
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
Tandem Diabetes has leveled up insulin pump technology with a new algorithm and expanded its continuous glucose monitor (CGM) compatibility. The new algorithm, Control IQ+, is built upon the previous Control IQ algorithm, offering several updated features. In June 2025, Tandem diabetes announced Libre 3+ is joining the family of compatible CGMs. Let’s uncover the details of this new algorithm and review the compatible CGM options.

Control IQ+ introduces several new features designed to enhance glycemic control.¹ These features are available for both the Tandem t:slim X2 and Mobi insulin pumps.
✅ Age: Control IQ+ is available for ages 2 years and up.
✅ Indication: This algorithm has approval for both Type 1 Diabetes and Type 2 Diabetes.
✅ Extended Bolus: This feature allows for extended boluses for up to 8 hours.
✅ Weight Range: The new algorithm now includes extended weight ranges from 20-440 lbs.
✅ Total Daily Dose of Insulin: For those with high insulin requirements, the total daily dose of insulin is now up to 200 units per day.
✅ Temp Basal Rate: The temp basal rate feature can be used for up to 72 hours while still staying in Control IQ+. Now users don’t need to stop the automated insulin delivery mode when requiring a temp basal rate for short-term needs like illness or exercise. The algorithm will continue to adjust the basal rate and give boluses if needed based on blood glucose levels.²
Tandem announced in June 2025 the approval of Libre 3+ to its current family of compatible CGMs. Per Tandem Diabetes Care, the Libre 3+ will be compatible with the t:slim X2 pump and is only available through an early access program, with a broader access announcement expected later this year.³ Currently, the compatible CGMs are:
🩸Dexcom G6 (For t:slim X2 and Mobi)
🩸Dexcom G7 (For t:slim X2 and Mobi)
🩸Libre 2 + (For t:slim X2 only)
Now that you know what’s new with Control IQ+ technology and the current CGM compatibility, you can confidently help clients develop a personalized approach to insulin pump management. Diabetes healthcare professionals can also help existing Tandem insulin pump users update their software to the new Control IQ+ algorithm. Individuals living with diabetes depend on your expertise to guide them through the maze of diabetes technology. During education sessions, reviewing the basics of how the algorithm works and specific features of the pump can be reassuring for individuals in our care. Additionally, assessing carbohydrate counting skills and discussing how to administer food and correction boluses along with preventing and managing hypoglycemia, can make a big difference.
Join us at our live San Diego Conference to learn more about Diabetes Technology with Diana Isaacs, PharmD CDCES, BC-ADM, FADCES. Check out the events page to see all the exciting options!

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during checkout to save
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
R.S. is a 60-year-old with type 2 diabetes who was recently placed on insulin lispro at meals. He has taken insulin glargine once a day for five years. Previously, non-insulin medications have been ineffective or not tolerated. He continues to have hyperglycemia despite the addition of insulin lispro. During his diabetes education visit today, he shared that he has not been taking his mealtime insulin lispro because he does not want to inject it in front of his grandchildren, who live with him. He feels overwhelmed by these additional injections but wants to get his blood glucose levels under better control so he can have the energy to play with his grandchildren and avoid losing his eyesight like his mother did.
As the diabetes care and education specialist, which of the following would be the most appropriate first step in addressing R.S.’s concerns?

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during check to save.
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
Earn 30+ CEs with Expanded Accreditation!
Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.

Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Celebrating Our Diabetes Education Scholarship Recipients
We are incredibly grateful for the overwhelming response to our Bridge Scholarships for both the CDCES Prep Boot Camp and Live Seminar Scholarships. Your passion, dedication, and commitment to advancing in diabetes care truly inspired us.
Each application we received was a powerful reminder of the incredible work being done across our healthcare community. Our panel of judges faced the challenging task of selecting recipients, carefully evaluating each application based on several important criteria: financial need, person-centered language, inclusivity, impact, volunteerism, and readiness to sit for the CDCES exam.
After thoughtful consideration, we are thrilled to announce the recipients of this round of scholarships! 🎉
These individuals represent the very best of what our community stands for—dedication, empathy, service, and the drive to grow professionally and personally. The scholarships they’ve received will not only recognize their hard work and achievements but also provide the support they need as they take the next step in their journey toward becoming Certified Diabetes Care and Education Specialists.
Please join us in congratulating our scholars! Their commitment to improving diabetes care and education will undoubtedly have a lasting impact on the communities they serve.
To our scholarship recipients: Congratulations! And to our entire community of healthcare professionals: Thank you for your continued passion, perseverance, and support. Together, we are building a stronger, more inclusive future in diabetes care.

FNP-C
Roswell, NM

MS, RDN
Sacramento, CA

BS, MSN, PHN
Los Angeles, CA

ADN, BA in Public Policy, Master's in International Development
South Hero, VT

Bachelor of Science in Dietetics - Registered Dietitian
Houston, TX

ARPN, FNP-C
Texarkana, TX

Bachelor of Science in Foods & Nutrition, RDN, LDN
Pinehurst, NC

Registered Nurse, BSN
Charleston, SC

RN
Chicago, IL

MS, RD, HWC
Hartford, CA

MS, BSN, CCRN-Pediatric, CPHQ
Sacramento, CA

RDN
Lodi, CA

MS, RDN, LDN
Charlotte, NC
MS, RDN, CD
Bellevue, WA
AGACNP, CNP, RN, CCRN
Minneapolis, MN
FNP- BC
Brooklyn. NY
BSN, RN
Kansas City, MO
MPH
Gooding, ID
BSN
Cary, NC
MS in Nursing, FNP
Corona, CA
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Time Restricted Eating- Best Approach. 86% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

MJ is a 56-year-old with type 2 diabetes (A1C 7.3%), HTN, and dyslipidemia. Current medications include metformin 1,000 mg twice daily, lisinopril, and atorvastatin. Activity includes walking 20–30 minutes most evenings. At their most recent visit, MJ is inquiring about using at 16:8 time-restricted eating plan and plans eating from 11 a.m. to 7 p.m. and will include coffee/unsweetened beverages outside that window. MJ checks their blood glucose once daily and there is no reported history of severe hypoglycemia.
What response would you provide MJ regarding the safety and effectiveness of an intermittent fasting, time-restrictive eating plan?
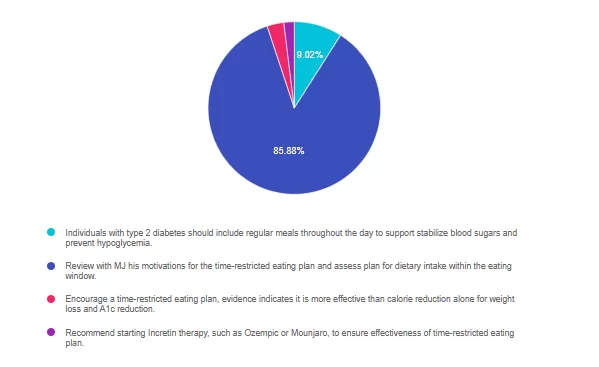
Answer 1 is incorrect. 9% chose this answer, “Individuals with type 2 diabetes should include regular meals throughout the day to support stabilize blood sugars and prevent hypoglycemia.” Random control trials have indicated that time-restricted eating is a safe and practical dietary approach for individuals with type 1 and type 2 diabetes. While assessment and prevention of hypoglycemia is a priority, MJ’s current medication regimen is of low risk. Even with higher risk medications, such as insulin or sulfonylureas modifications of medication, timing or dose can be made to support safety.
Answer 2 is correct. 86% of you chose this answer, “Review with MJ his motivations for the time-restricted eating plan and assess plan for dietary intake within the eating window.” Great Job! Time-restricted eating can be a safe and effective strategy for MJ. Reviewing motivation and current eating patterns may improve the ability to apply balanced meals within the eating window.
Answer 3 is incorrect. About 3% of respondents chose this, “Encourage a time-restricted eating plan, evidence indicates it is more effective than calorie reduction alone for weight loss and A1c reduction.” While time restricted eating may be a practical strategy, it has not been shown to be superior to continuous energy restricted dietary intake for weight loss and A1c outcomes.
Finally, Answer 4 is incorrect. About 2% chose this answer, “Recommend starting Incretin therapy, such as Ozempic or Mounjaro, to ensure effectiveness of time-restricted eating plan.” While we may consider addition of an incretin therapy to support A1c, weight and cardiovascular risk reduction, time-restricted eating does not require the addition of these medications to be effective.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Cardiovascular-kidney-metabolic (CKM) syndrome represents the interconnected systems of adiposity, metabolic dysfunction, kidney disease, and cardiovascular disease. In 2023, the American Heart Association’s (AHA) advisory panel defined a spectrum of risk by defining five progressive stages.¹ These stages span from stage 0 (no CKM risk factors), stage 1 (excess or dysfunctional adiposity), stage 2 (metabolic risk factors and CKD), stage 3 (subclinical cardiovascular disease in CKM) and Stage 4 (clinical cardiovascular disease (CVD) in CKM). This staging system emphasizes the continuum of risk, the importance of assessment across the lifespan, and the value of early interventions. The AHA advisory emphasized systematic screening (1) across all stages and lifespans to identify risk early. It is predicted that in the US, almost 90% of the population meets stage 1 or higher. (2) In collaboration with the community and medical care teams addressing CKM requires consideration of genetics, behavior, environment, and social determinants of health alongside pharmacotherapy, lifestyle and nutrition interventions. As diabetes educators, we are already skilled in assessing many of the metrics included within the staging assessments, making us well-positioned to implement CKM-based risk interventions.
In June 2025, the Journal of the American College of Cardiology published an expert review of evidence-based lifestyle interventions for CKM syndrome.² Although few studies have examined dietary interventions specifically for CKM syndrome, existing research for metabolic, kidney, and cardiovascular disease ❤️ highlights a consensus of diet quality and whole-diet patterns over single-nutrient approaches. Stage 0 encourages youth interventions to promote health through healthy diet, activity, and multi-component education within schools. In Stage 1, the goal is to prevent the development of metabolic risk factors in individuals with excess or dysfunctional adiposity. While intentional weight loss of at least 5% provides significant cardiometabolic prevention benefits, adopting a heart-healthy diet and increasing physical activity can improve health even without weight loss.¹ Stage 2 is focused on metabolic and CKD risk reduction, with DASH and Mediterranean diets recommended alongside aerobic and resistance training to support glycemic management and reduced blood pressure, hypertriglyceridemia, and progression of CKD.¹ ² Concerns of subclinical CVD modify recommendations in Stage 3 to focus on interventions that can reduce non-calcified arterial plaques and CVD events; however, only one dietary study was included within the review. The DISCO-CT trial² found that a dietitian-led DASH dietary pattern significantly reduced non-calcified plaque in individuals with non-obstructive stenosis. Nutrition should also focus on kidney preservation through individualized protein goals, increased plant-based foods 🥦, and limited processed-food consumption. In addition, medication optimization and high-intensity exercise are recommended. Dietary strategies for individuals with established CVD, Stage 4, focus on improving recovery and secondary prevention. The Mediterranean and low-fat dietary patterns are supported by evidence to reduce the recurrence of cardiovascular events post MI and reduce myocardial ischemia and coronary artery disease progression, respectively. In stage 4, like all stages, evidence-based pharmacotherapy and coordinated care with multi-disciplinary teams complement lifestyle interventions. While more research is needed to tailor strategies to individual needs at each stage, we can see that these stages have many overlapping recommendations. We can use a whole-person, comprehensive assessment approach instead of focusing on dietary interventions that treat diseases in isolation.
Dietary patterns and lifestyle strategies can be implemented using a simplified, patient-centered approach. The DASH and Mediterranean diets both support CKM syndrome outcomes but have slight differences in food patterns. DASH emphasizes fruits, vegetables, whole grains, low-fat dairy, lean protein, and limits on sodium. The Mediterranean diet prioritizes plant-based foods, healthy fats like olive oil, moderate fish and poultry, and limited red meat, with a focus on flavor and traditional eating patterns rather than strict nutrient targets. Both dietary patterns emphasize micronutrient dense, antioxidant rich and high fiber foods. By using these evidence-based dietary patterns as a framework, diabetes educators can tailor nutrition and lifestyle strategies to an individual’s preferences, abilities, and cultural context as we know is recommended by the American Diabetes Association.³ Practical considerations to address diet quality include seeking opportunities to increase vegetables and fruits, whole grains and legumes, plant proteins, fish, and nuts and seeds, while minimizing red/processed meat consumption, added sugars, sodium, and ultra-processed foods.³
Optimizing CKM health requires a comprehensive and collaborative approach.¹ This includes recognizing the impact of social determinants of health, expanding education and access to pharmacotherapies, and filling critical research gaps. It also means strengthening care coordination among providers, offering better education for both professionals and the public, and focusing on factors to address dysfunctional adiposity as a key driver of CKM. Finally, building strong partnerships across health systems and communities will be essential to support at-risk communities and help people achieve healthy outcomes. Diabetes educators can serve as guides, assisting individuals to understand their risks, supporting behavior change, and ensuring evidence-based CKM strategies are translated into practical, sustainable care.
References:
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
A 54-year-old with type 2 diabetes and hypertension is diagnosed with hypercortisolism. Despite lifestyle interventions and maximum doses of metformin, GLP-1 RA, and an SGLT2 inhibitor, her A1C remains 9.2%. They are started on mifepristone.
Which of the following best explains how mifepristone improves glycemic control in this setting?
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Invite your colleagues!! Join us September 16th @ 11:30 am PST!
If you are a health care professional considering becoming a CDCES and want to learn more about eligibility and benefits of joining the Diabetes Education Community, this FREE webinar is for YOU. Coach Beverly will provide clarification on requirements, exam content, and study strategies to prepare for success.
There’s still time to register!! Join us September 18th @ 11:30am PST!
Why are glucose levels elevated in the morning? When should insulin be started? What is the next step to get A1c to target?
During this course Coach Beverly addresses each of these glucose mysteries & more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns & correct common issues encountered by people living with type 2 diabetes.
Register above or simply visit our Online Store at DiabetesEd.net.
For more information or any questions, please email [email protected].
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on clinical clues to hypercortisolism. 53% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

AJ is a 52-year-old with type 2 diabetes presents with worsening hyperglycemia despite taking three diabetes medications. AJ says, “No matter what I do, I can’t seem to get my blood sugars down”.
Which of the following clusters of physical findings would increase your suspicion that AJ is struggling with hypercortisolism?
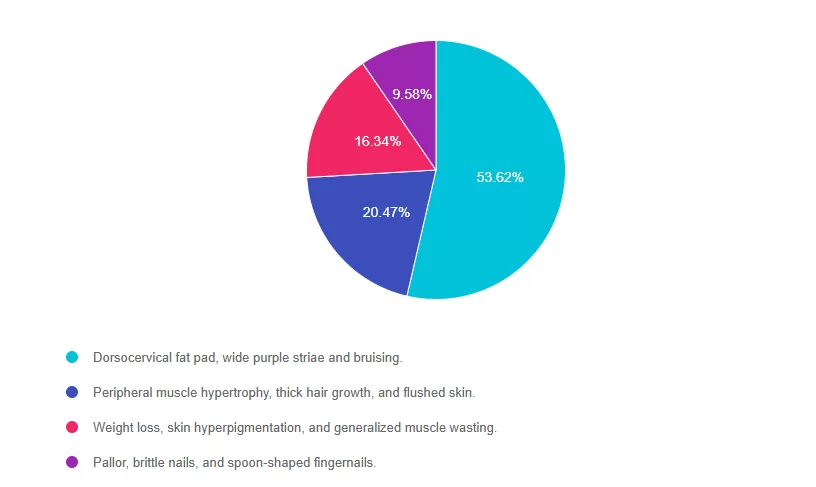
Answer 1 is correct. 53.62% chose this answer, “Dorsocervical fat pad, wide purple striae and bruising.” YES, GREAT JOB! These are classic physical features of hypercortisolism. Dorsocervical fat pad, wide purple striae and easy bruising along with proximal muscle weakness, and poor wound healing, should prompt evaluation for hypercortisolism in people with elevated glucose and hypertension, despite being on several medications for blood glucose and blood pressure.
Answer 2 is incorrect. 20.47% of you chose this answer, “Peripheral muscle hypertrophy, thick hair growth, and flushed skin.” These features are not characteristic of hypercortisolism; thick hair growth and muscle hypertrophy point to other conditions.
Answer 3 is incorrect. 16.34% of respondents chose this, “Weight loss, skin hyperpigmentation, and generalized muscle wasting.” These features are more consistent with Addison’s disease (adrenal insufficiency) or chronic illness, not hypercortisolism.
Finally, Answer 4 is incorrect.9.58% chose this answer, “Pallor, brittle nails, and spoon-shaped fingernails.” These findings are typically seen in iron-deficiency anemia, not hypercortisolism.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.