ presentation. She will expand the focus to include steps to collaborate with the person with diabetes. Using a case study approach, she will provide strategies to integrate the AGP with person-centered care that empowers individuals to experience increased confidence in their diabetes self-management.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments with a person-centered approach.
Topics include:
Review CGM key metrics and individualize time in-range goals.
Learn how to recognize patterns with the AGP report efficiently.
Recommend lifestyle and medication adjustments based on CGM data.
Utilize the AGP report coupled with a person centered approach when meeting with a person with diabetes.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Sleep and ADA Recommendations. 71% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
A 62-year-old with type 1 diabetes presents for their follow-up visit. They report struggling with fatigue, poor sleep quality, and difficulty with glucose management despite taking medications as prescribed. Upon review, you find their A1C is 7.6%, and their average nightly sleep duration is 4.5-6 hours per night.
Based on the 2025 ADA Standards of Care, which of the following interventions would be the most appropriate next step to address sleep and glucose management?
Answer Choices:
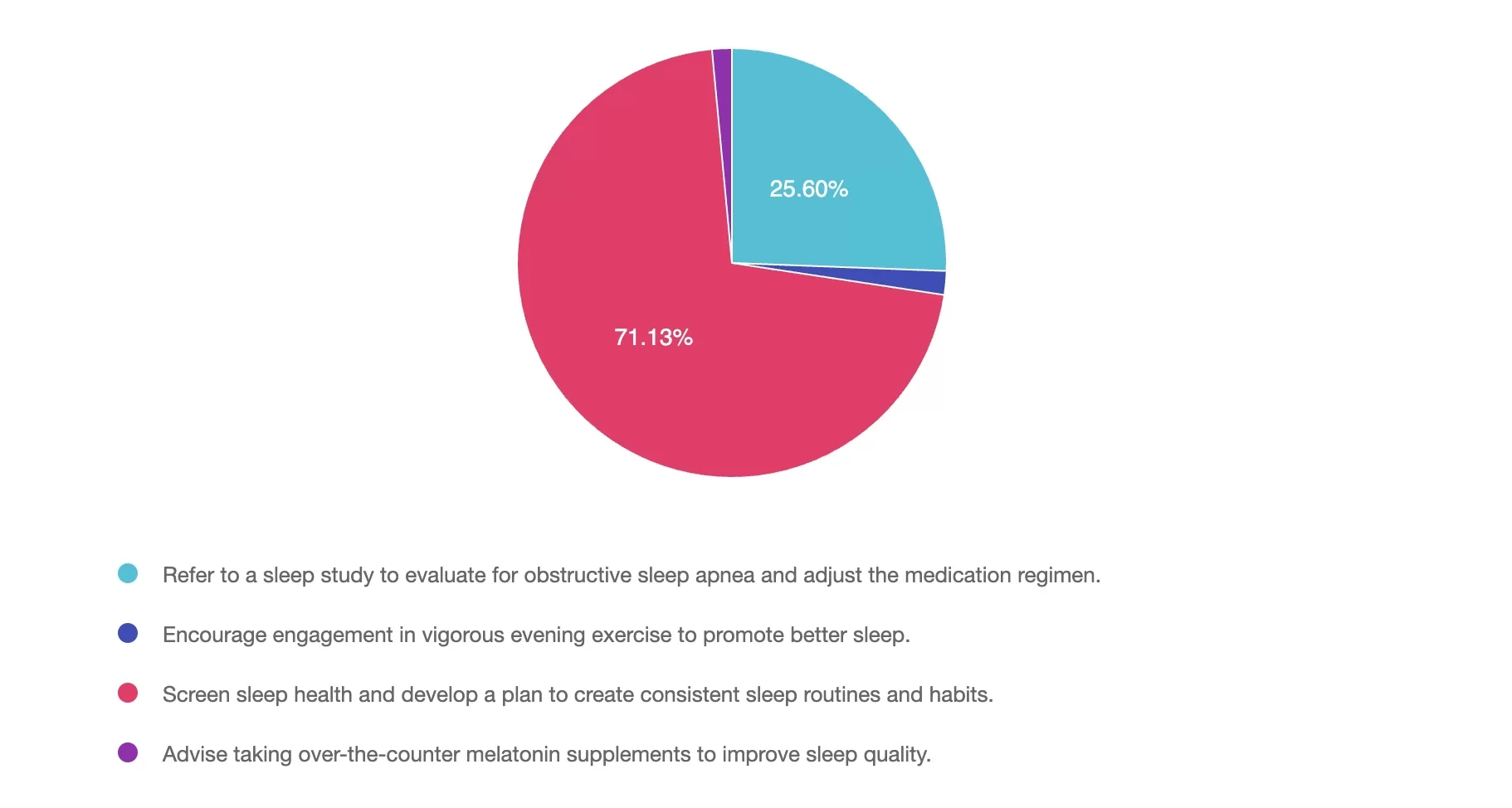
Answer 1 is incorrect. 25% chose this answer, “Refer to a sleep study to evaluate for obstructive sleep apnea and adjust the medication regimen.” While a sleep study may be recommended for suspected sleep disorders, such as sleep apnea (for example: loud snoring, daytime sleepiness), the first step should be a comprehensive sleep health screening. This screening helps identify potential causes of poor sleep, including symptoms of sleep disorders, disruptions from diabetes management (for example: nocturnal hypoglycemia, frequent urination), or anxiety about sleep. Based on the findings, appropriate treatment modifications and referrals can then be made.
Answer 2 is incorrect. 1% of you chose this answer, “Encourage engagement in vigorous evening exercise to promote better sleep.” Although exercise can improve sleep quality, vigorous evening exercise may increase alertness, making it harder to fall asleep. In individuals with type 1 diabetes, this timing of exercise can also increase the risk of nighttime hypoglycemia, further disrupting sleep. Before recommending vigorous exercise, it’s important to first assess sleep habits to better understand the underlying causes of poor sleep quality.
Answer 3 is correct. About 71% of respondents chose the BEST ANSWER – GREAT JOB! “Screen sleep health and develop a plan to create consistent sleep routines and habits.” The 2025 ADA Standards emphasize the importance of screening for sleep health and providing guidance on sleep-promoting routines and habits. Based on screening results, referrals to sleep medicine programs, adjustment in medications or behavioral therapy programs are a few that may be appropriate. Prioritizing improved sleep duration and consistency can support better glucose management, reduce fatigue, and enhance overall well-being.
Finally, Answer 4 is incorrect. 1% chose this answer, “Advise taking over-the-counter melatonin supplements to improve sleep quality.” While melatonin may be helpful for certain sleep disorders, its use should be evaluated on a case-by-case basis and is not recommended within the ADA 2025 Standards of Care. The first-line recommendation should focus on screening to better determine appropriate actions.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.