Happy Earth Day – 10 Action Steps We Took
Rationale of the Week | Get your Calculator – How many Pens?

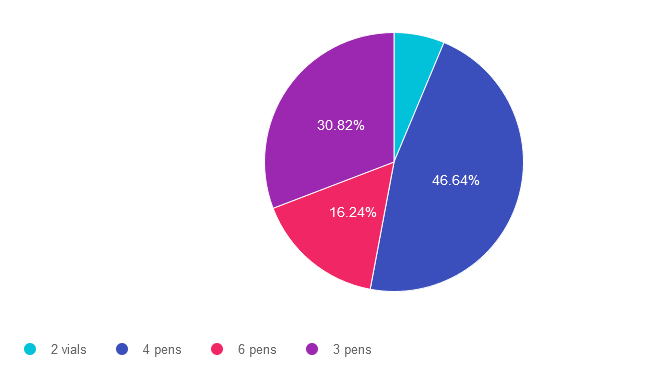
For last week’s practice question, we quizzed participants on counting every pen(ny.) 47% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: KL takes 5-10 units of insulin glulisine (Apidra) based on an insulin scale before each of their 3 daily meals and 30 units of glargine (Basaglar) at bedtime.
Based on this information, how many u-100 glulisine (Apidra) insulin pens would KL use a month?
Answer Choices:
- 2 vials
- 4 pens
- 6 pens
- 3 pens
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements, get rid of false answers, do any math very carefully and choose the BEST answer.
Answer 1 is incorrect. 6.31% chose this answer. “2 vials.” One way to quickly eliminate a wrong answer is to see if the units in the question match the units in the answer. The question asks, “How many pens” would JR need a month and this answer is in “vials”. We can cross this one off as false. **See complete math explanation below.
Answer 2 is correct. 46.64% of you chose this answer. “4 pens.” YES.. Great job. You not only calculated JR’s insulin needs, but added in extra insulin for priming too! **See complete math explanation below.
Answer 3 is incorrect. About 16.24% of respondents chose this. “6 pens.” This was a juicy answer that lured respondents into adding together the glulisine and glargine dose. The answer only asks for how many glulisine pens would JR need a month. **See complete math explanation below.
Finally, Answer 4 is incorrect. 30.82% chose this answer. “3 pens.” This was the juiciest answer of all. However, it doesn’t take into account the 2 units of insulin used to prime the pen before each injection. Also, if they had 3 pens of 300 units each, what if they made a mistake or wasted a dose, or needed a little extra.. they might be short on insulin. We always want to allow for a little cushion, just in case. **See complete math explanation below.
**Complete explanation – Doing the math.
If JR takes 5-10 units of insulin glulisine (Apidra) 3 times a day, we have to assume they will be taking the highest dose each time, so they don’t run out of insulin. That means JR uses 30 units a day of glulisine. 30 units a day x 30 days in a month = 900 units. But wait, JR needs to prime the pen first with a 2 unit “air shot” before each injection to make sure insulin is flowing through the needle before each of their 3 injections. So this means that JR is using up to 12 units of insulin 3 times a day or 36 units x 30 days = 1,080 units of glulisine a month. The next thing we need to know is that each U-100 glulisine pen holds 300 units of insulin (see our Insulin Storage Cheat Sheet 2023). Now, we can do the math. JR uses 1,080 units of insulin a day. Since each pen holds 300 units, we take 1080 and divide by 300 for a total of 3.6. This means JR will need 4 pens of glulisine each month to manage their diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question? Join our NEW
ReVive 5 Diabetes Training Program
Whether you are a novice or an expert in providing diabetes care, we invite you to attend this exciting training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management that will revolutionize your practice.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Join A Team of Experts – Save $100
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:

- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 14.0 CEs – Includes the 7-hour Session ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Speakers Interviews – Learn more about the ReVive 5 Team
What is the Biggest Takeaway when Addressing Diabetes Distress? – Dr. Susan Guzman
Do you have to be a Mental Health Expert to Tackle Diabetes Distress? – Dr. Lawrence Fisher
Why I Transformed my Approach to Diabetes Self-Management Education- Coach Beverly
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
5 Fresh Approaches to Help People Move More

For some people with diabetes, the thought of “exercise” can seem downright terrifying. We can help lift that fear by encouraging them to start with baby steps and substitute the term “activity” for “exercise”. Reassuring people that “any movement is better than no movement” allows them to shift their perspective and give themselves credit for something as simple as walking to the mailbox.
With spring in the air, it’s a perfect time to take a fresh approach to encourage activity.
The majority of people with diabetes are aware that regular activity is integral to diabetes self-care. With thoughtful coaching, we can support them to meet the target of 150 minutes of walking (or other activity) a week coupled with strength training.
Coach Beverly has outlined five strategies that she has found helpful in encouraging people to move more.
Everything off the Couch Counts
The goal is to accumulate about thirty minutes of activity a day, so taking a 10-minute walk after breakfast means they are one-third of the way there. Other activities that count include; gardening, housework, yard work, shopping, chasing kids, and those dance moves people do when no one is looking,
Keep it Practical and Fun
Starting and keeping new habits is challenging. By integrating activity into everyday life, people are likelier to keep it up. If the movement brings them joy, that is an added benefit. An excellent starting strategy is asking them what activities they like. Then explore if they can add it to their typical day. For example, taking a walk during a lunch break or hitting the gym before heading home. What about lifting weights with the kids or helping with after-dinner cleanup instead of relaxing in that favorite comfy chair? Joining an organized sport or dance class is also an option.
Activity Quips that Help Reignite the Passion
These simple sentences capture people’s attention and help them take that first step toward more movement. Please feel free to borrow and use these sayings in your practice!
- Even a ten-minute bout of activity can lower blood sugars for up to 24 hours.
- Each minute of activity lowers blood sugar by about one point.
- Walking for even 10 minutes after meals can help lower post-meal blood sugar levels.
- Even without weight loss, getting active can reduce A1C levels by 0.6%.
- Regular activity improves people’s mood, sex life, and balance.
- Keeping active helps people maintain their independence.
Prepare and PLAN for setbacks
Even the best-made plans may go differently than envisioned. Being ready for setbacks early on helps people set realistic expectations. As diabetes specialists, we can prepare people for obstacles and setbacks and remind them that a falter does not equal failure. According to Sylvia Gonsahn-Bollie, MD, assisting individuals to prepare for barriers with a PLAN helps for a quicker recovery.
PLAN stands for:
- Ponder what happened;
- Learn from it;
- Adjust the original goal;
- Now get back on track.
Encourage people to avoid black-and-white thinking, like, “Well, I missed my planned workout, so I might as well just give up.” Getting back on track as soon as possible keeps the momentum and prevents muscle deconditioning.
Exercise is medicine.
Regular physical activity can help prevent disease and improve well-being. Although exercise statistics are disheartening, improvement is possible. As health advocates, we can encourage systemic changes in health care and environmental changes in our neighborhoods to increase activity on a population level.
While waiting for more extensive changes, we have the power to equip individuals with personalized, actionable tools for improving and maintaining physical activity.
Our belief in people’s ability to get active is contagious. A person-centered collaborative approach can help people get moving, one step at a time.
Join our NEW
ReVive 5 Diabetes Training Program
Whether you are a novice or an expert in providing diabetes care, we invite you to attend this exciting training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management that will revolutionize your practice.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Join A Team of Experts – Save $100
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:

- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 14.0 CEs – Includes the 7-hour Session ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Speakers Interviews – Learn more about the ReVive 5 Team
What is the Biggest Takeaway when Addressing Diabetes Distress? – Dr. Susan Guzman
Do you have to be a Mental Health Expert to Tackle Diabetes Distress? – Dr. Lawrence Fisher
Why I Transformed my Approach to Diabetes Self-Management Education- Coach Beverly
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | JR is Skipping Provider Appointments
JR has type 1 diabetes and tells you, “My doctor just doesn’t seem to understand how to manage type 1 diabetes. Sometimes, I just skip my appointments because it feels like a waste of time.” JR’s most recent A1C was 8.7% and their time in ranges keeps decreasing with each visit.
Based on this, you realize that JR’s provider-related diabetes distress
- has intensified to clinical depression.
- requires urgent referral to a mental health professional.
- could be responsive to self-management coaching.
- may be a sign of disordered eating.
Click Here to Test your Knowledge
Rationale of the Week | Is JR at Risk for NASH?

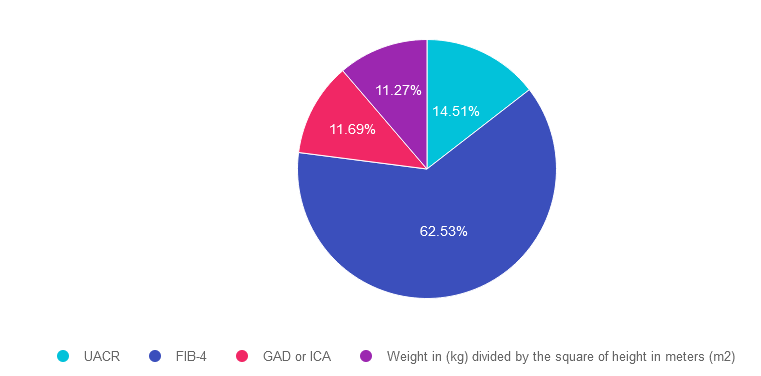
For last week’s practice question, we quizzed participants on being at risk for NASH. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 46 years old with type 2 diabetes and a BMI of 33. In addition, JR has hypertension and hyperlipidemia, with elevated liver enzymes (ALT and AST).
According to the latest ADA Standards, which of the following would best help determine if JR is at risk for liver fibrosis and cirrhosis?
Answer Choices:
- UACR
- FIB-4
- GAD or ICA
- Weight in (kg) divided by the square of height in meters (m2)
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 14.51% chose this answer. “UACR.” This is a juicy answer, however the Urinary Albumin Creatinine Ratio (UACR) evaluates kidney function and doesn’t provide any hepatic insights. Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
Answer 2 is correct. 62.53% of you chose this answer. “FIB-4.” GREAT JOB. The Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation. By entering the person’s age, AST, ALT and Platelet count using the FIB-4 calculator, a risk level is calculated (see slide below). The hope is that by screening for hepatic issues early, we can take action to protect the liver and improve outcomes.
Answer 3 is incorrect. About 11.69% of respondents chose this. “GAD or ICA.” Although this answer is familiar, it does not match the intent of the question. GAD and ICA are blood tests to determine if someone has autoimmune mediated type 1 diabetes. Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
Finally, Answer 4 is incorrect. 11.27% chose this answer. “Weight in (kg) divided by the square of height in meters (m2).” This answer is also familiar since it is the formula to determine a person’s body mass index (BMI). Instead we would recommend the Fibrosis-4 Index for Liver Fibrosis helps determine risk of hepatic cirrhosis and inflammation (see answer 2).
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity! Learn more by attending our Virtual Conference plus save $100 through April 18, 2023.
Register now for our Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
April eNews | Spring into Action | Save $100 on Diabetes Training
Question of the Week | Get your Calculator – How many Pens?
KL takes 5-10 units of insulin glulisine (Apidra) based on an insulin scale before each of their 3 daily meals and 30 units of glargine (Basaglar) at bedtime.
Based on this information, how many u-100 glulisine (Apidra) insulin pens would KL use a month?
- 2 vials
- 4 pens
- 6 pens
- 3 pens
Click Here to Test your Knowledge
Register now for our Virtual DiabetesEd Training Conference

Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Upcoming Webinars – Microvascular Complications, Prevention & Treatment on April 11th & Cardiovascular Disease on April 13th
You’re invited! Join us on April 11th & April 13th for our upcoming Standards of Care Intensive Updates!
Our Microvascular Complications, Prevention & Treatment | Eye, Kidney, Nerve Disease | Level 2 Webinar airs live on April 11th at 11:30 am PST
This course provides the need-to-know information regarding the microvascular complications of diabetes. It includes a brief overview of the pathophysiology & clinical manifestations along with prevention strategies & screening guidelines. This straightforward program will provide participants with the information they can use in a clinical setting & also provides critical content for certification exams.
Objectives:
- List the main factors contributing to eye, kidney, & nerve disease.
- Describe modifiable & non-modifiable risk factors for diabetes complications.
- State screening guidelines & prevention strategies.
Our Cardiovascular Disease & Diabetes | Level 2 Webinar airs live on April 13th at 11:30 am PST
This course takes a close look at insulin resistance syndrome & vascular complications. We discuss the impact of vessel disease from the heart to the toes. Included is a discussion of identifying & preventing vascular disease & a comprehensive review of the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes for heart disease.
Objectives:
- The impact of insulin resistance & hyperglycemia on vessel disease.
- State the complications & factors associated with vascular disease.
- List management goals to reduce the risk of vascular disease.
- Discuss strategies to promote health.
Virtual DiabetesEd Training Conference
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Group discounts are available!*
Download Course Flyer | Download Schedule
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.











