
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

The Virtual Conference starts next week. If you haven’t secured your spot yet, this is your final opportunity to register and join us.
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Remote Eye Screening Precautions. 84% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Retinal photography with remote reading by experts has great potential to provide screening services in areas where qualified eye care professionals are not readily available.
However, in person exams are still necessary in which of the following scenarios?
Answer Choices:
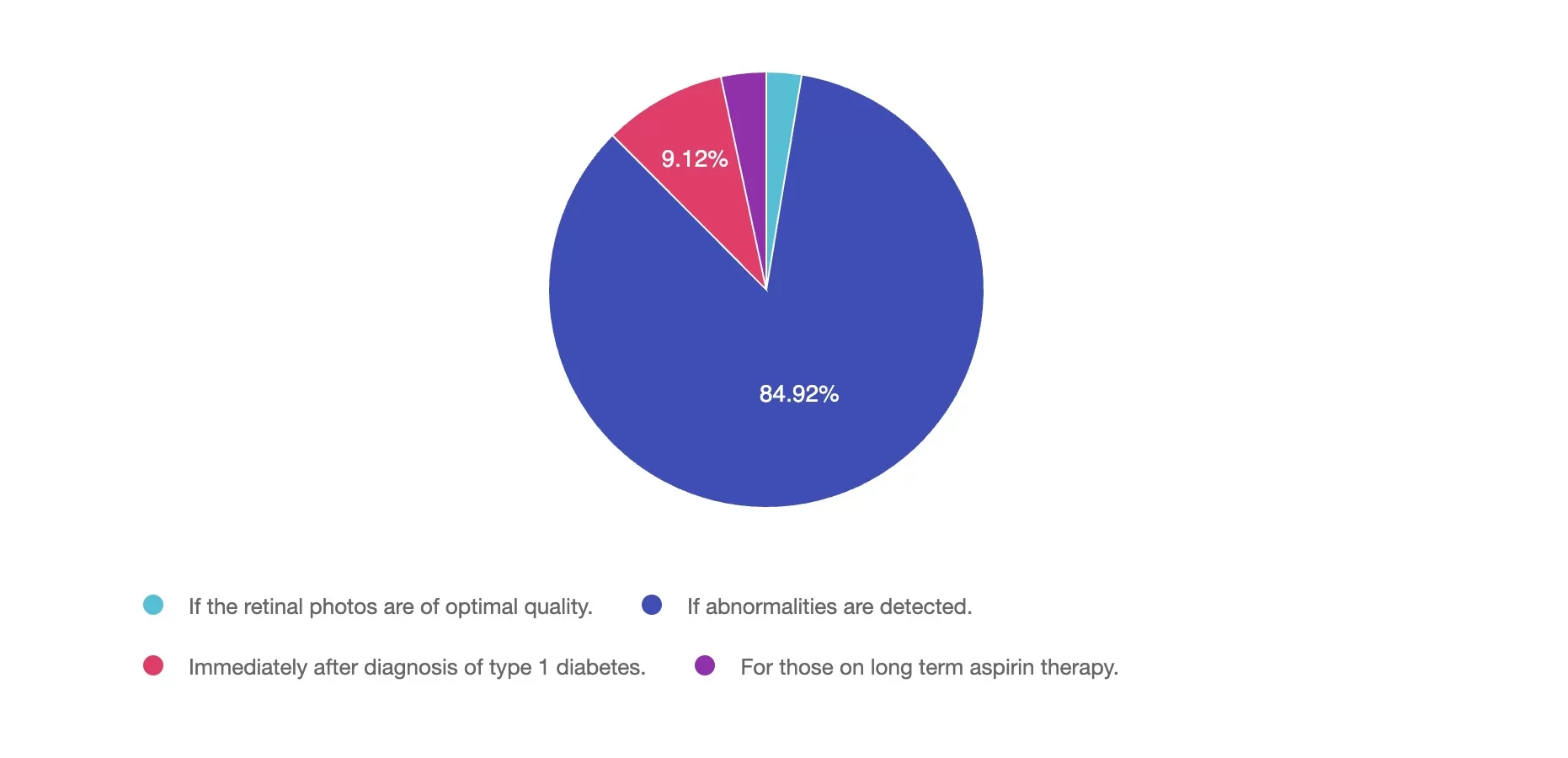
Answer 1 is incorrect. 2% chose this answer, “If the retinal photos are of optimal quality.” If retinal photos of are of high quality and there are no detected abnormalities, the retinal photo is sufficient.
Answer 2 is correct. 84% of you chose this answer, “If abnormalities are detected.” YES, GREAT JOB. If the retinal photos detect any abnormalities, an in-person comprehensive eye exam is necessary.
Answer 3 is incorrect. About 9% of respondents chose this, “Immediately after diagnosis of type 1 diabetes.” People diagnosed with type 1 diabetes are not required to get an immediate eye exam. The ADA Standards state that people with new type 1 diabetes need an eye exam within 5 years.
Finally, Answer 4 is incorrect. 3% chose this answer, “For those on long term aspirin therapy.” Since aspirin therapy does not elevate the risk of eye disease, individuals taking aspirin can safely participate in remote eye exams without concern.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
By: Beverly Thomassian

In the ever-evolving world of diabetes care, medications come in and out of favor based on new research, shifting safety data, and individual needs. Pioglitazone (Actos), once a go-to medication for improving insulin sensitivity, fell out of favor in the early 2010s due to concerns about bladder potential side effects and newer medications.
Now, pioglitazone is gaining renewed interest, especially for individuals with increased cardiovascular risk and steatosis, who may benefit from its unique profile. Even though pioglitazone only lowers A1C by 0.5 – 1.0%, this medication’s properties compel us to consider reintroducing it into the medical management of diabetes, especially in the presence of liver and heart disease. Plus, as a generic medication, its price tag of less than $5.00 a month makes it affordable for most people.
Pioglitazone is one of the thiazolidinedione (TZD) class of medications that work by enhancing insulin sensitivity, primarily through activation of PPAR-γ receptors in adipose and muscle tissue.
In a recent podcast, Banting Award Recipient, Dr. Ralph DeFronzo, provides an Insulin Resistance Master Class. He notes that pioglitazone, an insulin-sensitizing medication, improves cardiometabolic health, in part, by shifting fat distribution from visceral to subcutaneous areas. This redistribution of fat, may be associated with some weight gain. But, Dr. DeFronzo explains that this weight gain is actually a sign that the pioglitazone is working to improve insulin sensitivity. Compared to other oral agents, pioglitazone remains one of the most effective insulin sensitizers, especially useful in those with significant insulin resistance.
1. Cardiovascular Benefits – Decrease stroke and MI
The IRIS trial demonstrated that pioglitazone reduced the risk of stroke and myocardial infarction in insulin-resistant patients with a history of cerebrovascular events (Kernan et al., 2016). This benefit is being re-evaluated in the context of cardiometabolic risk, especially in people with atherosclerotic disease or metabolic syndrome.
The ADA Standard #3 states, “In people with a history of stroke and evidence of insulin resistance and prediabetes, pioglitazone may be considered to lower the risk of stroke or myocardial infarction. However, this benefit needs to be balanced with the increased risk of weight gain, edema, and fractures. Lower doses may mitigate the risk of adverse effects but may be less effective.”
2. Role in MASLD and MASH
Pioglitazone has shown promise in improving liver histology in people with metabolic-associated steatohepatitis (MASH), making it one of the few medications with such benefits (Cusi et al., 2017). Studies demonstrate it improves hepatic insulin sensitivity, reduces liver fat, and may slow fibrosis progression.
The ADA Standards of Care #4, include recommendations to start pioglitazone and GLP-1’s for individuals with diabetes and steatosis to prevent progression and slow fibrosis. “In phase 2 clinical trials, pioglitazone and some GLP-1 RAs have been shown to be potentially effective to treat steatohepatitis and to slow fibrosis progression. They may also decrease CVD, which is the number one cause of death in people with type 2 diabetes and MASLD.
3. Re-Evaluating Safety Concerns
Initial concerns about the risk of bladder cancer stemmed from observational studies; however, more recent analyses suggest that the risk is low or not statistically significant (Lewis et al., 2015). Furthermore, thoughtful prescribing—avoiding use in individuals with heart failure or active bladder cancer risk—helps mitigate potential harm. In addition, this medication is not recommended for those at risk of falls and fractures.
Comparative Benefits of Diabetes Medications
Here is a visual summary comparing the relative effects of pioglitazone versus other common medications:
Clinical Considerations
When considering pioglitazone (Actos), carefully assess:
Pioglitazone may also be especially helpful in combination with agents like metformin or GLP-1 receptor agonists, balancing out each other’s side effects and mechanisms of action.
Conclusion
Pioglitazone (Actos) may never regain its former status as a front-line diabetes treatment, but it has a clear and valuable role in today’s therapeutic landscape. For select individuals—especially those with insulin resistance, cardiovascular risk, or liver disease—pioglitazone offers an underutilized tool backed by strong evidence and decades of experience.
In diabetes care, what’s old can be new again—especially when paired with clinical wisdom and person-centered decision-making.
📚 References

This course provides the need-to-know information regarding the microvascular complications of diabetes. It includes a brief overview of pathophysiology & clinical manifestations along with prevention strategies & screening guidelines. This straightforward program will provide participants with the information they can use in a clinical setting & also provides critical content for certification exams.
A 62-year-old with type 1 diabetes presents for their follow-up visit. They report struggling with fatigue, poor sleep quality, and difficulty with glucose management despite taking medications as prescribed. Upon review, you find their A1C is 7.6%, and their average nightly sleep duration is 4.5-6 hours per night.
Based on the 2025 ADA Standards of Care, which of the following interventions would be the most appropriate next step to address sleep and glucose management?

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
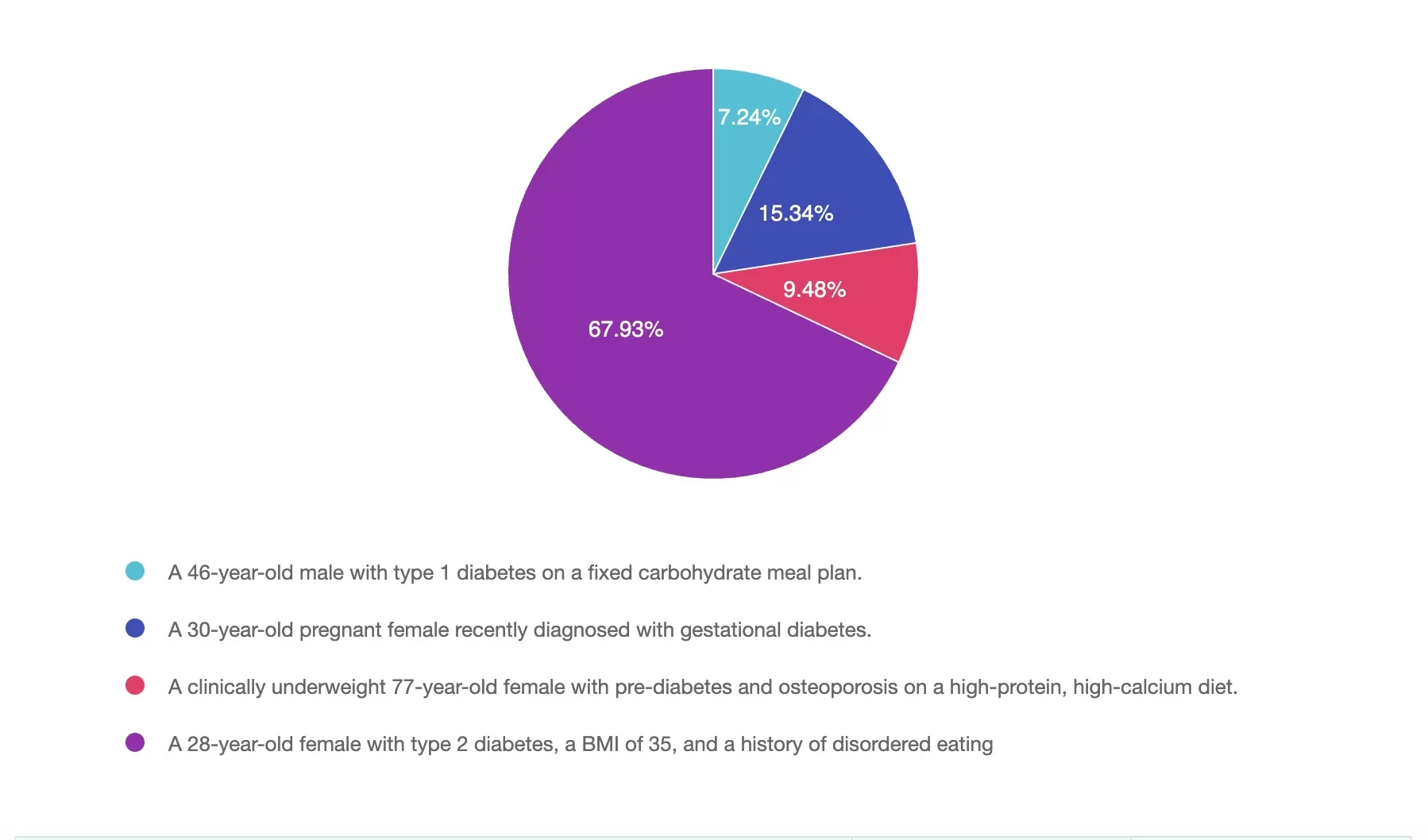
For last week’s practice question, we quizzed participants on Who Benefits Most from Mindful Eating as a Primary Strategy? 67% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Mindful eating can support diabetes management in various ways.
For which of the following individuals would mindful eating be most effective as a primary strategy rather than a complementary approach?
Answer Choices:
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Mindful eating is a flexible, non-restrictive approach that promotes awareness, self-regulation, and a healthier relationship with food. While many people with diabetes can benefit from mindful eating, individuals with a history of disordered eating often find it to be the most transformative strategy (Kristeller & Hallett, 1999; Miller et al., 2012; Mercado et al., 2021).
Answer 1 is incorrect. 7% chose this answer, “A 46-year-old male with type 1 diabetes on a fixed carbohydrate meal plan:
Answer 2 is incorrect. 15% of you chose this answer, “30-year-old pregnant female recently diagnosed with gestational diabetes:
Answer 3 is incorrect. About 9% of respondents chose this, “A clinically underweight 77-year-old female with prediabetes and osteoporosis on a high-protein, high-calcium diet:
Finally, Answer 4 is correct. 67% chose this answer, “A 28-year-old female with type 2 diabetes, BMI 35, and a history of disordered eating:
Mindful eating is most beneficial as a primary approach for individuals who have struggled with disordered eating patterns. Unlike restrictive diets, it provides a structured yet flexible way to reconnect with hunger cues, reduce emotional eating, and develop sustainable habits.
We hope this week’s rationale clarifies the diverse applications of mindful eating. Thank you for engaging with this question, and we look forward to more learning opportunities together!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
by Evgenia Evans, MS, RDN, CDCES
Aikens, J. E. (2012). Prospective associations between emotional distress and poor outcomes in type 2 diabetes. Diabetes Care, 35(12), 2472–2478. https://doi.org/10.2337/dc12-0181
Forman, E. M., Shaw, J. A., Goldstein, S. P., Butryn, M. L., Martin, L. M., Meiran, N., Crosby, R. D., & Manasse, S. M. (2016). Mindful decision making and inhibitory control training as complementary means to decrease snack consumption. Appetite, 103, 176-183. https://doi.org/10.1016/j.appet.2016.04.014
Framson, C., Kristal, A. R., Schenk, J. M., Littman, A. J., Zeliadt, S., & Benitez, D. (2009). Development and validation of the Mindful Eating Questionnaire. Journal of the American Dietetic Association, 109(8), 1439–1444. https://doi.org/10.1016/j.jada.2009.05.006
Fredrickson, B. L. (2004). The broaden-and-build theory of positive emotions. Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences, 359(1449), 1367–1377. https://doi.org/10.1098/rstb.2004.1512
Garland, E. L., Fredrickson, B. L., Kring, A. M., Johnson, D. P., Meyer, P. S., & Penn, D. L. (2010). Upward spirals of positive emotions counter downward spirals of negativity: Insights from the broaden-and-build theory and affective neuroscience on the treatment of emotion dysfunctions and deficits in psychopathology. Clinical Psychology Review, 30(7), 849–864. https://doi.org/10.1016/j.cpr.2010.03.002
Harvard T.H. Chan School of Public Health. (2024, November 7). Mindful Eating. The Nutrition Source. https://nutritionsource.hsph.harvard.edu/mindful-eating/
Kabat-Zinn, J. (2009). Full catastrophe living: Using the wisdom of your body and mind to face stress, pain, and illness. Random House Publishing Group.
Kristeller, J. L., & Hallett, C. B. (1999). An exploratory study of a meditation-based intervention for binge eating disorder. Journal of Health Psychology, 4(3), 357–363. https://doi.org/10.1177/135910539900400305
Kristeller, J. L., Wolever, R. Q., & Sheets, V. (2014). Mindfulness-based eating awareness training (MB-EAT) for binge eating: A randomized clinical trial. Mindfulness, 5(3), 282–297. https://doi.org/10.1007/s12671-012-0179-1
Mercado, C., Marasigan, K., Cardona, J., & Ko, E. (2021). Mindfulness-based interventions for emotional eating and binge eating in adults: A meta-analysis. Appetite, 164, 105265. https://pmc.ncbi.nlm.nih.gov/articles/PMC11893636/
Miller, C. K. (2017). Mindful eating with diabetes. Diabetes Spectrum, 30(2), 89–94. https://doi.org/10.2337/ds16-0040
Miller, C. K., Kristeller, J. L., Headings, A., Nagaraja, H., & Miser, W. F. (2012). Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A pilot study. Journal of the Academy of Nutrition and Dietetics, 112(11), 1835–1842. https://doi.org/10.1016/j.jand.2012.07.036
Miller, C. K., Kristeller, J. L., Headings, A., & Nagaraja, H. (2014). Comparative effectiveness of a mindful eating intervention to a diabetes self-management intervention among adults with type 2 diabetes: A randomized controlled trial. Health Education & Behavior, 41(2), 145–154. https://doi.org/10.1177/1090198113493092
Nicolucci, A., Kovacs Burns, K., Holt, R. I. G., Comaschi, M., Hermanns, N., Ishii, H., Kokoszka, A., Pouwer, F., Skovlund, S. E., Stuckey, H., Tarkun, I., Vallis, M., Wens, J., & Peyrot, M. (2013). Diabetes Attitudes, Wishes and Needs second study (DAWN2™): Cross-national benchmarking of diabetes-related psychosocial outcomes for people with diabetes. Diabetic Medicine, 30(7), 767–777. https://doi.org/10.1111/dme.12245
Nelson, J. B. (2017). Mindful eating: The art of presence while you eat. Diabetes Spectrum, 30(3), 171–174. https://doi.org/10.2337/ds17-0015
Enroll in our upcoming webinar led by Evgeniya Evans, MS, RDN, CDCES
This engaging and practical webinar, developed by Evgeniya Evans, MS, RDN, CDCES, a positive psychology practitioner, is tailored explicitly for healthcare professionals including dietitians, diabetes care specialists, and providers.
Using evidence-based strategies, participants will gain a deeper understanding of the benefits of incorporating mindfulness into the eating experience, including enhanced glycemic management, improved emotional well-being, and healthier eating behaviors. The webinar includes an overview of mindfulness and mindful eating strategies, such as engaging all five senses, recognizing hunger cues, addressing cravings, and using practical tools to create supportive eating environments.

Participants will also learn how to adapt these approaches to diverse populations and the unique needs of individuals. Join us to deepen your expertise, participate in insightful discussions, and empower individuals to cultivate sustainable, positive relationships with food while achieving long-term health goals.
Course topics:

Evgeniya Evans, MAPP, RDN, LDN, CDCES, specializes in chronic disease prevention, diabetes management, and women’s health. Her unique approach integrates mindfulness-based nutrition and positive psychology, creating transformative impacts on her patients’ health and well-being.
Evgeniya’s academic journey reflects her dedication to lifelong learning and her holistic understanding of nutrition and health. She began with four years of Sociology studies at Omsk State University in Russia, followed by earning a Bachelor of Science in Nutrition and Dietetics from the University of Illinois Chicago. She furthered her expertise with a master’s degree in Applied Positive Psychology from the University of Pennsylvania. This diverse educational foundation allows her to address the socio-psychological factors that influence dietary behaviors and deliver a well-rounded approach to patient care.
At Cook County Health’s Diabetes Clinic within the Endocrinology Department, Evgeniya provides medically tailored nutrition therapy and culturally sensitive counseling. She works with individuals from various socio-economic backgrounds, guiding them through their unique health challenges with compassion and precision. Her dedication to creating personalized, sustainable dietary strategies highlights her commitment to promoting long-term health and vitality for her patients.
In addition to her clinical practice, Evgeniya is a passionate educator. She teaches several classes at her clinic, including Pillars of Diabetes Management with Lifestyle, Nutrition for Health and Vitality, and The Art of Mindful Eating. Her emphasis on education underscores her belief in the transformative power of fostering a healthy, enjoyable lifestyle supported by mindful eating and a positive mindset.
Evgeniya envisions a world where individuals are free from the struggles of dieting and food-related shame. She dreams of a future where no one feels deprecated by their appearance or food choices, and everyone enjoys the vitality and health to pursue their dreams. She is devoted to fostering vibrant, authentic lives where cooking, eating, and sharing meals with loved ones are sources of joy, love, and positive connection.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

The use of GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists has expanded significantly in diabetes care. Their proven efficacy in lowering blood glucose levels, promoting weight loss, improving cardiovascular outcomes, and providing kidney protection has contributed to their popularity.
However, research shows that over one-third of individuals with diabetes discontinue these medications within one year.1 A 2024 JAMA study, which did not include the newest incretin tirzepatide, identified key factors contributing to this trend.
Discontinuation rates were significantly higher among individuals with increased out-of-pocket costs, those from Black or Hispanic populations, individuals with more significant social needs, and those experiencing gastrointestinal intolerances.1
Education and support, frequency of follow-up visits after therapy initiation, and proactive management of gastrointestinal symptoms are recommended to enhance therapy tolerance and increase the likelihood of continued use. Understanding effective strategies to manage gastrointestinal side effects is essential for symptom mitigation in individuals on incretin therapy.
Gastrointestinal intolerance (GI) occurs in 10-30% of individuals taking incretin medications2 and symptoms are typically transient, most noted after an increase in dose. Dose modifications and extending dose titration timing are recommended for individuals with persistent GI symptoms. In addition, the ADA 2025 Standards of Care recommends counseling on dietary modifications to mitigate GI side effects3, and a referral to a dietitian is recommended for individuals needing advanced support.4
Nausea is the most reported GI side effect. Diabetes Care and Education Specialists (CDCES) can encourage the pacing of meals, eating smaller portions, awareness of fullness, and avoiding high-fat or spicy foods. In some cases, consuming easy-to-digest, bland foods such as crackers, apples, mint, or ginger-based products and avoiding strong smells may provide relief.2
Diabetes educators can also advise individuals to stay upright after meals, including adequate hydration but avoiding rapid fluid intake (avoid the use of straws) to prevent exacerbating symptoms. If symptoms persist, coordination with a prescriber to consider anti-nausea or prokinetic agents and assessment of medication dosing may support symptom reduction.2
Vomiting and diarrhea, while less common than nausea, can impact quality of life and if severe may pose health risks. For vomiting, it is important to ensure adequate hydration, and use strategies discussed above to support nausea reduction. Emphasizing broths, liquids, and lower-fiber foods can also help until symptoms resolve. For diarrhea, it is essential to identify and avoid trigger foods and beverages such as sugar alcohols, isotonic sports drinks, coffee, alcohol, carbonation, and high-lactose foods.3 Including soluble fiber food sources can help with diarrhea symptoms. Healthcare professionals can work with prescribers to consider anti-emetic medications, a slower titration schedule, or discontinue therapy if symptoms persist.
Unlike nausea and vomiting, constipation symptoms may occur as a more chronic condition. The reduction in thirst caused by incretins may exacerbate this symptom. Strategies to support increased fluid intake, a minimum of 64 oz per day, are recommended. Dietary intervention strategies such as increasing dietary fiber intake from fruits, vegetables, and whole grains and promoting regular physical activity are key interventions.3 For individuals experiencing persistent constipation, a fiber supplement, stool softener, or laxative may be considered.
Diabetes care and education specialists, play a crucial role in supporting people using GLP-1 or GIP/GLP-1 RA medications. Referring individuals to a Registered Dietitian Nutritionist can provide personalized recommendations based on each patient’s symptoms and dietary patterns.
Working together in a team approach for lifestyle and medication management can reduce symptoms effectively. We can offer support for communities at risk of therapy discontinuation. Through education about common side effects, and providing practical strategies to manage symptoms, we can improve medication continuity and enhance long-term treatment success.

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
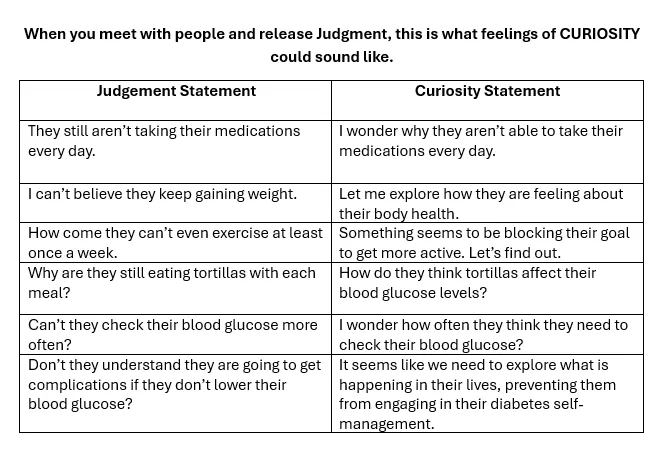
As healthcare professionals, I believe we can let go of the assumptions and judgments that so often cloud our perception of the very person we are trying to care for and lean into curiosity.
Feelings of judgment are more commonplace than you may think – almost like an unconscious thought pattern. These feelings can block the creation of a meaningful connection and leave the healthcare professional and the person in our care feeling …disconnected, misunderstood, or unseen. When judgment takes the lead, it builds a quiet wall that can prevent trust from forming and healing from taking root.
But when we become aware of these unconscious patterns and intentionally set them aside, we create space for empathy, curiosity, and genuine connection. It’s in that space that the healthcare professional and the person in our care can feel respected, valued, and heard.
You can become more aware of feelings of judgment and notice what they are saying to you. This awareness is the first step to showing up for the people in our care with deeper authenticity and compassion.
If you hear yourself thinking these thoughts or something similar, at first, simply commit to noticing it. Don’t beat yourself up for having these thoughts and feelings. As healthcare professionals, we have a whole trunk full of biases and lived experiences. It’s okay; we are actively working on releasing the shackles of judgment from ourselves and the people in our care. Now, take a deep breath and see if you can reframe this thought through the lens of curiosity.
By exchanging judgment with curiosity, you actively engage in more mindful practice and start meeting people where they are – with compassion. Curiosity does not judge; it leans in with openness, seeking to understand rather than to label. It invites connection, discovery, and the possibility of seeing things, especially people—in a new and compassionate light.
After all, we all signed up for this profession to make a positive impact in people’s lives. Meeting people with the lens of curiosity brings out the best in us, matching the reason we entered health care in the first place – to help with healing.
The goal is give yourself permission to set those feelings of judgment aside so you can show up as your best self and make the difference you want.
This approach has numerous benefits for the caregiver and the person receiving care.
When you provide nonjudgmental care infused with curiosity and compassion, you honor the strengths of the people you’re serving. You’re also infusing your consciousness with kindness in place of judgment. This approach, based on curiosity and compassion, leads to more effective care and healing that flows both ways.
We know these unconscious feelings can get in the way, yet no one talks about them. Let’s start an open and honest dialogue about these feelings. The best caregiver in the world experiences moments of judgment that can get in the way of how they show up for people. The solution is to talk about these feelings with colleagues and friends in a safe space.
We’ve developed a community to do just that. It’s a community for healthcare professionals involved in caring for people with chronic diseases. We all want the same things – which is to provide more effective care based on compassion. When you meet other people in this community, you’re going to realize that you’re not alone and that other people experience the same feelings you do. And instead of you dealing with it by yourself, there is going to be an entire community of healthcare professionals supporting each other.
– Professionals can share authentic feelings around caregiving and find connection
– Give permission to these common feelings that you and other people experience
– Know that you’re not alone in this – you don’t need to feel bad or judge yourself
– these are normal human feelings that caregivers have and it’s time that we acknowledge them


Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
By: Coach Beverly Thomassian

In April 2025, the International Diabetes Federation (IDF) officially recognized a previously underdiagnosed form of diabetes, termed Type 5 Diabetes. This condition primarily affects young, undernourished individuals in low- and middle-income countries, particularly in regions like Asia and Africa.
Estimates suggest that up to 25 million people worldwide may be affected with type 5 diabetes.
The recognition of type 5 diabetes marks a turning point in the global understanding of diabetes, expanding the framework beyond the traditionally defined types. The IDF is working to include the creation of a global research registry and the development of educational modules to train healthcare professionals in recognizing and managing this under recognized type of diabetes.
Clinically, type 5 diabetes refers to severe insulin-deficient diabetes (SIDD)— marked by elevated blood glucose levels due to defective pancreatic beta cells that fail to produce adequate insulin. Type 5 diabetes arises from long-term undernutrition, especially during key developmental periods in childhood and adolescence. This leads to impaired pancreatic development, setting it apart as a distinct clinical entity. This condition is often hereditary, with a 50% chance of transmission if a parent carries the gene.
Although this form of diabetes has been observed since the mid-20th century, it has often been misclassified and largely overlooked in global health discussions. Earlier theories attributed the condition to insulin resistance, but recent research—led in large part by the Type 5 Diabetes Working Group co-chaired by Dr. Meredith Hawkins, endocrinologist and founding director of the Global Diabetes Institute at Albert Einstein College of Medicine in New York and Dr. Nihal Thomas, professor of endocrinology at Christian Medical College (CMC) in Vellore, India. —has established its unique metabolic profile.
Individuals with Type 5 diabetes often present with symptoms similar to other forms of diabetes, such as increased thirst and urination, unexplained weight loss, fatigue, blurred vision and slow-healing wounds. Most are young and thin, so they are often misclassified as having type 1 diabetes. But based on clinical experience, treating them with insulin did not help and sometimes led to dangerously low blood glucose levels.
Type 5 diabetes is different than type 1 or type 2. That’s because it is caused by malnutrition, which leads to low insulin production due to pancreatic damage. This leaves the body unable to make enough insulin to effectively manage blood glucose. It typically appears in early teens or 20s, especially in young men in Asia and Africa with a body mass index (BMI) of 19.
Diagnosis involves a combination of blood tests to assess insulin levels and glucose metabolism, along with genetic testing to identify mutations in genes like TCF2 or HNF1B, which are associated with this form of diabetes.
People with type 5 diabetes are insulin-deficient but not insulin-resistant, meaning many can be treated with oral medications rather than insulin injections.
The emergence of this classification brings hope for more cost-effective and tailored care, and strengthens efforts to address the growing burden of diabetes.
Currently, there is no standardized treatment for Type 5 diabetes. Management strategies focus on nutritional interventions, including:
Identifying if someone has type 5 (and not type 1 or type 2), is particularly important in low-resource settings, where injectable insulin may be less accessible or affordable.
The IDF’s recognition of Type 5 diabetes aims to raise awareness and promote research into effective treatments, especially in regions where the condition is prevalent.
The formal acknowledgment of Type 5 diabetes by the IDF is a significant step toward addressing a long-neglected health issue. With millions affected, particularly in underdeveloped regions, this recognition is expected to:
As the global medical community focuses on Type 5 diabetes, there is hope for better management and improved quality of life for those affected by this condition.
For more information on Type 5 diabetes, you can refer to the IDF’s announcement: idf.org.

Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!