
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

Live Webinar – Mindful Eating for Successful Diabetes Management
📅 June 11, 2025 | 🕚 11:30 AM PST
Join Evgeniya Evans, MS, RDN, CDCES, for a powerful, practice-based webinar designed for healthcare professionals. Discover how to integrate mindful eating strategies into diabetes care to support improved glycemic outcomes, emotional well-being, and sustainable lifestyle changes.
You’ll explore evidence-based tools, cultural adaptations, and real-world techniques for helping individuals build a healthier relationship with food.
✅ Practical strategies
✅ CE-focused learning
✅ Tools you can use immediately in your practice
Reserve your spot now and empower your care recipient with mindful, meaningful nutrition care. Includes video, podcast, quiz, and resources—available on-demand for 1 year.
Live Webinar – From Tots to Teens: Pediatric Diabetes Standards
📅 June 12, 2025 | 🕚 11:30 AM PST | 🎓 1.75 CEs
Join us for this Level 2 course focused on the unique needs of children and teens with diabetes. Taught by nationally recognized expert Beverly Thomassian, RN, MPH, CDCES, BC-ADM, this session will guide you through updated guidelines for Type 1 and Type 2 diabetes in youth—covering clinical care, growth milestones, psychosocial considerations, and strategies to prevent complications.
💡 Designed for healthcare professionals working with pediatric populations
📘 Includes standards of care, goals of therapy, and age-appropriate approaches
🧠 Great prep for certification or to strengthen your clinical knowledge.
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

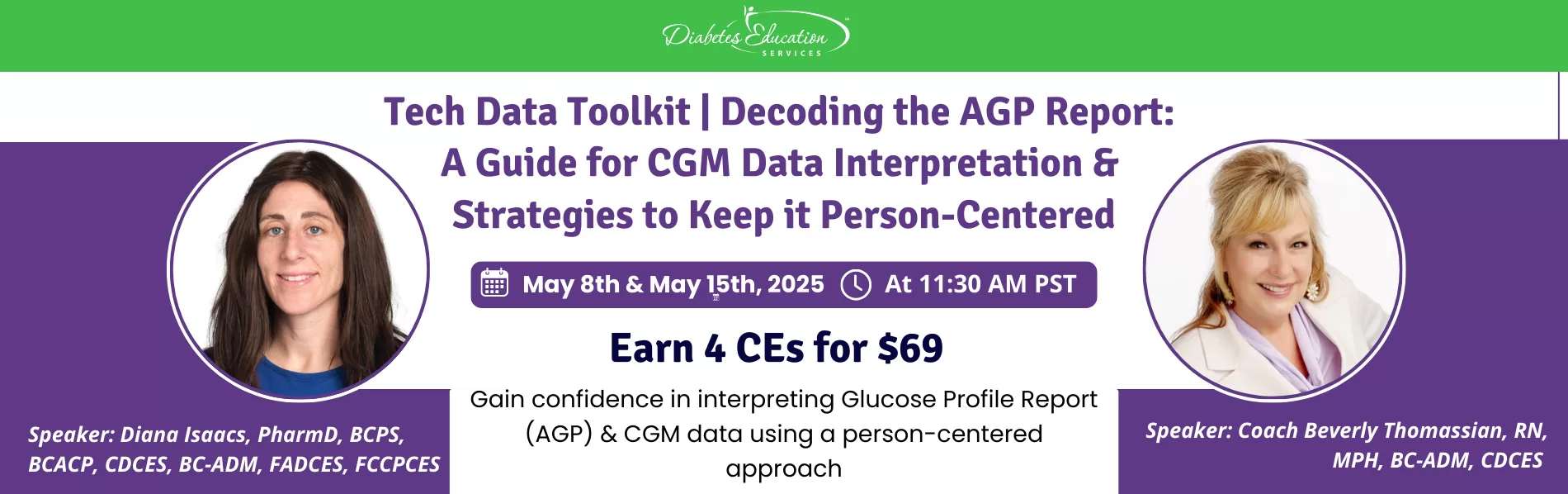
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
Upon completion of this activity, participants should be able to:



Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
CEO of DiabetesEd Services
Christine Craig, MS, RD, CDCES
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
 Christine Craig, MS, RD, CDCES – CEO of Nutrition for Daily Living
Christine Craig, MS, RD, CDCES – CEO of Nutrition for Daily LivingDisclosures:
Christine Craig has the following relevant financial relationships:
Bio:
Activity Start and End Date: 6/20/25 to 6/20/2027
Estimated time to complete the activity: 19 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 19.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 19.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 19.50 contact hour(s) (1.950 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-188-H01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 19.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 19.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 19.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
Disclosure of Unlabeled Use:
This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings.
Disclaimer:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
Instructions for Credit
Participation in this self-study activity should be completed in approximately 19 hours and 30 minutes. To successfully complete this activity and receive CE credit, learners must follow these steps during the period from 6/20/2025 through 6/20/2027.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on DKA Prevention After T1D Diagnosis. 52% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: A 10-year-old child with newly diagnosed type 1 diabetes is being discharged from the hospital. Which of the following components is most critical to include in the initial outpatient diabetes management plan to reduce the risk of diabetic ketoacidosis (DKA) and hospital readmission?
Answer Choices:
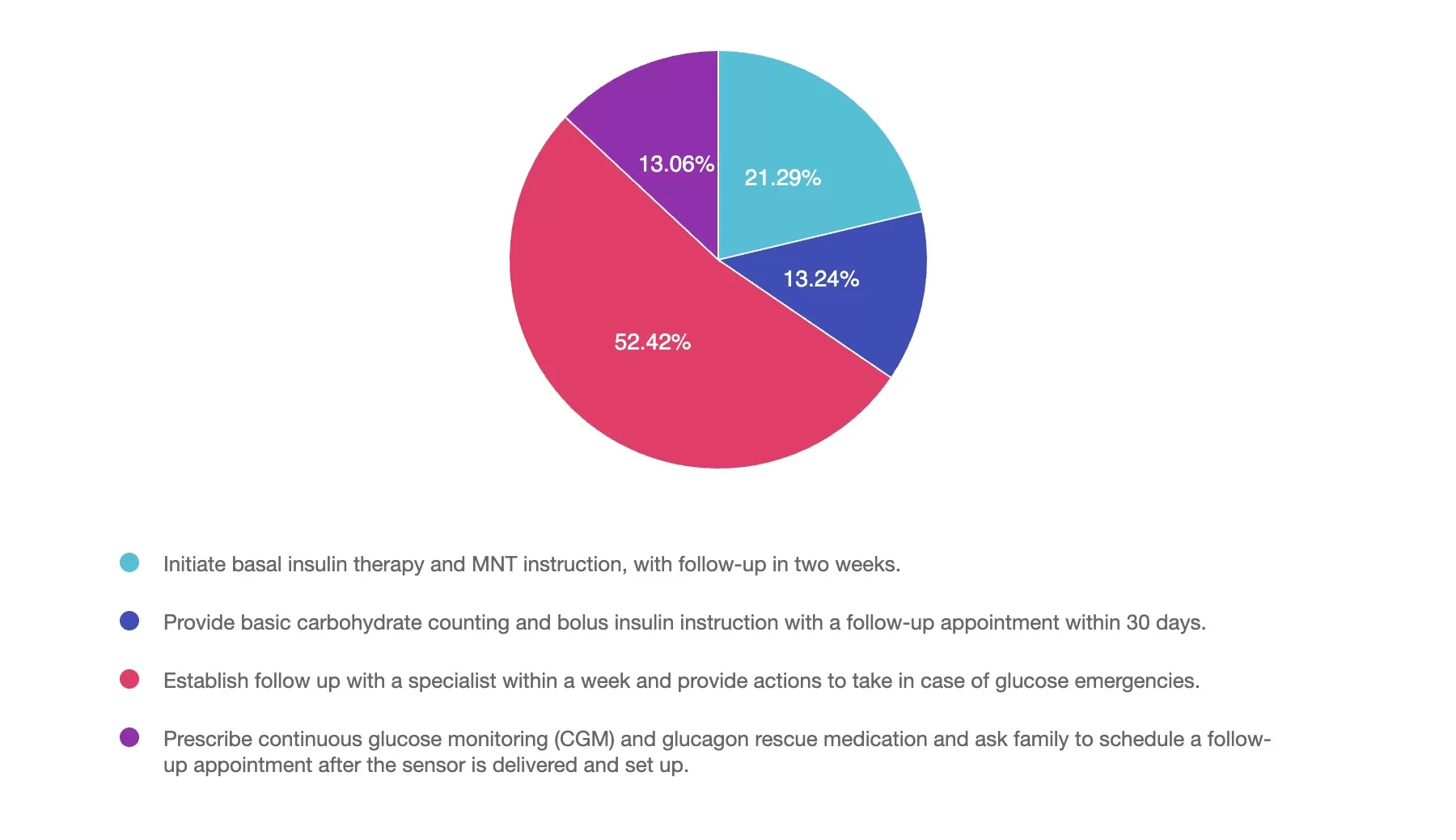
Answer 1 is incorrect. 21% chose this answer, “Initiate basal insulin therapy and MNT instruction, with follow-up in two weeks.” Basal insulin alone is insufficient; children require both basal and bolus insulin to mimic physiologic insulin needs and prevent DKA.
Answer 2 is incorrect. 13% of you chose this answer, “Provide basic carbohydrate counting and bolus insulin instruction with a follow-up appointment within 30 days.” Delayed follow-up increases the risk of complications. Carbohydrate counting and bolus insulin are important, but must be paired with timely, ongoing support.
Answer 3 is correct. About 52% of respondents chose this, “Establish follow up with a specialist within a week and provide actions to take in case of glucose emergencies.” Early involvement of a diabetes specialist and problem solving in case of glucose crises, significantly reduce the risk of DKA and readmission. Frequent follow-up in the first week is associated with better outcomes.
Finally, Answer 4 is incorrect. 13% chose this answer, “Prescribe continuous glucose monitoring (CGM) and glucagon rescue medication and ask family to schedule a follow-up appointment after the sensor is delivered and set up.” While CGM is valuable, delaying education and clinical engagement is risky; immediate education and care planning are essential.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Join us live on June 11, 2025, at 11:30 am PST to watch our brand new webinar, Mindful Eating for Successful Diabetes Management by Evgeniya Evans, MS, RDN, CDCES
This engaging and practical webinar, developed by Evgeniya Evans, MS, RDN, CDCES, a positive psychology practitioner, is tailored explicitly for healthcare professionals including dietitians, diabetes care specialists, and providers.
Using evidence-based strategies, participants will gain a deeper understanding of the benefits of incorporating mindfulness into the eating experience, including enhanced glycemic management, improved emotional well-being, and healthier eating behaviors. The webinar includes an overview of mindfulness and mindful eating strategies, such as engaging all five senses, recognizing hunger cues, addressing cravings, and using practical tools to create supportive eating environments.
Participants will also learn how to adapt these approaches to diverse populations and the unique needs of individuals. Join us to deepen your expertise, participate in insightful discussions, and empower individuals to cultivate sustainable, positive relationships with food while achieving long-term health goals.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

Abbott has recently announced that as of September 30, 2025, the Libre 2 and Libre 3 CGM systems will be discontinued and replaced with the Libre 2+ and Libre 3+ CGM systems. As a diabetes education specialist, you wear many hats, including diabetes technology expert. Education, communication, and collaboration with those living with diabetes are the keys to a smooth and successful transition into updated technology.
Over 7 million people living with diabetes worldwide use a Libre Continuous Glucose Monitoring (CGM) system (1). The American Diabetes Association (ADA) 2025 Standards of Care recommends CGM as the standard of care for glucose monitoring for those on insulin therapy. The ADA also notes that CGM can be considered for those with diabetes who do not use insulin. (2)
Since the early days of CGM technology, the Libre CGM systems have undergone several changes, and they recently announced the latest round of system improvements. They will be replaced with the Libre 2+ and Libre 3+ CGM systems.
What changes with New Libre 2+ and 3+:
What stays the same:
Individuals using these devices are advised to contact their healthcare provider to request a new prescription for the updated sensors. After September 30, 2025, any leftover 2 or 3 systems can still be used until their expiration date. The diabetes education specialist plays a crucial role in creating a plan to help navigate this technology transition.
A new, universal updated phone app was released in April 2025. This changes the need for separate Libre 2 and Libre 3 apps to a universal Libre app compatible with the Libre 2, Libre 3, Libre 2+, and Libre 3+ sensors. The universal Libre app will remove the need for separate app downloads for those switching between the currently available Libre sensors. Additional features of the updated app include an easier-to-navigate platform, and users can silence alarms for a customized timeframe of up to six hours (3,4).
FreeStyle Libre 2 and FreeStyle Libre 2 Plus Sensor users will receive real-time glucose readings sent automatically to their smartphone when used with the Libre app. The Libre 2 and 2+ users will only need to scan the sensor to backfill and recover glucose data to fill in gaps on the home screen graph during periods of signal loss.
Managing a chronic illness such as diabetes takes a team effort between those living with diabetes, the healthcare team, and family or caregivers. The LibreLinkUp app invites family members or caregivers who are helping with diabetes management to have access to glucose readings and alarms. Libre View is a cloud-based connected system between the person living with diabetes and the healthcare team. Using the Libre phone app, clients can permit healthcare providers to access their Libre CGM data to assist with creating an individualized plan of care. Abbot has also announced a collaboration with the Epic electronic medical records (EMR) system for data integration from LibreView into the EMR (1).
Libre 2+ and Libre 3+ can now integrate with selected automated insulin delivery (AID) systems. This will allow those using a Libre CGM to use an AID insulin pump as part of their glucose management plan. (5)
Here is a list of the current insulin pump compatibility:
Over-the-counter (OTC) CGM is now an option for diabetes management. It is also available for those without diabetes who want to know more about glucose fluctuations. Libre now offers two OTC options, gaining approval in the US for use in 2024.
Libre Rio is an OTC CGM FDA approved for glycemic monitoring in adults 18 years and older who are not on insulin. This device can provide insightful data for those living with diabetes or prediabetes.
Libre Lingo is an OTC CGM in the health and wellness space, which is FDA approved for monitoring glucose variations to gain insight into the metabolic response to food and activity in those 18 years and older. (6)
Helping those living with diabetes navigate the changes to the Libre systems and apps can reduce frustration and data gaps. As diabetes education specialists and technology experts, you play a key role in preparing clients for upcoming changes to their diabetes technology. Understanding the differences between the Libre devices and what features are available will help create an individualized approach to diabetes care and education. If you want more information on improving your CGM data interpretation skills, check out the latest Tech Data Toolkit webinar.
It has come to our attention that Libre 2 and Libre 2+ no longer require scanning when using the Libre app to receive glucose data. Scanning is required to backfill glucose data when there is a signal loss. Intermittent scanning is still required to obtain glucose data when using the Libre 2 or 2+ with the receiver. The article has been corrected with this updated information, and we greatly apologize for any confusion.

We are thrilled to welcome Sarah Beattie, DNP, APRN-CNP, CDCES, diabetes content expert to our team. As a Nurse Practitioner in a busy Endocrinology Clinic, Dr. Beattie is passionate about improving diabetes care. In addition, she creates engaging and educational content for healthcare providers as the owner of DNP Health Writer, LLC.
References

Gain confidence in interpreting the Glucose Profile Report (AGP) & CGM data using a
person-centered approach
As diabetes technology is becoming commonplace in our practice, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience.
Topics include:

JT, a 17-year-old recently hospitalized with a new diagnosis of type 1 diabetes, is using Multiple Daily Injections (MDI) therapy. JT uses fingerstick blood glucose monitoring but wants to move to a CGM. JT’s mother wants to know how long fingerstick monitoring must be used before a CGM can be started. According to the ADA 2025 Standards of Care, when can a CGM be initiated after a type 1 diabetes diagnosis?

Gain confidence in interpreting the Glucose Profile Report (AGP) & CGM data using a
person-centered approach
As diabetes technology is becoming commonplace in our practice, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience.
Topics include:
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

C.K. is a 55-year-old elementary school teacher diagnosed with type 1 diabetes ten years ago and is managing glycemic control with multiple daily injections (MDI) and a CGM. You are seeing C.K. for diabetes education due to an increasing hemoglobin A1c from 7.0% to 9.9%. During the appointment, C.K. reports missing mealtime doses due to being “too busy to get all that stuff out” at both work and home. C.K. notes that a friend from church has an insulin pump and asks if an insulin pump would help improve their A1c.
As the diabetes care and education specialist, what factors do you need to assess before determining if C.K. is ready for insulin pump therapy?
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Walking is often recognized as the most accessible and underrated form of exercise. While some may argue in favor of high-intensity cardio or resistance training, a growing body of evidence suggests that walking offers significant benefits—especially when approached with intention and consistency.
According to Dr. Elroy Aguiar, an assistant professor of exercise science at The University of Alabama, walking remains one of the most beneficial forms of movement due to its low barriers to entry—minimal cost, equipment, or skill required. “That’s why we say it’s the best,” Dr. Aguiar notes. And yet, despite this accessibility, many individuals struggle to find time to incorporate walking into their busy, sedentary lives.

Not all walking provides the same health return. The intensity, particularly cadence (steps per minute), plays a crucial role in determining health outcomes.
🕒 100 steps per minute is considered moderate intensity
⚡ 130 steps per minute qualifies as vigorous intensity
Dr. Aguiar’s research, published in the British Journal of Sports Medicine, indicates that health benefits from walking begin to accumulate at moderate or higher intensities. Most people naturally walk at a pace of 110–115 steps per minute when moving briskly. Increasing cadence just slightly can shift the effort from moderate to vigorous, maximizing the health payoff in a shorter time span.
For those looking to increase the challenge of walking, rucking—walking with a weighted backpack—offers a practical solution.
Adding resistance increases oxygen demand, raises heart rate, and enhances caloric burn without requiring a change in pace or duration. According to Dr. Aguiar, this method can also improve lower body strength and bone density, particularly with consistent practice over time.
While it won’t replace traditional strength training, rucking offers an accessible way to gain some muscular benefits while walking. A light weight to start, gradually increased, can help prevent injury and support adaptation.
A 2024 study published in the Scandinavian Journal of Medicine and Science in Sports found that both the quantity and intensity of physical activity are associated with better health outcomes. Remarkably, even one minute of higher-intensity activity per day was linked to a lower likelihood of having metabolic syndrome—a cluster of risk factors including visceral adiposity, high blood pressure, high blood sugar, low HDL cholesterol, and elevated triglycerides.
Dr. Aguiar explains that an individual’s most intense one-minute activity across the day can serve as a strong indicator of metabolic health. Even brief, high-intensity bursts of activity may help reduce risk for diabetes, hypertension, and cardiovascular disease.
Another practical strategy supported by research is post-meal walking. A 15-minute walk after meals can help blunt spikes in blood glucose, particularly in older adults at risk for glucose intolerance.
When muscles are active, they draw glucose from the bloodstream to use for energy, thereby reducing blood sugar levels and easing the demand on insulin. Over time, this can help prevent insulin resistance, a precursor to Type 2 diabetes.
Dr. Aguiar notes that consistent post-meal movement can reduce the workload on the pancreas and enhance the muscles’ ability to absorb and use glucose. This daily practice may offer long-term protection against metabolic syndrome, hypertension, and diabetes.
Large-scale studies have shown clear associations between step count and mortality risk. A 2023 meta-analysis published in the European Journal of Preventive Cardiology found:
Additionally, a study by the University of Granada concluded that while more steps bring more benefits, the majority of cardiovascular protection appears to occur around 7,000 steps/day. The popular goal of 10,000 steps per day, while not evidence-based, remains a useful motivational benchmark.
For elite athletes, walking may offer limited fitness returns. However, for individuals who are sedentary or new to exercise, walking provides a low-impact, effective entry point to better health.
Some key benefits of walking for the general population include:
Walking is especially valuable for individuals managing or at risk for Type 2 diabetes, obesity, hypertension, and metabolic syndrome.
Walking delivers significant, sustainable health benefits with minimal risk
Walking is a powerful yet underappreciated form of movement. Whether used to regulate blood sugar, reduce cardiovascular risk, or improve mental clarity, walking remains one of the most effective and inclusive health strategies available.
For anyone looking to improve overall health without the barriers of cost, complexity, or time—walking offers a proven path forward.
📚 References
Gain confidence in interpreting Glucose Profile Report (AGP) & CGM data using a person-centered approach! Earn 4.0 CEs
If you are preparing for certification exams or want to up your game using CGM data to improve outcomes, this course is for you.
1:30am to 2:30pm PST
Gain confidence in interpreting Glucose Profile Report (AGP) & CGM data using a person-centered approach.
As diabetes technology is becoming commonplace in our practice, figuring out how to make sense of all the data can seem overwhelming. Join Diana Issacs and Coach Beverly for a truly unique learning experience.
Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Coach Beverly will build on Dr. Isaacs’ presentation and switch the focus to the person living with diabetes. Using a case study approach, she will provide strategies to integrate the AGP with person-centered care that empowers individuals to experience increased confidence in their diabetes self-management.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments with a person-centered approach.
Topics include:
Review CGM key metrics and individualize time in-range goals
Learn how to recognize patterns with the AGP report efficiently
Utilize the AGP report as a discussion guide when meeting with a person with diabetes
Recommend lifestyle and medication adjustments based on CGM data
Strategies to recognize the expertise of the individual and collaborate on person-centered problem solving.
For last week’s practice question, we quizzed participants on Decoding AGP Report-Test Your Knowledge. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: AJ asks you why their blood glucose levels are “all over the place”. When you look at the AGP, you notice the coefficient of variation is 26%. What is the best response?
Answer Choices:
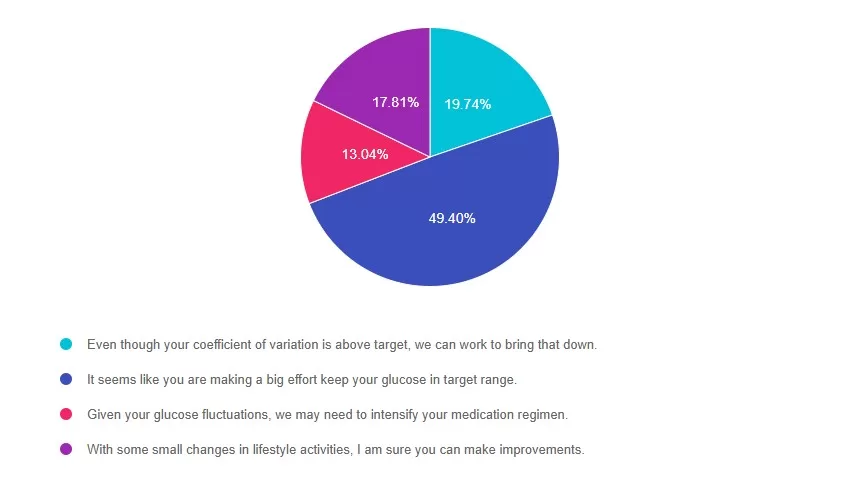
Answer 1 is incorrect. 19% chose this answer, “Even though your coefficient of variation is above target, we can work to bring that down.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Answer 2 is correct. 49% of you chose this answer, “It seems like you are making a big effort keep your glucose in target range.” YES, this is the BEST Answer. AJ has a coefficient of variation of 26%. That is 10% below the target of 36%. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Answer 3 is incorrect. About 13% of respondents chose this, “Given your glucose fluctuations, we may need to intensify your medication regimen.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
Finally, Answer 4 is incorrect. 17% chose this answer, “With some small changes in lifestyle activities, I am sure you can make improvements.” According to ADA Standards, the goal for glucose variability (or coefficient of variation) is less than 36%. AJ has a coefficient of variation of 26%, which is significantly below the target. This is a wonderful opportunity to recognize AJ’s self-management efforts.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) report to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM data for various types of people with diabetes including type 2 and people with type 1 not on pumps.
Topics include:
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

Could a Vitamin Hold the Key to Improving Insulin Sensitivity?
Beyond its well-known role in bone health, vitamin D has gained attention for its potential impact on glucose metabolism and insulin resistance. Vitamin D is a fat-soluble vitamin, but it acts more like a hormone, helping regulate calcium and phosphorus balance, modulating immune function, cell differentiation and inflammation, and influencing whole-body insulin sensitivity.
An inverse relationship has been observed between vitamin D status and markers of inflammation, insulin resistance, and glucose intolerance. An estimated 41% of the U.S. population has vitamin D insufficiency, with even higher prevalence during winter months and among women, non-Hispanic Black Americans, and older adults.1 Low vitamin D levels have been associated with an increased risk of developing type 2 diabetes2 and macrovascular and microvascular complications in individuals with type 2 diabetes. These risks spark interest in whether vitamin D supplementation could play a role in preventing and managing diabetes.
Mechanisms Linking Vitamin D and Insulin Resistance
Vitamin D receptors (VDRs) are located in pancreatic β-cells, adipose tissue, and skeletal muscle, which are all key sites in glucose metabolism. Adequate vitamin D levels support insulin secretion, enhance tissue sensitivity to insulin, reduce the expression of proinflammatory cytokines, and regulate metabolic pathways that influence insulin resistance. These physiological mechanisms explain how vitamin D status might influence the development and progression of type 2 diabetes.
Conflicting Evidence from Clinical Research
Recent studies have sought to clarify whether vitamin D supplementation can improve insulin sensitivity. A 2023 meta-analysis published in Scientific Reports analyzed 18 randomized controlled trials and 20 observational studies involving over 12,000 participants.3 It found that vitamin D supplementation was associated with significant reductions in fasting insulin, glucose levels, and HOMA-IR scores, suggesting improved insulin sensitivity. Their reviewed observational studies, however, suggested that improvements were not independent of other variables.
Overall, their findings concluded individuals with low levels may benefit from supplementation.
However, a 2020 meta-analysis of 18 randomized control trials, published in Diabetes Care,4 found no significant improvements in insulin sensitivity using gold-standard measures such as the hyperinsulinemic-euglycemic clamp, the Matsuda index, or intravenous glucose tolerance tests.
They concluded there was no evidence that Vitamin D supplementation benefited individuals with or at risk of insulin resistance.
Differences in study populations, vitamin D dosing amounts, baseline vitamin D status, and outcome measures likely account for outcome differences between the two meta-analysis reports.
Vita D Clinical Guidelines: Conflicting Recommendations
Clinical recommendations vary regarding vitamin D supplementation for diabetes prevention. The 2024 Endocrine Society Clinical Practice Guidelines (endorsed by AACE) provide updated supplementation guidance.5 But the American Diabetes Association took a different stance.
2024 Endocrine Society Clinical Practice Guidelines
For healthy adults the guidelines recommend adhering to the Institute of Medicine’s RDAs: 600 IU (15 μg) daily for ages 18-50 and 800 IU for ages 50-74. The guidelines also identify groups such as older adults (over 75), youth (under 18), pregnant individuals, and people with prediabetes who may benefit from higher intakes and supplementation. They suggested empiric Vitamin D supplementation in individuals with prediabetes to reduce the risk of progression to diabetes, but they did not name a specific recommended dose. They noted that optimal Vitamin D intake and serum 25 (OH)D concentration for disease prevention were uncertain and did not suggest routine screening.5 The guideline referenced the reviewed clinical trial dosing of 842 – 7543 IU daily. However, these recommendations are cautious and emphasize daily over high-dose intermittent supplementation. Supplementation guidelines for individuals with diabetes were not reviewed.
In contrast, the American Diabetes Association (ADA) Standards do not recommend vitamin D supplementation solely for the prevention of type 2 diabetes.6 While some studies suggest a potential link between vitamin D deficiency and an increased risk of developing diabetes, ADA states that more research is needed to confirm a causal relationship and to determine whether vitamin D supplementation can effectively delay or prevent the onset of diabetes.
Implications for Practice
For diabetes educators, these findings highlight the importance of individualized care and the need for thoughtful evaluation of vitamin D status in people with or at risk for diabetes. While vitamin D supplementation may not be universally recommended for improving insulin sensitivity or preventing diabetes, supplementation can be considered in high-risk groups to support potential health benefits. Until we have conclusive recommendations, educators can remain up to date with emerging research and tailor care strategies to an individual’s health status, risk, lifestyle, and curiosity about Vitamin D supplementation.
References:

This session provides healthcare providers with actionable strategies to integrate weight-inclusive care into diabetes management practices, focusing on improving outcomes through respect for body diversity and individual autonomy. Weight stigma is a well-documented barrier to effective care, contributing to poorer glycemic control, disordered eating, and care avoidance. By shifting from a weight-focused approach to one aligned with Health at Every Size (HAES®), providers can foster trust, enhance participant engagement, and support sustainable health behaviors.
Jessica Jones, MS, RD, CDCES, will share evidence-based insights on mitigating weight stigma and applying HAES-aligned strategies in practice. Participants will learn how to build rapport, set realistic nutrition goals, and implement interventions that prioritize blood sugar management, joyful movement, and intuitive eating. This session equips providers with tools to deliver compassionate, person-centered care, improving both clinical outcomes and the provider-participant relationship.