Heart Health improves Brain Health
 Exciting study results were just released by the Journal of the American Medical Association. This study assessed cardiovascular health in older adults and sought to find an association between cardiovascular health and risk of dementia.
Exciting study results were just released by the Journal of the American Medical Association. This study assessed cardiovascular health in older adults and sought to find an association between cardiovascular health and risk of dementia.
The results, published Tuesday, is a clear message to health care professionals and people with diabetes alike.
Focus on cardiovascular fitness for the sake of preserving cognitive health, experts said.
Cardiovascular health is commonly linked to chronic diseases of the body. However, taking care of cardio vascular health seems to have positive affects on brain health.
The study included 6,626 individuals aged 65 or older from various areas in France. Their scores of cardiovascular health were assessed using seven measures: diet, exercise, weight management, smoking status, blood pressure, blood sugar, and cholesterol. The subjects were given, “a score of 0,1, or 2 for each of the categories to reflect whether their compliance with the measures were poor, intermediate, or optimal.”
Results were compelling, “6.5% of study participants had optimal measurements for at least five of the seven categories.” With each additional measure met at optimal levels, “the risk of dementia fell by about 10%.” The study also took place over 8.5 years in which 745 of the 6,626 subjects were diagnosed with dementia.
Among the individuals with the lowest scores for cardiovascular health, risk for dementia increased “at a rate of 13.3 cases per 100 people.” Compared to those with the highest scores for cardiovascular health had much lower rates at 7.1 cases per 100 people. These results should encourage physicians and other medical professionals to understand and teach the importance of cardiovascular health to preserve cognitive function in their patients.
For more information on cardiovascular health and cognitive function, read the official study Association of Cardiovascular health level in older age with cognitive decline and incident dementia.
A summarized version by the Los Angeles Times may be accessed at The more you do to promote your cardiovascular health, the lower your risk of dementia.
Contributed by Sofia Sepulveda
30 Million Americans Now Have Diabetes
 Sharp increases in diabetes are being reported by the U.S. Centers for Disease Control and Prevention (CDC).
Sharp increases in diabetes are being reported by the U.S. Centers for Disease Control and Prevention (CDC).
14% of adults living in the United States now have diabetes and only 10% are aware of it.
This translates into 1 in 7 Americans living with diabetes. The CDC believes a number of factors are responsible for the sudden increase, including an aging population and an epidemic of obesity. 95% of diabetes cases are Type 2 and are tied to lifestyle factors, where as 5% are Type 1 and typically are diagnosed early in life and do not correlate with lifestyle choices.
- Surprisingly, many more men are now living with diabetes. The study revealed that 16% of men and 12% of women have diabetes.
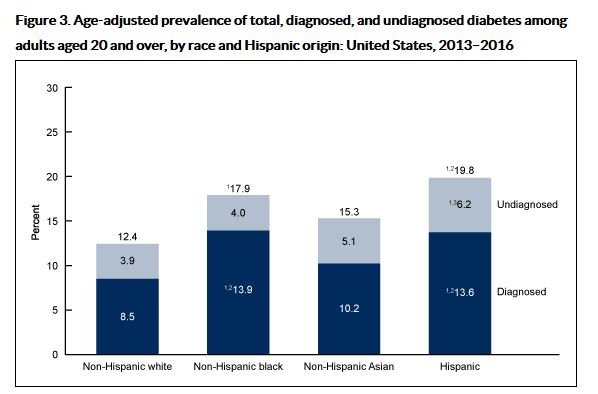
- Diabetes is also more common within certain groups. 20% of Hispanics, 18% Blacks and 15% Asians and 12% whites are living with type 2 Diabetes, according to data collected via the U.S. National Health and Nutrition Examination Survey.
People who are overweight and obese are also more likely to develop diabetes, the researchers found. Only 6 percent of underweight or normal-weight adults had the disease, while 12 percent of overweight adults and 21 percent of obese adults did.
Although treatment for diabetes is available, said lead researcher Mark Eberhardt, an epidemiologist at CDC’s National Center for Health Statistics (NCHS). The public health goal should be taking steps to prevent the disease. “Sometimes prevention is the best treatment,” he said.
As Diabetes Educators, we can take a leadership role in our communities by creating and supporting diabetes prevention programs and by providing amazing care to people living with diabetes.
 Learn more about starting a Diabetes Prevention Program on our Prevention Resource Page.
Learn more about starting a Diabetes Prevention Program on our Prevention Resource Page.
To learn more, visit the CDC Website National Center for Health Statistics Site
To learn more: 30 Million Americans Now Have Diabetes – Health Day
Source: Prevalence of total, diagnosed, and undiagnosed diabetes among adults: United States, 2013–2016.
NCHS Data Brief, no 319. Mendola ND, Chen T-C, Gu Q, Eberhardt MS, Saydah S. Hyattsville, MD:
National Center for Health Statistics. 2018.
Losing sleep can lead to weight gain
 Sleep is possibly the most overlooked aspect of successful weight loss. While there is a well known link between obesity and sleep, the actual role sleep plays in appetite regulation and glucose metabolism is often overlooked.
Sleep is possibly the most overlooked aspect of successful weight loss. While there is a well known link between obesity and sleep, the actual role sleep plays in appetite regulation and glucose metabolism is often overlooked.
A recent study conducted by Uppsala University in Sweden found evidence that, “lack of sleep encourages the body to store more fat, altering the body’s metabolism.” The study demonstrated that even a small shift in an individual’s sleep schedule may have significant effects on metabolism leading to weight gain.
“Chronic sleep loss, social jet lag, and shift work—widespread in our modern 24/7 societies—are associated with an increased risk of numerous metabolic pathologies, including obesity, metabolic syndrome, and type 2 diabetes,” researchers explain in the new study. “Even minor weekly shifts in sleep timing, or as few as five consecutive nights of short sleep, have been associated with an increased risk of weight gain in healthy humans.”
In this study, fifteen volunteers were separated into two groups. One group received a normal night’s sleep and the other group had no sleep. Both groups gave samples of fat, muscle tissue, and blood. They were also asked to keep a food diary for the duration of the experiment.
The most significant difference was in gene activity referred to as DNA methylation. This activity, “was linked to cells increasing their tendency to absorb lipids, boosting the body’s ability to store fats.” The participants who received no sleep also had a decreased ability to build or at least maintain muscle mass. Their bodies also experienced an increased state of inflammation and a higher risk for developing type 2 diabetes.
To learn more: “Losing sleep can lead to more extra pounds” ZME Science
Diabetes Educators as Nutrition Coaches for Providers
 Providers often share nutrition recommendations with patients. In spite of best intentions, sometimes these recommendations may not match latest standards or reflect evidence based studies . A survey by the Nutrition and Lifestyle Working Group of the American College of Cardiology sought to understand just how much nutrition education physicians were actually receiving during medical school and throughout their careers.
Providers often share nutrition recommendations with patients. In spite of best intentions, sometimes these recommendations may not match latest standards or reflect evidence based studies . A survey by the Nutrition and Lifestyle Working Group of the American College of Cardiology sought to understand just how much nutrition education physicians were actually receiving during medical school and throughout their careers.
The results of this survey concluded that while nearly 70% of physicians believed that nutrition education is vital in healing process, only 57% engaged in direct discussion with their patients. Almost 25% of physicians, “recall receiving no nutrition education in medical school” and 35% said their knowledge of nutrition, “often came from a single lecture.” In residency, a shocking 73% received no nutrition education whatsoever. With nutrition being a vital aspect of the healing process, it is hard to ensure you are receiving a complete treatment plan when physicians may not have the proper education to support their recommendations.
For Diabetes Educators, this provides a wonderful opportunity to coach our referring providers on the latest nutrition guidelines. This can be accomplished by sending brief nutrition updates to providers, inviting guest speakers who have expertise on the latest nutrition guidelines and other strategies. Since we work in interdisciplinary teams, maintaining professional respect is an important aspect for long term collaboration and growth.
With the rise of CVD, Type 2 Diabetes, and other health conditions an intervention is required. “Improving education of physicians through more comprehensive nutrition training in medical schools and advanced postgraduate training is an essential step that can facilitate improvement.”
To learn more about the lack of nutrition education in our healthcare system, visit The Deficit of Nutrition Education of Physicians.
Serious genital infection alert with SGLT2 inhibitors
FDA warns about rare occurrences of a serious infection of the genital area with SGLT2 inhibitors
The U.S. Food and Drug Administration (FDA) is warning that cases of a rare but serious infection of the genitals and area around the genitals have been reported with the class of type 2 diabetes medicines called (SGLT2) inhibitors. This serious rare infection, called necrotizing fasciitis of the perineum, is also referred to as Fournier’s gangrene.
Please let patient know about this new warning to be added to the prescribing information of all SGLT2 inhibitors.
Patients should seek medical attention immediately if they experience any symptoms of tenderness, redness, or swelling of the genitals or the area from the genitals back to the rectum, and have a fever above 100.4 F or a general feeling of being unwell. These symptoms can worsen quickly, so it is important to seek treatment right away.
Health care professionals should assess patients for Fournier’s gangrene if they present with the symptoms described above. If suspected, start treatment immediately with broad-spectrum antibiotics and surgical debridement if necessary. Discontinue the SGLT2 inhibitor, closely monitor blood glucose levels, and provide appropriate alternative therapy for glycemic control.
Fournier’s gangrene is an extremely rare but life-threatening bacterial infection of the tissue under the skin that surrounds muscles, nerves, fat, and blood vessels of the perineum. The bacteria usually get into the body through a cut or break in the skin, where they quickly spread and destroy the tissue they infect. Having diabetes is a risk factor for developing Fournier’s gangrene; however, this condition is still rare among diabetic patients. Overall published literature about the occurrence of Fournier’s gangrene for men and women is very limited. Publications report that Fournier’s gangrene occurs in 1.6 out of 100,000 males annually in the U.S., and most frequently occurs in males 50-79 years (3.3 out of 100,000).1-3 In our case series, however, we observed events in both women and men.
In the five years from March 2013 to May 2018, we identified 12 cases of Fournier’s gangrene in patients taking an SGLT2 inhibitor. This number includes only reports submitted to FDA* and found in the medical literature,4-6 so there may be additional cases about which we are unaware. In 2017, an estimated 1.7 million patients received a dispensed prescription for an SGLT2 inhibitor from U.S. outpatient retail pharmacies.7 Although most cases of Fournier’s gangrene have previously been reported in men, our 12 cases included 7 men and 5 women. Fournier’s gangrene developed within several months of the patients starting an SGLT2 inhibitor and the drug was stopped in most cases. All 12 patients were hospitalized and required surgery. Some patients required multiple disfiguring surgeries, some developed complications, and one patient died. In comparison, only six cases of Fournier’s gangrene (all in men) were identified in review of other antidiabetic drug classes over a period of more than 30 years.
To help FDA track safety issues with medicines, we urge patients and health care professionals to report side effects involving SGLT2 inhibitors or other medicines to the FDA MedWatch program, using the information in the “Contact FDA” box.
For more information, please see the FDA Warning Post
Download our Diabetes Medication Pocket Cards
We need more time to provide diabetes education – let legislators know!
More time needed to provide diabetes education – Support Medicare Expansion Bill
3 things you can do today |
Back to School – Extend your Courses and Save!
It’s not too late to finish your homework!
Not able to complete your Online University courses?
Go “Back to School” and extend your courses for an additional year!
Online Course Bundle Extensions
Have you run out of time to study, but still want to access your courses?
Extend your courses for one additional year for a small fee. You can purchase the extension while your courses are still accessible, or when they expire.
10 Spots Remaining | Diabetes Ed Course
10 Spots Remaining at the Diabetes Educator Course | San Diego, CA – September 5th-7th, 2018

Sign up now to reserve your spot, space is very limited!
“More than a course, it’s an experience!”
Come join us at our Level 2, Diabetes Educator Course in sunny San Deigo, California. Whether you are new to diabetes or a seasoned expert, you’ll leave our live seminars with the latest research plus teaching tools you can immediately apply to your clinical practice. Beverly and her teaching team translate the complex science of diabetes into understandable terms, while keeping it real, practical and fun.
Dates: September 5th – 7th, 2018
Diabetes Educator Course San Diego Brochure