Question of the Week | Pregnancy & Diabetes Medication
AR is 6 weeks pregnant, what action is recommended?
AR has PCOS and type 2 diabetes and is in shock because they just discovered they are 6 weeks pregnant. AR takes metformin 1000mg BID plus empagliflozin (Jardiance) 25 mg and their most recent A1C is 8.6%.
Which of the following actions do you recommend?
- Stop empagliflozin
- Stop metformin, keep empagliflozin
- Stop metformin and empagliflozin, start insulin.
- Stop empagliflozin, start a GLP-1 inhibitor.
Click Here to Test your Knowledge
Want to learn more about this question? Enroll in our
Level 2 | Pregnancy & Diabetes
Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Intended Audience: A great course for healthcare professionals seeking to enhance their knowledge of the issues surrounding pregnancy and diabetes and appropriate care to improve outcomes.
Level 2 | Hospitals & Hyperglycemia
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to goal in the hospital setting.
Intended Audience: A great course for healthcare professionals seeking strategies to manage and improve inpatient diabetes care.
You’re invited – FREE Prep for CDCES Webinar on May 23rd
Question of the Week | AR is pregnant and Worried
AR has PCOS type 2 diabetes and worried because they just discovered they are 6 weeks pregnant. AR takes metformin 1000mg BID plus empagliflozin (Jardiance) 25 mg and their most recent A1C is 8.6%.
Which of the following is a potential complication associated with hyperglycemia during the first 10 weeks of pregnancy?
- Intrauterine hypoglycemia
- Macrosomia and post-natal jaundice
- Neonatal respiratory distress
- Diabetic embryopathy
Click Here to Test your Knowledge
Want to learn more about this question? Enroll in our
Level 2 | Pregnancy & Diabetes | 1.5 CEs

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Intended Audience: A great course for healthcare professionals seeking to enhance their knowledge of the issues surrounding pregnancy and diabetes and appropriate care to improve outcomes.
Level 2 | Hospitals & Hyperglycemia | 1.5 CEs
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to goal in the hospital setting.
Intended Audience: A great course for healthcare professionals seeking strategies to manage and improve inpatient diabetes care.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Older Adults & Tots to Teens Webinars | Airs Live May 16th & May 18th
Getting ready for certification exams and feeling overwhelmed by the Standards of Care?
Join us live this week to dissect the Older Adults & Children to Adolescents ADA Standards.
Tuesday, May 16th at 11:30 am PST
Level 2 | Older Adults & Diabetes | 1.5 CEs
We are living longer & more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering the reduction of medication & insulin therapy intensity. The older population has unique issues & special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Objectives:
- Self-management considerations for older individuals.
- Strategies to prevent complications & maintain optimal quality of life.
- The role of the Diabetes Care & Education Specialist as an advocate.
Intended Audience: An important course for healthcare professionals seeking to gain an understanding of the special issues and goals for older adults.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Thursday, May 18, 2023, at 11:30 am PST
Level 2 | From Tots to Teens | Diabetes Standards | 1.5 CEs
This course includes updated goals & guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes & their families. We discuss the clinical presentation of diabetes, goals of care, & normal growth & development through the early years through adolescence. Strategies to prevent acute & long-term complications are included with an emphasis on positive coping for families & children with diabetes.
Objectives:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes.
- State Strategies to prevent acute and chronic complications.
- Discuss the importance of positive psychosocial adjustment & resources.
Intended Audience: A great course for healthcare professionals seeking information about providing care for children with diabetes and their families.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Happy International Nurses Day – 5 Ways to say Thank You
When I was considering college, my dad offered me some simple advice, “Why don’t you become a nurse?” Four years later, I stood proudly with my white cap and nursing pin securely fastened as an RN graduate.
As I reflect on my years in this noble profession, I have witnessed the most unselfish acts of love and pure heroism by my nursing colleagues. I have highlighted some top qualities that represent my gratitude, but this thank you list could encompass an entire page.
Like the founder of nursing, Florence Nightingale, you are all “Holding the Lamp” and shining it in dark places that are often scary and unknown to provide comfort to those with the greatest need.
This week is a perfect time to let our nursing colleagues, mentors, professors, and friends know how much they are appreciated.
Coach Beverly thanks each nurse who has cared for me, held my hand, and reassured me that I am going to be okay.

5 Ways to Thank a Nurse
- Send them a handwritten note sharing how they helped you when you needed it most.
- A bundle of colorful flowers with a special note
- A basket of fruit or healthy snacks with a few sweet treats too!
- Sharing a heartfelt story on social media about how a nurse made an impact on your life.
- Letting their supervisor know how they provided you with care and comfort.
- Let a nurse mentor or teacher know how they impacted your life.
These are just a few ideas to get started. As you think of that special moment of gratitude, maybe you will come up with the perfect idea for that one special nurse.
With gratitude,
Coach Beverly
Level 2 | Older Adults & Diabetes | 1.5 CEs
We are living longer & more people are getting diabetes. The American Diabetes Association has updated the Older Adults Standards, with special attention to considering the reduction of medication & insulin therapy intensity. The older population has unique issues & special needs that require consideration as we provide diabetes self-management education. This online course highlights key areas of assessment, intervention, and advocacy for older clients living with diabetes.
Objectives:
- Self-management considerations for older individuals.
- Strategies to prevent complications & maintain optimal quality of life.
- The role of the Diabetes Care & Education Specialist as an advocate.
Intended Audience: An important course for healthcare professionals seeking to gain an understanding of the special issues and goals for older adults.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What’s Wrong with JR’s Foot?

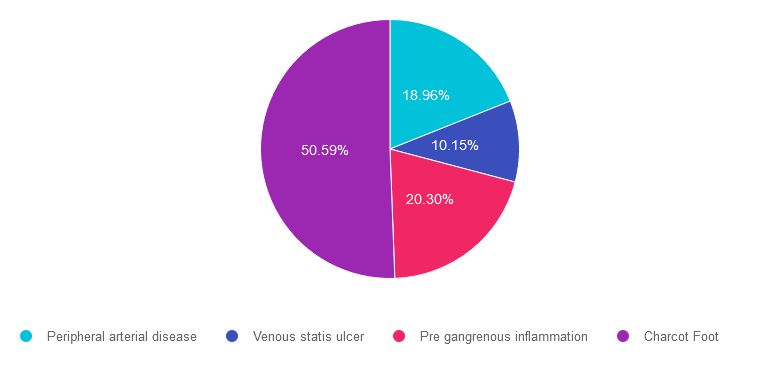
For last week’s practice question, we quizzed participants on what is wrong with JR’s foot. 51% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR arrives at the clinic wearing a walking boot due to a recent foot injury. Tells you that they “banged their foot” on some farm equipment and since then it has been warm and swollen. It hurt at first, but the pain has diminished with time.
When JR takes off the boot, you see that the left foot needs attention.
Based on this photo, what diabetes-related foot condition do you suspect?

Answer Choices:
- Peripheral arterial disease
- Venous statis ulcer
- Pre gangrenous inflammation
- Charcot Foot
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 18.96% chose this answer. Peripheral arterial disease. People experiencing peripheral arterial disease usually present with thinner, pale, lower extremities. They complain of pain in their calves or buttocks when walking due to intermittent claudication. Pulses are difficult to palpate due to diminished circulation to lower extremities.
Answer 2 is incorrect. 10.15% of you chose this answer. Venous statis ulcer. This person may have lower extremity venous disease as evidenced by the marked edema and darkened skin. However, although the foot is red and swollen there is no ulcer present in this photo.
Answer 3 is incorrect. About 20.30% of respondents chose this. Pre gangrenous inflammation. This person is certainly experiencing inflammation and edema. However, we can’t determine if their lower extremity is moving toward gangrene just from this photo.
Finally, Answer 4 is correct. 50.59% chose this answer. Charcot Foot. YES, this is the BEST answer. GREAT JOB. This person arrived with a suddenly misshapen foot, coupled with edema and redness. The skin was intact and the individual denied pain. This presentation is the hallmark of Charcot foot, a condition that is a combination of neuropathy and diminished circulation coupled with elevated blood glucose levels. It requires immediate medical attention by a foot specialist. JR sought care from a Podiatrist and his foot was secured in a cast to protect the foot and prevent further damage.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Enroll in our
Level 2 | Lower Extremity Assessment | 1.5 CEs
People with diabetes are at increased risk of Lower Extremity Complications. This course reviews the steps involved in performing a detailed assessment of the lower extremities, including how to use a monofilament and tuning fork to detect neuropathy. We also discuss the significance of the Ankle Brachial Index and strategies to prevent lower extremity complications.
Objectives:
- Describe the risk factors for lower extremity complications.
- Discuss prevention strategies.
- Demonstrate steps involved in a lower extremity assessment.
Intended Audience: This is a great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | What Meds for 14 Year Old with
KS is 14 years old and recently diagnosed with type 2 diabetes. Their A1C is 8.6%, LDL cholesterol is 137 mg/dL and their GFR is greater than 90.
Based on this clinical information and the ADA Standards for Pediatric Care, in addition to lifestyle and behavior changes, what medication(s) would be recommended?
- Dulaglutide (Trulicity) and Metformin
- Metformin and an ACE Inhibitor
- Exenatide XR (Bydureon) and a statin
- Empagliflozin (Jardiance) or Metformin
Click Here to Test your Knowledge
Want to learn more about this question? Enroll in our
Level 2 | From Tots to Teens | Diabetes Standards | 1.5 CEs
This course includes updated goals & guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes & their families. We discuss the clinical presentation of diabetes, goals of care, & normal growth & development through the early years through adolescence. Strategies to prevent acute & long-term complications are included with an emphasis on positive coping for families & children with diabetes.
Objectives:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes.
- State Strategies to prevent acute and chronic complications.
- Discuss the importance of positive psychosocial adjustment & resources.
Intended Audience: A great course for healthcare professionals seeking information about providing care for children with diabetes and their families.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Diabetes Tech Data with Dr. Diana Isaacs | Airs August 30th
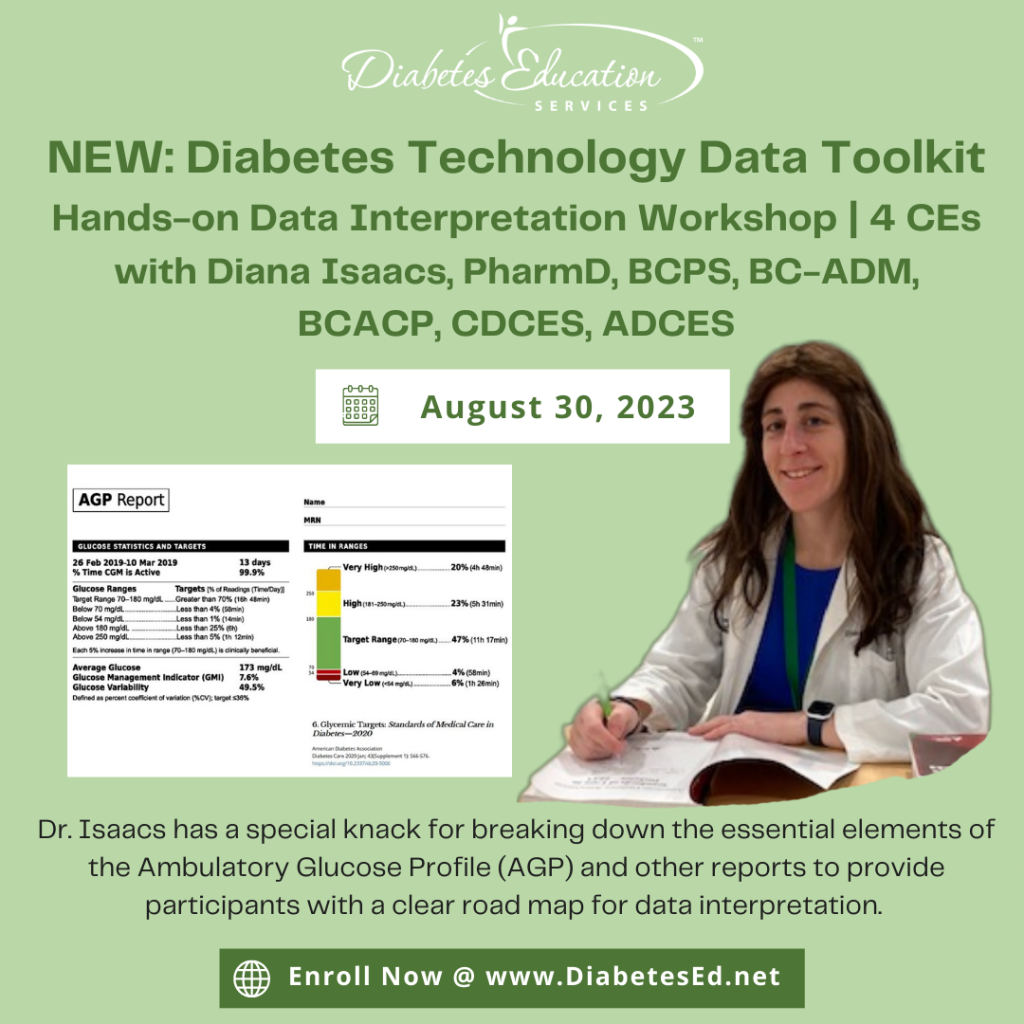
Join us live on August 30th, 2023, at 11:30 am PST for our NEW: Diabetes Technology Data Toolkit: Hands-on Data Interpretation Workshop with Dr. Diana Isaacs
As diabetes technology is becoming commonplace in our practice, figuring out how to make sense of all the data can seem overwhelming. Dr. Isaacs has a special knack for breaking down the essential elements of the Ambulatory Glucose Profile (AGP) and other reports to provide participants with a clear road map for data interpretation. She includes many sample practice cases utilizing CGM, connected pens, and insulin pumps.
By attending this interactive workshop, participants will become more confident in interpreting the AGP and continuous glucose monitor (CGM) data and determining needed medication and lifestyle adjustments.
Topics include:
- Learn how to review the ambulatory glucose profile (AGP) report systematically and efficiently.
- Understand the key metrics of CGM Data and person-centered goals.
- Utilize CGM and connected data to make medication adjustments and lifestyle/behavior recommendations.
- Apply data interpretation principles to a wide variety of cases in people with type 1 and type 2 diabetes.
Instructor: Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES, was awarded ADCES Diabetes Care and Educational Specialist of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She is the Director of Education & Training in Diabetes Technology at the Cleveland Clinic. She has numerous diabetes publications and research projects focusing on medications, CGM, and diabetes technology. You won’t want to miss this hands-on workshop with an international expert in the field.
All hours earned count toward your CDCES or BC-ADM
Accreditation Information: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.* The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Want to learn more about Diabetes Technology?
Register now for our Virtual DiabetesEd Training Conference
Available now On-Demand!

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.










