Can Fruits Boost Positive Mental Health?
Good news! People with diabetes can experience more joy and less depression by incorporating fruit into their diet. A study published in the British Journal of Nutrition found that swapping out cookies or chips for a few servings of fruit a day, boosted positive mental health.
How many times have you heard people or providers say they can’t eat fruit because it will wreak havoc on their diabetes? That statement is actually not accurate nor is it backed by science.
The truth is, people who consume a diet rich in fruits and vegetables, including fresh, canned, and frozen varieties, report a more positive psychological state. In addition, they are less likely to have symptoms of depression, stress, and anxiety compared to those who do not eat these nutrient-rich foods on a regular basis.

Why are fruits so good for our mental health?
Snacking on fruits throughout the day can promote the synthesis of serotonin, which improves moods. Plus, healthy gut bacteria thrive on the fiber and nutrients provided by these nutritional powerhouses. As a result, there is improved gut-brain communication and cognition and decreased inflammation.
Eat More Fruit and Fewer Snack Foods
These study results provide new insights into the associations between certain types of food and psychological health, and the mechanisms that may mediate the effect. This study identified that frequent fruit consumption has a direct positive relationship with mood. Whereas more frequent consumption of savory snacks, like packaged chips and other high-fat snack foods, was associated with increased symptoms of depression, stress, anxiety, and reduced psychological wellbeing.
People with diabetes are encouraged to celebrate fruit
Even though this study did not specifically evaluate people living with diabetes, they can still celebrate this news. Many people with diabetes think they have to avoid fruit since it contains sugar. However, by spreading their fruit consumption throughout the day, they can enjoy three servings a day, guilt-free. By watching portions, they can enjoy a rainbow of fruit knowing that they are boosting their mental health and well-being. In addition, we can encourage them to explore ways to include vegetables in their usual meals. These little changes can add up to big improvements in well-being and cognition.
For a quick list of fruit servings sizes in English and Spanish, you can download our Carbohydrate Cheat Sheets here, Carb Counting Quick Reference and Spanish Carb Counting Quick Reference.
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Specialist Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Course and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Right amount of insulin for 83 year old?

MS is an 83-year-old admitted to the hospital for a broken hip. MS has a BMI of 22.4, A1C of 6.9% on metformin 500mg twice daily. UACR is less than 30 and GFR is 48. The MD writes to stop oral meds in prep for surgery and start on basal-bolus insulin therapy.
Based on MS’s profile, what would be the most accurate formula to calculate their total daily insulin dose?
- 0.3 units of insulin / kg/day
- 0.5 units of insulin /kg/day
- 0.5 – 1.0 units of insulin /kg /day
- Start with 10 units of basal insulin
Click Here to Test your Knowledge
Want to learn more about this question? Join us for our
Level 4 | Basal Bolus Therapy in Hospitals | 1.5 CEs
Airs Thursday, August 25th, 2022

Glucose control in the hospital matters! This course provides participants with a step-by-step approach to safely and effectively implement Basal Bolus Insulin Therapy in the inpatient setting. We discuss appropriate insulin dosing based on the patient’s clinical presentation and apply dosing strategies to a variety of case studies. Included are hard-to-manage situations that commonly occur in hospital settings and a discussion of solutions that will keep patients safe and get glucose levels to goal. In addition, sample basal/bolus and insulin drip guidelines plus lots of resource articles are included.
Objectives:
- Discussing appropriate insulin dosing based on the patient’s clinical presentation
- Applying dosing strategies to a variety of case studies
- Introduce hard-to-manage situations that commonly occur in hospital settings
- A discussion of solutions that will keep patients safe and get glucose levels to goal
- Sample basal/bolus and insulin drip guidelines plus lots of resource articles are included
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best Action for Glucagon Rescue after too many beers?

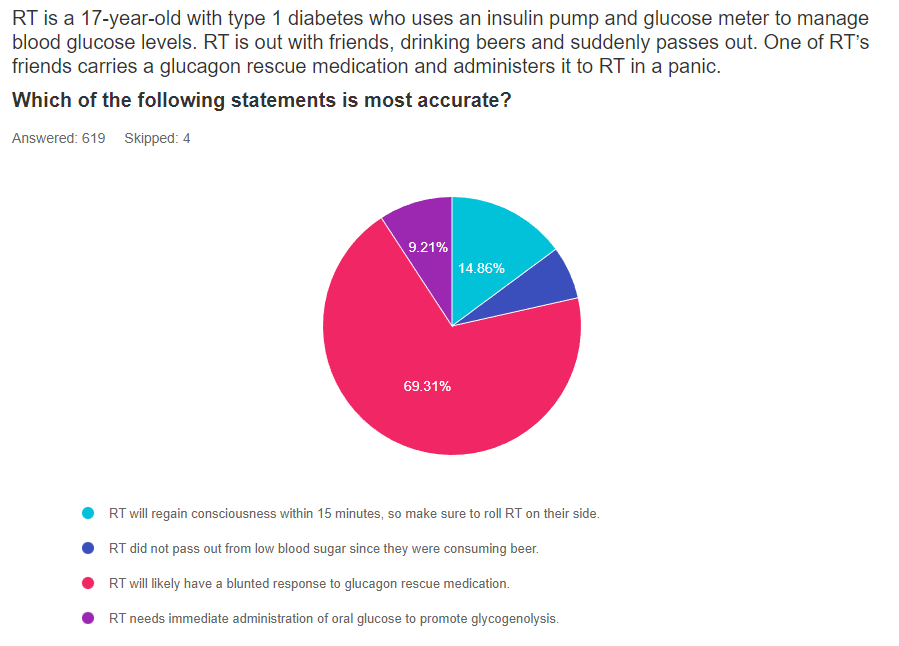
For last week’s practice question, we quizzed test takers on the best action for glucagon rescue medicine with beer. 70% of respondents chose the best answer. Great JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
RT is a 17-year-old with type 1 diabetes who uses an insulin pump and glucose meter to manage blood glucose levels. RT is out with friends, drinking beers and suddenly passes out. One of RT’s friends carries a glucagon rescue medication and administers it to RT in a panic.
Which of the following statements is most accurate?
Answer Choices:
- RT will regain consciousness within 15 minutes, so make sure to roll RT on their side.
- RT did not pass out from low blood sugar since they were consuming beer.
- RT will likely have a blunted response to the glucagon rescue medication.
- RT needs immediate administration of oral glucose to promote glycogenolysis.
Getting to the Best Answer
Answer 1 is incorrect. 15% chose this answer, “RT will regain consciousness within 15 minutes, so make sure to roll RT on their side.” Since alcohol consumption slows glycogen breakdown in the liver, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications. While we hope the RT regains consciousness quickly, there is a real possibility that it will take longer than 15 minutes. However, the second half of the answer offers sound advice. Since people often get nauseated and may vomit after receiving glucagon, it is a good idea to roll RT on their side. See our Blog for more info – Warning Alcohol can Blunt Impact of Glucagon
Answer 2 is incorrect. 5% of you chose this answer, “RT did not pass out from low blood sugar since they were consuming beer.” Although beer may contain some carbohydrate, the body considers alcohol a toxin and as soon as it reaches the bloodstream, the liver prioritizes metabolizing the alcohol and breaking it down. During this clean-up process, the liver is distracted from hormone signals that direct the liver to break down glycogen for energy and liberate glucose into the bloodstream. This clean-up can last for up to 8 hours, making delayed hypoglycemia a real possibility. See our Blog for more info – Warning Alcohol can Blunt Impact of Glucagon
Answer 3 is correct. 70% of respondents chose this answer, “RT will likely have a blunted response to the glucagon rescue medication.” YES, this is the best answer. Alcohol consumption slows glycogen breakdown in the liver, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications. When a person with type 1 diabetes drink alcohol, they at increased risk of hypoglycemia because the liver is less capable of breaking down stored glycogen.
Having a conversation with people with type 1 about the suppressive nature of alcohol on glycogen release for many hours after consuming alcohol is very important.
As a general rule of thumb, encouraging people with type 1 to eat 15gms of carbs with each drink and have a glass of water in between, may help make sure they have enough circulating carbs and slow the pace of alcohol consumption to help the liver with processing. They may also consider decreasing their insulin dose in association with alcohol intake to prevent this serious side effect. See our Blog for more info- Warning Alcohol can Blunt Impact of Glucagon
Finally, Answer 4 is correct. 9% chose this answer, “RT needs immediate administration of oral glucose to promote glycogenolysis.” This is a juicy answer. AFTER RT regains consciousness, they will certainly need to consume an oral form of energy to replete their glycogen stores and stabilize glucose levels. Of course, it isn’t safe to administer oral glucose when a person loses consciousness. Instead, emergency responders would administer glucagon or dextrose through an IV. See our Blog for more info- Warning Alcohol can Blunt Impact of Glucagon
Read more in our blog
Does Alcohol Intake Blunt Impact of Glucagon?
LS tells you that they frequently attend company mixers where they feel compelled to have at “least a few drinks”, to fit in and network.
The tricky part is that LS lives with type 1 diabetes. Since they don’t have a working pancreas, their circulating levels of insulin and glucagon are often mismatched to their body’s needs.
If LS has several drinks, then loses consciousness from hypoglycemia, will emergency treatment be effective?
There is emerging evidence that glucagon rescue medications may have a blunted response when ingesting alcohol.
Want to learn more about this question?
Enroll in our upcoming webinar series updates
Level 4 | Advanced Level & Specialty Topic Courses | 13+ CEs
Join us live beginning August 9th through November 9th at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about Specialty Topics for their clinical practice or for those who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) certification exam.
2022 Live Webinar Updates
Previously recorded & available for on-demand viewing
- The Impact of Adverse Childhood Experiences on Health | 1.0 CE
- 3 Steps to Save Feet; Assess, Screen, and Report | 1.0 CEs
- Solving Glucose Mysteries for Type 1 | 1.5 CEs
- Solving Glucose Mysteries for Type 2 | 1.5 CEs
All courses air at 11:30 a.m. (PST)
- August 23, 2022 | Insulin Calculation Workshop – From Pumps & Beyond | 1.5 CEs
- August 25, 2022 | Basal Bolus Therapy in Hospital |1.5 CEs
- September 15, 2022 | Type 2 Diabetes Intensive | 2 CEs
- October 26, 2022 | Cancer & Diabetes | 1.25 CEs
- November 9, 2022 | Getting to the Gut (& Skin) | 1.0 CEs
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.

Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Warning – Food Dates Can Lead to Unnecessary Waste
Have you inspected a salad mix that you bought last week and wondered if you should toss it because it expired yesterday? If you said yes, you are not alone. About 40% of food waste happens in the kitchen, when consumers throw away foods that have passed the expiration date.

However, food and legal experts are asking consumers to reconsider their thinking.
According to an NPR Article, “The U.S. Department of Agriculture, the Food and Drug Administration, the Harvard Food Law Clinic – all say that consumer uncertainty about the meaning of food dates is part of the food waste problem. And it’s not just about wasting food or wasting the water and resources that went into making it. Food is the main thing we send to U.S. landfills.” Food in landfills is converted to methane, a highly potent greenhouse gas.
Consider all the money we are throwing way every day by disposing of foods that might be perfectly fine for consumption. For people living with diabetes on a limited or fixed income, it can really add up. In addition, people may avoid purchasing fresh fruits and vegetables if they are worried about eating it by the date stamped on the package.
Research shows that one in three bags of groceries purchased will end up in the trash due to dates stamped on food items. What do these dates mean anyway?
The federal government doesn’t require dates on any food except baby formula. According to the United States Department of Agriculture (USDA), foods are still safe for consumption after these expiration dates pass, but make sure to look out for an off odor, flavor, or texture that mean the food has spoiled and should not be eaten.
The FDA says the dates on food aren’t serving a safety role. A food and law expert, Broad Leib says, “however, you do want to pay attention to dates on food in the prepared food section, including deli meat, raw fish, unpasteurized milk and cheese.”
But for most foods, like a box of mushrooms or a bottle of ketchup, Broad Leib suggests we take a pause to look at the food. Smell and taste it to determine if it seems okay to eat. We can tell if something went bad.
Except for infant formula, dates are not an indicator of the product’s safety and are not required by Federal law.
Where do the dates come from? Since the federal government doesn’t require the dates, the “sell by” or “enjoy by” dates are determined mostly by the manufacturers. Manufacturers put the date on the package to encourage consumers to eat the food product when it tastes best, not when the food will go “bad”. They want to protect their brand and encourage the consumer to purchase their product again.
Sometimes states will get involved in determining a shelf life of a product for various reasons, including supporting local companies. For this reason, there is a lot of discrepancy from state to state, since the date isn’t based on food spoilage data. An example is that in Montana, milk has to be sold within 12 days of pasteurization. In Idaho, the milk can stay on the shelf for 23 days.
Deciphering Food Label dates:
- “Best if Used By/Before” indicates best flavor or quality. It is not a safety date.
- “Sell-By” date tells the store how long to display the product for sale for inventory management. It is not a safety date.
- “Use-By” date is the last date recommended for the use of the product while at peak quality. It is not a safety date except for when used on infant formula*.
Food makers, grocery stores, federal agencies are ready to decrease the confusion and food waste. They suggest getting rid of all the “enjoy-by, packaged on” dates and have only two options – best if used by or use by.
“Best if used by” would tell consumers this ketchup would be best by this date, but you could still eat it after.
“Use by” would tell consumers, after this date, it’s probably not a good idea to eat the mustard.
The next time you are ready to toss your salad mix or Worchester sauce, look it over, take a whiff or a taste and you will know if it’s still good to eat.
For more information, see our Protecting the Planet Resource Page.
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Training Conference
30+ CEs
Airs October 12-14th, 2022
Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
?Group discounts are available!*
Download Course Flyer | Download Schedule
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Should I toss food if it’s past the date?

A person comes into the clinic for a diabetes education appointment. They are on a budget and ask you if they should throw away food if it is older than the date on the package?
What is the most accurate response?
- Manufacturer’s stamp foods with date to comply with federal safety standards.
- Before throwing away the food, look at it and smell or taste it to see if it has gone bad.
- The date on food packaging indicates when it is no longer safe to consume.
- Food packaging dates are federally regulated and help keep consumers safe.
Click Here to Test your Knowledge
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Training Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Training Conference and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Read more in our blog
Food Dates Can Lead to Unnecessary Waste

Have you inspected a food product that you bought last week and wondered if you should toss it because it expired yesterday? If you said yes, you are not alone.
About 40% of food waste happens in the kitchen, when consumers throw away foods that have passed the expiration date.
Are we throwing away perfectly good food based on the date stamped on the package?
Dates are confusing and they are often not associated with safety concerns. Learn why food and legal experts are asking consumers to reconsider their thinking.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Premeal Glucose is Too Low

For last week’s practice question, we quizzed test takers on what to do when premeal glucose is too low. 49% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: RL carb counts and takes 1 unit of insulin for every 10 gms of carbohydrate. RL also uses a correction ratio and takes 1 unit for every 40 points above their glucose target of 120. RL’s asks you what to do if their premeal glucose is less than 70 before their lunch meal at work. RL often has blood sugar drops right before lunch and usually eats a sandwich, chips, berries and some sparkling water for lunch.
Given the situation, what is the best recommendation for JL to do if their pre-lunch glucose is less than 70 mg/g?
Answer Choices:
- Immediately eat 15gms of berries and recheck glucose in 15 minutes.
- Decrease usual insulin carb coverage for this meal by 1 or 2 units.
- Encourage RL to eat lunch immediately and give insulin afterward.
- Discuss which strategies would work best for RL in this situation.
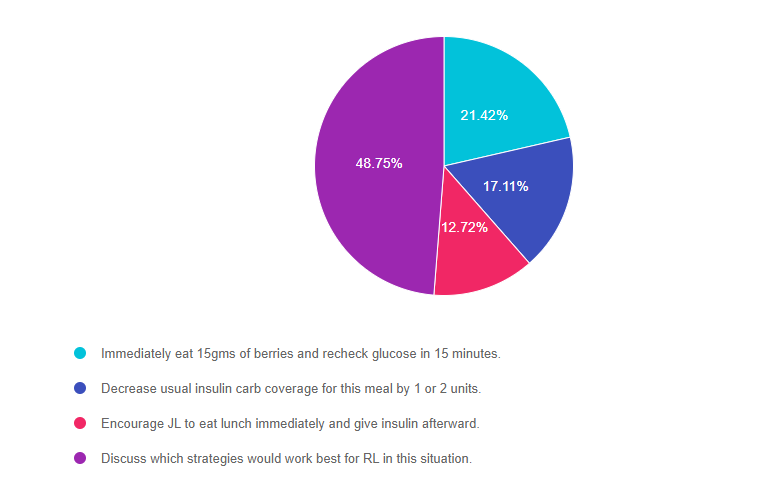
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 21.42% chose this answer, “Immediately eat 15gms of berries and recheck glucose in 15 minutes.” This answer is a right answer, but it is not the BEST answer. Yes, we recommend treating low blood sugar with 15 gms of carbohydrate, but is this the preferred treatment strategy for RL? Would RL choose this option?
Answer 2 is incorrect. 17.11% of you chose this answer, “Decrease usual insulin carb coverage for this meal by 1 or 2 units.” This also could be a right answer, but it is not the BEST answer. When faced with a premeal low blood sugar, some people may choose to decrease their bolus insulin dose by 1-2 units, but is this the preferred treatment strategy for RL?
Answer 3 is incorrect. 12.72% of respondents chose this answer, “Encourage RL to eat lunch immediately and give insulin afterward.” This also could be a right answer, but it is not the BEST answer. When faced with a premeal low blood sugar, some people may choose to eat first then give their insulin afterward, based on glucose levels, but is this the preferred treatment strategy for RL?
Finally, Answer 4 is correct. 48.75% chose this answer, “Discuss which strategies would work best for RL in this situation.” YES, this is the BEST answer. RL may choose any of the above mentioned strategies, or RL may have some other ideas on how to manage this situation. Our goal is to keep it person centered and recognize the expertise of the individual who lives with diabetes everyday.
Level 4 | Advanced Level & Specialty Topic Courses | 13+ CEs
Join us live beginning August 9th through November 9th at 11:30 am PST

This bundle is specifically designed for healthcare professionals who want to learn more about Specialty Topics for their clinical practice or for those who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) certification exam.
2022 Live Webinar Updates
Previously recorded & available for on-demand viewing
- The Impact of Adverse Childhood Experiences on Health | 1.0 CE
- 3 Steps to Save Feet; Assess, Screen, and Report | 1.0 CEs
- Solving Glucose Mysteries for Type 1 | 1.5 CEs
All courses air at 11:30 a.m. (PST)
- August 11, 2022 | Solving Glucose Mysteries for Type 2 | 1.5 CEs
- August 23, 2022 | Insulin Calculation Workshop – From Pumps & Beyond | 1.5 CEs
- August 25, 2022 | Basal Bolus Therapy in Hospital |1.5 CEs
- September 15, 2022 | Type 2 Diabetes Intensive | 2 CEs
- October 26, 2022 | Cancer & Diabetes | 1.25 CEs
- November 9, 2022 | Getting to the Gut (& Skin) | 1.0 CEs
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Warning – Alcohol can Blunt Impact of Glucagon Rescue Meds
LS tells you that they frequently attend company mixers where they feel compelled to have at “least a few drinks”, to fit in and network. The tricky part of this scenario is that LS lives with type 1 diabetes. Since they don’t have a working pancreas, their circulating levels of insulin and glucagon are often mismatched to their body’s needs.
When discussing the situation, LS says they feel confident they can handle alcohol and prevent lows since they have lived with type 1 diabetes for over ten years. LS shares, “I feel comfortable recognizing when both arrows are pointing down and I am heading for a glucose crash”.
As educators, we are committed to taking person-centered approach while encouraging safe practices.
In regards to LS, we realize alcohol’s impact on the thought process and blood glucose levels. We know that alcohol can affect critical thinking and possibly impair recognition of an impending hypoglycemic event. Inebriation also has many symptoms in common with hypoglycemia. Plus, alcohol consumption slows glycogen breakdown in the liver, which increases the risk of hypoglycemia. Lastly, based on a study published in Endocrinology Advisor, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications.
In the worst-case scenario, if LS experiences severe low blood sugar and passes out, alcohol ingestion can blunt the effectiveness of the glucagon rescue medications.
Alcohol and Glucagon Pathophysiology Review
The body considers alcohol a toxin and as soon as it reaches the bloodstream, the liver prioritizes metabolizing the alcohol and breaking it down. During this clean-up process, the liver is distracted from responding to endogenous glucagon, the hormone that signals the liver to break down glycogen for energy and liberate glucose into the bloodstream. This clean-up can last for up to 8 hours, making delayed hypoglycemia a real possibility.
When a person with type 1 diabetes drink alcohol, they at increased risk of hypoglycemia because the liver isn’t breaking down stored glycogen to increase blood glucose levels.
Let’s get back to LS. What if LS is drinking gin and diet tonics and only munching on low-carb vegetables and cheeses during the mixer? LS is not ingesting many carbohydrates, so glycogen stores may be low and the liver is busy cleaning up the alcohol and blood sugars start dropping. By the 4th drink, LS isn’t thinking very clearly, says they “feel funny” and passes out.
A colleague of LS carries a glucagon emergency kit and provides LS with a dose and calls 911. After 15 minutes, LS still hasn’t regained consciousness, so a second dose is administered. The paramedics arrive and check the glucose, it is 53.
Simply put, glucagon rescue medications may not work if the person drinks too much alcohol.
After reviewing the package inserts of all available US manufactured Glucagon Rescue Meds, there are no warnings for alcohol intake decreasing the effectiveness of glucagon rescue meds. So, I dug a little deeper and found a decent study on the topic which describes the impact of alcohol ingestion on glucose-regulating hormones.
I also found a very helpful monograph published by Lilly Baqsimi in Canada. Baqsimi is a powdered glucagon rescue medication that is delivered nasally. The Baqsimi monograph clearly states several warnings, “Alcohol can suppress hepatic gluconeogenesis and chronic alcoholism can deplete liver glycogen stores. Therefore BAQSIMI may be less effective in presence of acute or chronic alcohol ingestion. Alcohol-induced hypoglycemia is associated with a failure of blood glucose levels to rise normally after glucagon administration. BAQSIMI may not work if the person drinks too much alcohol.“.
Keeping it Real and Safe
In conclusion, having a conversation with people with type 1 about the suppressive nature of alcohol on glycogen release for many hours after consuming alcohol is very important. Another important teaching point is that glucagon rescue meds may not be as effective and timely in raising glucose to safe levels.
As a general rule of thumb, encouraging people with type 1 to eat 15gms of carbs with each drink and have a glass of water in between, may help make sure they have enough circulating carbs and slow the pace of alcohol consumption to help the liver with processing. They may also consider decreasing their insulin dose in association with alcohol intake to prevent this serious side effect.
Download our Glucagon Rescue Med PocketCard for more information here.
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Specialist Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Course and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Best Action for Glucagon Rescue with Beer?

RT is a 17-year-old with type 1 diabetes who uses an insulin pump and glucose meter to manage blood glucose levels. RT is out with friends, drinking beers and suddenly passes out. One of RT’s friends carries a glucagon rescue medication and administers it to RT in a panic.
Which of the following statements is most accurate?
- RT will regain consciousness within 15 minutes, so make sure to roll RT on their side.
- RT did not pass out from low blood sugar since they were consuming beer.
- RT will likely have a blunted response to the glucagon rescue medication.
- RT needs immediate administration of oral glucose to promote glycogenolysis.
Click Here to Test your Knowledge
Want to learn more about this question?
Enroll in our upcoming webinar series updates
Level 4 | Advanced Level & Specialty Topic Courses | 12+ CEs
Join us live beginning August 9th through November 9th at 11:30 am PST
This bundle is specifically designed for healthcare professionals who want to learn more about Specialty Topics for their clinical practice or for those who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) certification exam.
2022 Live Webinar Updates
Previously recorded & available for on-demand viewing
- The Impact of Adverse Childhood Experiences on Health | 1.0 CE
- 3 Steps to Save Feet; Assess, Screen, and Report | 1.0 CEs
All courses air at 11:30 a.m. (PST)
- August 9, 2022 | Solving Glucose Mysteries for Type 1 | 1.5 CEs
- August 11, 2022 | Solving Glucose Mysteries for Type 2 | 1.5 CEs
- August 23, 2022 | Insulin Calculation Workshop – From Pumps & Beyond | 1.5 CEs
- August 25, 2022 | Basal Bolus Therapy in Hospital |1.5 CEs
- September 15, 2022 | Type 2 Diabetes Intensive | 2 CEs
- October 26, 2022 | Cancer & Diabetes | 1.25 CEs
- November 9, 2022 | Getting to the Gut (& Skin) | 1.0 CEs
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.

Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Read more in our blog
Does Alcohol Intake Blunt Impact of Glucagon?
LS tells you that they frequently attend company mixers where they feel compelled to have at “least a few drinks”, to fit in and network.
The tricky part is that LS lives with type 1 diabetes. Since they don’t have a working pancreas, their circulating levels of insulin and glucagon are often mismatched to their body’s needs.
If LS has several drinks, then loses consciousness from hypoglycemia, will emergency treatment be effective?
There is emerging evidence that glucagon rescue medications may have a blunted response when ingesting alcohol.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








