Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Diabetes Tech and Distress
The world of diabetes technology is advancing at a record pace. There is no doubt that technology intends to make life with diabetes a bit easier. In the United States, over 50% of adults living with diabetes have experienced some level of diabetes distress.¹ The impact of diabetes technology on mental well-being is complicated. Diabetes technology, including insulin pumps, continuous glucose monitors (CGMs), and connected insulin pens, can either lessen or aggravate diabetes distress.

Understanding Diabetes Distress
The American Diabetes Association (ADA) defines diabetes distress as “significant negative psychological reactions related to emotional burdens and worries specific to an individual’s experience in having to manage a demanding chronic condition such as diabetes.”.² Diabetes distress is a natural reaction to the daily burden of managing diabetes. Signs of diabetes distress can include avoiding blood glucose monitoring, omitting medications, and struggling to achieve personal hemoglobin A1c targets.
The ADA recommends screening for diabetes distress at least annually. More frequent screening is recommended if clients are not meeting treatment goals, develop diabetes-related complications, and during times of life transitions.²
To access these validated diabetes distress screening tools in English and Spanish, I encourage you to visit this helpful website, DiabetesDistress.org
- Diabetes Distress Scale (DDS-17)
- Type 1 Diabetes Distress Scale (T1-DDS)
- The Type 2-Diabetes Distress Assessment System (T2-DDAS)
Can Technology Improved Diabetes Distress?
Let’s explore how diabetes technology can have a positive impact on diabetes distress.
✅ CGMs: With current CGMs, fewer fingerstick readings are needed to make treatment decisions. CGMs provide information on blood glucose trends and impending hyperglycemia or hypoglycemia, creating more peace of mind.
✅ Record Keeping: Various forms of diabetes technology can log blood glucose values, insulin doses, site changes, and total daily doses of insulin. This eliminates the need for clients to worry about detailed record-keeping.
✅ Automated Insulin Delivery: Automated insulin pumps can decrease decision fatigue by making automated adjustments to both basal and correction insulin doses. This approach to insulin delivery can also benefit individuals with an active lifestyle. Utilizing wearable insulin delivery devices and algorithms can reduce the mental burden of diabetes self-management.
✅ Connectivity: Remote data sharing supports communication with parents, caregivers, and friends to create a diabetes support team. Connectivity with healthcare providers enhances communication with the care team, allowing adjustments to treatment plans between clinic visits.
✅ Empowerment: The data trends can empower individuals living with diabetes to take control and gain confidence in making and evaluating medication and lifestyle adjustments in response to changes in glycemic control.
Can Technology Worsen Diabetes Distress?
As diabetes healthcare professionals, it is important to understand how diabetes technology can negatively impact diabetes distress.
❌ Information Overload: Diabetes technology generates an enormous amount of data. This can cause distress by constantly feeling the need to monitor glucose trends and numbers throughout the day and night, leading to feelings of anxiety and overwhelm.
❌ Alarms: Alarms on diabetes technology are rooted in safety, but for those living with these devices, this can lead to diabetes distress. Alarms can disrupt sleep or bring unwanted attention from others in public. Erroneous alarms for hyperglycemia or hypoglycemia can cause stress, frustration, and alarm fatigue.
❌ Perfectionism: Diabetes technology provides a continuous insight into glycemic control, which for some can create a need for perfection. Some clients feel like they fail when they don’t reach their time-in-range goal each day.
❌ Physical Impact: Wearable devices not only carry a psychological burden but can also cause physical distress. Skin irritation and allergic reactions to adhesives cause physical pain and embarrassment. Those who wish to keep diabetes private, wearing a CGM, insulin pump, or other wearable device that puts diabetes on display, causing distress.
❌ Technical issues: Losing connectivity with CGMs or an AID system can cause frustration and make it challenging to achieve optimal glycemic control. Insurance coverage, prior authorizations, out-of-pocket costs, and access to supplies for diabetes technology can all contribute to or worsen diabetes distress.
Diabetes Healthcare Professionals Help – Recognize and Address
The 7A’s Framework provides a useful interview tool when assessing for Diabetes Distress:
- Aware: Be aware of diabetes distress.
- Ask: Ask about diabetes distress.
- Assess: Use a validated screening tool for assessment.
- Advise: Explain diabetes distress.
- Assist: Develop an action plan.
- Assign: If you are not equipped to help, assign the client to another healthcare professional.
- Arrange: Set up follow-up as needed. 3
Here are some other actionable tips you can use to help those with diabetes distress:
- Refer clients to local or virtual diabetes support groups.
- Discuss with clients that diabetes distress is common and not a character flaw or failure
- Collaborate to choose the best technology based on their technology readiness, skill level, and comfort level.
- Set realistic goals for time-in-range and other data metrics.
- Educate clients on how to troubleshoot their devices regarding alarms or connectivity issues.
- Support a healthy relationship with diabetes tech.
References
Alexander, D.S., Saelee, R., Betsy Rodriguez, B., Koyama, A. K., Cheng, Y. J., Tang, S., Rutkowski, R. E., & Bullard, K. M. (2025). Diabetes distress among US adults with diagnosed diabetes, 2021. Preventing Chronic Disease: Public Health Research, Practice, and Policy, 22(E07), 1-7. https://www.cdc.gov/pcd/issues/2025/24_0287.htm#:~:text=Among%20US%20adults%20with%20diabetes%2C%20an%20estimated%201.6%20million%20(6.6,income%20compared%20with%20their%20counterparts.
- American Diabetes Association Professional Practice Committee. (2025). Facilitating positive health behaviors and well-being to improve health outcomes: Standards of care in diabetes—2025. Diabetes Care, 48(Supplement_1): S86–S127. https://diabetesjournals.org/care/article/48/Supplement_1/S86/157563/5-Facilitating-Positive-Health-Behaviors-and-Well?searchresult=1
- American Diabetes Association. (n.d.). Professional development: Behavioral health toolkit. https://professional.diabetes.org/professional-development/behavioral-mental-health/behavioral-health-toolkit
- Healing through Connection for Healthcare Professionals by Beverly Thomassian
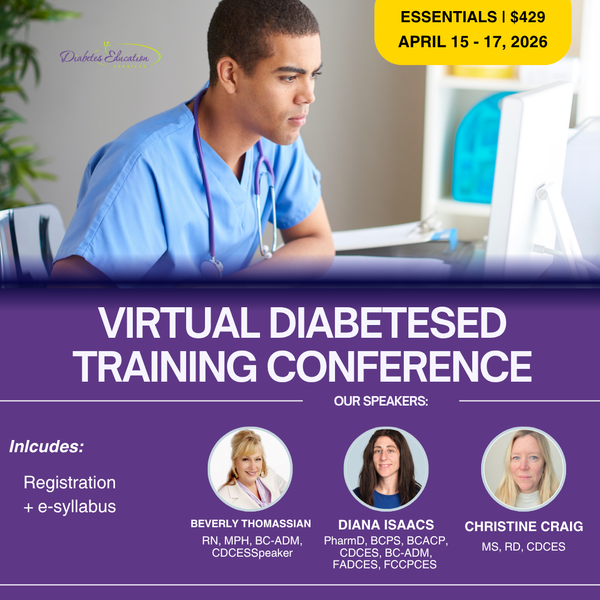
Learn More From the Experts:
Coach Beverly Thomassian, Dr. Diana Isaacs, & Christine Craig
Virtual DiabetesEd Training Conference | April 15th-17th, 2026
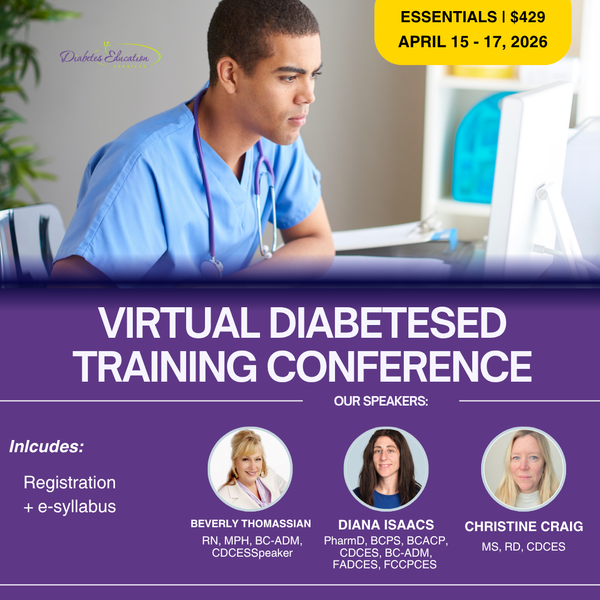
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
Registration Options at a Glance
- 📜 Essentials: Includes registration and electronic syllabus.
- 🌟 Deluxe: Includes registration, electronic syllabus, and the ADA Standards Book for deeper study.
- 🏆 Complete: Best value! Includes everything listed above, plus the ADCES Review Guide of over 400 practice questions for exam prep.
Registration Fee includes
- 🎤 3 days of engaging, expert-led education
- 📘 100-page electronic syllabus +
- 🎓 12 FREE bonus online courses ($375 value) to boost your prep
Question of the Week | Individual vs. Group DSMES
After the initial assessment JM is scheduled for an individual visit instead of a group DSMES class.
According to Medicare guidelines, which of the following would NOT justify providing individual DSMES instead of group DSMES?
- When scheduling, JM requested an individual appointment
- The referral for DSMES stated JM has a language barrier
- A group DSMES class is not available within the next 3 months
- JM was referred for training on starting insulin therapy
Prepare for the CDCES Exam
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Prepare for the BC-ADM Exam

Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our comprehensive BC-ADM Online Study Programs are specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe BC-ADM Boot Camp Bundle include:
- Levels 2, 3, and 4 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
Registration Options at a Glance
- 📜 Essentials: Includes registration and electronic syllabus.
- 🌟 Deluxe: Includes registration, electronic syllabus, and the ADA Standards Book for deeper study.
- 🏆 Complete: Best value! Includes everything listed above, plus the ADCES Review Guide of over 400 practice questions for exam prep.
Registration Fee includes
- 🎤 3 days of engaging, expert-led education
- 📘 100-page electronic syllabus +
- 🎓 12 FREE bonus online courses ($375 value) to boost your prep
Making the Connection – Creativity and Health Professionals

Announcements
___________________
- Join a Virtual Conversation and Interview with Coach Bev on Feb 20th at 11:30am PST
- Get FREE Audio Version of Chapter 6 here >>
- Download Free Work Sheet – Exploring Your Creativity.
Healing through Connection for Healthcare Professionals is available in:
- Paperback with quantity discounts for you and your team.
- Audible and Kindle Version on Amazon.
- Write Your Review of Healing through Connection
Some days it’s not easy being a healthcare professional.
- Being present with the pain and suffering of the people in our care.
- Navigating medication coverage and the complexities of insurance companies.
- Advocating for evidence-based care and not being heard or recognized by colleagues.
Like me, I am sure you have experienced moments of intense frustration when you wanted to scream or give up!
Maybe you had to show up when you were emotionally spent and felt like you had nothing else to give.
I see you and I celebrate you—the hardworking healthcare professional who shows up day after day with heart and courage. In my book, Healing through Connection, I honor your journey and share strategies to help you care for your own well-being as you care for others.
Join a Virtual Conversation and Interview with Coach Bev on Feb 20th at 11:30am PST to delve into the healing power of creative endeavors.
If you can’t make the interview, enjoy this excerpt from Chapter 6, that dives into the Healing Power of Self-Expression and encourages you to dive into your creativity for healing, rejuvenation, and pure JOY.
Taking Time for Creativity & Self- Expression
Even if you can only commit to engaging creativity for a few minutes or half an hour a week, it makes a difference. Stop thinking about all the reasons you can’t do it, and instead, listen to that internal hum, get in the metaphorical car, turn on the ignition, and drive.
Within you lives a quiet, creative spark waiting for attention and care. When you tend to it, you renew your capacity to show up with presence, compassion, and strength, for yourself and for those in your care.
Healing through Connection is both a reminder and a roadmap; an invitation to care for yourself with the same compassion you offer others. It provides a rare perspective on mutual healing.
As we heal ourselves, we expand our capacity to help others with healing. Within the pages of this book, you’ll find a toolbox for exploring your truth, tapping into your emotions, and cultivating creativity. Together, we’ll explore the often-overlooked connection between your own lived experiences and those of the individuals in your care.
Continue reading to discover how making time for creative expression might offer you some unexpected benefits and opportunities for joy!
The Healing Power of Creative Expression
Did you know that Nobel Prize recipients are nearly three times more likely to engage in creative hobbies than their scientific counterparts?
Theoretical physicist Albert Einstein often played the violin when he encountered challenges in his theoretical work. He believed that music helped him think creatively and tap into his subconscious, enabling breakthroughs such as the theory of relativity.
Marie Curie, a two-time Nobel laureate for physics in 1903 and chemistry in 1911, went for frequent walks in the countryside, which allowed her to reflect and rejuvenate. These moments of tranquility likely helped her maintain focus during the grueling work of isolating radioactive elements.
Why Are Nobel Prize Winners More Likely to Have Artistic Hobbies?
It’s because they’re simply more open to having hobbies. They are more open to novel experiences and often turn to their creative endeavors when working through challenges. These seemingly unrelated scientific pursuits and personal hobbies can open doors for scientists to crosspollinate ideas across different fields, enabling them to gain fresh perspectives and uncover new insights.
Now, you may not be working toward securing the title of a Nobel laureate. Still, you might be interested in learning the secrets of expanding your mind, creating new connections, and better integrating the two sides of your brain hemispheres to provide better care or nurture your inner life.
You may be wondering how having an artistic hobby or winning a Nobel Prize in science relates to excelling as a diabetes specialist or healthcare professional. As a healthcare professional, you have likely lived through difficult experiences or witnessed profound suffering firsthand.
Plenty of science supports the idea that engaging in creative pursuits offers an outlet to express complex emotions that are not accessible through words alone.
The act of playing an instrument, taking an art class, exploring nature, or playing the bongo drums may provide a gateway to address unrequited trauma or pain, helping you to become more fully aware and present with your feelings. Did you have a childhood or adult hobby you loved doing? One that made you lose track of time as you entered the zone referred to as “flow”? Have you given yourself permission to make time for that hobby and lose yourself in that creative process?
You may want to take a ceramics or writing class, join the local choir, or start a band. Perhaps you found an old camera and want to learn more about photography or realized you’re good at painting. It can be hard to start as a beginner and potentially look silly or unskilled.
Here’s my advice: Let go of those sky-high expectations. No one expects you to paint like Monet in your first art class.
My motto is, if something makes me uncomfortable, I know I’m in the right place—because that’s where growth happens.
I encourage you to take that leap of faith and tolerate the momentary discomfort for long-term gain. It gets better, and before you know it, you will blossom in ways you never expected.
Download this worksheet to explore 20 creative endeavors that may spark inspiration within you. You may already be practicing some of these—or perhaps you have new ideas to add. Wonderful—keep going!
As a dance teacher for the past twenty years who can still balance a sword on her head, I am reminded every day that it is never too late to rediscover your joy.
- You can listen to FREE Audio Version of Chapter 6 here >> on The Power of Self-Expression and Creative Endeavors.
- You can also purchase the entire book, Healing through Connection for Healthcare Professionals in Audible or Kindle by clicking here.
- Download Creativity Worksheet here.
Connection & Interview with Coach Beverly
Healing through Connection on Friday, Feb 20th, 2026 at 11:30 am PST
Coach Beverly is honored to invite you to this special gathering and intimate conversation. During this virtual book launch, a special guest interviewer will join Coach Bev for a heartfelt conversation about why this book matters now and the real stories from clinical practice that inspired it.
Coach Bev will also share the personal journey of writing Healing through Connection and how she discovered her voice along the way. We will conclude with an interactive question-and-answer session and allow time for connection.
Come celebrate connection, healing, and the power of story as we honor the shared human experience at the heart of healthcare.
Thank you for YOUR support and commitment to promoting healing and connection every day!
Rationale of the Week | What Not to Say to Overwhelmed Individual
For last week’s practice question, we quizzed participants on which of the following responses is the least appropriate (i.e., the WRONG thing to say) to Maria. 58.54% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Maria, a 52‑year‑old woman with type 2 diabetes for 8 years, attends a follow‑up visit. Her A1C has risen from 7.8% to 9.2% over the past year. She reports feeling “overwhelmed” and says she didn’t want to start the medication her clinician recommended at the last visit. She explains, “I’m scared of side effects, and I feel like needing medication means I failed.”
Which of the following responses is the least appropriate (i.e., the WRONG thing to say) to Maria?
- “It sounds like you’re feeling overwhelmed. Can you tell me more about what worries you most about starting this medication?”
- “Many people feel this way. Let’s look at your options together so you can make a choice that works for you.”
- “I understand that this is challenging and overwhelming. However, if you don’t start this medication, you are choosing to risk complications like kidney disease or blindness.”
- “It’s completely understandable to have concerns. Would it help if we reviewed what the medication does, talk about the pro’s and the con’s, and about what alternatives exist?”
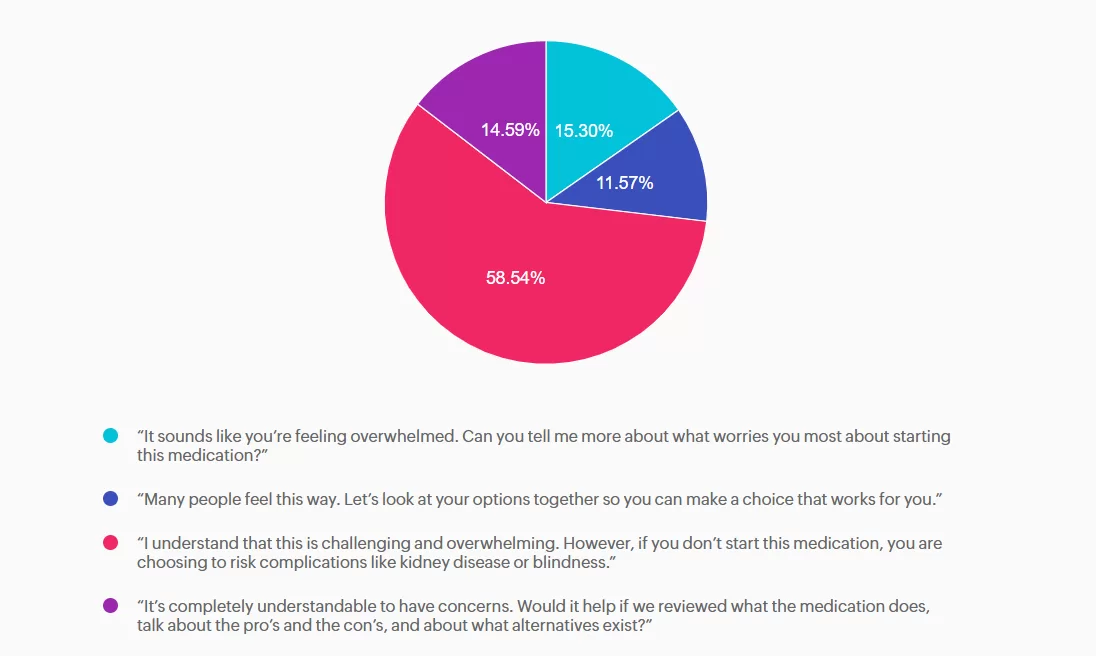
Getting to the Best Answer
Answer A is incorrect: 15.3% chose this answer,“ It sounds like you’re feeling overwhelmed. Can you tell me more about what worries you most about starting this medication?” Appropriate — Person centered, exploratory. This response uses reflective listening and invites the patient to share her concerns. It aligns with ADA Standards of Care recommendations for collaborative communication and supports assessment of diabetes distress.
Answer B is incorrect: 11.57% chose this answer, “Many people feel this way. Let’s look at your options together so you can make a choice that works for you.” Appropriate — Normalizes feelings and supports shared decision making. This option reduces stigma by acknowledging that many people experience similar emotions. It reinforces autonomy and partnership, which are core components of effective diabetes self management support.
Answer C is correct: 58.54% chose this answer, “I understand that this is challenging and overwhelming. However, if you don’t start this medication, you are choosing to risk complications like kidney disease or blindness.” Incorrect — Stigmatizing, blaming, and fear based. This statement uses threat based language (“you are choosing to risk complications…”) and implies personal failure. It increases shame, undermines trust, and can worsen diabetes distress. It does not incorporate person first language or collaborative care or help identify barriers and personalized solutions. Oh, and it probably won’t be very successful!
Answer D is incorrect: 14.59% chose this answer, “It’s completely understandable to have concerns. Would it help if we reviewed what the medication does, talk about the pro’s and the con’s, and about what alternatives exist?” Appropriate — Validates concerns and offers. Information without pressure. This response acknowledges the patient’s emotions and provides an opening for education and shared exploration of options. It supports autonomy and reduces the sense of failure associated with medication use.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn More From The Experts:
William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD
ENGAGING THE DISENGAGED | Live in San Diego at Marina Village
April 18th, 2026 from 9 AM to 4 PM PST!

In this course, William H. Polonsky, PhD, CDCES, and Susan Guzman, PhD, examine the powerful role of psychosocial factors in diabetes self-management. Through innovative strategies, participants will learn how to recognize and address common barriers to effective self-care and cardiometabolic medication initiation and maintenance, while fostering respectful, stigma-free clinical encounters.
Through a collaborative and person-centered approach, the course emphasizes communication strategies that enhance motivation, build confidence, and reinforce the value of self-management. Participants will develop skills in diabetes-focused action planning, addressing medication hesitancy, and providing ongoing support and resources to sustain behavior change over time. The goal is to help clinicians make diabetes care more doable, meaningful, and effective for people living with diabetes.
High Five for Fiber

Dietary fiber is a complex carbohydrate and bioactive food compound that has an important role in diabetes management and cardiometabolic health. High-fiber dietary patterns are associated with a lower risk of type 2 diabetes, cardiovascular disease, obesity, gastrointestinal disorders, and certain cancers. ¹,²
In individuals with diabetes, fiber-rich eating patterns have been shown to improve glycemia, reduce postprandial glucose excursions, and improve lipid profiles. ¹ A recent meta-analysis found that for individuals with type 1 diabetes, a high- fiber diet not only supports A1c reduction but is also associated with reduced hypoglycemia risk due to its role in slowing digestion and absorption. ³ Despite this evidence most adults fail to meet recommended fiber intake guidelines, presenting an opportunity for nutrition interventions.
Dietary Fiber and Diabetes
The Dietary Reference Intake (DRI) for fiber, established by the Institute of Medicine, along with the 2026 ADA Standards of Care ¹ , recommends 14 grams of fiber per 1,000 Calories, corresponding to an Adequate Intake of approximately 25–38 grams per day depending on age, gender, and energy needs. 4 Higher-fiber dietary patterns greater than 35 grams per day ³ and up to 50 grams per day 1 may provide additional glycemic benefits for individuals with diabetes.
Both the 2020–2025 and 2025–2030 Dietary Guidelines for Americans 5 emphasize fruits, vegetables, whole grains, and legumes as primary fiber sources; however, the recommended portions of these food groups differ between guidelines. The newly released 2025–2030 guidelines place greater emphasis on overall dietary patterns and whole-food sources, with reduced total grain servings, increased emphasis on legumes, and a prioritization of reduced processed foods rather than focusing on fiber as an isolated nutrient.
However, the Scientific Report of the guidelines does reference an optimal fiber intake range of 25–29 grams per day. ² Aligning with ADA Standards of Care, the focus shifts from individual nutrients to overall eating patterns, supporting health professionals to encourage food choices that help individuals meet evidence-based guidelines for fiber recommendations.
Disparities Occurring With Dietary Fiber Intake
Despite serving-size guidance and scientific evidence on the benefits of fiber, average intake in the United States remains far below recommendations. Fewer than 5-7% of adults meet daily fiber requirements. 5 Disparities in intakes among groups have grown over time, with data from the 2017–2018 USDA Economic Research Service showing that, within Hispanic populations, fiber consumption was highest at about 9 grams per 1,000 Calories, compared with
7.7 grams per 1,000 Calories among non-Hispanic White individuals, and 7.0 grams per 1,000 Calories among Black individuals 6 .
Although the amount varies across groups, most individuals reach only 58% of the daily fiber recommendations. Inadequate intake stems from not only food preferences but tolerance, food cost and access, time constraints, nutrition literacy, as well as, other social determinants of health. To help the U.S. population meet fiber goals, practical strategies consider not only culturally relevant nutrition interventions but food assistance programs, systems planning, and community resources that improve access to fiber-rich foods.
Understanding Fiber: “Good Source” Versus “Excellent Source”
Therapeutically, the type of fiber matters, with insoluble or soluble providing different health benefits. Insoluble fiber creates bulk within the stool and can promote bowel regularity and reduces risk of certain cancers. Whereas, soluble fiber forms a viscous gel in the gastrointestinal tract and provides metabolic benefits, including reduced postprandial glucose responses and lower cholesterol levels. 7
While not specific to type, understanding fiber claims on food labels is a practical entry point for guiding individuals toward higher-fiber food choices. According to FDA labeling regulations, foods may be labeled a “good source” of fiber if they provide 10–19% of the Daily Value per serving (≥3 grams), while an “excellent source” of fiber provides greater than or equal to 20% of the Daily Value per serving (≥5 grams). 8
Additionally, the FDA has approved the use of “will reduce the risk of coronary heart disease” health claims
on food packaging due the cardioprotective effects of high soluble fibers β-glucan (found in oats and barley) and psyllium. 9 Emphasizing dietary patterns, food quality assessment, label literacy, and considerations for additional functional fiber supplementation can support individuals with diabetes to make informed food choices and shifts in their intake.
Practical Strategies & Ideas to Implement Higher Fiber Intake
Practical strategies to promote higher fiber intake are outlined in the 2026 ADA Standards of Care¹ (Check out Nutrition Behaviors to Encourage ¹ within section 5: Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes) and can be reinforced through simple, actionable “High-Five for Fiber” tips.
These tips are a catchy way to encourage health behaviors that may help individuals gradually add fiber (slow addition improves gut tolerance) to meet daily recommendations. Ideas can include having individuals choose at least one “high- fiber, excellent source” daily (which has more than 5 g fiber per serving), discover high soluble fiber foods, strive for five, or more, servings from vegetables and/or fruits each day, and/or “take five” to plan meals that include whole grains, fruits, vegetables, legumes, and/or nuts and seeds each week. These tips encourage choice, helping individuals find foods that fit their personal preferences, affordability, cultural traditions, and lifestyles ¹ while supporting sustainable, health-promoting dietary patterns.
High-Five Food Ideas:
- Chickpeas (6 grams per ½ cup cooked)
- Black beans (6 grams per ½ cup cooked)
- Lentils (8 grams per ½ cup cooked)
- Black-eyed peas (5 grams per ½ cup cooked)
- Raspberries (8 grams per 1 cup)
- Blackberries (8 grams per 1 cup)
- Avocado (6 grams per ½ medium)
- Brussels sprouts (5 grams per 1 cup cooked)
- Artichoke (6 grams per ½ medium cooked)
- Boiled collard greens (5 grams per 1 cup cooked)
- Chia seeds (6 grams per 2 tablespoons)
- Barley (6 grams per 1 cup cooked)
- Whole wheat pita (~ 5 grams fiber per 1 pita)
References:
- American Diabetes Association Professional Practice Committee for Diabetes. 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2026. Diabetes Care 1 January 2026; 49
(Supplement_1): S89–S131. https://doi.org/10.2337/dc26-S005 - Guo Y, Li M, Huang Y. Association of dietary fiber intake with all-cause and cardiovascular mortality in U.S. adults with metabolic syndrome: NHANES 1999–2018. Front Nutr. 2025;12:1659000. doi:10.3389/fnut.2025.1659000.
- Zeng J, Beck M, Barouti AA, Löfvenborg JE, Carlsson S, Lampousi AM. Effects of different dietary patterns on glucose management in type 1 diabetes: a systematic review and meta-analysis of randomized controlled trials. EClinicalMedicine. 2025 Apr 28;83:103222. doi:10.1016/j.eclinm.2025.103222.
- Institute of Medicine (US) Committee to Review Dietary Reference Intakes. Summary Tables. Washington, DC: National Academies Press (US); 2011. Accessed January 18, 2026. https://www.ncbi.nlm.nih.gov/books/NBK56068/table/summarytables.t4/?report=objectonly
- U.S. Department of Health and Human Services (HHS) & U.S. Department of Agriculture (USDA) (2026). Dietary Guidelines for Americans, 2025–2030.
- Guthrie J, Lin BH, Smith TA. Food Consumption and Nutrient Intake Trends Emerge Over Past Four Decades. U.S. Department of Agriculture, Economic Research Service. August 28, 2024. Accessed January 18, 2026. https://www.ers.usda.gov/amber-waves/2024/august/food-consumption-and-nutrient-intake-trends-emerge-over-past-four-decades/
- McRorie JW Jr, McKeown NM. Understanding the Physics of Functional Fibers in the Gastrointestinal Tract: An Evidence-Based Approach to Resolving Enduring Misconceptions about Insoluble and Soluble Fiber. J Acad Nutr Diet. 2017
Feb;117(2):251-264. doi: 10.1016/j.jand.2016.09.021. - Food and Drug Administration, Department of Health and Human Services. 21 CFR § 101.54: Nutrient Content Claims for “Good Source,” “High,” “More,” and “High Potency.” Electronic Code of Federal Regulations. Updated through December 31, 2025. Accessed January 18, 2026. https://www.ecfr.gov/current/title-21/chapter-I/subchapter-B/part-101/subpart-D/section-101.54
- U.S. Food and Drug Administration. Authorized Health Claims That Meet the Significant Scientific Agreement (SSA) Standard. FDA. Accessed January 18, 2026.
https://www.fda.gov/food/nutrition-food-labeling-and-critical-foods/authorized-health-claims-meet-significant-scientific-agreement-ssa-standard
Learn More With Upcoming Webinars & Spreading the Love Sale!
Prepare for the CDCES Exam: Get Ready for Success!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Get exam-ready with confidence.
Our CDCES Boot Camp Online Prep Bundle is a comprehensive, high-impact program built specifically for healthcare professionals preparing for the Certified Diabetes Care and Education Specialist (CDCES) exam who want to level-up their clinical knowledge and skills.
✔ Learn at your pace with expert-led, exam-focused content
✔ Everything you need—organized, practical, and in one place
✔ Perfect for self-directed learners who want complete, person-centered content for clinical practice and exam prep.
✔ Build knowledge, sharpen test-taking skills, and prepare with confidence—on your schedule.
Focused. Flexible. Proven.
Basic & e-Deluxe CDCES Boot Camp Bundle Includes:
- Levels 1, 2, and 3 of our Online University
- 30+ expert-led courses
- 50 CE/CPEUs
- 400+ online practice questions
- Handouts, podcast, video and one year access—all in one streamlined platform.
Spreading the Love Sale
Save 15% on ALL of Our Online Courses
Use the Code "LOVE15" for 15% Off at Checkout!
Sale Ends on February 16th, 2026!
The Healing Shift: How a Chinese Restaurant Became My Refuge
By: Beverly Thomassian
Gung Hay Fat Choy.
Every Chinese New Year brings a wave of gratitude for Alex and Ying, who welcomed an akward 14-year-old into their family-style restaurant and made her feel loved and cared for. Their generosity and belief in me left a lasting imprint on my heart.
I invite you to enjoy this excerpt from my recent book Healing through Connection for Healthcare Professionals. Join Coach Beverly for an intimate virtual interview on the writing of this book on Feb. 20 at 11:30am PST.

When I was fourteen and a half, I found refuge in an unexpected place—a small Chinese restaurant tucked between a Kinney Shoe Store and an Italian eatery in a strip mall in the San Fernando Valley. While my home life was unraveling, I was quietly being stitched back together behind the counter at Ying’s Kitchen.
I didn’t know it then, but this restaurant would do more than offer me a paycheck. It would shape my work ethic, show me what being part of a team meant, and serve as a foundation for the healthcare professional I would one day become. In that busy kitchen filled with the scent of onions and sizzling oil, I learned the beauty of hard work—and the profound healing that comes when someone believes in you.
Finding Refuge in Ying’s Kitchen
As the latest in the long line of high school girls, my job was to answer phones, bag the food, ring up the orders, and answer customer questions for $1.25 an hour. Barely a teenager with no restaurant experience, I approached my assigned tasks with a combination of diligence and confusion.
Early on, I stumbled. Anne, a high school senior in charge of training me, told me, in no uncertain terms, that I was “not keeping pace with the training program, and they might let me go.” This awkward coaching session is seared into my brain. It pushed me into high gear, and I became determined to be the best Ying’s Kitchen employee ever! That moment lit a fire in me. I doubled down, became the fastest phone answerer in the West Valley, and soon trained the new hires myself. It was more than pride, it was survival. A sense of belonging, and a safe place to grow.
Beyond being my employers, Alex and Ying looked out for me. Alex asked me about my day at school and practiced Chinese with me. Before closing, he would ask me if I was hungry. My favorites were the pork fried rice and the egg rolls, and on special nights, he would make me moo goo gai pan. During the summer, Alex coached me on the importance of drinking hot water to cool down. He asked me about my boyfriends and made sure I was keeping up with my homework. Best of all, he always smiled, showing his one gold tooth when I walked through the door.
His wife, Ying, only spoke a few words of English, but she had a way of letting me know she saw me. During springtime, she would call me over and take one strand of my hair, wrapping it carefully around a Jasmine flower from her yard. As I walked through my work shift, I could smell the scent of jasmine and know that I had a found family who treasured me.
Post-Traumatic Growth in Practice
In their book What Happened to You, Oprah Winfrey and Dr. Bruce Perry describe how post-traumatic growth can emerge when safe adults and healing relationships interrupt a cycle of pain. I am living proof of that truth.
Working at Ying’s Kitchen didn’t erase the pain of my past, but it gave me the structure, accountability, and connection I needed to believe in a future beyond it. It became the cornerstone of how I eventually built Diabetes Education Services—a company whose mission is rooted in decreasing shame and blame in diabetes care. The resilience, empathy, and grit that carried me through adolescence now fuel my passion for advocating person-centered, trauma-informed healthcare.
What This Means for Healthcare Professionals
As healthcare professionals, we may look for sophisticated solutions to complex human problems. But sometimes, the most transformative interventions are also the simplest: a steady routine, a safe space, and someone who believes in you.
This is especially true for people living with diabetes and other chronic conditions. Many carry unspoken histories of trauma. When we show up with kindness, curiosity, and consistency, we’re not just delivering care—we’re becoming part of someone’s healing journey.
Whether you’re precepting a student, mentoring a colleague, or counseling a patient, consider the ripple effect of your presence. Like Alex and Ying, you might be offering more than a service—you could be anchoring someone in a storm.
From Survival to Service
Looking back, I see how Alex and Ying laid the groundwork for how I lead today. Those years at Ying’s Kitchen profoundly shaped how I built and now manage my company. The lessons of diligence and love became my guiding light, helping me navigate even the roughest waters and steer my ship toward calmer horizons. The discipline I learned behind that counter still guides how I show up—whether teaching a course, writing a book, or sitting with someone in their hardest moment.
While my early life was shaped by adversity, the safe haven of Ying’s Kitchen taught me that healing often begins with being seen. That’s something we can all offer, no matter our title or training.
Sometimes, the most profound lessons in healing don’t come from textbooks—they come from trusted adults, jasmine flowers, and the quiet grace of being loved into wholeness.
Healing through Connection by Coach Beverly Thomassian now available in print, Audible and Kindle versions.
Paperback version with quantity discounts for you and your team
Audible and Kindle Version on Amazon
Write Your Review of Healing through Connection Here>>
Why Join?
Because you deserve a space to rest, reflect, and reconnect — not just with others, but with yourself. Together, we can remind one another of the humanity behind the healthcare, and rediscover the power of connection in healing.
Your presence matters. Your story matters. And we’re honored to walk this journey with you.
💖 Thank you for being a part of Healing Through Connection.
Join Coach Beverly for a Virtual Interview and Heartfelt Conversation
Feb. 20th at 11:30.
“Healing Through Connection for Health Care Professionals.”
Coach Beverly is thrilled to invite you to this special gathering and celebration. During this virtual book launch, a special guest interviewer will join Coach Bev for a heartfelt conversation about why this book matters now and the real stories from clinical practice that inspired it.
Coach Bev will also share the personal journey of writing Healing through Connection and how she discovered her voice along the way. We will conclude with an interactive question-and-answer session and allow time for connection.
Come celebrate connection, healing, and the power of story as we honor the shared human experience at the heart of healthcare.
Question of the Week | TIR (Time of Range) of 89% – What Is Your Concern?
JZ is proud of their Time of Range of 89%. You notice their time below range is 7%. JZ uses a rapid-acting insulin pen 4–6 times daily to keep glucose in target range and occasionally increases the glargine dose when evening glucose is elevated.
What is your primary concern?
- Is JZ consistently rotating injection sites to prevent lipohypertrophy?
- What is JZ’s rationale for adjusting the glargine dose?
- How is JZ feeling about their frequency of hypoglycemia?
- Does JZ adjust insulin for physical activity?
Learn More From The Experts:
Coach Beverly Thomassian, Dr. Diana Isaacs, & Christine Craig
Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Rationale of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
For last week’s practice question, we quizzed participants on which feature most strongly supports a diagnosis of hyperosmolar hyperglycemic state (HHS) rather than diabetes ketoacidosis (DKA). 59.77% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

A 32-year-old with newly discovered diabetes is brought to the emergency department with polyuria and lethargy. They have been sleeping more than usual.
Initial labs show:
- Plasma glucose: 680 mg/dL
- Potassium 3.7 mEq/L
- Serum osmolality: 335 mOsm/kg
Based on the following labs, which feature most strongly supports a diagnosis of hyperosmolar hyperglycemic state (HHS) rather than diabetes ketoacidosis (DKA)?
- Markedly elevated plasma glucose
- Absence of significant metabolic acidosis
- Out of range potassium level
- Elevated effective serum osmolality
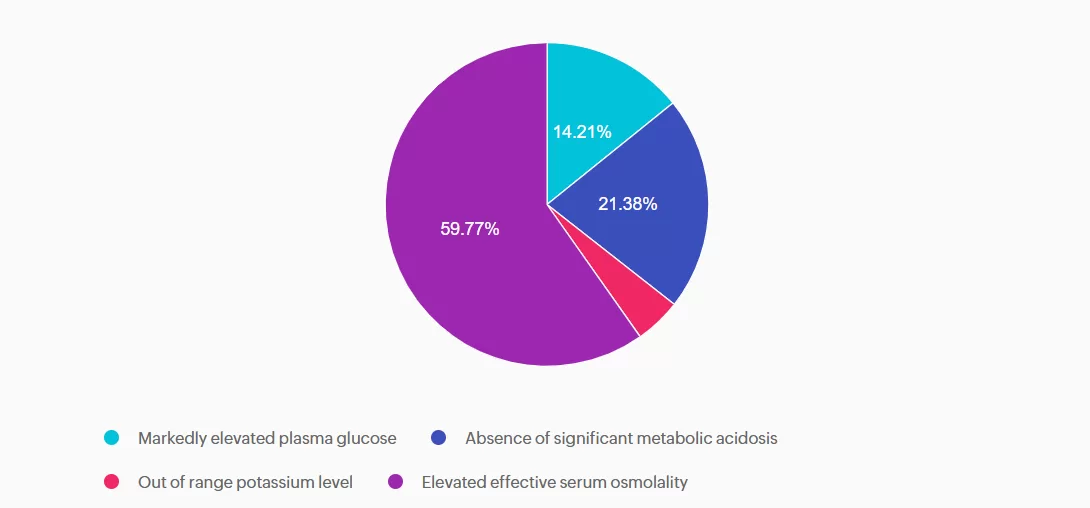
Getting to the Best Answer
Answer A is incorrect: 14.21% chose this answer, “Markedly elevated plasma glucose.” This answer is tempting, because glucose levels do become markedly elevated with HHS. However, very high glucose levels can also occur with DKA. So this answer doesn’t differentiate between these two hyperglycemic crises.
Answer B is incorrect: 21.38% chose this answer, “Absence of significant metabolic acidosis.” This juicy answer is tempting, since with HHS there is the absence of metabolic acidosis. However, based on the question details, there is no information on pH or ketone status, so we can’t make that assumption.
Answer C is incorrect: 4.64% chose this answer, “Out of range potassium level.” The potassium level of 3.7 is within normal range and doesn’t help us differentiate between HHS and DKA.
Answer D is correct: 59.77% chose this answer, “Elevated effective serum osmolality.” YES, this is the BEST Answer. Great Job! One of the main features of HHS, is increased serum osmolality (greater than 300), due to a combination of elevated glucose and dehydration.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn More About DKA & HHS
With Level 2 | Hyperglycemic Crises (DKA, HHS & EDKA) & Our CDCES Boot Camp!
Spreading the Love Sale
Save 15% on ALL of Our Online Courses

Sale Ends on February 16th, 2026!