
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

In May 2023, the FDA approved the Beta Bionics iLet Bionic Pancreas insulin pump for individuals 6 years and older. This is the first automated insulin delivery (AID) system to eliminate the need to enter carbohydrate (carb) counts for meals or snacks.
With over 1 million people worldwide utilizing insulin pump therapy, removing the intricate skill of carb counting has grabbed the attention of the diabetes community.¹
Diabetes is a disease that can be overwhelming, causing a substantial risk of distress and burnout. As a diabetes health care professionals, you help individuals living with diabetes choose technology to enhance their self-management and reduce some of the associated burdens.
The iLet Bionic Pancreas is a continuous subcutaneous insulin infusion (CSII) system, also commonly referred to as an insulin pump. Like other tubed insulin pumps on the market, it features a small cartridge that holds insulin, an operating system that delivers the insulin, integration with a continuous glucose monitor (CGM), and is connected to the body via tubing with an insertion set.
CGM compatibility includes:
☑️ Dexcom G6
☑️ Dexcom G7
☑️ Libre 3+
The Bionic Circle app enables iLet users to invite up to 10 friends or family members to view alerts, blood glucose trends, meal announcements, and insulin doses. Healthcare providers utilize the Healthcare Provider Bionic Portal to download iLet data for review during office visits or for remote patient monitoring.
The most significant difference with the iLet is that there are NO traditional pump settings. The only initial settings used are the individual’s weight and target range. Because there are no traditional settings, there is no user input for corrections or carb counting.
Three different algorithms drive insulin delivery. Let’s look at each algorithm²:
Basal Algorithm
Corrections Algorithm
Meal Announcement Algorithm
The only adjustable setting is the glucose target range. There are three different glucose targets to choose from. Two different blood glucose targets can be set within a 24-hour period.³
When using the iLet there are a few crucial points to consider:
🥖 Carbohydrate education is not gone! Although no carb counting is required, clients must be aware of carbs. They will still need a basic understanding of which foods contain carbs to accurately determine the size of the meal.
📲 There are no traditional pump settings to manage. The only setting that can be changed is the target range. Education is key for clients who would self-adjust pump settings with previous insulin pumps.
🏃♂️ Managing exercise has changed. There is no exercise mode, activity mode, or temp basal setting to adjust insulin delivery for physical activity. Please see tips from Beta Bionics on managing physical activity with the iLet at https://www.betabionics.com/articles/exercise/.
As a diabetes healthcare professional, you support individuals living with diabetes in setting personalized goals and developing tailored treatment plans. After assessing the client’s needs and barriers, you may find that they are overwhelmed or distressed by the constant need for carb counting. You may also find those who prefer to be ‘hands-off’ with their diabetes for many reasons. These individuals may find that an AID system like the iLet can improve glycemic control without increasing treatment burden.
If you’re looking for more information on diabetes technology or identifying barriers to self-management, join our 2-Day Training Seminar in San Diego to help those living with diabetes continue to thrive.
References
Association of Diabetes Care and Education Specialists. (n.d.). The DCES and pump therapy. Danatech Diabetes Technology. https://www.adces.org/education/danatech/insulin-pumps/pumps-in-professional-practice/dces’s-and-pump-therapy
Beta Bionics. (n.d.). HCP webinars. https://www.betabionics.com/hcp/hcp-webinars/
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements. See Training Schedule Here >>
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Didn’t pass the CDCES exam? It’s okay — and you’re not alone. Over 30% of healthcare professionals don’t pass on their first try. This setback doesn’t define you — it’s just part of the journey.
Join Coach Bev for a FREE, supportive webinar to help you:
Regroup and refocus
Avoid common pitfalls
Build a clear action plan
Boost your confidence for next time
With 25+ years of experience coaching thousands of diabetes care professionals, Coach Bev is here to help you turn this moment into a comeback.
You’ve got this — and we’ve got you.
👉 Register Now

Menopause brings hormonal and metabolic changes that can complicate diabetes management. This webinar explores how menopause impacts glycemic control and insulin resistance — and what clinicians can do about it.
Key Takeaways:
Understand how menopause affects glucose metabolism
Recognize its impact on diabetes self-management
Evaluate hormone therapy options for people with type 2 diabetes
Apply individualized care strategies, including lifestyle and symptom management
Know when to refer or collaborate with menopause specialists
Objective:
Use evidence-based approaches to support people managing both diabetes and menopause for better outcomes.

Register above or simply visit our Online Store at DiabetesEd.net.
For more information or any questions, please email [email protected].
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | The Impact of Adverse Childhood Experiences on Health awards 1.0 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
All hours earned count toward your CDCES Accreditation Information
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

Monitoring carbohydrates remains a key strategy for managing blood glucose in both type 1 and type 2 diabetes¹. While not suitable for everyone, carbohydrate management strategies have shown overall improved glycemic outcomes and can promote greater awareness of dietary intake.
Advanced carbohydrate counting often requires not only knowing the amount of carbohydrate in a food but also understanding the impacts of mixed meals (including fats, proteins, and fiber content) and the glycemic impact of specific food choices relative to insulin dosing. This becomes especially challenging when dining out, eating mixed dishes, navigating unfamiliar food choices, estimating portion sizes, or consuming meals without nutrition labels². Variability in preparation methods and hidden ingredients can further complicate accuracy.
Apps and generative artificial intelligence (GenAI) can now analyze not only total carbohydrate content but are now starting to consider factors such as meal composition, glycemic load³, individual glycemic responses⁴ and even individual microbiome.
These tools offer the potential for more personalized information.
Apps like SNAQ, MyNetDiary, MyFitnessPal, SnapCalorie, and many others now in app stores are integrating AI and image recognition. These apps enable users to take a photo of their meals, and the app then identifies specific foods, estimates portion sizes, and provides a breakdown of the meal’s nutritional content. Apps such as Undermyfork, RXFood, January AI, GlucoseBuddy with Meal IQ, GlucoSense AI, and again many more go further by integrating CGM data, insulin/medication dosing, and physical activity to provide personalized glucose insights.
Recently, the Dexcom G7 app added a Smart Food Log feature that utilizes AI to generate meal descriptions from food photos. This feature could simplify the logging process and help both diabetes care providers and individuals living with diabetes interpret meals consumed and glucose data. As a dietitian, this feature has been supportive due to its ease of use and reduced app burden for my clients. Having food information integrated into a tool an individual already uses can boost engagement and lead to meaningful discussions about meal planning and insulin dosing strategies. While the feature doesn’t yet provide detailed carbohydrate or nutrient analysis, there is much to gain by just knowing what individuals are consuming.
They compared two GenAI platforms for accuracy in calculating the amount of carbohydrates in fifty packaged and non-packaged meals, including the addition of minimal, moderate, or extensive descriptive data. As we have learned with all language learning models, accuracy is improved when more specificity is added. They found that with full details, such as weight, meal descriptions, and pictures, the meal’s absolute percentage error was 13.7% and 13% for ChatGPT and Gemini, but with minimal conditions the error was 34.8% and 45%, respectively.
Additionally, ChatGPT exhibited substantial variability in accuracy between non-prepackaged and prepackaged meals. In terms of time, for improved accuracy entering the additional condition details would be like manually entering data into a food database. Apps can frequently misidentify foods that look alike, struggle with portion accuracy, and have trouble understanding how a dish was prepared or what ingredients are hidden.
In one AI meal app, my hummus, consumed with celery, was incorrectly identified as peanut butter, and the portion was close, but it underestimated the actual amount. However, for individuals with significant or inconsistent carb estimation errors it may still lead to clinically significant improvements.
For example, a recent study⁵ found clinically meaningful (where carbohydrate estimates were off by more than 10 grams) estimation errors in 45% of meals logged by patients themselves, but only in 38% using the SNAQ app; the outcomes for diabetes clinical indicators is unknown. These studies showed the potential of AI tools to enhance carbohydrate estimation, but also highlights the need for continued model improvements and user validation.
Apps and GenAI may have fees and can become too costly; they require internet access and smartphone use, and may be a barrier for individuals with limited digital literacy. The 2025 ADA Standards of Care emphasize that while diabetes technology has the potential to improve outcomes, access disparities exist. If these tools lead to meaningful outcomes, we must also consider barriers to access.
We can utilize the ADCES ICC framework to select, configure and ingrate apps⁶ for each individual. As AI continues to integrate into diabetes management, meal monitoring is just one area of consideration. As a diabetes health care professional, exploring these tools for their value and faults can help us improve our understanding of usability and address concerns.
References
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit (taught by blog author, Christine Craig, MS, RD, CDCES) and bonus content that also meets CDCES renewal requirements. See DiabetesEd Training Schedule Here >>
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Invite your colleagues!! Join us August 19th @ 11:30am PST!
Coach Beverly will review examination process, sample test questions, and the reasoning behind choosing the BEST answers. Gain valuable insights on the exam content and boost your knowledge and test taking confidence. Hope to see you there!
News Flash! Starting in January 2025, this exam changed hands. The BC-ADM is now owned by the CBDCE, along with the CDCES certification.
This webinar highlights how this ownership change impacts the exam process and answers your questions about achieving Board Certification in Advanced Diabetes Management.
Webinar topics:
There’s still time to register!! Join us August 20th @ 11:30am PST!
Register above or simply visit our Online Store at DiabetesEd.net.
For more information or any questions, please email [email protected].
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
At Diabetes Education Services, we’re committed to giving healthcare professionals the opportunity to gain the skills and training they need to become confident, impactful diabetes educators. That’s why we’re thrilled to announce two special scholarships designed to help you advance your skills, earn valuable continuing education credits, and bring high-quality diabetes care to the communities that need it most.
Scholarship Offerings:
-10 Bridge Scholarships for our CDCES Prep Bundle
-2 Making a Difference Scholarships for our DiabetesEd Training Seminar in San Diego.

For 26 years, the San Diego DiabetesEd Conference has brought together healthcare professionals from across the country .🌟 This event blends cutting-edge diabetes education with connection, fun, and inspiration.
We’re committed to breaking down financial barriers so a diverse group of healthcare professionals can attend and make a lasting impact in their communities. This year, we have something extra special: the “Making a Difference” Scholarship is now open!
We are offering two scholarships that cover the $559 registration fee for our San Diego DiabetesEd Live Training Seminar.
Here’s what you’ll receive if selected:
-2 days of in-person learning in beautiful San Diego
-12 bonus virtual courses you can access for an entire year
-30+ CE credits from accredited bodies including AMA, ACPE, ANCC, and CDR
-A chance to network, learn, and grow with a passionate community of healthcare professionals
Applications Close: August 29th
Please note: Travel and lodging are not included.
1.) We have hosted this conference for 26 years with thousands of super satisfied program attendees! 🌟 Avg rating 4.8/5.
2.) You will not only learn a TON of super helpful info, you will have fun doing it! 🤩
3.) You will win prizes, eat nutritious and delicious foods, and play games. 🎉
4.) You will have time to network, share stories and connect with your colleagues. 👥
5.) You will be prepared to take your CDCES and BC-ADM certification exams.
6.) You will enjoy bay walks, 🌴palm trees and gorgeous sunsets!
7.) Earn 30 CE’s ⚕️, which includes 2 days of live content and over 12 BONUS recorded CE Courses -good for one year!
Earn 30 CE’s through the following accrediting bodies:
|
|
At Diabetes Education Services, we believe cost should never stand in the way of professional growth. That’s why we’re excited to open applications for the Bridge – Making a Difference Scholarship to giveaway 10 CDCES Online Prep Bundles — a comprehensive virtual program to help you prepare for the Certified Diabetes Care and Education Specialist (CDCES) exam.
If you’re committed to advancing your skills, earning your CDCES credential, and improving access to diabetes care in underserved areas, we invite you to apply.
What the Scholarship Covers ✨
-Full registration for the CDCES Online Prep Bundle
-Comprehensive online training to prepare you for the CDCES exam
-1-year access to all course materials and resources
-30+ CE credits through accredited bodies (AMA, ACPE, ANCC, CDR)
Applications close Aug. 29th and recipients will be announced on Sept. 5th. Don’t miss your chance to take the next step toward your CDCES and join a supportive network of like-minded professionals.🌟
By: Beverly Thomassian with excerpt from, Healing through Connection.
We have all struggled with feelings of discouragement or self-doubt.
This is especially true when a HCP doesn’t pass their CDCES Exam. I encourage you to acknowledge your disappointment AND keep moving forward! This IS a really tough exam and over 30% of really smart and successful healthcare professionals, just like YOU, don’t pass the exam on their first try. If you are in this boat, be reassured that you are not alone.
You CAN pass this exam by making a few adjustments to your approach! I have seen it happen time and time again!
Over the past twenty years, I counseled and encouraged dozens of disheartened healthcare professionals who did not successfully pass the CDCES exam to keep trying! There have been plenty of tears and insights during these coaching sessions – for both me and the HCP on the other end of the line. As we explore the test-taking experience and its results, a recurring discovery emerges.
The majority of test-takers hold the answers to the questions inside them, but there are consistent barriers that block the best answer from taking center stage.
These common barriers are often linked to fear sprinkled with a little bit of self-doubt.
You will notice that the first four barriers have nothing to do with knowing the content, memorizing the medication names, or knowing common carb portions. It has to do with our critical internal dialogue and difficulty believing in our abilities and knowledge- which I completely understand! I have been there! (see excerpt from Chapter 3 from Healing through Connection below.)
Not passing the CDCES exam can feel disheartening—but you are not alone. Over 30% of healthcare professionals don’t pass their CDCES on their first try.
Join Coach Bev on August 26th for this free, supportive webinar designed to help you regroup, refocus, and reignite your confidence. Bev will share practical tips, common pitfalls, and an action plan to boost your readiness for next time. With over 25 years of experience training thousands of diabetes care professionals, Coach Bev believes in your ability to pass—and she’s here to walk with you every step of the way. Let’s turn this setback into a powerful comeback. You’ve got this!
Topics covered include:
• Strategies to address test anxiety.
• Tips to experience exam success.
• Review of study tips and test-taking practice questions.
We will review the examination process, sample test questions, and the reasoning behind choosing the BEST answers. We believe in your success!
Everyone has moments of self-doubt, especially when you are
expected to be the expert with a quickly accessible best response. It’s
natural to second-guess yourself when put on the spot, wondering if
you’re offering the correct information or making the best choice.
But deep down, beneath the layers of self-doubt, I encourage you
to tap into that quiet but unwavering belief that you will figure out
what it will take to succeed. This inner assurance reminds you that,
even in unfamiliar territory, you have the capacity to learn, adapt, and
grow. This is an important consideration: confidence doesn’t always
come from knowing everything at the outset but from trusting your
ability to acquire the skills and knowledge needed along the way.
I needed to learn that lesson the hard way by looking my fear in the face.
A strange combination of fear and courage defined my midtwenties to early thirties. In this decade, fear of failure became my constant companion and greatest motivator. Since childhood, the fear of not being good enough had shadowed me, urging me to push harder, do better, and keep proving that I was worthy of love. This fear had a particular benefit—the more doubt whispered into my ear, the more it fueled my fierce determination to prove it wrong.
This complicated relationship with fear has, at times, held me in its grip, inflicting me with intense feelings of self-doubt. Yet, paradoxically, it has also propelled me toward achievements I never thought possible. My own experiences with self-doubt and fear have sharpened my ability to recognize it in others when providing care. This recognition creates a powerful connection and allows me to hold space for their fear while reflecting back my belief in their
strength and resilience.
It’s for those moments when selfdoubt whispered that you weren’t ready or good enough, and that voice stopped you from going after that dream job, taking that certification exam, asking for the raise you deserved, or daring to do something bold to improve patient care. You’ll learn how you can reframe those feelings as fuel for growth. Through shared stories and insights, you will start to see fear not as a barrier but as a steppingstone toward greater resilience, courage, and fulfillment.

Get ready for two days of expert-led, info-packed learning at our in-person DiabetesEd Live Seminar! Whether you’re preparing for your certification exam or looking to sharpen your clinical skills, this intensive event is designed to give you the tools, confidence, and knowledge you need.
💡Ideal for exam prep and clinical refresh
💡 Interactive sessions with real-world applications
💡Network with peers and diabetes care experts
📅 Mark your calendar — October 22–23
📍 San Diego – beautiful location, powerful learning!
Diabetes Education Services has teamed up with Partners for Advancing Clinical Education (Partners) to expand our accreditation offerings.
You can now earn CE credit for the Live San Diego Conference through the following accrediting bodies:
“Making a Difference” Scholarship for DiabetesEd Seminar is now open!
We are geared up to help grow and mentor future Certified Diabetes Care and Education Specialists (CDCES) to meet the increasing and varied needs of our diabetes community.
We are offering 2 DiabetesEd Seminar “Making a Difference Scholarships” which cover the registration cost for our most popular DiabetesEd Live Training Program in San Diego. This two day live conference will provide you with diabetes fundamentals and beyond! Earn 30+ CE’s with access to the courses for one year! Valued at $559*. (*Travel and lodging expenses not included.)
Applications Close Aug 29th
Recipient announced Sept 5th
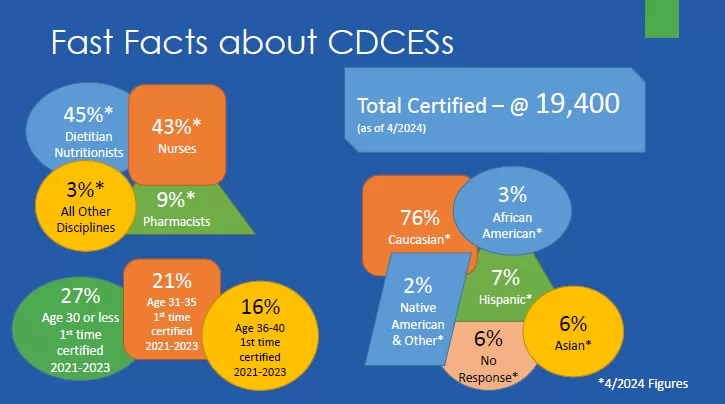
Over the next 10 years our goal is to welcome 500 new diabetes education specialists into the field. If you know a healthcare professional seeking a new challenge and eager to pursue a meaningful and rewarding specialty, please invite them to consider becoming a Certified Diabetes Care and Education Specialist (CDCES).
Diabetes Education Services is committed to improving equity and access to diabetes training and education for a diverse group of healthcare professionals. We don’t want financial barriers to stop anyone from attending this conference. These scholarships are an appreciation of those who are role models and advocates for practicing the best diabetes care in their communities.
The Diabetesed Training Scholarship program is not just about learning—it’s about creating connections, fostering growth and building a community of passionate diabetes care professionals. We are excited to offer this incredible opportunity to those who are committed to advancing their skills and knowledge in diabetes education. Together, we can make a real difference in the lives of those living with diabetes.
These scholarships are awarded to healthcare professionals who provide care and education to under-served communities that lack access to Diabetes Specialists and healthcare resources. Applicants must be in the process of gaining practice hours and planning to take their CDCES Exam within the next 3 years.
Applications Close Aug 29th
Recipient announced Sept 5th
The goal of these scholarships are three-fold:
Who is eligible?
If you are a healthcare professional who wants to learn the steps to enter the rewarding field of diabetes education, we have created a new FREE webinar that outlines the benefits and steps involved in “Becoming a Diabetes Specialist.”
We want to share this information with as many healthcare professionals as possible to encourage them to consider specializing in diabetes. Our goal is to cast this net far and wide to address the rising prevalence of diabetes and empower health care professionals to enter the field.
Visit this page to gain ideas on how to get your 1000 practice hours and to use our hours tracker.
Visit the official CBDCE website or relevant professional bodies for more detailed guidance or recent updates.
Visit our CDCES Prep Page for more information and to register for FREE Webinars with lots of helpful information.
We believe in your success! Learn the steps involved in preparing for the certification exams, earning CEs, and gaining confidence as a Diabetes Education Specialists and more!
Take a trip through our 10 Step Roadmap to Success for easy access to the tools and resources you need to succeed at either or both certification exams!
Want to learn more about our accreditation and how our CEs can help you meet the requirements for the CDCES exam? Click above to explore the details of our accredited courses.
Coach Beverly’s goal is to support our Diabetes Education Community and provide meaningful resources that are useful for your daily practice. Please enjoy these FREE resources that we have put together for you.
Our FREE webinars will help you discover the steps required to become a CDCES and will transform your test anxiety into calm self-confidence and test-taking readiness.
Can’t join us live?
Don’t worry, if you register, we will send you a link to the recorded version.
If you are a health care professional considering becoming a CDCES and want to learn more about eligibility and benefits of joining the Diabetes Education Community, this FREE webinar is for YOU. Coach Beverly will provide clarification on requirements, exam content, and study strategies to prepare for success.
We will review examination process, sample test questions, and the reasoning behind choosing the BEST answers.
Building a Bridge Program: At Diabetes Education Services, our goal is to mentor the next generation of Certified Diabetes Care and Education Specialists (CDCES). We are committed to welcoming healthcare professionals with diverse experiences and backgrounds to enter the diabetes field. Our online programs and scholarship programs aim to provide emerging CDCES professionals with the knowledge, skills, and confidence to address the unique challenges encountered by people with diabetes from all walks of life, while also preparing them for certification.

Author, Nurse, Educator, Clinician, and Innovator, Beverly has specialized in diabetes management for over twenty years and has successfully passed the CDCES exam six times. As president and founder of Diabetes Education Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
“Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian
“The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.“
– Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes.
Reason 2: Currently, 13% of people in the U.S. have diabetes and another 36% have pre-diabetes which means 49% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities.
Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.
SJ is a 62-year-old long-haul truck driver with type 2 diabetes for the past 18 years. They take basal insulin nightly and metformin twice daily. Despite consistency of medications and a recent focus on lifestyle changes, Time in Range remains at 5% with a GMI of 9.2%. Last A1c was 9.7%. No history of hypoglycemia nor signs of retinopathy or neuropathy are documented. Incretin therapy or SGLT-2 inhibitor has been recommended but SJ shares that the insurance share of cost makes those medications unaffordable. SJ has an erratic schedule and drives across multiple states for work. They report fatigue during long drives but denies difficulty with driving nor any episodes of low blood glucose. SJ is motivated to improve diabetes management but is concerned about their livelihood if license were to be impacted.
As the diabetes care and education specialist, which of the following is the most appropriate next step in SJ’s care plan?
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants will be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.