Question of Week | What explains JR’s sudden DKA?

JR, a 67-year-old with type 2 diabetes for seven years and an A1C of 9.7% was started on empagliflozin 10mg two weeks ago. Other labs include a GFR of 49 and a UACR of 34 mg/g. Other diabetes medications include glucotrol 10mg twice daily and sitagliptin 100mg daily. JR sometimes has a few shot’s of whiskey before bed, especially if they had a stressful day. JR’s partner calls you in a panic and says JR is admitted to the hospital in DKA.
What is the most likely explanation?
- Excess alcohol intake leading to starvation ketosis
- Potential side effect of SGLT-2 Inhibitors
- Low GFR and elevated UACR increase hyperglycemic risk
- JR is misdiagnosed and likely has type 1 diabetes
Click Here to Test your Knowledge
Want to learn more about Diabetes Medications and Side Effects? Dr. Diana Isaacs will be sorting fact from fiction in our
Virtual DiabetesEd Training Conference | 30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Training Conference and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Uvalde T-Shirt Installation Connects Art to Heart

After the Uvalde shooting, a group of mothers who belonged to a monthly book club, decided not to talk about their book of the month. Instead they dedicated their gathering to sharing their deep grief and feelings of powerlessness about the senseless loss of 19 beautiful children in Uvalde, Texas. Children, just like their own, who were excited to learn, hang out with friends and wrap up school for the summer.
I am one of the book club mothers.
We committed to shine a light on this tragedy and connect to our common humanity through art. We are often afraid to talk about gun violence because it is such a fraught conversation. However, we know one thing we all have in common regardless of our political affiliation or upbringing.
We all want our school aged children to be safe and free of death from gun violence in their schools, homes and communities.
Let’s start our conversation with this belief in mind.
To express our grief and touch the hearts of others, we created an art installation featuring 21 orange t-shirts of different sizes, with the hand-painted names of the children and teachers who died that day in May. We call it the “Uvalde T-shirt Clothesline”.
The Uvalde T-Shirt Clothesline speaks of the empty shirts left behind: shirts that will never be played in, worn to school, or hugged at night.
We displayed this at our local Farmer’s Market where many people stopped, looked up and reflected on the loss. It now it hangs at the entrance of the museum of northern california, monca.



Uvalde T-Shirt Clothesline Story
On May 24, 2022, in the small town of Uvalde, Texas, nineteen innocent children and two teachers were gunned down at school by an 18-year-old with an automatic weapon. Out of our grief and dismay over this tragic loss of life arose this installation of 21 orange t-shirts, hand-painted with the names of the children and teachers who died that day.
The Uvalde T-Shirt Clothesline speaks of the empty shirts left behind: shirts that will never be played in, worn to school, or hugged at night. Shirts whose young owners will never reach their full potential. We chose orange shirts since orange is the commemorative color of gun violence prevention.
Empty orange shirts on a clothesline serves as a metaphor for the ordinary act of hanging our family’s clothes to dry, a commonplace fixture of household routine. It connects to the tragic reminder that gun violence in our schools is also becoming routine.
Firearms are the leading cause of death for children in the United States. Every two and a half-hours, a child loses their life due to firearm violence, accidents, or suicide. We hope this display touches hearts and shines a light on the senseless loss of these beautiful souls. Through connection and conversation, we can make a difference.
Please share any questions or comments regarding this blog with [email protected]. Thank you.
T-Shirt Clothesline Tribute makes local paper front page.
Maybe other communities could create their own clothesline? Read Enterprise Record Article here.
Resources
Download a List of Gun Violence Prevention Organizations
Nurses Union Addresses Gun Violence
Art Displays
Uvalde mural honors Robb Elementary School shooting
September 2022 eNews | Boosting Nutrition Health & Jumping for Joy
September 2022 eNews | Boosting Nutrition Health & Jumping for Joy

September Greetings
We are experiencing a food crisis. Ten percent of Americans in every state, across rural and urban households, experienced food insecurity at least some time during 2020. With food prices on the rise, how do we help people with prediabetes and diabetes make healthy food choices within their means? There is good news! A national nutrition task force has unveiled its findings and ambitious strategies to improve nutrition access and reduce diet-related diseases. These thought leaders and food experts have outlined an innovative plan to address the food crisis by increasing nutrition education and access, including funding cooking classes and more.
Good news in diabetes tech. The first ever tubeless integrated insulin delivery system was just FDA approved for toddlers 2 years old and up. Parents and providers alike are celebrating this latest advance in insulin delivery technology for kids and adults alike.
We all know that exercise is good for you, but does it elicit feelings of joy? A researcher has identified a series of one-minute movements that not only improve coordination, balance, and strength but also bring a smile to your face. Give it a try and invite your friends and family to join you in Jumping for Joy.
In preparation for our 25th year anniversary, we are adopting a higher tech Online University Learning Platform. This means easier navigation and more bells and whistles for our subscribers. We plan to make the switch in early Fall, so keep your eyes open for more info as we get closer to the date.
Finally, we are thrilled to announce two Flower Scholars for our October Virtual DiabetesEd Course. They are making a big difference in their communities, and we are overjoyed to celebrate both of them.
You and your colleagues are invited to join our three FREE Webinars this month. If you feel like a challenge, take a moment to check out our Question and Rationale of the Week.
Thank you in advance for your actions and advocacy on behalf of people living with diabetes.
Beverly, Bryanna, Robert, and Amanda
Click here to read our full September 2022 newsletter.
Featured Articles
- Task Force aims to Help Americans Eat Healthier
- New Tubeless Insulin Delivery for Toddlers
- Can Movement Increase Feelings of Joy?
- DiabetesEd University Launches New Platform
- Question of the Week
- Rationale of Week
- Flower Scholarship Recipients
Upcoming Webinars
- Virtual DiabetesEd Specialist Conference | Oct. 12-14th
- What We Say | Sept 13th
- BC-ADM Prep | Sept 20th
- CDCES Exam Prep | Sept 22
- ADCES Book Bundle
- Free Resources
Upcoming FREE Webinar
What We Say Matters: Language that Respects the Individual and Imparts Hope| Airs September 13th
What we say matters.

As educators, advocates, spouses, friends, and providers, our use of language can deeply affect the self-view of people living with diabetes every day.
Intentional communication is a powerful tool that can uncover trauma, identify barriers, and move both the provider and person with diabetes toward a greater understanding of the issues involved.
The language used in the health care setting is immensely important in determining trust, mutual respect, and meaningful long-term relationships.
Many people with diabetes have experienced injustice, trauma, and marginalization, and are often struggling with feelings of shame and blame.
- Let’s lift people through our commitment to careful listening.
- Let’s choose a language that is person-centered and free from judgment.
- Let’s empower our interactions by identifying and addressing trauma and the impact of social determinants.
FREE Webinar – Lifting People Up
Topics covered include:
- Learn phrases, words, and approaches that can be left behind.
- Describe diabetes language that is respectful, inclusive, person-centered, and imparts hope.
- Discuss how to evaluate for ACE and provide trauma-informed care
- Practice communicating about diabetes using phrases free from judgment with a focus on a strength-based approach.
This mini-webinar is free, and no CEs are provided, but there is lots of great info!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Abdominal lumps and insulin injections

For last week’s practice question, we quizzed test takers on abdominal lumps and insulin injections. Only 46% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
JL is 67 years old, with a BMI of 23 and A1C of 7.6% and injects insulin 4 times a day to manage their type 1 diabetes. On visual inspection, you notice that there are many areas of lipohypertrophy on JL’s abdominal region.
Which of the following interventions would be the best recommendation?
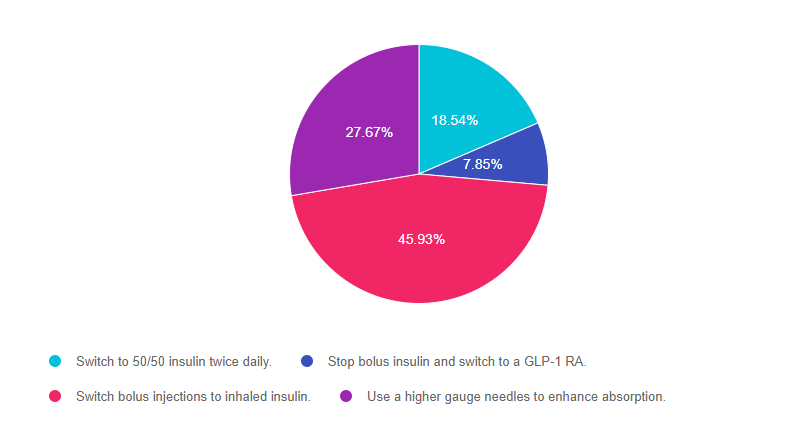
Answer Choices:
- Switch to 50/50 insulin twice daily.
- Stop bolus insulin and switch to a GLP-1 RA.
- Switch bolus injections to inhaled insulin.
- Use a higher gauge needles to enhance absorption.
Getting to the Best Answer
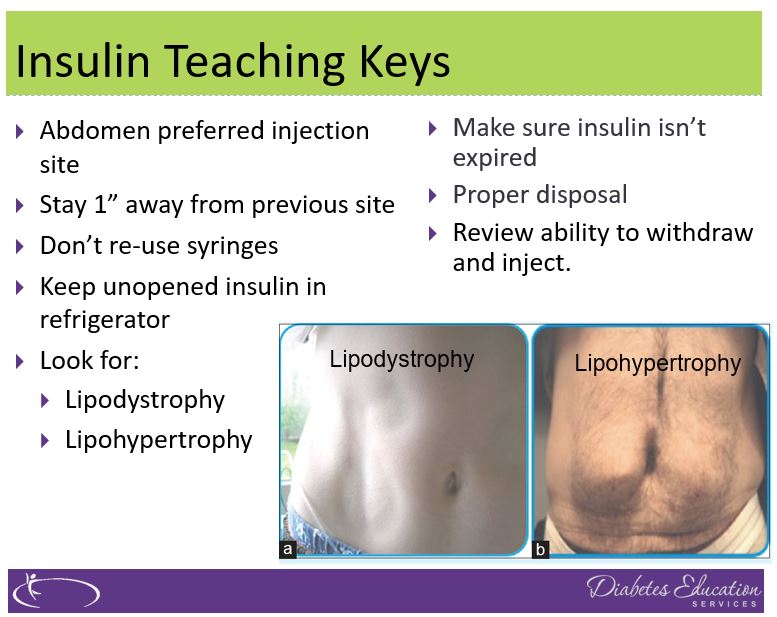
Answer 1 is incorrect. 18.54% chose this answer, “Switch to 50/50 insulin twice daily.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to 50/50 insulin may even lead to worsening blood sugars since it is a premixed basal bolus insulin that would be difficult to fine tune for people with type 1 diabetes. (See photo of lipohypertrophy below)
Answer 2 is incorrect. 7.85% of you chose this answer, “Stop bolus insulin and switch to a GLP-1 RA.” This is not the best answer since GLP-1 RA’s are not FDA approved to treat people with type 1 diabetes*. If a person with type 1 diabetes stopped their bolus insulin, they would become very insulin deprived and likely experience severe blood glucose elevations and hyperglycemic crisis. Plus, this answer doesn’t address the core issue of injection site overuse and fat accumulation. *Footnote: some people with type 1 are prescribed a GLP-1 RA (off label) in ADDITION to basal bolus insulin to lower glucose levels and help with weight management. (See photo of lipohypertrophy below)
Answer 3 is correct. 45.93% of respondents chose this answer, “Switch bolus injections to inhaled insulin.” YES, GREAT JOB. Lipohypertrophy, a lump of fat accumulation due to frequent injections, has been shown to affect ?50% of people injecting insulin and results from lack of injection site rotation and needle. Injecting into these “lumps” reduces insulin absorption and action, raises postprandial glucose, and greatly increases insulin uptake variability. Despite this, inspection of injection sites is not routinely performed by health care professionals or people with diabetes, which reveals the “unexplained” nature of many blood glucose fluctuations. (Excerpted from this Article on Insulin Injection Technique- Clinical Diabetes, 2019).
To avoid lipohypertrophy, we can transition people to boluses of inhaled insulin to cover for food and hyperglycemia and still provide one basal injection a day, using sites free of fatty lumps. This reduction of the injection frequency allows time for tissue healing and reduces creation of new lipohypertrophy sites. Download our FREE Insulin PocketCards here.
If a person decides to stay on injections, encourage them to systematically space them at least 1 cm (about the width of an adult finger) from each other; this helps to avoid repeat tissue trauma. One approach involves dividing sites into quadrants (or halves when using the buttocks or thighs), using one quadrant per week and moving from quadrant to quadrant in a consistent direction (e.g., clockwise). Encourage people to rotate injections between sites, as well as within a site. Use needles once and toss, since excessive reuse of needles can traumatize the skin and underlying structures. (See photo of lipohypertrophy below)
Finally, Answer 4 is incorrect. 27.67% chose this answer, “Use a higher gauge needles to enhance absorption.” This is not the best answer since it doesn’t address the core issue of injection site overuse and fat accumulation. Switching to a higher gauge needle just means the barrel of the needle is thinner and hurts less when passing through the skin. Improper injection site rotation and needle reuse are the most common factors associated with lipohypertrophy. (See photo of lipohypertrophy below)
Read more great info here, The Injection Technique Factor: What You Don’t Know or Teach Can Make a Difference – Article from Clinical Diabetes, 2019. You are also invited to join our Virtual Conference where we tackle this topic and many more factors that affect diabetes self-care.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Ambulatory Glucose Profile Confusion

LS is 72 years old with type 2 diabetes and injects insulin 4 times a day. They were started on a CGM device last month and you are looking at the Ambulatory Glucose Profile (AGP) together. You notice their time in range is 60%, their time above range is 38%, in low range is 2% and their coefficient of variation is less than 36%.
What is the best response?
- We still need to improve your coefficient of variation.
- Based on these results, let’s decrease your insulin by 20%.
- Time in range should be 70% or greater for your age group.
- This information is going to help with problem solving.
Click Here to Test your Knowledge
Want to learn more about this question?
Join our Virtual Conference to gain valuable insights from
Technology Expert, Dr. Diana Isaacs
and/or
Join our FREE live Webinar on September 13th, from 11:30 am to 12:15 pm
What We Say Matters: Language that Respects the Individual and Imparts Hope

Many people with diabetes have experienced injustice, trauma, and marginalization, and are often struggling with feelings of shame and blame.
Topics covered include:
- Learn phrases, words, and approaches that can be left behind.
- Describe diabetes language that is respectful, inclusive, person-centered, and imparts hope.
- Discuss how to evaluate for ACE and provide trauma-informed care
- Practice communicating about diabetes using phrases free from judgment with a focus on a strength-based approach.
Intended Audience: A great course for healthcare professionals who want to learn the steps involved in providing a thorough lower extremity assessment.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
All hours earned count toward your CDCES Accreditation Information
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Belly Dance “Fun”damentals
Belly Dance “Fun”damentals – Women of all ages and body shapes invited!
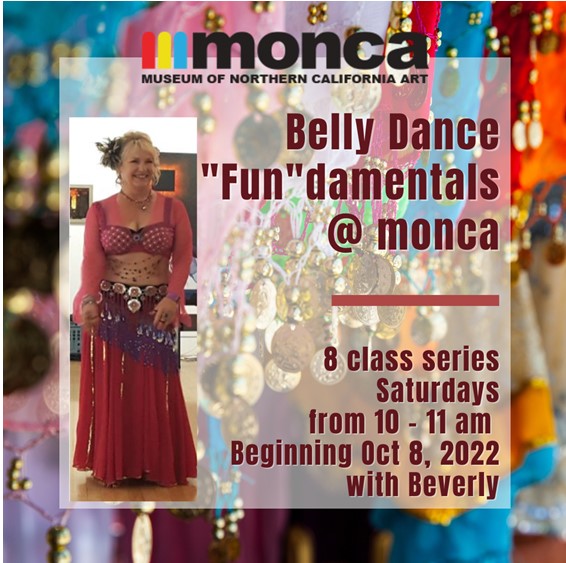
Join us in a safe, body-accepting environment and experience a sense of community while having fun learning the fundamentals of belly dance. Students wear workout clothes that they feel comfortable in and we supply sparkly hip shawls and veils. The movements of belly dance help strengthen core muscles, improve balance, and build self-confidence. This performance art is open to people of all ages and shapes. Join us to celebrate our strength and express joy through community, belly rolls and lots of shimmies!
Location: monca art museum
900 Esplanade, Chico, CA 95926
Time: Saturdays from 10am – 11am
Cost: $10 a class or $60 for 8 classes
All proceeds are donated to monca to support the arts.
You can mail payment to monca or bring payment to first class.
You can also venmo @Beverly-Thomassian
Click on this Link to Sign Up and hold your spot.
Instructor:
Belly Dance Fundamentals with Anushala (Beverly). She started shimmying when she turned 40 and hasn’t stopped since. Dancing lightens her life and brings immense joy. Plus, she loves sharing this art form with others. She believes in the healing powers of dance and community.
Share this flyer and invite your friends! We will have so much FUN!
We hope you can join us. You can email questions to [email protected].
Rationale of the Week | Right amount of insulin for 83 year old?

For last week’s practice question, we quizzed test takers on the right amount of insulin for an 83 year old. Only 50% of respondents chose the best answer, which indicates that there was some confusion. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
MS is an 83-year-old admitted to the hospital for a broken hip. MS has a BMI of 22.4, A1C of 6.9% on metformin 500mg twice daily. UACR is less than 30 and GFR is 48. The MD writes to stop oral meds in prep for surgery and start on basal-bolus insulin therapy.
Based on MS’s profile, what would be the most accurate formula to calculate their total daily insulin dose?
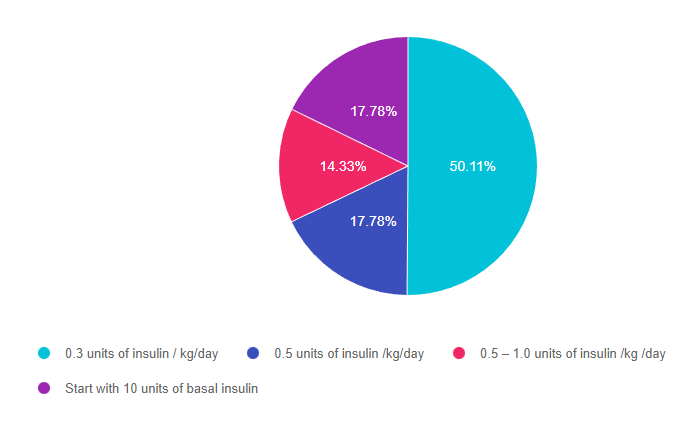
Answer Choices:
- 0.3 units of insulin / kg/day
- 0.5 units of insulin /kg/day
- 0.5 – 1.0 units of insulin /kg /day
- Start with 10 units of basal insulin
Getting to the Best Answer
Answer 1 is correct. 50.11% chose this answer, 0.3 units of insulin / kg/day.” YES, GREAT JOB. This is the best answer for several reasons. We can tell from the case study that MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting on a VERY conservative total daily insulin dose is the best and safest approach.
Answer 2 is incorrect. 17.78% of you chose this answer, “0.5 units of insulin /kg/day.” This is a juicy answer However MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting MS on 0.5 units/kg total daily insulin might be too much and might put MS at risk of hypoglycemia due to over insulinization.
Answer 3 is incorrect. 14.33% of respondents chose this answer, “0.5 – 1.0 units of insulin /kg /day.” This is another juicy answer However MS is a frail 83-year-old who is probably very insulin sensitive based on the following details: BMI of 22.4, A1C of 6.9% and GFR is 48. Leaner individuals need less insulin and people with a low GFR have slower renal clearance of insulin putting them at higher risk of hypoglycemia. In addition MS is insulin naïve and their A1C is on target on only 1000mg of Metformin daily. For all these reasons, starting MS on 0.5 – 1.0 units/kg total daily insulin might be too much and might put MS at risk of hypoglycemia due to over insulinization.
Finally, Answer 4 is incorrect. 17.78 chose this answer, “Start with 10 units of basal insulin.” This answer is appealing, since we often start people on 10 units of basal insulin. However, in this case study, we don’t have MS’s body weight to calculate their total daily insulin needs. Since we don’t have their weight in kgs, we don’t know what the right starting basal dose. For this reason, this is not the best answer.
Want to learn more about this question? Join us for our
Level 4 | Basal Bolus Therapy in Hospitals | 1.5 CEs
Recently updated and ready to watch!

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely and effectively implement Basal Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the patient’s clinical presentation and apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings and a discussion of solutions that will keep patients safe and get glucose levels to goal. In addition, sample basal/bolus and insulin drip guidelines plus lots of resource articles are included.
Objectives:
- Discussing appropriate insulin dosing based on the patient’s clinical presentation
- Applying dosing strategies to a variety of case studies
- Introduce hard-to-manage situations that commonly occur in hospital settings
- A discussion of solutions that will keep patients safe and get glucose levels to goal
- Sample basal/bolus and insulin drip guidelines plus lots of resource articles are included
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Abdominal lumps and insulin injections

JL is 67 years old, with a BMI of 23 and A1C of 7.6% and injects insulin 4 times a day to manage their type 1 diabetes. On visual inspection, you notice that there are many areas of lipohypertrophy on JL’s abdominal region.
Which of the following interventions would be the best recommendation?
- Switch to 50/50 insulin twice daily.
- Stop bolus insulin and switch to a GLP-1 RA.
- Switch bolus injections to inhaled insulin.
- Use a higher gauge needles to enhance absorption.
Click Here to Test your Knowledge
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Training Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Training Conference and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








