Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | What defines overbasalization according to 2025 ADA Standards?
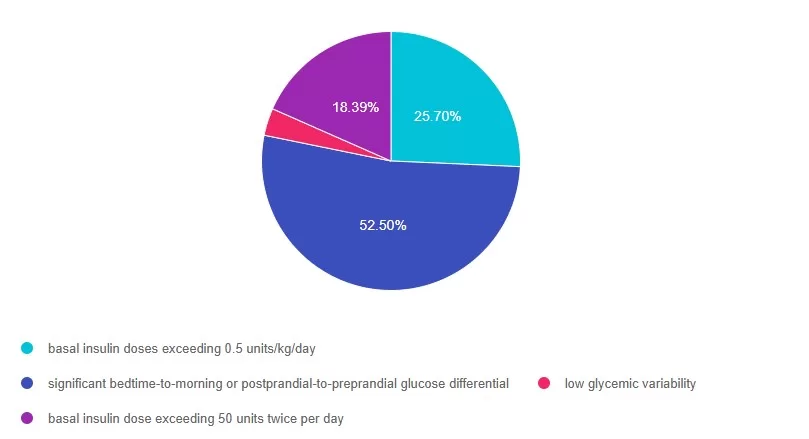
For last week’s practice question, we quizzed participants on what defines overbasalization according to 2025 ADA Standards?. 52% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
What defines overbasalization according to 2025 ADA Standards?
According to the new 2025 ADA Standards of Care, which of the following most accurately reflects overbasalization?
Answer Choices:
- basal insulin doses exceeding 0.5 units/kg/day
- significant bedtime-to-morning or postprandial-to-preprandial glucose differential
- low glycemic variability
- basal insulin dose exceeding 50 units twice per day
Getting to the Best Answer
Answer 1 is incorrect. 25% chose this answer: basal insulin doses exceeding 0.5 units/kg/day. This year, the ADA Recommendation was revised to remove consideration of basal insulin doses exceeding 0.5 units/kg/day as evidence of overbasalization. Instead, signs of overbasalization including significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability should be used.
Answer 2 is correct. 52% of you chose this answer: significant bedtime-to-morning or postprandial-to-preprandial glucose differential. GREAT JOB! In the 2025 ADA Standards (9), they define overbasalization as significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability.
Answer 3 is incorrect. About 18% of respondents chose this: low glycemic variability, This is a juicy and tempting answer. However, high glycemic variability (lots of ups and downs) is more closely associated with hypoglycemia.
Finally, Answer 4 is incorrect 3% chose this answer: basal insulin dose exceeding 50 units twice per day. Overbasalization is not defined by the amount of insulin used, but by the glucose response including significant bedtime-to-morning or postprandial-to-preprandial glucose differential, occurrences of hypoglycemia (aware or unaware), and high glycemic variability
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our Level 3
Diabetes Mastery & Cert Readiness
Ready for your certification exams? Our Level 3 course series is the final step in your exam prep, complementing our Level 1, 2, or 4 bundles. Designed for healthcare professionals preparing for diabetes certification exams in 3-6 months, this master-level series covers key topics like pharmacology, technology, MNT, and person-centered care, all based on the latest ADA Standards of Care.
Each course includes a video, podcast, practice test, and additional resources—available immediately for one full year. Boost your knowledge and confidence to succeed in your certification!
Rationale of the Week | ADA Standards identify another 1st Line med to treat kidney disease. Which one?
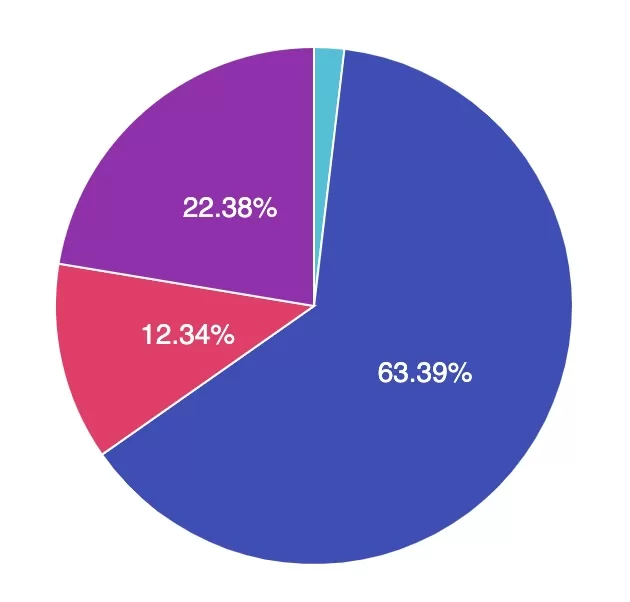
For last week’s practice question, we quizzed participants on ADA Standards identify another 1st line med to treat kidney disease. 63.39% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
According to the ADA 2025 Standards, new clinical trials suggest that another diabetes medication (besides SGLT-2i) can be used as a first line agent to treat chronic kidney disease.
Which of the folowing diabetes meds is effective as a first-line agent for people with CKD?
Answer Choices:
- Afrezza inhaled insulin
- Semaglutize (Ozempic)
- Amylin (Pramlintide)
- Sitagliptin (Januvia)
Getting to the Best Answer
Answer 1 is incorrect. 2% chose the answer, Afrezza inhaled insulin. Insulin helps lower blood glucose levels, which contributes to improved overall vessel health. However, there are currently no specific studies supporting the use of Afrezza as a first-line treatment strategy for managing chronic kidney disease.
Answer 2 is correct. 63.39% of you chose this answer the best answer, semaglutide (Ozempic). GREAT JOB! According to the 2025 ADA Standards, “a recent clinical trial suggests that the GLP-1 RA semaglutide has a beneficial effect on CVD, mortality, and kidney outcomes among people with Chronic Kidney Disease (CKD), leading to the recommendation that semaglutide can be used as another first-line agent for people with CKD.”
Answer 3 is incorrect. About 12.34% of respondents chose Amylin (Pramlintide). Amylin is an injected hormone mimetic that helps lower blood glucose levels. However, there are currently no specific studies supporting the use of Amylin as a first-line treatment strategy for managing chronic kidney disease.
Finally, Answer 4 is incorrect. 22.38% chose this answer, Sitagliptin (Januvia). Sitagliptin helps lower A1C levels by 0.5-0.7%. However, there are currently no specific studies supporting the use of sitagliptin as a first-line treatment strategy for managing chronic kidney disease.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our Standards of Care Course
This is our most popular course of the year, offering the perfect opportunity to immerse yourself in the essential content featured in this comprehensive 300-page clinical guidebook.
“As always, Bev delivers comprehensive human-centered material to make me a better educator and leader.“- DiabetesEd Student
We hope to see you there!
Rationale of the Week | Diabetes & Malnutrition Risk
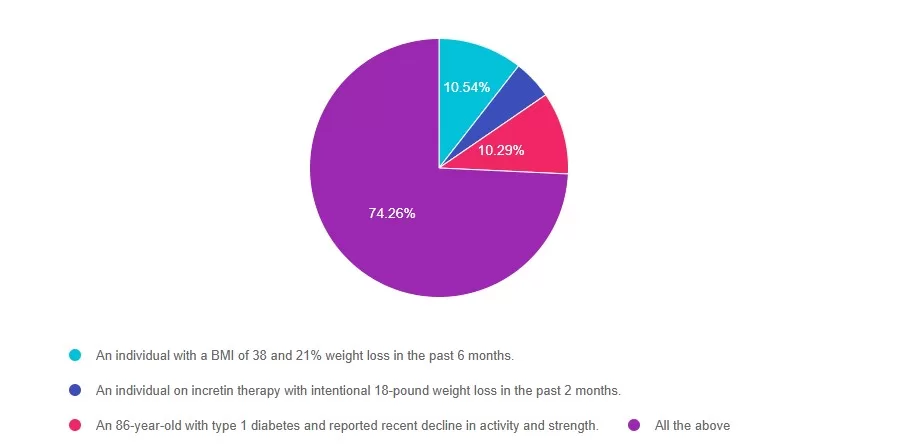
For last week’s practice question, we quizzed participants on Diabetes & Malnutrition Risk 74.26% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: The 2025 ADA Standards of Care have added recommendations for malnutrition screening.
According to these updated standards, who could be at risk for malnutrition?
Answer Choices:
- An individual with a BMI of 38 and 21% weight loss in the past 6 months.
- An individual on incretin therapy with intentional 18-pound weight loss in the past 2 months.
- An 86-year-old with type 1 diabetes and reported recent decline in activity and strength.
- All the above
Getting to the Best Answer
Answer 1 is incorrect. 10.54% chose this answer: “An individual with a BMI of 38 and 21% weight loss in the past 6 months”. Although Answer A is true, it is not the best answer. Malnutrition risk is not solely based on BMI. According to the 2025 ADA Standards of Care, individuals with diabetes experiencing significant weight loss, greater than 20%, may be at risk for malnutrition regardless of starting BMI.
Answer 2 is incorrect. 4.90% of you chose this answer: “An individual on incretin therapy with intentional 18-pound weight loss in the past 2 months.” This answer is also true, but there is a better answer. Even though the weight loss was intentional on incretin therapy, a rapid drop in weight, more than 4 kg/month, can still place an individual at risk for malnutrition. Monitoring nutrition status during weight loss pharmacotherapy is essential.
Answer 3 is incorrect About 10.29% of respondents chose this: “An 86-year-old with type 1 diabetes and reported recent decline in activity and strength”. This answer is true but not the best answer. Older adults, especially those with type 1 diabetes, are at greater risk for malnutrition, particularly when they experience declines in physical activity and strength. Malnutrition and sarcopenia, a loss of lean body mass, may develop simultaneously.
Finally, Answer 4 is correct. 74.26% chose this correct answer – GREAT JOB! All these scenarios indicate an increased risk of malnutrition and warrant additional screening. The ADA Standards of Care emphasize screening for malnutrition in individuals who have lost significant weight, especially individuals’ post-metabolic surgery, on incretin therapy, and individuals managing multiple chronic conditions who may experience an increased risk of developing sarcopenia and malnutrition. Check out the 2025 ADA Standards of Care Section 5 and Section 8 for the latest on malnutrition screening recommendations.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on Jan. 30th for our
Standard of Care Course
Level 2
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standard of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
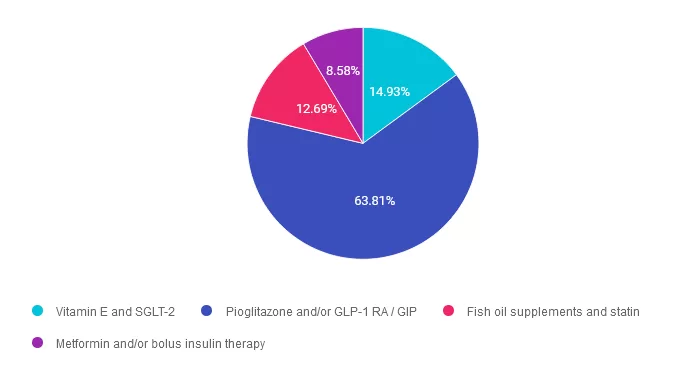
Rationale of the Week | Best Meds to Treat MASH – 2025 Standards
For last week’s practice question, we quizzed participants on best meds to treat MASH. 64% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: In the 2025 ADA Standards, they have updated the term Non-Alcoholic Steatohepatitis (NASH) to Metabolic Associated Steatohepatitis (MASH). They also recommend pharmacologic agents along with lifestyle interventions to treat people with diabetes and MASH.
Which of the following are the recommended diabetes medications to treat MASH?
Answer Choices:
- Vitamin E and SGLT-2
- Pioglitazone and/or GLP-1 RA / GIP
- Fish oil supplements and statin
- Metformin and/or bolus insulin therapy
Getting to the Best Answer
Answer 1 is incorrect. 14.93% chose this answer. “Vitamin E and SGLT-2.” While SGLT-2’s will help lower glucose levels and may result in some weight loss, the ADA does not recognize it as a treatment for steatosis. As far as Vitamin E, according to the ADA 2025 Standards, “it may be beneficial for the treatment of MASH in people without diabetes. However, in people with type 2 diabetes, vitamin E monotherapy was found to be ineffective in a small RCT, and it did not seem to enhance pioglitazone’s efficacy when used in combination, as reported in an earlier trial in this population.
Answer 2 is correct. 63.81% of you chose this answer. “Pioglitazone and/or GLP-1 RA / GIP.” GREAT JOB, this is the best answer. According to the ADA Standards In adults with type 2 diabetes with biopsy-proven MASH or those at high risk for liver fibrosis (based on noninvasive tests), pioglitazone, a GLP-1 RA, or a dual GIP and GLP-1 RA is preferred for glycemic management because of potential beneficial effects on MASH.
Answer 3 is incorrect. About 12.69% of respondents chose this. “Fish oil supplements and statin.” Part of this answer is correct. Based on the 2025 ADA Standards, “Statin therapy is safe in adults with type 2 diabetes and compensated cirrhosis from MASLD and should be initiated or continued for cardiovascular risk reduction as clinically indicated. In people with decompensated cirrhosis, statin therapy should be used with caution, and close monitoring is needed, given limited safety and efficacy data. However, the ADA does not recommend fish oil supplements to treat MASH.
Finally, Answer 4 is incorrect. 8.58% chose this answer. “Metformin and/or bolus insulin therapy.” Although metformin therapy and insulin are effective at addressing insulin resistance and lower glucose levels, they are not first line recommended agents to treat MASH.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us for this upcoming webinar!
Test Taking Practice Exam Toolkit
Jan. 13th @ 11:30am PST
You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
For many of us, taking the certification exam is a nerve-wracking process
During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | What do the NEW 2025 ADA Standards Say?
For last week’s practice question, we quizzed participants on 2025 ADA Standards & hyperglycemic crises. 43% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: What do the NEW 2025 ADA Standards Say?
According to the Newly Published 2025 Standards of Care, which of the following statements reflect the latest guidelines to treat hyperglycemic crises?
Answer Choices:
- Administer low dose basal insulin analog in addition to intravenous insulin infusion to improve glucose management.
- If serum pH is below 7.4, administer IV bicarb, along with a glucose infusion to resolve severe acidosis.
- To differentiate between DKA and HHS, the most important lab indicators are the anion gap and glucose levels.
- Lactated Ringers is now the preferred intravenous solution for fluid resuscitation.

Getting to the Best Answer
Answer 1 is correct. 43.04% chose this answer. “Administer low dose basal insulin analog in addition to intravenous insulin infusion to improve glucose management.” YES, great job, this is the best answer. According to ADA Standard 16 on Hospital Care, “Studies have reported that the administration of a low dose of basal insulin analog in addition to intravenous insulin infusion may prevent rebound hyperglycemia without increased risk of hypoglycemia.”
Answer 2 is incorrect. 19.59% of you chose this answer. “If serum pH is below 7.4, administer IV bicarb, along with a glucose infusion to resolve severe acidosis.” Since this pH is in the normal range, this person is not in ketoacidosis. According to ADA Standard 16 on Hospital Care, “Several studies have shown that the use of bicarbonate in people with DKA made no difference in the resolution of acidosis or time to discharge, and its use is generally not recommended.”
Answer 3 is incorrect. About 20.10% of respondents chose this. “To differentiate between DKA and HHS, the most important lab indicators are the anion gap and glucose levels.” According to the 2024 Consensus Statement, to differentiate between the two conditions, the most decisive lab indicators are beta hydroxybutyrate or urine ketones to verify insulin deficiency along with pH levels to verify acidosis and osmolality to determine hydration status in HHS.
Finally, Answer 4 is incorrect. 17.27% chose this answer. “Lactated Ringers is now the preferred intravenous solution for fluid resuscitation.” According to the 2024 Consensus Statement, Normal saline or Ringer’s lactate are both accepted IV rehydration solutions.
You are invited to register for our Hyperglycemic Crises – New criteria and treatment guidelines for DKA, Euglycemic DKA and HHS | 1.25 CE – Recorded and Ready for Viewing.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on Jan 30, 2025 for our
ADA Standards of Care
Level 2 | Standards of Care Intensive
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standard of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
Objectives:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
Learning Outcome: Participants will identify updates and articulate recommendations from the 2024 ADA Standards of Care that can be applied to their practice.
Target Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
Why Attend These Webinars?
- Accessible learning: All webinars are available online, so you can attend from the comfort of your home or office.
- Expert-led: Presentations are led by experienced diabetes educators, healthcare professionals, and researchers.
- Practical advice: Each session is designed to give you actionable strategies that can be applied in your daily life or practice.
- Up-to-date information: Stay informed about the latest research, guidelines, and technology in diabetes care.
How to Register?
Register above or simply visit our website.
For more information or any questions, please email [email protected].
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
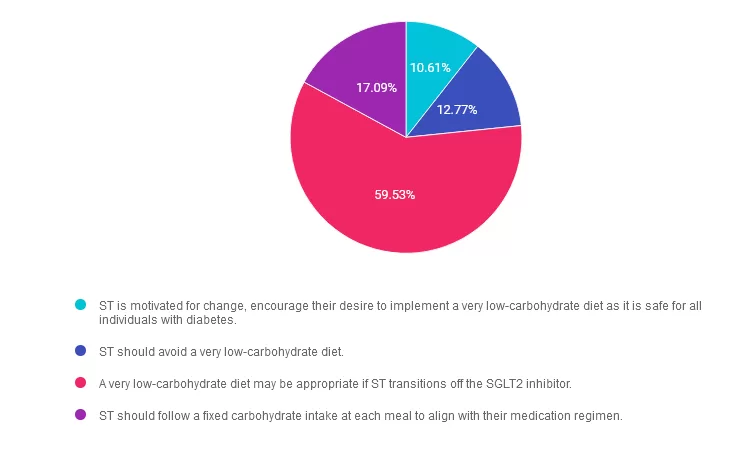
Rationale of the Week | Low carb diets and SGLT-2’s a good mix?
For last week’s practice question, we quizzed participants on SGLT-2’s & low carb diets. 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: ST is a 56-year-old presenting for MNT and diabetes education. Their last A1c was 7.4%, and they are currently taking 1000 mg of Metformin and 10 mg of empagliflozin daily for glucose management. They recently read that a very low-carbohydrate eating pattern can help individuals with type 2 diabetes reduce A1C and the need for additional medications and are motivated to implement diet changes.
What would be your primary considerations and guidance in response to ST?
Answer Choices:
- ST is motivated for change, encourage their desire to implement a very low-carbohydrate diet as it is safe for all individuals with diabetes.
- ST should avoid a very low-carbohydrate diet.
- A very low-carbohydrate diet may be appropriate if ST transitions off the SGLT2 inhibitor.
- ST should follow a fixed carbohydrate intake at each meal to align with their medication regimen.
Getting to the Best Answer
Answer 1 is incorrect. 10.61% chose this answer. “ST is motivated for change, encourage their desire to implement a very low-carbohydrate diet as it is safe for all individuals with diabetes.” While very-low-carbohydrate diets has evidence for reducing A1c and need for additional medications, they may not be universally safe for all individuals. Keep reading to learn more.
Answer 2 is incorrect. 12.77% of you chose this answer. “ST should avoid a very low-carbohydrate diet.” A very-low-carbohydrate diet is not inherently contraindicated for individuals with diabetes, but careful planning and potential discontinuation of the SGLT2 inhibitor is recommended to reduce the risk of euglycemic ketoacidosis.
Answer 3 is correct. About 59.53% of respondents chose this. “A very low-carbohydrate diet may be appropriate if ST transitions off the SGLT2 inhibitor.” Use SGLT2 inhibitors with caution when implementing a low carbohydrate diet and strong consideration should be made to cease this medication if implementing a very low carbohydrate diet, less than 50 grams of carbohydrate per day. Very low carbohydrate diets may increase the risk of euglycemic ketoacidosis by lowering insulin levels. After additional clinical review, a very-low-carbohydrate diet can be considered for ST if they transition off the SGLT2 inhibitor. Educating ST about the difference between physiological ketosis and pathological ketoacidosis may also be considered.
Finally, Answer 4 is incorrect. 17.09% chose this answer. “ST should follow a fixed carbohydrate intake at each meal to align with their medication regimen.” While fixed carbohydrate intake can sometimes simplify diabetes management, it does not align with ST’s interest in very-low-carbohydrate eating patterns. The current medication regimen does not necessarily require a fixed carbohydrate plan. Simply educating on this approach without additional shared decision making may not provide an individualized dietary intervention.
Reference: American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement_1): S77–S110. https://doi.org/10.2337/dc24-S005
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Check out these upcoming class offerings!
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | A1C 13.6% – Next Important Step?
For last week’s practice question, we quizzed participants on what steps to address an elevated A1C. 56% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KT is a 17-year-old with newly diagnosed diabetes and an A1C of 13.6%. The provider starts KT on 30 units of basal insulin and 10mg empagliflozin (Jardiance). KT is asked to get C-peptide levels checked and their C-peptide level is 0.9 ng/mL.
Based on this information, what is the next most important step?
Answer Choices:
- Add bolus insulin and stop empagliflozin
- Discuss the importance of starting CGM
- Evaluate auto immune markers
- Decrease basal insulin and start metformin

Getting to the Best Answer
Answer 1 is incorrect. 20.78% chose this answer. “Add bolus insulin and stop empagliflozin.” Since KT’s c-peptide level is 0.9ng/mL, it is between the normal range of 0.5 and 2.0 nanograms per milliliter (ng/mL). This means there is no urgent need to start KT on basal bolus insulin therapy, as long as we have basal insulin on board and we are monitoring blood glucose levels. According to ADA Standards, we can continue both the basal insulin and Jardiance and even consider adding metformin or a pediatric approved GLP-1 RA. Once we have the type 1 antibody results, we can determine best path forward.
Answer 2 is incorrect. 14.29% of you chose this answer. “Discuss the importance of starting CGM.” While it is important to monitor glucose levels, this is not the MOST important next step. To determine if KT has type 1 diabetes, we quickly need to evaluate if they are experiencing autoimmunity by testing for these; autoantibodies to insulin, GAD, islet antigen 2, ZnT8. If one or more of these comes back positive, it verifies KT has immune mediated type 1 diabetes and has a clear indication for basal bolus insulin therapy.
Answer 3 is correct. About 56.40% of respondents chose this. “Evaluate auto immune markers.” YES, GREAT JOB. This is the best answer. Since KT’s C-peptide is within the normal range, we need to evaluate immune markers. To determine if KT has type 1 diabetes, we quickly need to evaluate autoimmunity by testing for; autoantibodies to insulin, GAD, islet antigen 2, ZnT8. If one or more of these comes back positive, it verifies KT has immune mediated type 1 diabetes and is an indication for basal bolus insulin therapy.
Finally, Answer 4 is incorrect. 8.53% chose this answer. “Decrease basal insulin and start metformin.” Given that KT’s C-peptide is in normal range, we certainly could consider adding metformin and decreasing basal insulin. However, KT may still be in the honey moon phase and may be producing some insulin. For this reason, to determine if KT has type 1 diabetes, we quickly need to evaluate autoimmunity by testing for; autoantibodies to insulin, GAD, islet antigen 2, ZnT8. If one or more of these comes back positive, it verifies KT has immune mediated type 1 diabetes and is an indication for basal bolus insulin therapy.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on December 17, 2024 for our
Meds Management Update for Type 2 Diabetes
Level 2 Standards of Care Intensive

In this exciting webinar, Coach Beverly walks participants through the “Management of Hyperglycemia in Type 2 Diabetes” as outlined by the most recent American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes guidelines. She kicks it off with a brief overview of the different classes of medications and then uses a case study approach to apply the ADA algorithm.
Objectives:
- Describe the role of Diabetes Care & Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate & adjust oral & injectable therapy using a person-centered approach.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 2 | Meds Management Update for Type 2 Diabetes awards 1.5 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
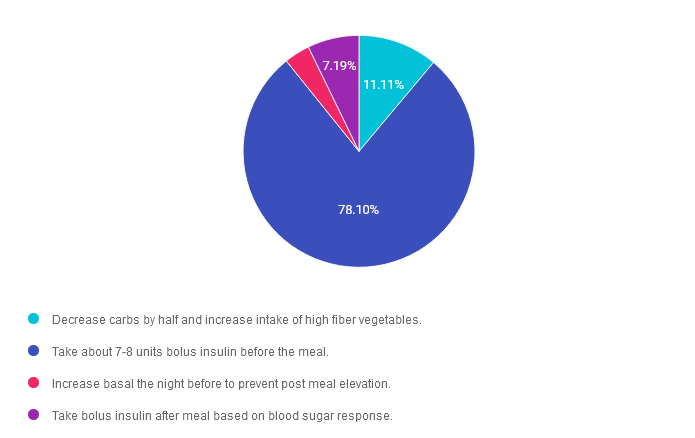
Rationale of the Week | Best Action to Avoid Thanksgiving Post Meal Elevation?
Happy Thanksgiving everyone!
For last week’s practice question, we quizzed participants on avoiding Thanksgiving post meal elevation. 78% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

 Question: JR is excited about enjoying Thanksgiving with family but is a little worried about post-Thanksgiving meal blood sugar elevations. JR takes 1 unit bolus insulin for every 10 gms of carb, with a correction factor of 1 unit for every 50 points above 120, plus 23 units of basal insulin at night. For Thanksgiving JR plans to eat:
Question: JR is excited about enjoying Thanksgiving with family but is a little worried about post-Thanksgiving meal blood sugar elevations. JR takes 1 unit bolus insulin for every 10 gms of carb, with a correction factor of 1 unit for every 50 points above 120, plus 23 units of basal insulin at night. For Thanksgiving JR plans to eat:
- 1 cup of mashed potatoes
- Spoonful of green beans
- Gravy
- 1 Roll with lots of butter
- ½ cup of sweet potatoes
- Turkey leg
- A glass of white wine
If JR’s blood Sugar is 173 before the meal, what is the best approach?
Answer Choices:
- Decrease carbs by half and increase intake of high fiber vegetables.
- Take about 7-8 units bolus insulin before the meal.
- Increase basal the night before to prevent post meal elevation.
- Take bolus insulin after meal based on blood sugar response.
Getting to the Best Answer
Answer 1 is incorrect. 11.11% chose this answer. “Decrease carbs by half and increase intake of high fiber vegetables.” Although it is always a great idea to start the meal with high fiber foods to help regulate post meal glucose, we are not big fans of asking JR to reduce their carb intake by half on Thanksgiving. As long as JR takes adequate bolus insulin before the meal, they can enjoy Aunt Martha’s mashed potatoes and some of their favorite stuffing too.
Answer 2 is correct. 78.10% of you chose this answer. “Take about 7-8 units bolus insulin before the meal.” YES, this is the best answer. Trying to gauge exactly how much carbs is in a holiday meal is challenging, but it appears that this meal contains about 65-80 gms of carb. Since JR takes 1 unit of insulin for every 10 gms of carb, they will need about 7-8 units of insulin to cover this holiday feast.
Answer 3 is incorrect. About 3.59% of respondents chose this. “Increase basal the night before to prevent post meal elevation.” This isn’t the best answer, because increasing the basal the night before might cause morning hypoglycemia and isn’t designed to cover post meal elevations.
Finally, Answer 4 is incorrect. 7.19% chose this answer. “Take bolus insulin after meal based on blood sugar response.” Since JR is worried about post meal glucose elevations, the most effective strategy to prevent that from happening is to take the insulin bolus at least 15 minutes before the meal.
Happy Thanksgiving everyone! We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!