
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
 What Action Can I Take to Prevent Cognitive Decline?
What Action Can I Take to Prevent Cognitive Decline?During a follow-up medical nutrition therapy visit for diabetes, LC shares that they are concerned about their family history of both type 2 diabetes and dementia. They inquire about actions and interventions they can take to prevent cognitive decline.
Although LC may have inherited familial risk factors, it is well known that both type 1 and type 2 diabetes increase the risk of cognitive impairment and can double the risk for the development of Alzheimer’s disease and vascular dementia.1 The link between diabetes and cognitive impairment is multifaceted, with contributing factors including insulin resistance, chronic hyperglycemia, glucose variability with hypoglycemia, inflammation and oxidative stress, and cardiometabolic vascular risks. As diabetes care and education specialists, LC’s inquiry presents an opportunity to explore interventions that not only improve blood glucose but also support vascular and cognitive health.
A recent article published in Diabetes Care explored using neuroimaging to estimate brain age.1 The difference between estimated brain age and chronological age is known as the Brain Age Gap (BAG). The World Health Organization defines dementia as “a syndrome in which there is deterioration in cognitive function beyond what might be expected from the usual consequences of biological aging.”2
A higher BAG indicates a brain that appears older than its chronological age and is associated with an increased risk of cognitive decline and dementia. In individuals with type 2 diabetes, researchers found a significantly increased BAG of 2.29 years, while those with prediabetes showed an increase of 0.50 years.
The most significant BAG was observed in individuals with two or more cardiometabolic risk factors (3.08 years) and individuals with a baseline A1C above 8.0% (4.18 years).
The study also revealed the beneficial effects of participation in healthy lifestyle behaviors, including:
These lifestyle behaviors significantly reduced the BAG to 0.78 years. Notably, dietary factors were not assessed in this study. These findings highlight potential interventions for improving brain in individuals with diabetes, including optimizing glycemic and cardiometabolic measures, smoking cessation, alcohol moderation, and incorporating physical activity into daily routines.
Mitochondria, often described as the “powerhouse” of our cells, play a vital role in producing energy for the brain and other parts of the body. Besides energy production, mitochondria help our brain cells adapt and can protect brain cells during short-term stress. Chronic hyperglycemia and hypoglycemia can create chronic oxidative stressors, also called “allostatic overload,” that can cause mitochondrial damage and neural dysfunction.2
This damage can impair brain function, leading to long-term issues with memory, thinking, and other neurological disorders. When mitochondria are overwhelmed by chronic stress, they lose their capacity to help the brain adapt, contributing to cognitive decline. Additionally, hyperglycemia can increase beta-amyloid production, which interferes with cell signaling—a key feature of dementia. A recent 2024 article in JAMA indicated that an A1c target of 6.5-7.5 %, in individuals with type 2 diabetes managed in primary care, was associated with lower dementia incidence3. Other studies have shown the highest dementia risk in individuals with A1c > 9%.4 While A1c is a frequent measure within reported studies, glycemic variability is also a known risk factor; using time in the range may be a better future indicator, especially in individuals with increased hypoglycemia risk.
Nutrition also has a significant impact on cognitive function. For individuals with Alzheimer’s dementia and diabetes, the Mediterranean, DASH, (Dietary Approaches to Stop Hypertension), and MIND diet (Mediterranean-DASH Intervention for Neurodegenerative Delay) have promising outcomes showing reduced risk of cognitive decline.5
These diets are rich in antioxidants like flavonoids and carotenoids, omega-3 fatty acids, and plant-based foods, all linked with improved brain health. The MIND diet, has also been associated with improvements in cardiometabolic measures.6
As indicated above, cardiometabolic health has a strong association with an increased risk of dementia, and managing cardiovascular risk factors such as hypertension, dyslipidemia, smoking cessation, stress reduction, and adequate sleep can also all play a role in preserving cognitive function.
Cognitive decline and dementia can be a significant concern for individuals living with diabetes, but there are steps we can take to protect brain health.
Not all factors are modifiable, but managing contributing factors like chronic hyperglycemia, hypoglycemia severity and frequency, insulin resistance, and cardiometabolic risks can slow brain aging and narrow the brain age gap (BAG).
Article Contributor: Christine Craig, MS, RDN, CDCES is the winner of the 2023 Impact on Diabetes Award. She is a leader in the field of nutrition, technology, and diabetes care. She has served as a preceptor, lecturer, researcher, and is an active association board member. She has worked across health systems; within Diabetes Care Centers, Endocrinology clinics, Primary Care, Telemedicine Rural Health, and Virtual-First Primary Care. Currently she is owner of Nutrition for Daily Living, where it is her mission to increase access to compassionate and evidenced-based nutrition and diabetes care.

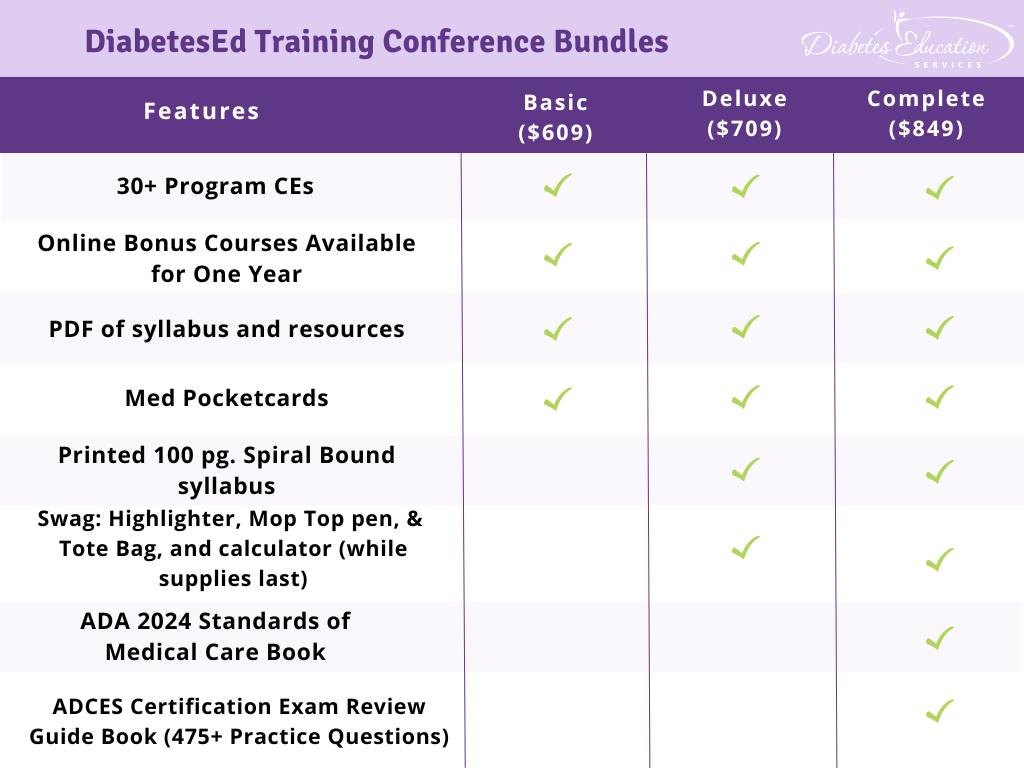
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
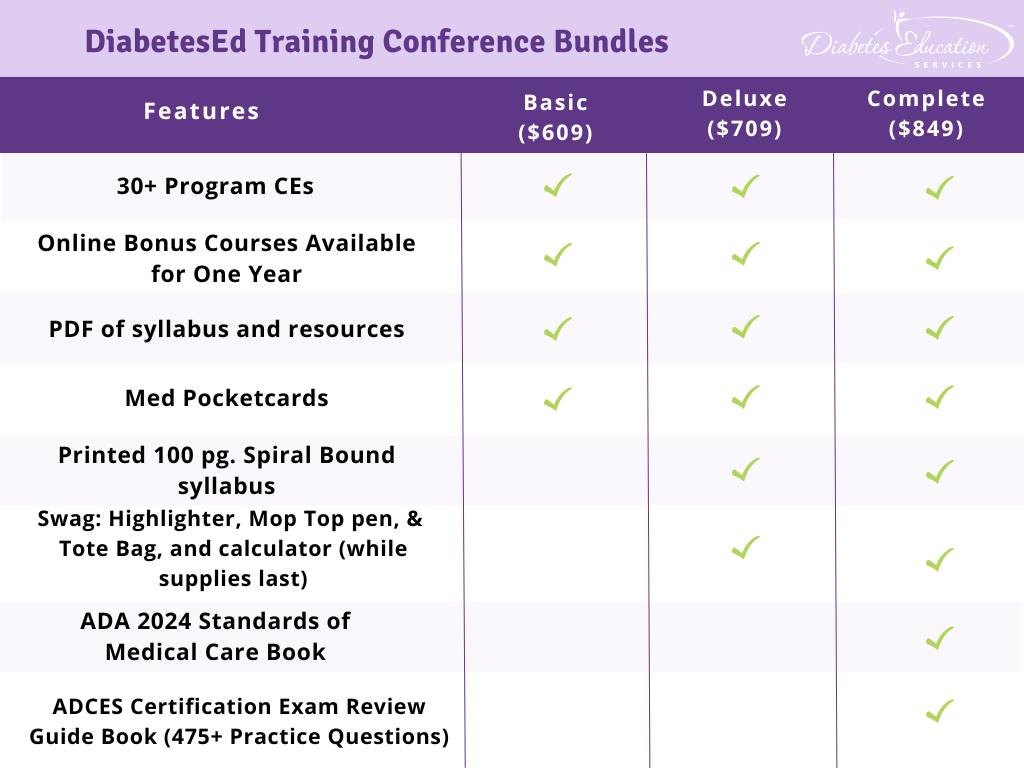
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Our team at Diabetes Education Services recognizes the powerful role art plays in healing, particularly in its capacity to improve mental wellbeing. Art offers a bridge between emotions and the mind, making it a valuable tool not just in personal wellness but also for healthcare professionals. By incorporating art into therapeutic settings, we can offer new avenues of expression and mindful connection to feelings.
To highlight and celebrate the importance of art, DiabetesEd Services will spotlight an artistic contribution in each issue of our newsletter. Art Corner is a new initiative that aims to highlight the artist in all of us and by exploring how art is a form of emotional and mental health support. We want to create opportunity for subscribers to share their stories through their artwork.
For our first submission, we are thrilled to feature Tiffany, one of our integral team members at DiabetesEd Services. Tiffany’s creativity extends far beyond her professional responsibilities. For her, creating art is not merely a hobby; it is a vital aspect of her mental health and well-being. She believes wholeheartedly in the healing power of creativity and hopes to inspire others to explore their artistic sides as well.
Tiffany specializes in oil painting with a focus on emotional depth and symbolic imagery. Her work explores themes of self-reflection and inner dialogue through vibrant colors and detailed brushwork. “There is healing taking place during the creative process that offers us a chance to unplug from our busy lives,” Tiffany states. “I know that it has made me more compassionate and engaged with the world around me.” Find out more about Tiffany’s Artwork by visiting her website www.raeanart.com.
While traditional methods are valuable in managing mental health, creative outlets such as art, provide a unique opportunity for self-expression and healing. Engaging in artistic activities—whether painting, poetry, photography, drawing, dancing, sculpting, or even journaling—has been shown to reduce stress, promote relaxation, and foster mindfulness.
Creating art allows individuals to express feelings they may struggle to articulate verbally, which is particularly beneficial for those experiencing distress. For example, a person might create a painting to symbolize the highs and lows of blood glucose levels, using color and texture to convey their emotional experience. In doing so, they have an opportunity to externalize their feelings, which can help express the internal struggles and bring them to the light of day.
There are several ways in which creating art can help improve mental wellness for people living with diabetes and health care professionals alike.
You don’t need to be an artist to benefit from creative activities. Art is for everyone, and its therapeutic benefits lie in the process, not the result. Here are some simple ways to incorporate art into your routine:
Start a Visual Journal: Combine written entries with sketches or doodles to capture your thoughts and feelings each day.
Experiment with Color: Use paints, pastels, or even markers to play with color and texture, allowing yourself to freely express how you feel at any given moment.
Art Classes and Communities: Joining a local art class or participating in an online creative community can provide not only structure but also a supportive environment where you can share your experiences and connect with others.
Create a Mood Board: Craft a collage or mood board to visually represent your goals, emotions, or anything else you’re processing in your diabetes journey.
Not only does art offer a powerful outlet for self-expression, but it also provides an opportunity to cultivate mindfulness and emotional balance. By embracing art as a tool for mental wellness, a person living with or without diabetes can find relief from the emotional challenges of their condition and improve their overall quality of life.
In each issue of our newsletter, our company will continue to celebrate the transformative power of art, showcasing an artist who reminds us just how vital creativity is to our mental and emotional well-being.
We recognize the importance of art along with science within healthcare. We would love to highlight the creative works from our community members in our monthly newsletter. If you have artwork, a photo, poem, collage, or other artforms you would like featured in our newsletter, CLICK HERE to send us a photo of your piece. Thank you for taking a risk, it is worth it!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on Triglyceride Management. [%] of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

JT is 58-years-old and has type 2 diabetes, hypertension, and BMI is 32 kg/m². Medications include metformin, lisinopril, and atorvastatin. Diet intake includes frequent highly processed foods, sugary beverages, no alcohol consumption, and minimal physical activity. Recent lab work indicates A1c: 7.2%, LDL:82 mg/dL, HDL: 38 mg/dL, triglycerides: 345 mg/dL, AST/ALT were both normal.
Given these findings, what is the recommended first-line intervention for managing his elevated triglycerides according to the 2025 ADA Standards of Care?
Answer Choices:

Answer 1 is [in/correct]. [%] chose this answer. [Answer 1]
Answer 2 is [in/correct]. [%] of you chose this answer. [Answer 2]
Answer 3 is [in/correct]. About [%] of respondents chose this. [Answer 3]
Finally, Answer 4 is [in/correct]. [%] chose this answer. [Answer 4]
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
 If you are not sure about where to start with person-centered coaching, this blog by our guest contributor, Jane Giambrone, RN, CDCES, CPCC provides some helpful insights.
If you are not sure about where to start with person-centered coaching, this blog by our guest contributor, Jane Giambrone, RN, CDCES, CPCC provides some helpful insights.
Person-centered coaching engages clients with diabetes where they are in their journey and provides a judgment-free space utilizing specific coaching skills and processes. Coaching starts with a discovery process, identification of barriers, developing strategies for overcoming them, and ultimately, working toward goal achievement.
As diabetes care and education specialists know, change takes time and focused attention, which needs to last longer than when motivation has waned. Person-centered coaching and support is invaluable in supporting this long-term change.
In my book, Take Charge of Types 2 Diabetes…Successfully Solve Your Diabetes Puzzle, I take my 30-plus years of experience working with clients as a CDECS, Life Coach, and RN, and write about a simple approach to understanding diabetes and learning how effective self-coaching to make lasting changes.
Although time with a CDECS or a coach is ideal, clients spends most of the time self-managing their diabetes outside of a health care appointment. I wrote the book because I found that knowledge, self-reflection, and self-coaching are powerful tools for empowering clients to make lasting changes. An additional benefit is more productive and insightful client follow-up visits with their healthcare professionals.
Coaching and Self-Coaching Skills
Curiosity evokes self-awareness. The client will reflect on the question, “What am I willing to do to change my life that will positively affect my health and diabetes?”
Powerful Questions using open-ended instead of yes-or-no questions. This approach provides insight and awareness into behavior. Some examples of powerful questions would be, “What is holding me back? What healthy habit do I want to start?”
Values Clarification is essential in determining what is important to the client. Knowing core life values helps a person understand what has meaning for them. Values may include family, friends, learning, humor, honesty, loyalty, productivity, etc.
How often have you noticed that people would do more for family or friends than they would for themselves?
Perspective Coaching involves examining many ways of thinking (perspectives, beliefs, frames of reference) and identifying alternative ways that are more clarifying and empowering. This is a similar skill to reframing different possibilities. For example, “I am a failure; I ate too many cookies, and my blood sugar is high now” reframed to “I realize I ate too many cookies. I am doing the best I can. Next time, I will have fewer cookies.”
SMART Goal Setting is a practical framework for creating more specific, attainable goals. The acronym SMART stands for Specific, Measurable, Attainable, Relevant, and Time-Bound goals.
Self-coaching using coaching skills is a strategy for helping clients address self-limiting behavior, which often manifests strongest when people experience barriers to change. It is an effective way for a diabetes educator to assist clients in making the most significant changes. Additionally, coaching can be added to one’s “toolkit “to help clients get the most out of their visits/time with the healthcare professional.
Jane Giambrone, RN, CDCES, CPCC, is a nurse, certified life coach, and diabetes educator for over 30 years. She specializes in type 2 diabetes and owns Diabetes Help 4U, which provides coaching, consulting, and education. She wrote, Take Charge of Type 2 Diabetes …Successfully Solve Your Diabetes Puzzle. Her book can be found on Amazon at https://www.amazon.com/dp/B0CH2BSSQW.

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

It’s been five year since you passed your exam. Now you are approaching your renewal date, so how do you maintain this hard-earned certification? To help you stay on top of this important process, we’ve gathered some essential updates from the CBDCE website.
This year, the CBDCE published new rules to renew certification which you might have missed. To make sure there are no surprises during your renewal process, here are key considerations from the CBDCE Website that we hope you find helpful!
To promote quality and inclusive diabetes care and education, the CBDCE Board changed the continuing education (CE) content requirements. Certificants will still need to complete 75 CE units over a five year period. However, to make sure CDCES’s stay abreast of the latest standards and promote inclusive care, the Board is now requiring participation in CE courses that provide updates on the ADA Standards of Care at least twice during the individual’s renewal cycle.
This means that starting in 2024, certificants will need to start acquiring these more specific CEs in preparation for 2025 renewal.
If you are renewing your CDCES in 2025 or later by completing 75 CE units over the five-year period, the CBDCE requires that you demonstrate completion of the following type of CE Activities (you can immediately start accumulating these needed CEs). The CBDCE encourages the following CE activities at least once during your renewal cycle:
*Since Diabetes Education Services is Accredited by the Commission on Dietetic Registration (CDR), all of our courses can be applied toward your CDCES Renewal.
Our content incorporates the ADA Standards and Content Requirement
The bundles listed below are well-suited for meeting CDCES renewal requirements. Additionally, we refresh our entire content library every year to stay current with the latest ADA Guidelines.
In addition, our DiabetesEd Training Programs cover the ADA Standards of Care with clarity and intention by a trio of experts, including Diana Issacs, PharmD, BC-ADM, CDCES, and FADCES a contributing author to the ADA Standards.
Plus, all of our content incorporates education principles and teaching strategies, with a special emphasis on population health, equity, diversity, and inclusion.
We are here to help you succeed. Whether you are starting your journey or working toward recertification, our ADA Standards of Care CE Course, Standards of Care Intensive, CDCES Basic Prep Bundle, and our new “Certification Renewal Bundle” or DiabetesEd Training Conferences are perfect options to meet your goals.
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.
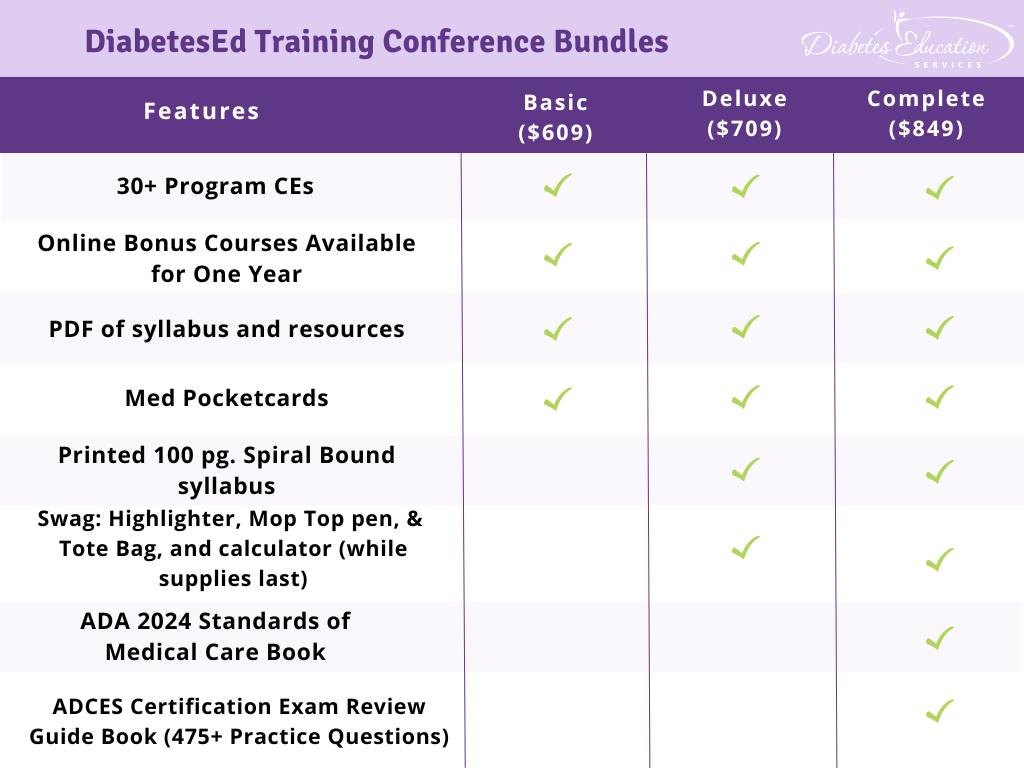
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standard of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
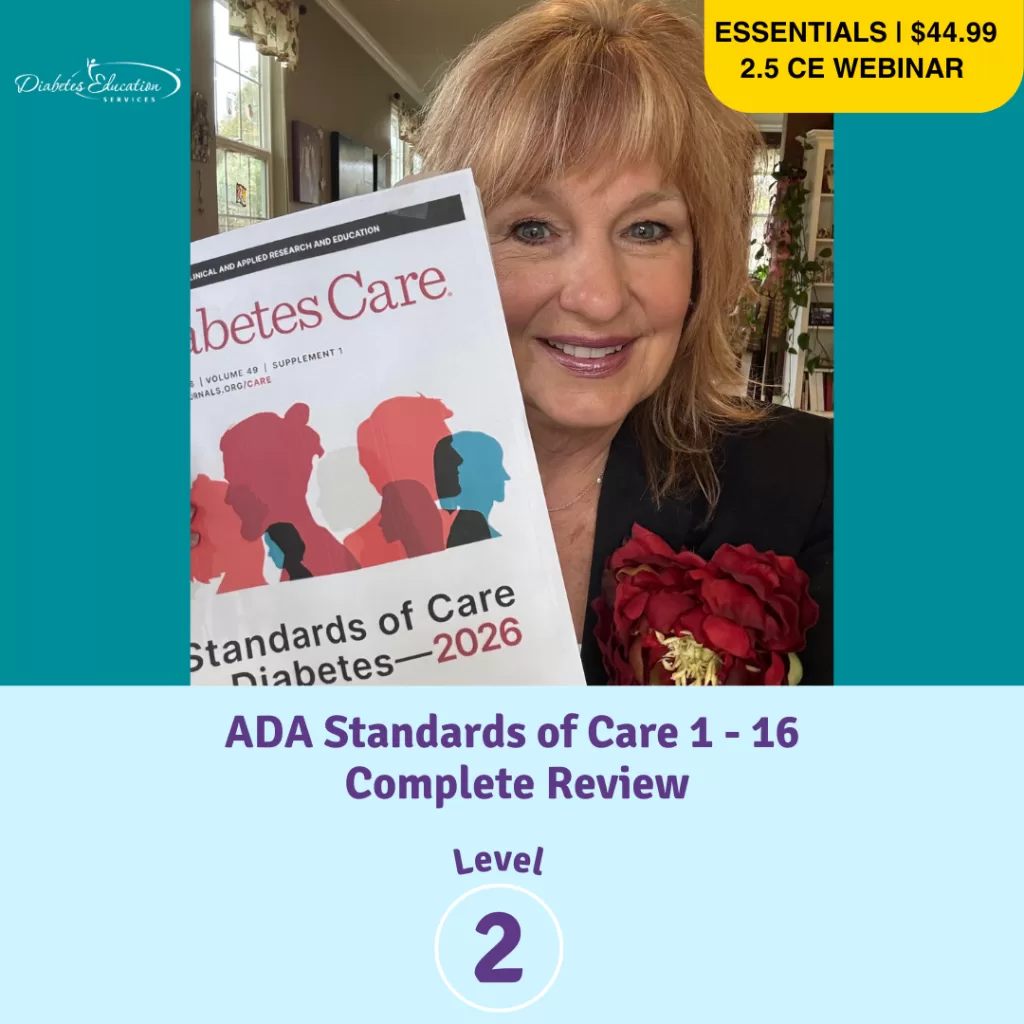
For last week’s practice question, we quizzed participants on how much basal bolus insulin at each meal. 50% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Answer Choices:
Question: KT weighs 60 Kgs and is newly diagnosed with diabetes and needs to start insulin therapy.
Based on the 50/50 rule for determining insulin dosing, which of the following is the most accurate bolus dose for each meal?
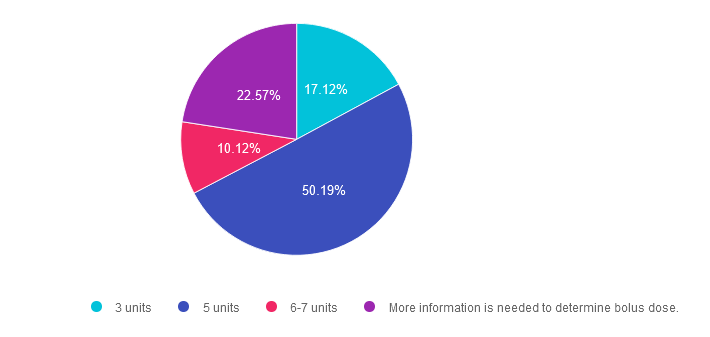
Answer 1 is incorrect. 17% chose this answer. “3 units.” The 50/50 rule for insulin is a dosing strategy based on body weight. The formula looks like this; Take body weight is kg times 0.5 to get total daily needs per day. Then give 50% as basal and 50% as bolus insulin. The last step is to divide the bolus insulin by 3 meals to get the meal time bolus dose. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal.
Answer 2 is correct. 50% of you chose this answer. “5 units.” Yes, this is the BEST answer. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal. Super easy.
Answer 3 is incorrect. About 10% of respondents chose this. “6-7 units.” The 50/50 rule for insulin is a dosing strategy based on body weight. The formula looks like this; Take body weight is kg times 0.5 to get total daily needs per day. Then give 50% as basal and 50% as bolus insulin. The last step is to divide the bolus insulin by 3 meals to get the meal time bolus dose. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal.
Finally, Answer 4 is incorrect. 22.57% chose this answer. “More information is needed to determine bolus dose.” Although this is a tempting answer, it’s not the best answer since this is a straight forward dosing calculation problem. There is no information about their social determinants of health or any barriers. Given those facts, answer B is the best answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Determining basal & bolus rates for multiple daily injections or insulin pumps can seem overwhelming. This course provides participants with a step-by-step approach to determining basal rates, bolus ratios & how to problem-solve when blood glucose levels aren’t on target. During this course, Coach Beverly provides abundant case studies to give participants hands-on practice & build confidence when calculating insulin doses for a variety of situations.
Objectives:
Learning Outcome:
Participants will have an increased knowledge of how to calculate bolus/basal insulin therapy based on person-specific factors and will be able to recommend insulin adjustments based on individual needs.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

JR returns to clinic after trying to keep a three day 7-point data log. Looking at log, the diabetes specialists notice several blood sugar readings are missing.
What is the best response?
Good job, but we will need to repeat this experiment since we are missing quite a few results.
Looks like you captured most of your blood sugar patterns.
I am sorry, but to make insulin adjustments, we are going to need more data.
I appreciate you trying. What do you think is stopping you from completing the log?

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on getting glucose to goal. 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS wears an insulin pump and uses lispro insulin. LS has an average basal rate of 0.6 units and hour, a 1:15 carb ratio and a 1:50 correction ratio. Based on the ambulatory glucose profile, LS is experiencing elevated glucose levels from 4am to 7am.
To get glucose to target, what is the best next step?
Answer Choices:
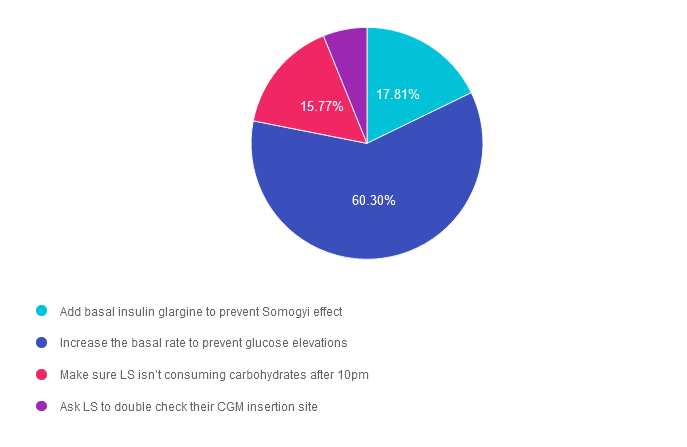
Answer 1 is incorrect. 17.81% chose this answer.” Add basal insulin glargine to prevent Somogyi effect.” If a person is using insulin pump therapy, glargine injections would not be added in addition to the pump therapy. In addition, no basal insulins (like glargine) are used in pump therapy, only bolus insulins. Lastly, Somogyi effect is defined as a hypoglycemic event that triggers a burst of counterregulatory hormones that causes a substantial increase in blood glucose. There is no evidence that the person is experiencing hypoglycemia in this scenario.
Answer 2 is correct. 60.30% of you chose this answer. “Increase the basal rate to prevent glucose elevations.” YES, this is the best answer. LS is most likely experiencing Dawn Phenomena, which if the natural rise in blood sugars starting around 3-4 am due to the early morning release of cortisol and growth hormones. By increasing the pump’s basal rate to match this insulin resistant phase, we can help LS get blood glucose closer to target.
Answer 3 is incorrect. About 15.77% of respondents chose this. “Make sure LS isn’t consuming carbohydrates after 10pm.” This juicy answer does not explain why LS’s blood glucose always rises at 4am. Also, people with diabetes have the freedom to eat carbohydrates throughout the day and evening, they would just need to provide adequate bolus insulin coverage for late night carbs.
Finally, Answer 4 is incorrect. 6.12% chose this answer. “Ask LS to double check their CGM insertion site.” Since we can see a pattern of blood glucose levels rising each day at 4am, we assume that the CGM working correctly (we can always double check using a glucose meter to confirm)
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Determining basal & bolus rates for multiple daily injections or insulin pumps can seem overwhelming. This course provides participants with a step-by-step approach to determining basal rates, bolus ratios & how to problem-solve when blood glucose levels aren’t on target. During this course, Coach Beverly provides abundant case studies to give participants hands-on practice & build confidence when calculating insulin doses for a variety of situations.
Objectives:
Learning Outcome:
Participants will have an increased knowledge of how to calculate bolus/basal insulin therapy based on person-specific factors and will be able to recommend insulin adjustments based on individual needs.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | Insulin Calculation Workshop | From Pumps & Beyond awards 1.5 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.