
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Best approach: Fasting During Ramadan
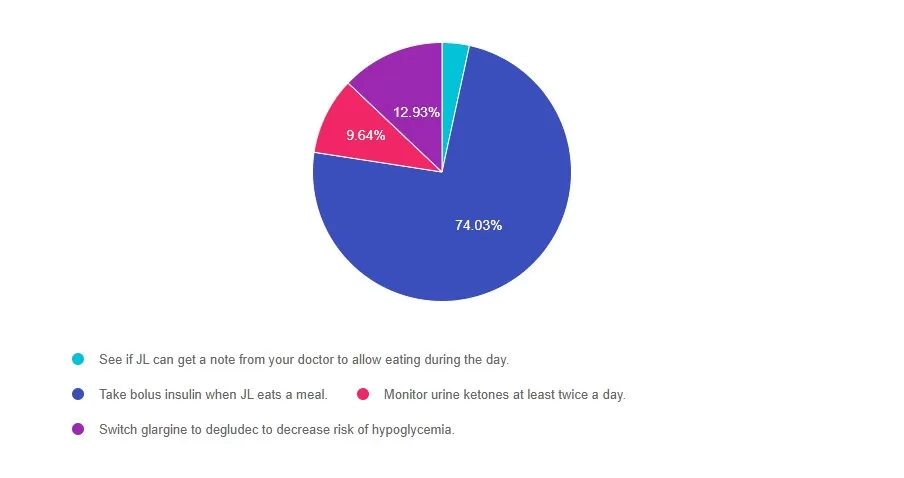
For last week’s practice question, we quizzed participants on best approach: fasting during Ramadan . 74% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JL observes Ramadan and fasts from sunrise to sunset. JL has type 2 diabetes and usually takes 4 units of bolus insulin three times a day with meals and 10 units of glargine (Rezvoglar) at bedtime.
What would be the best recommendation for JL?
Answer Choices:
- See if JL can get a note from your doctor to allow eating during the day.
- Take bolus insulin when JL eats a meal.
- Monitor urine ketones at least twice a day.
- Switch glargine to degludec to decrease risk of hypoglycemia.
Getting to the Best Answer
Answer 1 is incorrect. 3% chose this answer, See if JL can get a note from your doctor to allow eating during the day. With careful planning and insulin adjustments, we can honor JL’s religious fast and cultural beliefs.
Answer 2 is correct. 76% of you chose this answer, Take bolus insulin when JL eats a meal. Yes, this is the BEST answer. If the basal insulin is dosed correctly, it won’t cause hypoglycemia while fasting. JL can hold bolus insulin during fasting, and take bolus insulin when eating.
Answer 3 is incorrect. About 9% of respondents chose this, Monitor urine ketones at least twice a day. There is no need to monitor ketones, since JL will be taking basal insulin daily and bolus insulin with meals, which will prevent ketosis.
Finally, Answer 4 is incorrect. 12% chose this answer, Switch glargine to degludec to decrease risk of hypoglycemia. There is no need to switch basal insulins. JL can stay on glargine, recognizing that it may need to be adjusted.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | Based on ADA Standards, what is next med addition?
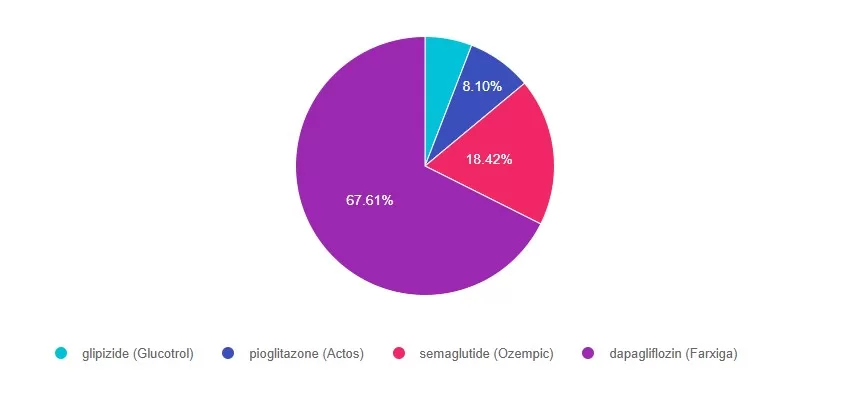
For last week’s practice question, we quizzed participants on ADA Standards & what is next med addition? 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JR has type 2 diabetes and takes Metformin 1000mg BID and sitagliptin (Januvia), A1C 8.1%. GFR 47, UACR 158mg/g. Recent diagnosis of congestive heart failure. These are the medications their insurance covers.
Of the following medications, which addition would most benefit JR?
Answer Choices:
- glipizide (Glucotrol)
- pioglitazone (Actos)
- semaglutide (Ozempic)
- dapagliflozin (Farxiga)
Getting to the Best Answer
For a helpful reference, please see our PocketCards for more information.
Answer 1 is incorrect. 5% chose this answer, “Glipizide (Glucotrol)”. Even though glipizide would help lower blood glucose, considering JL’s CHF and worsening kidney function, it is not the best choice.
Answer 2 is incorrect. 8% of you chose this answer, “pioglitazone (Actos)”. Even though pioglitazone would help lower blood glucose, considering JL’s CHF and worsening kidney function, it is not the best choice.
Answer 3 is incorrect. About 18% of respondents chose this, “Semaglutide (Ozempic)”. Even though semaglutide would help lower blood glucose and would address worsening kidney function, considering JL’s CHF and worsening kidney function, it is not the best choice.
Finally, Answer 4 is correct. 67% chose this answer, “Dapagliflozin (Farxiga)”. YES, GREAT JOB. Dapagliflozin is a SGLT-2i that will help lower blood glucose, address worsening kidney function and CHF. Plus, it is covered by insurance. Considering JL’s health profile, it is the best choice.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | 2025 ADA Standards: Key Nutrition Behaviors for Individuals with Diabetes
For last week’s practice question, we quizzed participants on. 79% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question.
Question:
According to the 2025 ADA Standards of Care, which of the following nutrition behaviors are strongly encouraged for individuals with diabetes?
Answer Choices:
- Incorporate onions, garlic, celery, carrots and other vegetables for a base of homemade
foods. - Use herbs and spices to season foods instead of salt containing preparations.
- Water should be the primary beverage of choice.
- Include family or roommate in meal preparation.
- All of the above
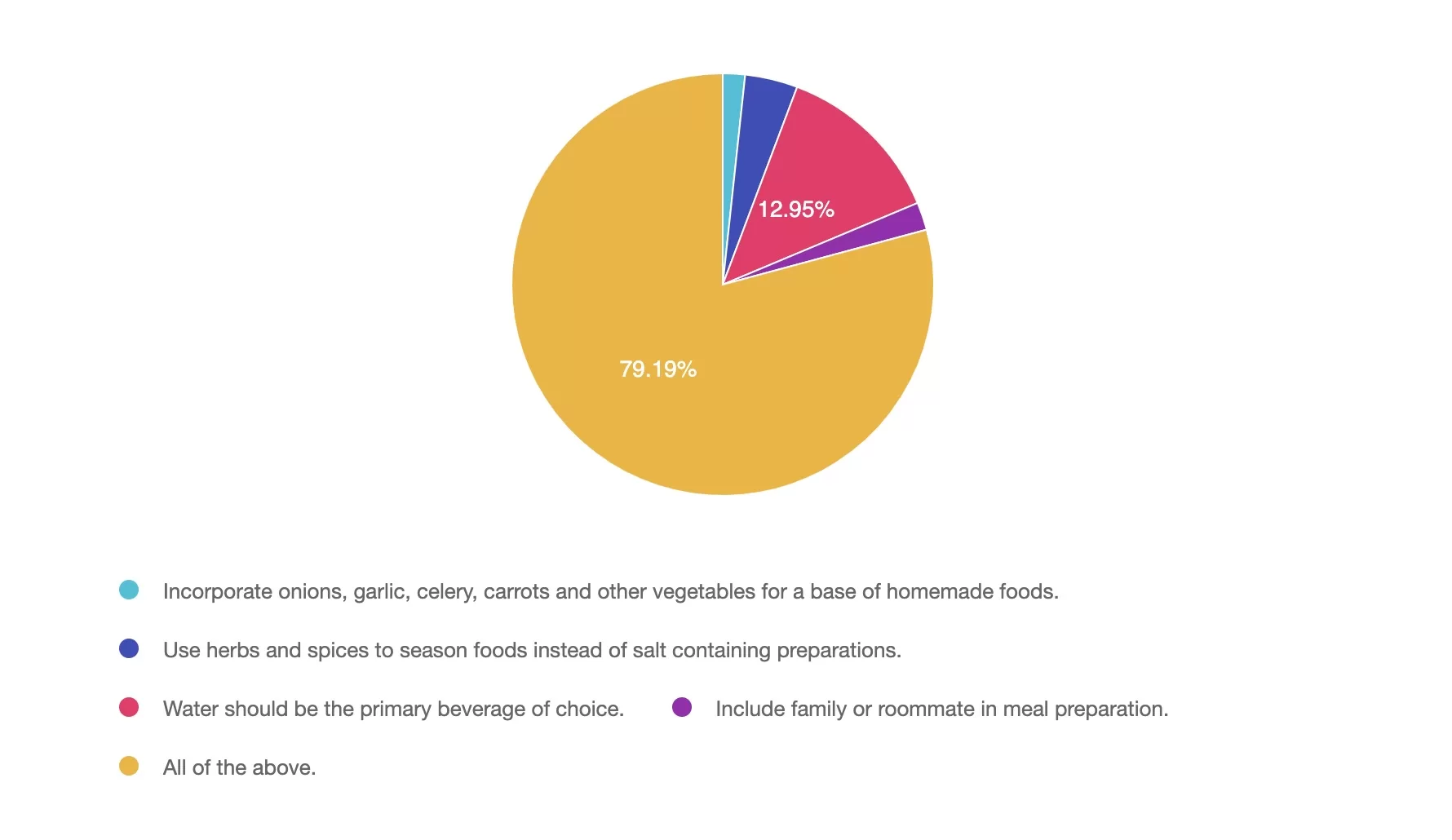
Getting to the Best Answer
Answer 1 is incorrect. 1.7% chose this answer, ” Incorporate onions, garlic, celery, carrots and other vegetables for a base of homemade foods.” Although this answer is true, it is not the best answer. Incorporate onions, garlic, celery, carrots, and other vegetables for a base of homemade foods. These foods can serve as a base to many dishes and incorporates flavor, fiber, vitamins, and minerals while encouraging vegetable consumption.
Answer 2 is incorrect. 4% of you chose this answer, “Use herbs and spices to season foods instead of salt containing preparations.” Although this answer is true, it is not the best answer. 90% of people in the US exceed the daily recommended limits for sodium. Reducing salt intake is important for heart health, managing blood pressure and meeting dietary guidelines. Herbs and spices not only enhance flavor and may provide additional health benefits.
Answer 3 is incorrect. About 12% of respondents chose this, “Water should be the primary beverage of choice.” Although this answer is true, it is not the best answer. The 2025 ADA Standards of Care have emphasized water as the primary beverage of choice. Alternatives to plain water can include no calorie alternatives. Suggestions to add lemon, lime or cucumber to water, choose sparkling no calorie beverages and no-calorie carbonated beverages are also encouraged.
Answer 4 is incorrect. 2% chose this answer, “Include family or roommate in meal preparation.” Although this answer is true, it is not the best answer. Engaging others in meal preparation can create a supportive environment, encourage healthier eating habits, and make cooking more enjoyable. Social support can be especially helpful in managing diabetes long-term.
Answer 5 is correct. 79% chose this answer, “All of the above.” The 2025 ADA Standards of Care encourages all the above nutrition behaviors.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Rationale of the Week | Action needed to prevent heart failure?
For last week’s practice question, we quizzed participants oAction needed to prevent heart failure. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
Adults with diabetes are at increased risk for the development of asymptomatic or symptomatic heart failure.
According to the ADA 2025 Standards of care, what action is needed to facilitate prevention of heart failure?
Answer Choices:
- Recommend the DASH Diet.
- Measure natriuretic peptide (BNP or pro-BNP).
- Assess ankle circumference at each visit.
- Recommend echocardiography after age 55.
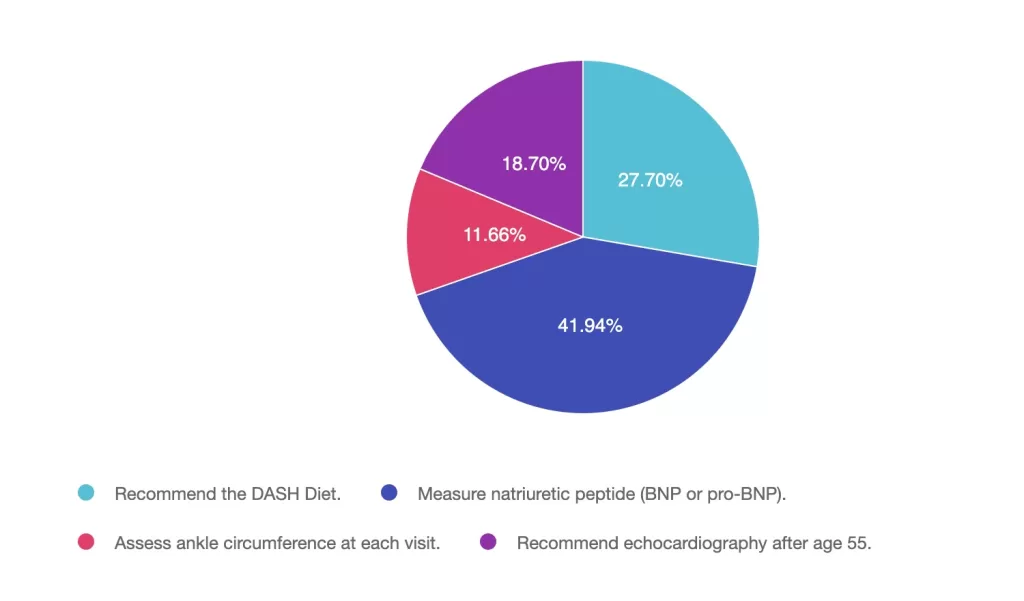
Getting to the Best Answer
Answer 1 is incorrect. 27% chose this juicy answer. “Recommend the DASH Diet.” Although the DASH Diet with lower sodium content is helpful once someone is diagnosed with heart failure, this dietary approach alone won’t prevent heart failure. In order to prevent heart failure, it needs to first be diagnosed to determine best treatment plan.
Answer 2 is correct. 49% of you chose this answer. “Measure natriuretic peptide (BNP or pro-BNP).” YES, Great JOB. According to the ADA Standard on ASCVD, “Adults with diabetes are at increased risk for the development of asymptomatic cardiac structural or functional abnormalities (stage B heart failure) or symptomatic (stage C) heart failure. Consider screening adults with diabetes by measuring a natriuretic peptide (B-type natriuretic peptide [BNP] or N-terminal pro-BNP [NT-proBNP]) to facilitate prevention of stage C heart failure. In asymptomatic individuals with diabetes and abnormal natriuretic peptide levels, echocardiography is recommended to identify stage B heart failure.”
Answer 3 is incorrect. About 11% of respondents chose this. “Assess ankle circumference at each visit.” Although pedal edema and shortness of breath are both indicators of heart failure, the BNP or NT-proBNP lab test is more definitive.
Finally, Answer 4 is incorrect. 18% chose this answer. “Recommend echocardiography after age 55.” According to ADA standards, we would first check the BNP or NT-proBNP lab test. In asymptomatic individuals with diabetes and abnormal natriuretic peptide levels, echocardiography is then recommended to identify stage B heart failure.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
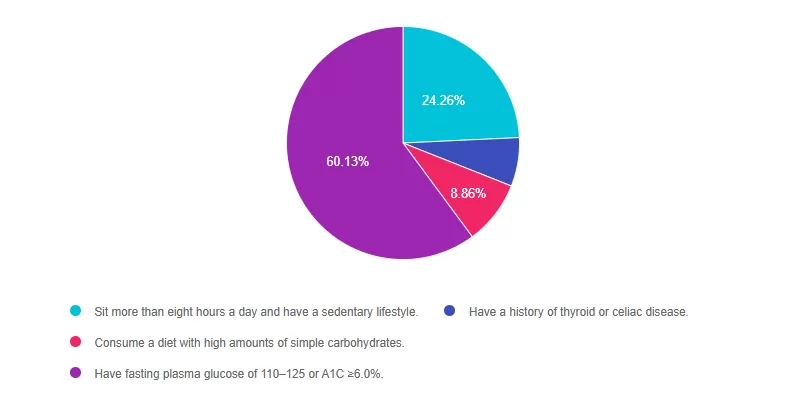
Rationale of the Week | ADA 2025: Intensive Prevention for High-Risk Individuals with BMI >35 kg/m2
For last week’s practice question, we quizzed participants on what defines overbasalization according to 2025 ADA Standards? 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
According to ADA 2025 Standards, more intensive preventive approaches should be considered in individuals who are at particularly high risk of progression to diabetes, including individuals with BMI ≥35 kg/m2 who:
Answer Choices:
- Sit more than eight hours a day and have a sedentary lifestyle.
- Have a history of thyroid or celiac disease.
- Consume a diet with high amounts of simple carbohydrates.
- Have fasting plasma glucose of 110–125 or A1C ≥6.0%.
Getting to the Best Answer
Answer 1 is incorrect. 25% chose this answer, “Sit more than eight hours a day and have a sedentary lifestyle”. Although the ADA Standards recommend getting up and moving every half-hour, they don’t specify that eight hours of sitting a day qualifies a person as higher risk to progressing to diabetes.
Answer 2 is incorrect. 7% of you chose this answer “Have a history of thyroid or celiac disease”. These autoimmune conditions are more closely associated with immune mediated type 1 diabetes and do not place a person as higher risk for progression to type 2 diabetes.
Answer 3 is incorrect. About 9% of respondents chose this, “Consume a diet with high amounts of simple carbohydrates.” While eating foods rich in fiber and a variety of nutrients is important to decrease risk of diabetes, the ADA does not state that eating simple carbohydrates puts individuals in a higher risk category of progressing to diabetes.
Finally, Answer 4 is correct 60% chose this answer, “Have fasting plasma glucose of 110–125 or A1C ≥6.0%.” Great job. This is the BEST answer. According to ADA 2025 Standards, “More intensive preventive approaches should be considered in individuals who are at particularly high risk of progression to diabetes, including individuals with BMI ≥35 kg/m2, those at higher glucose levels (e.g., fasting plasma glucose 110–125 mg/dL [6.1–6.9 mmol/L], 2-h post challenge glucose 173–199 mg/dL [9.6–11.0 mmol/L], and A1C ≥6.0% [≥42 mmol/mol]), and individuals with a history of gestational diabetes mellitus.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
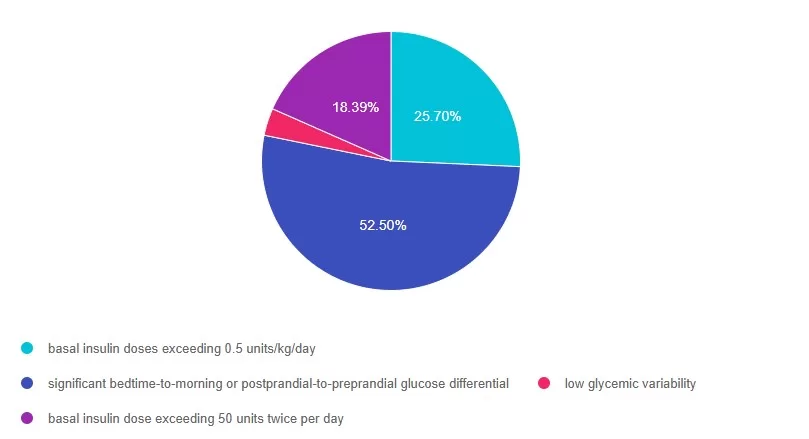
Rationale of the Week | What defines overbasalization according to 2025 ADA Standards?
For last week’s practice question, we quizzed participants on what defines overbasalization according to 2025 ADA Standards?. 52% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
What defines overbasalization according to 2025 ADA Standards?
According to the new 2025 ADA Standards of Care, which of the following most accurately reflects overbasalization?
Answer Choices:
- basal insulin doses exceeding 0.5 units/kg/day
- significant bedtime-to-morning or postprandial-to-preprandial glucose differential
- low glycemic variability
- basal insulin dose exceeding 50 units twice per day
Getting to the Best Answer
Answer 1 is incorrect. 25% chose this answer: basal insulin doses exceeding 0.5 units/kg/day. This year, the ADA Recommendation was revised to remove consideration of basal insulin doses exceeding 0.5 units/kg/day as evidence of overbasalization. Instead, signs of overbasalization including significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability should be used.
Answer 2 is correct. 52% of you chose this answer: significant bedtime-to-morning or postprandial-to-preprandial glucose differential. GREAT JOB! In the 2025 ADA Standards (9), they define overbasalization as significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability.
Answer 3 is incorrect. About 18% of respondents chose this: low glycemic variability, This is a juicy and tempting answer. However, high glycemic variability (lots of ups and downs) is more closely associated with hypoglycemia.
Finally, Answer 4 is incorrect 3% chose this answer: basal insulin dose exceeding 50 units twice per day. Overbasalization is not defined by the amount of insulin used, but by the glucose response including significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our Level 3
Diabetes Mastery & Cert Readiness
Ready for your certification exams? Our Level 3 course series is the final step in your exam prep, complementing our Level 1, 2, or 4 bundles. Designed for healthcare professionals preparing for diabetes certification exams in 3-6 months, this master-level series covers key topics like pharmacology, technology, MNT, and person-centered care, all based on the latest ADA Standards of Care.
Each course includes a video, podcast, practice test, and additional resources—available immediately for one full year. Boost your knowledge and confidence to succeed in your certification!
Rationale of the Week | ADA Standards identify another 1st Line med to treat kidney disease. Which one?
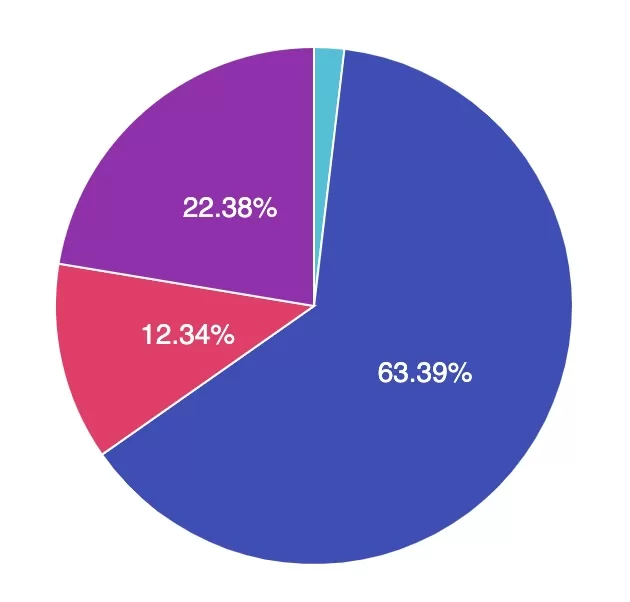
For last week’s practice question, we quizzed participants on ADA Standards identify another 1st line med to treat kidney disease. 63.39% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
According to the ADA 2025 Standards, new clinical trials suggest that another diabetes medication (besides SGLT-2i) can be used as a first line agent to treat chronic kidney disease.
Which of the folowing diabetes meds is effective as a first-line agent for people with CKD?
Answer Choices:
- Afrezza inhaled insulin
- Semaglutize (Ozempic)
- Amylin (Pramlintide)
- Sitagliptin (Januvia)
Getting to the Best Answer
Answer 1 is incorrect. 2% chose the answer, Afrezza inhaled insulin. Insulin helps lower blood glucose levels, which contributes to improved overall vessel health. However, there are currently no specific studies supporting the use of Afrezza as a first-line treatment strategy for managing chronic kidney disease.
Answer 2 is correct. 63.39% of you chose this answer the best answer, semaglutide (Ozempic). GREAT JOB! According to the 2025 ADA Standards, “a recent clinical trial suggests that the GLP-1 RA semaglutide has a beneficial effect on CVD, mortality, and kidney outcomes among people with Chronic Kidney Disease (CKD), leading to the recommendation that semaglutide can be used as another first-line agent for people with CKD.”
Answer 3 is incorrect. About 12.34% of respondents chose Amylin (Pramlintide). Amylin is an injected hormone mimetic that helps lower blood glucose levels. However, there are currently no specific studies supporting the use of Amylin as a first-line treatment strategy for managing chronic kidney disease.
Finally, Answer 4 is incorrect. 22.38% chose this answer, Sitagliptin (Januvia). Sitagliptin helps lower A1C levels by 0.5-0.7%. However, there are currently no specific studies supporting the use of sitagliptin as a first-line treatment strategy for managing chronic kidney disease.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our Standards of Care Course
This is our most popular course of the year, offering the perfect opportunity to immerse yourself in the essential content featured in this comprehensive 300-page clinical guidebook.
“As always, Bev delivers comprehensive human-centered material to make me a better educator and leader.“- DiabetesEd Student
We hope to see you there!
Rationale of the Week | Diabetes & Malnutrition Risk
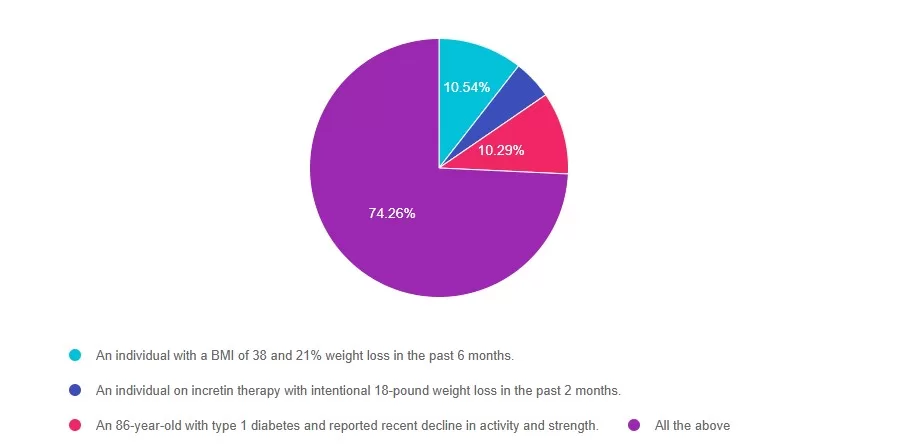
For last week’s practice question, we quizzed participants on Diabetes & Malnutrition Risk 74.26% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: The 2025 ADA Standards of Care have added recommendations for malnutrition screening.
According to these updated standards, who could be at risk for malnutrition?
Answer Choices:
- An individual with a BMI of 38 and 21% weight loss in the past 6 months.
- An individual on incretin therapy with intentional 18-pound weight loss in the past 2 months.
- An 86-year-old with type 1 diabetes and reported recent decline in activity and strength.
- All the above
Getting to the Best Answer
Answer 1 is incorrect. 10.54% chose this answer: “An individual with a BMI of 38 and 21% weight loss in the past 6 months”. Although Answer A is true, it is not the best answer. Malnutrition risk is not solely based on BMI. According to the 2025 ADA Standards of Care, individuals with diabetes experiencing significant weight loss, greater than 20%, may be at risk for malnutrition regardless of starting BMI.
Answer 2 is incorrect. 4.90% of you chose this answer: “An individual on incretin therapy with intentional 18-pound weight loss in the past 2 months.” This answer is also true, but there is a better answer. Even though the weight loss was intentional on incretin therapy, a rapid drop in weight, more than 4 kg/month, can still place an individual at risk for malnutrition. Monitoring nutrition status during weight loss pharmacotherapy is essential.
Answer 3 is incorrect About 10.29% of respondents chose this: “An 86-year-old with type 1 diabetes and reported recent decline in activity and strength”. This answer is true but not the best answer. Older adults, especially those with type 1 diabetes, are at greater risk for malnutrition, particularly when they experience declines in physical activity and strength. Malnutrition and sarcopenia, a loss of lean body mass, may develop simultaneously.
Finally, Answer 4 is correct. 74.26% chose this correct answer – GREAT JOB! All these scenarios indicate an increased risk of malnutrition and warrant additional screening. The ADA Standards of Care emphasize screening for malnutrition in individuals who have lost significant weight, especially individuals’ post-metabolic surgery, on incretin therapy, and individuals managing multiple chronic conditions who may experience an increased risk of developing sarcopenia and malnutrition. Check out the 2025 ADA Standards of Care Section 5 and Section 8 for the latest on malnutrition screening recommendations.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on Jan. 30th for our
Standard of Care Course
Level 2
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standard of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.






