App for Remotely Managing Hypertension Effective in Type 2
A new study shows a positive outcome for people with type 2 diabetes and utilizing a smartphone application to monitor blood pressure.
The study gave a Bluetooth-connected blood pressure monitoring device to 276 people with elevated BP for 6 weeks. After the device read their BP, the participants were sent their results along with helpful tips, and a reminder to take their medications.

During the study, there was also education provided to all participants with a goal to help lower BP ratings.
“Participants who had the highest blood pressure at baseline were the most likely in multivariable modeling to see reductions in both systolic and diastolic pressure by the end of the study.”
Researchers believe that using the app helped participants not only become more aware of their blood pressure regulation, but also fostered positive medication adherence and lifestyle changes.
To learn more: Smartphone App for Remotely Managing Hypertension Effective in Type 2 – Endocrinology Advisor
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Is Weight Stigma a Barrier to Effective Education? | July Newsletter
July Newsletter Now Available!
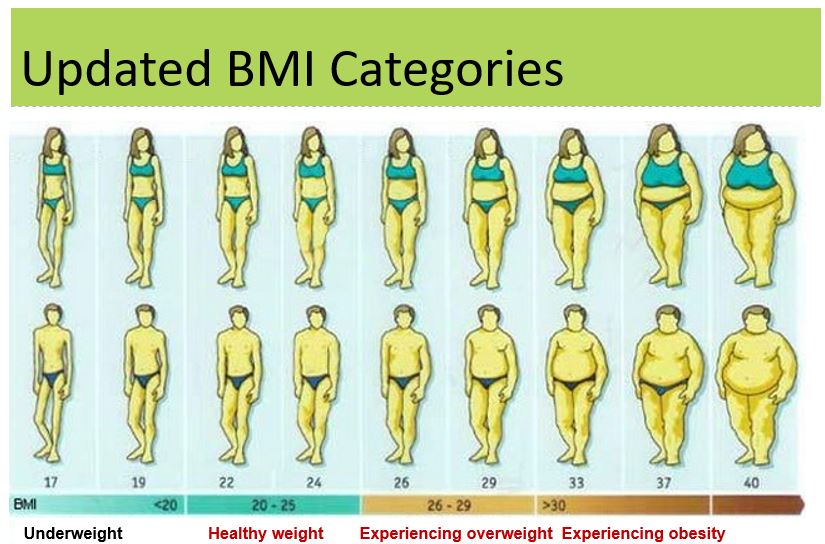
Most of us aren’t even aware that weight bias is embedded in our everyday medical language, in scientific papers, and in our client interactions. But with awareness, we start hearing and seeing this bias all around us and realize that change is needed.
In our July Newsletter, we explore weight bias language and provide some examples and fixes. Plus, we invite you to apply for our diabetes education scholarship and highlight the approval for a GLP-1 RA for pediatrics with type 2 diabetes.
July Newsletter Topics
- What is weight bias and how do we fix it.
- You are invited to apply for our Diabetes Educator Course Scholarship in San Diego, CA – Deadline July 22, 2019.
- Approval for a GLP-1RA for pediatrics with type 2 diabetes.
- Digital PocketCards Updated.
- Bring a Friend – $80 discount on the Diabetes Educator Course.
Click here to read our newsletter
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]How to Avoid Stigmatizing Kids with Obesity

Sensitive and appropriate language is a real struggle for health care providers when trying to tackle the topic of weight. National Public Radio (NPR) published an article on How Doctors Can Stop Stigmatizing and Start Helping Kids with Obesity, which recognized that many primary care providers may feel awkward in the limited window of time they have to sensitively and effectively find healthy solutions for those struggling with excess weight.
With this struggle, it makes sense that an American Diabetes Association (ADA) study has found many providers, accidentally or otherwise, show weight bias. See, Overcoming Weight Bias in the Management of Patients with Diabetes and Obesity.
The same study explains that weight bias can manifest as an attitude that “patients with obesity are lazy, lack self-control and willpower, personally to blame for their weight, noncompliant with treatment, and deserving targets of derogatory humor.” This is why, NPR explains, “the American Medical Association passed a resolution in 2017 designed to teach health care providers to use ‘people-first language.” Some examples are to avoid the words overweight, obese, or extremely obese and instead use phrases like excess weight or elevated body mass index. And instead of saying “obese patient”, use terms like person with obesity, person with elevated BMI or person with excess weight.
Eliminating weight bias from our written and spoken language is challenging. It requires honest reflection and an open mind. Our whole team at Diabetes Education Services is dedicated to using person centered language. Yet, we are still learning and working on transitioning all of our content to be respectful and free of weight bias.
Language matters and health care professionals are in such an important position to effect change in people’s lives. For more tips on how you can change how you talk about diabetes and weight, see our webinar on Language & Diabetes.
Evaluate your Weight Bias –Harvard’s Project Implicit
Project Implicit is a non-profit organization that provides international collaboration between researchers interested in implicit social cognition – the thoughts and feelings outside of conscious awareness and control. The goal of the organization is to educate the public about hidden biases and to provide a “virtual laboratory” for collecting data on the Internet.
For more information on weight bias and stigma, read our July Newsletter.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]23andMe launches a predisposition test for Type 2 diabetes
This past March, 23andMe, a personal genomics and biotechnology company announced their latest reporting technology, a test that determines a person’s predisposition to Type 2 diabetes.
The test itself is to help people identify what level of risk they may have in developing Type 2. However, it is not meant to imply that the report actually diagnoses a person with Type 2.

The company has recently partnered with Lark Health, a platform that uses artificial intelligence to help people manage chronic disease. The idea is that 23andMe will help identify the risk of chronic disease through the examination of genetic data. Once you are aware of the risk level, you would then use Lark Health to change lifestyle habits.
The release of this test is significant, as it is the first test that utilizes the data collected to examine risk for disease. “For a company like 23andMe, increasing the number of tests they offer adds a lot of value, and can have a snowball effect: the more data they collect, the more tests they can develop and the more tests they offer the more data they can collect (since new tests will drive new users to the service).”
The rates of Type 2 diabetes continues to increase, affecting 1 in 10 Americans and costing more than $327 billion dollars a year. By informing consumers of their risk of Type 2, 23andMe hopes to help increase prevention efforts.
The announcement of the new risk test was met with some push-back, stating that screening tests are already in place, the difficult part is encouraging someone to actually change their habits and lifestyle to better their health.
23andMe hopes that their evidence-based approach with the widespread qualitative diagnosis of pre-diabetes will help people take the diagnoses more seriously.
With diabetes expected to affect half the population, 23andMe is hoping “When customers learn about their genetic likelihood of developing Type 2 diabetes, we believe there is an opportunity to motivate them to change their lifestyle and ultimately to help them prevent the disease.”
To Learn More: 23andMe launches predisposition test for Type 2 diabetes – mobihealthnews
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Could work-related stress increase Type 2 risk in women?
A recent study featured in the European Journal of Endocrinology finds that work stress may contribute to the risk of Type 2 Diabetes, particularly in women.
Recent data shows that 9 percent of the United States population is now living with diabetes and another 84 million people are living with pre-diabetes.
“Risk factors for type 2 diabetes include a lack of physical activity, elevated BMI, being aged 45 years or older, having high cholesterol and high blood pressure, or having a family history of diabetes, heart disease, or stroke.”

There are also psychological risk factors to consider such as depression, which can increase the risk of developing type 2 diabetes. This new study finds that for women, work-related stress may impact their risk of developing diabetes over time.
70,000 women were studied over a 22 year period. During the study, researchers were studying the link between mentally tiring work and the increased risk of developing type 2 diabetes.
75% of the women studied were teachers and expressed that their work was mentally tiring.
Over the 22 year period, 4,187 participants developed type 2 diabetes. However, research revealed that diabetes was considerably higher among participants that deemed their work mentally taxing.
“Specifically, those who said that their job was “very” mentally taxing at the start of the study were 21 percent more likely to develop the condition than women with “little or not mentally tiring work.”
Researchers did consider outside factors, but still found the the rates were the same. The study concluded the importance of stress management in the workplace and how it can affect long term health.
Researchers hope to examine the effects of work-related stress on those already living with type 2 diabetes.
To learn more: Type 2 diabetes: Work stress may increase risk in women – Medical News Today
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Free Resource Friday | Updated Digital PocketCards

FREE Updated PocketCards | Download yours today!
Our digital Injectable Meds PocketCard has been updated in the CDCES Coach App and Online to reflect the new FDA approval of liraglutide (Victoza) for pediatrics (age 10-17) with type 2 diabetes.
Want to learn more about diabetes medications, insulin management and technologies?
Join our Diabetes Ed Course in San Diego, Sept 4-6, 2019. Earn over 30 CEs while having fun!
Medical Myths – Top 10 List

Over 400 common medical practices were contradicted by rigorous research. For this blog, I highlight six widely held theories that are refuted by thousands of studies.
For all 10 myths below and more, we invite you to check out this scientific review led by Dr. Vinjay Prasad of Oregon Health and Science University who said, “Very smart and well-intentioned people came to practice these things for many, many years. But they were wrong.”
Myth – Fish oil reduces risk of heart disease
Truth – In a trial involving 12,500 people at risk for heart trouble, daily omega-3 supplements did not protect against heart disease.
Myth – Step counters and calorie trackers help people lose weight.
Truth – Based on a study of 470 “dieters” who were using digital assistance and tracked for two years, those who wore tracking devices actually lost less weight than those who followed standard advice.
Myth – A single dose of oral opioids to treat emergency room patients works better than medications like aspirin and ibuprofen.
Truth – Clinical trial showed that medications like aspirin and ibuprofen are much safer alternatives which relieve pain just as well among emergency room patients.
Myth – Ginkgo biloba protects against memory loss and dementia
Truth – Made from the leaves of ginkgo trees, this supplement was widely used is promoted as a way to preserve memory. A large federal study, published in 2008, definitively showed the supplement is useless for this purpose.
Myth- Peanut allergy risk is higher if a child is exposed to peanuts before age three.
Truth – Children exposed to peanuts before age 1 have no greater risk of peanut allergies.
Myth – Lifelike doll carried around by teenager will prevent unplanned pregnancy
Truth – It turns out that these “infant simulators” were actually associated with a slightly increased risk of pregnancy.
For a complete list as published in the New York Times article, 10 Medical Myths We Should Stop Believing. Doctors, Too.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
1 in 3 Young Adults Suffers From Loneliness in the U.S.
A new study suggests that suffering from loneliness is common for young adults between the ages of 18-24. Even young and active adults can feel isolated.
Data from 1200 participants revealed that at least 20% felt “left out,” lonely or isolated at times and provided low ratings for mental and physical health.
Loneliness was more commonly reported in adults younger than 25 with 30%, where only 11% of adults 65 and older reported similar feelings.
The “Loneliness Epidemic” has been highlighted by many studies and supported by numerous researchers. “Last year, a study of more than 20,000 U.S. adults found that nearly half felt lonely at least sometimes. And only 53 percent said they had meaningful face-to-face interactions everyday.”
Researchers believe this is no longer just a social issue and should be considered a public health issue. Chronic loneliness is linked to an increased risk of hyptertension, cardiovascular disease, dementia, and other mental health issues.
“It’s possible the relationship goes in “both directions” — with loneliness and health issues feeding each other.”
The lead researcher on the study, Dr. Rebecca Mullen, talks about the difference between being lonely and having “alone time.” Alone time in many cases can be healthy and many people are happy to be alone.
“Subjective loneliness is different. It makes people feel bad. And, Maddux said, that can come with a “whole package” of issues, like poor diet, poor sleep and time spent on the couch instead of being physically active.”
Maddux dives into theories as to why a typically socially active group, ages 18 – 24, would be suffering from loneliness. In the age of smartphones, Maddux believes this may be robbing young people of face to face interactions. A number of studies support this theory stating that screen time is directly correlated with depression and loneliness.
“Young people, she added, may have a harder time keeping those social media experiences in perspective — and understanding that when other people post, they are probably trying to present their lives in the shiniest terms possible.”
It is important to address your own feelings of loneliness, but also recognize the signs in others. It is easy for someone to isolate themselves. Maddux hopes to destigmatize the issue in order to shed some light on the importance of mental health and community.
To learn more: 1 in 3 Young Adults Suffers From Loneliness in the U.S. – HealthyDay
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]







