Rationale of the Week | Exercise & Heart Rate Mystery

For our April 13th Question of the Week, 62% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: LR loves going to the gym 3 times a week. LR is 78, with Latent Autoimmune Diabetes (LADA) and is on basal bolus insulin. LR also takes a statin and ACE Inhibitor. LR has a history of retinopathy and peripheral neuropathy. During your assessment, LR proudly shares that when on the treadmill, their heart rate never goes above 100 beats per minute.
What best explains this heart rate?
Answer Choices:
- Excellent cardiovascular health from regular exercise
- Cardiac autonomic neuropathy
- Stiff heart syndrome
- ACE Inhibitors can contribute to lower heart rates
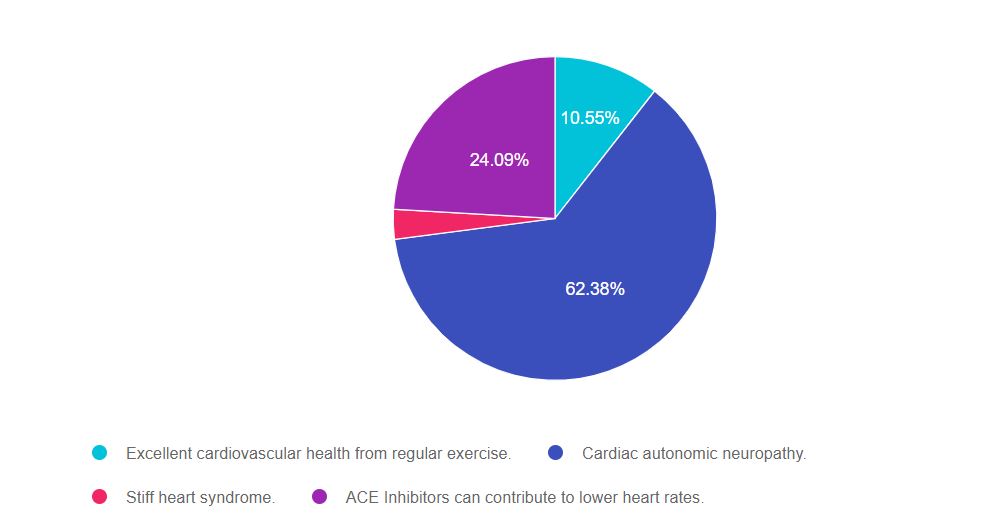
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 1, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 10.55% chose this answer, “Excellent cardiovascular health from regular exercise .” On first blush, this answer is tempting, yet it doesn’t consider in all the factors described in the case study. If we look at his age and the presence of microvascular disease and neuropathy, we are correct to suspect that he may also have autonomic neuropathy. Therefore, his low heart rate isn’t an indication of robust health but a sign of autonomic dysfunction.
Answer 2 is correct, 62.38% of you chose this answer, “Cardiac autonomic neuropathy.” Good job! When we look at his age and the presence of microvascular disease and neuropathy, we are right to suspect he also has cardiac autonomic neuropathy. As a result of nerve disease, his heart rate isn’t able to respond to the cardiac demand of intense exercise and never exceeds 100. This “fixed heart rate” is a sign of autonomic dysfunction that warrants further investigation.
Answer 3 is incorrect, 2.98% of you chose this answer, “Stiff heart syndrome.” People with diabetes are more likely to have stiff fibrotic hearts and this can lead to increased risk of heart failure. However, there is no such condition as a “stiff heart syndrome”. This answer was a distractor.
Answer 4 is incorrect, 24.09% of you chose this answer, “ACE Inhibitors can contribute to lower heart rates.” This was our juicy answer. The blood pressure class of ACE Inhibitors does not lower heart rates but does lower blood pressure. The blood pressure class Beta Blockers, can lower heart rate, but it was not included in this question. See our Med Cheat Sheets 2021 | Hypertension, Lipids, and Neuropathy for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more?
Join us for our Level 2 – Critical Assessment – Fine-Tuning your Diabetes Detective Skills – 2.0 CEs.

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: 90-minute video presentation, podcast, practice test, and additional resources.
This course integrates the ADA Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies and real-life situations, we discover often hidden causes of hyperglycemia and other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, and more. We delve into therapy for complicated situations and discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, and Transplants. Join us for this unique and interesting approach to assessing and evaluating the hidden complications of diabetes.
Topics Include:
- Identify common yet often underdiagnosed complications associated with type 1 and type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia and other conditions including, transplant, cystic fibrosis and liver disease.
Intended Audience: A great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | Mystery Condition?

ML has had type two diabetes for 12 years, a BMI of 33.7, an A1 C of 8.3%, and elevated triglycerides and LDL cholesterol levels. You notice ML’s palms are deeply red.
Which of the following conditions is ML most likely experiencing in addition to diabetes?
- Non-alcoholic fatty liver disease
- Dermatomyositis secondary to inflammation
- Auto immune renal hypertension
- Acanthosis Nigracans of the palmar surface
Click here to test your knowledge!
Want to learn more about this question and more?
Join us live on April 28th from 11:30 am to 1:30 pm for our Level 2 – Critical Assessment – Fine-Tuning your Diabetes Detective Skills – 2.0 CEs.

Diabetes Education Services Online University Courses are an excellent way to study for your exam anytime and anywhere that is convenient for you. You will have immediate access to your courses for 1 year after your purchase date. Each individual online course includes a: 90-minute video presentation, podcast, practice test, and additional resources.
This course integrates the ADA Standard of Care on elements of a comprehensive medical assessment (Standard 4) of the individual living with prediabetes, diabetes, or hyperglycemia. Through case studies and real-life situations, we discover often hidden causes of hyperglycemia and other complications, such as liver disease, sleep apnea, pancreatitis, autoimmune diseases, fractures, and more. We delve into therapy for complicated situations and discuss management strategies for other conditions associated with hyperglycemia such as Cystic Fibrosis, and Transplants. Join us for this unique and interesting approach to assessing and evaluating the hidden complications of diabetes.
Topics Include:
- Identify common yet often underdiagnosed complications associated with type 1 and type 2 diabetes.
- State strategies to identify previously undiscovered diabetes complications during assessments.
- Discuss links between hyperglycemia and other conditions including, transplant, cystic fibrosis and liver disease.
Intended Audience: A great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Can’t join live? No worries, we will record the webinar and post it to the Online University!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
FREE Webinars | Free Resource Friday
For Free Resource Friday, we want to share our Free webinars with you!

Be a part of our diabetes community while learning about the latest in diabetes care. Plus, Coach Beverly provides an interactive question and answer session at the end of each live webinar.
Certification and FREE Webinars Include:
CDCES or BC-ADM – Which Certification is Right for me? – Ready for Viewing
Read More: CDCES or BC-ADMAre you considering pursuing certification in diabetes care, but are not sure which certification is right for you and how to get started? Topics include:

- Discuss the similarities and differences between the CDCES and BC-ADM credentials
- List the academic and experiential qualifications to take both exams
- Explore which certification best match your personal and professional goals
- Describe the steps to study and prepare for exam success for both certifications
Coach Beverly will share her personal journey on achieving both her CDCES and BC-ADM over 20 years ago and how these credentials have impacted her opportunities as a diabetes specialist and president of her own company.
Click on the link below for more info!
Preparing for the CDCES Exam – Airs July 8th
Read More: CDCES Exam PrepJoin us to get ready to succeed a the CDCES Exam. This course will transform your test anxiety into calm self-confidence and test taking readiness. Topics covered include:

- Changes in requirements for 2021
- Exam eligibility and test format
- Strategies to succeed
- Review of study tips and test taking tactics.
We will review sample test questions, and the reasoning behind choosing the right answers.
After registering, you will receive a confirmation email containing information about joining the webinar.
Join us live! Click on the link below for upcoming dates! All FREE Preparing for the CDCES Exam Webinars air from 11:30 a.m. – 1:00 p.m. PST.
Preparing for the BC-ADM Exam – Airs July 15th
Read More: BC-ADM Exam Prep
This free webinar will review changes in BC-ADM requirements for 2021 exam eligibility and test format, strategies to succeed along with a review of study tips and test taking tactics. We review sample test questions, and reasoning behind choosing the right answers.
Join us live- Click on the link below for upcoming dates! All FREE Preparing for the BC-ADM Webinars will air from 11:30 a.m. PST – 1:00 p.m. PST.
Test Taking Practice Exam Sample Questions Toolkit – Ready for Viewing
Read More: Sample Exam Practice QuestionsFor many of us, taking the certification exam is a nerve-wracking process.

During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times.
You are invited to join Coach Beverly for this FREE Webinar. And, if you want to have access to an additional 220+ sample practice online questions, you can purchase the complete Test Taking Toolkit.
What We Say Matters: Language that Respects the Individual and Imparts Hope – Airs May 18th
Read More: Language & Diabetes
What we say matters. As educators, advocates, spouses, friends, and providers, our use of language can deeply affect the self-view of people living with diabetes everyday. The language used in the health care setting is immensely important in determining the success of the interaction and long term relationships. Thoughtful communication provides a sense of support and empathy and moves both the provider and person with diabetes toward greater satisfaction and success.
New Horizons – Getting to the Gut, Meet Your Microbiome – Airs November 9th
Read More: Getting to the Gut
This one-hour complimentary journey will expand your view of how trillions of bacterial hitchhikers profoundly influence our health. We will discuss how foods, the environment and our medical practices have impacted our gut bacteria over time and strategies we can take to protect these old friends. Join us!
Mindfulness and Compassion in the Diabetes Encounter Webinar – Ready for Viewing
Read More: Mindfulness & CompassionBeing a diabetes educator can be challenging. This one-hour presentation by Heather Nielsen, MA, LPC, CHWC will provide diabetes educators with helpful hands-on strategies to incorporate mindfulness and self-compassion into our daily lives and professional practice
No CE units are provided for our FREE Webinars, but we have good news: Visit our Diabetes Ed Online University where you can earn CEs from your desk!
View All Diabetes Education Services Free Webinars here
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Type 1, Ramadan & Fasting

For our April 6th Question of the Week, 47% of respondents chose the best answer. We wanted to “take a closer look” into this question.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: RS observes Ramadan and fasts from sunrise to sunset. RS is 13 years old, has type 1 diabetes, uses an insulin pump and CGM. RS’s insulin-to-carb ratio is 1:12 and correction is 1:45. Basal settings range from 0.5 -1.2 units an hour.
What would be the best recommendation for RS to keep blood sugars in the target range during Ramadan?
Answer Choices:
- See if RS can get a note from their doctor to allow eating during the day.
- Take bolus insulin when RS eats a meal or snack.
- Decrease basal insulin rate by 50% during periods of fasting.
- Monitor urine ketones at least twice a day.
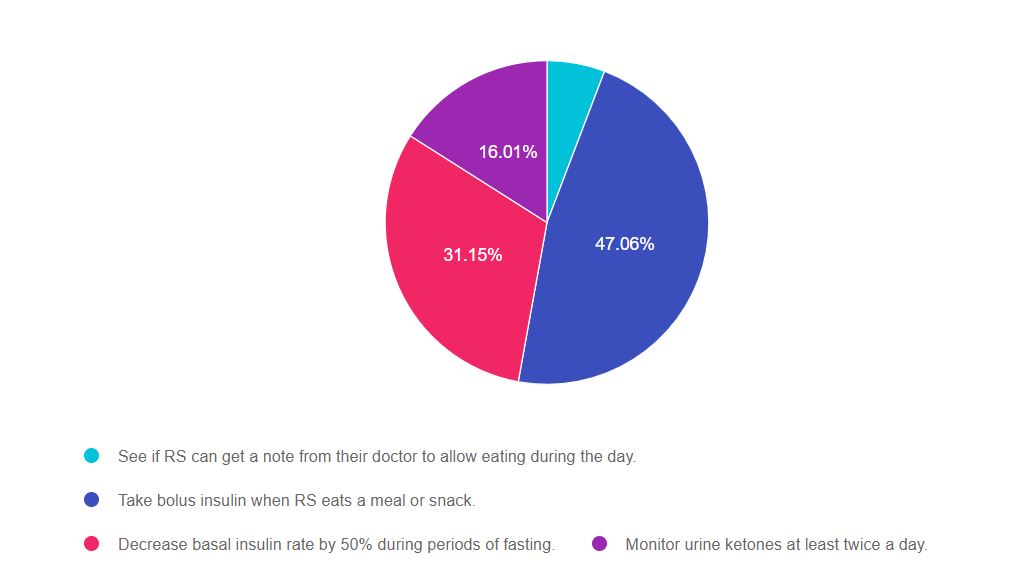
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 5.79% chose this answer, “See if RS can get a note from their doctor to allow eating during the day.” As diabetes specialists, we are at our best when we tap into our cultural humility. We may not be familiar with the customs and celebrations of other cultures, but we can honor these traditions and express sincere interest in learning more about them. In this situation, we would respect their tradition, explore potential issues surrounding fasting and help with problem solving and creating a back up plan in case an issue arises.
Answer 2 is correct, 47.06% of you chose this answer, “Take bolus insulin when RS eats a meal or snack.” Good Job! When the basal rates of an insulin pump are set correctly, a person with type 1 diabetes can fast and still keep glucose on target. This background or basal insulin works to manage glucose levels in between meals and through the night. Actually, this period of fasting will provide an opportunity to evaluate if basal settings need adjustment or if they are set correctly. When RS breaks the fast at sunset, they will just need to dose for carbohydrates and cover for hyperglycemia if needed.
Answer 3 is incorrect, 31.15% of you chose this answer, “Decrease basal insulin rate by 50% during periods of fasting.” When the basal rates of an insulin pump are set correctly, a person with type 1 diabetes can fast and still keep glucose on target. This background or basal insulin works to manage glucose levels in between meals and through the night. If RS is receiving too much basal insulin and experiences low blood sugars during periods of fasting, they will need to fine tune their basal rates. However, we would not suggest to automatically decrease basal rate by 50% in preparation for fasting.
Answer 4 is correct, 16.01% of you chose this answer, “Monitor urine ketones at least twice a day.” Since RS has an insulin pump that delivers basal insulin 24 hours a day, they are at low risk for ketosis. Ketosis is usually a result of insufficient insulin administration. Without adequate insulin, fats are utilized as an alternate energy source, leading to positive ketones. In this situation, RS is receiving adequate insulin through the pump and is not at increased risk of significant ketosis.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
On Sale | Now just $24.95
ADA 2021 Standards of Medical Care in Diabetes Book
The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
One of the most important pieces of literature to read prior to becoming a Diabetes Care and Education Specialist and for clinical practice, the Standards of Care book is a study must!
The book includes:
- ADA’s standards for diagnosing and treating diabetes
- Nutrition recommendations and principles
- Position statements on managing diabetes and its complications in various settings
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Virtual DiabetesEd Specialist Conference Begins Tomorrow | Reserve Your Spot!
It’s not too late to reserve your spot for our
Virtual DiabetesEd Specialist Conference | April 15-17, 2021
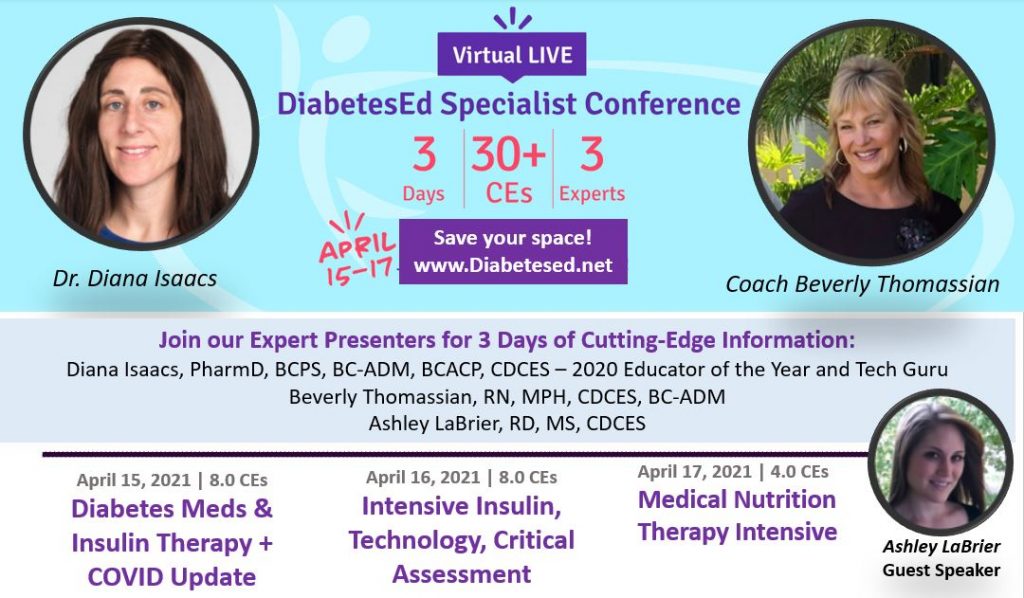
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. If you are interested in taking the CDCES or BC-ADM exam or are seeking a state-of-the-art review of current diabetes care, this course is for you.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Entire Program Fee: $399
Dates: April 15-17, 2021
3 Expert Speakers
CEs: 30+ CE hours
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Come join our Virtual DiabetesEd Specialist Program.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
- Live Q & A Session with the instructor after each webinar
- Presentations by our team of experts
- Handouts and Resources for each session
- Post-test questions
- A sense of community
- If you can’t attend the live webinars, a recorded version will be posted later the same day for viewing.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
*The use of DES products do not guarantee successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.”**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve continuing education.
Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”
Question of the Week | Exercise & Heart Rate Mystery

LR loves going to the gym 3 times a week. LR is 78, with Latent Autoimmune Diabetes (LADA) and is on basal bolus insulin. LR also takes a statin and ACE Inhibitor. LR has a history of retinopathy and peripheral neuropathy. During your assessment, LR proudly shares that when on the treadmill, their heart rate never goes above 100 beats per minute.
What best explains this heart rate?
- Excellent cardiovascular health from regular exercise
- Cardiac autonomic neuropathy
- Stiff heart syndrome
- ACE Inhibitors can contribute to lower heart rates
Click here to test your knowledge!
It’s not too late to register for our Virtual DiabetesEd Specialist Course
Earn 30+ CEs | April 15-17, 2021
Virtual DiabetesEd Specialist Program
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
If you are interested in taking the CDCES or BC-ADM exam or are seeking a state of the art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need.
Can’t join live? No worries, your registration guarantees access to the recorded content through Dec 31, 2021!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
Bonus Courses worth 14 + CEs FREE – When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
April eNews | Diabetes Certification Exam Updates You Need to Know
The Steps to Getting Certified Have Changed – A LOT

I remember clutching my calculator and driver’s license as I entered the crowded test site to take my Certified Diabetes Educator (CDE) Exam for the first time 29 years ago.
Back in the early 90s, applicants needed 2000 hours of diabetes self-management practice experience to qualify and a #2 pencil to bubble in the right answers on the exam scantron.
I felt queasy as I opened the test booklet and looked at the first question, which was a long vignette with a complex chart of blood sugar data. A terrifying thought crossed my mind “What if I fail, what would my staff think”?
Over 3 hours later, I gave my bubbled-in scantron to the proctor, stepped out into the sunshine, and took a big breath of relief.
Thinking back on this day, I clearly remember a lack of study tools and resources to prepare for the exam. Our little group studied the “AADE Blue Books” and created practice quizzes, but I still felt extremely unprepared for the exam in front of me.
This profound experience kick started the creation of our company, dedicated to making sure that health care professionals have the tools and resources needed to realize their professional dream of achieving (and maintaining) certification.
In truth, achieving my CDCES is one of the best and most meaningful investments in my professional career!
For this newsletter, we celebrate diabetes certification.
We dive into the modified eligibility requirements for the CDCES exam. We also provide a simplified explanation for certification renewal. Coach Beverly shares her journey to become a CDCES. Plus, we explore our most popular Question of the Week ever and pose a new question regarding Type 1 and Ramadan. To celebrate Spring, the ADA Standards Book is on sale too!
Wherever you are on this journey, we are here to cheer you on each step of the way. Let us know how we can help!
Coach Beverly, Bryanna, and Jackson
Featured Blogs
- CDCES Exam Eligibility Update
- Renewing My CDCES – What is Required?
- Coach Beverly’s Journey to Becoming a CDCES
- Question of the Week – How Many Insulin Pens?
- Rationale of the Week – Get Your Calculators
- CDCES Success Story – Congratulations Sandra!
Featured Items
- Preparing for CDCES FREE Webinar – April 1st
- Preparing for BC-ADM FREE Webinar – April 8th
- Lower Extremity Assessment Webinar – April 21st
- ADA Standards of Care Book
- Free Resources Catalog
On Sale | Now just $24.95
ADA 2021 Standards of Medical Care in Diabetes Book
The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
One of the most important pieces of literature to read prior to becoming a Diabetes Care and Education Specialist and for clinical practice, the Standards of Care book is a study must!
The book includes:
- ADA’s standards for diagnosing and treating diabetes
- Nutrition recommendations and principles
- Position statements on managing diabetes and its complications in various settings
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Black Spots in Eyes

For our March 30th Question of the Week, 79% of respondents chose the best answer. We wanted to “take a closer look” into this question. What is the best action to take for some one who is experiencing eye issues?
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR was recently diagnosed with type two diabetes. JR‘s A1 C was 13.9%, but now blood sugars are running in the 100 to 180 range. JR mentions that they have been noticing “black spots” floating in their eyes.
What is the best response by the diabetes specialist?
Answer Choices:
- This is an expected finding when blood sugars drop rapidly.
- On a scale of 1 to 10, how much are these spots affecting your daily quality of life?
- That must be really scary. Make sure to mention this at your next provider visit.
- Let’s get you scheduled in to see ophthalmology.
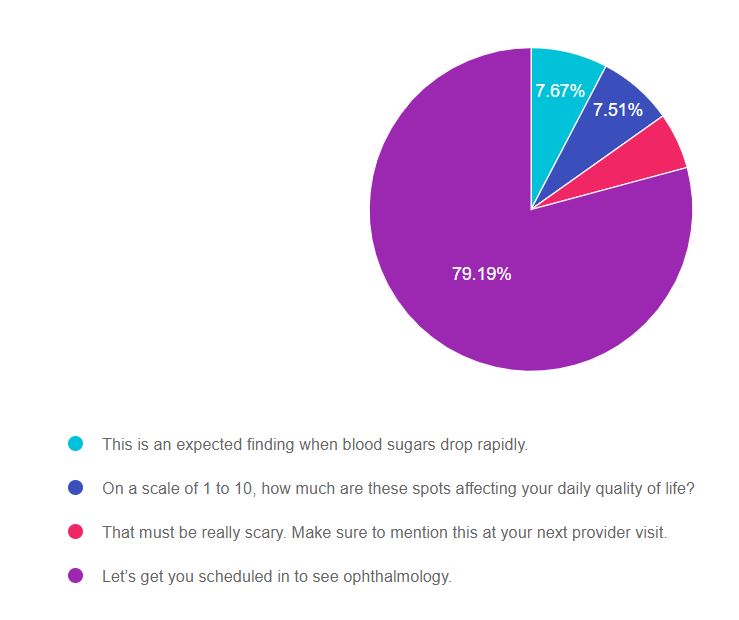
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the ADA Standards of Care and best clinical practice.
Answers & Rationale
Answer 1 is incorrect, 7.67% chose this answer, “This is an expected finding when blood sugars drop rapidly.” Actually, this is not an expected finding and warrants immediate investigation.
When people with diabetes experience fluctuations in blood sugars, they may complain of blurry vision and their glasses not working due to fluid shifts. However, a rapid drop in glucose can intensify the risk of retinal bleeds. “Black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 2 is incorrect, 7.51% of you chose this answer, “On a scale of 1 to 10, how much are these spots affecting your daily quality of life?” This assessment question would be appropriate if the person was receiving treatment for eye problems already and we are evaluating the impact on daily life. However, this is not the case.
This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 3 is incorrect, 5.63% of you chose this answer, “That must be really scary. Make sure to mention this at your next provider visit.” Yes, it is important to notify the provider, IMMEDIATELY. What if the next provider visit is in 6 months or a year? What if JR misses that appointment and gets lost to follow-up?
This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems.
Answer 4 is correct, 79.19% of you chose this answer, “Let’s get you scheduled in to see ophthalmology.” GREAT JOB. Most of you chose this answer. This sudden appearance of black dots” or floaters can indicate retinal bleeding and warrant an immediate evaluation by an eye professional (Ophthalmologist or Optometrist). Delayed treatment can lead to serious eye problems and many people with diabetes don’t receive regular eye care. Let’s help break down barriers and make sure people with diabetes get the eye care they deserve.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








