You’re invited to our Upcoming Webinars!
See Full Calendar for Diabetes Education Services Webinars and Seminars
Starting your journey to becoming a CDCES?
Join us live August 10th at 11:30 am PST for our
Preparing for the CDCES Exam FREE Webinar
This course will transform your test anxiety into calm self-confidence and test taking readiness.
Can’t join us live?
Don’t worry, register and we will send you a link to the recorded version.
Webinar Topics
Read More: Preparing for CDCES Exam Webinar TopicsPreparing for the CDCES Exam |
FREE Webinar
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
CDCES Online Prep Bundle (Levels 1, 2, and 3) +
ADCES Review Guide with 480+ Practice Questions
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
August 2022 eNews | Diabetes Safety Update | Does Alcohol Blunt Glucagon Effectiveness?
August 2022 eNews | Diabetes Safety Update | Does Alcohol Blunt Glucagon Effectiveness?

Happy August
There is still time to celebrate warm summer nights before the days lengthen and get cooler. For people living with diabetes, summer parties, with their special treats and yummy drinks, can be complicated to navigate.
In our first article, we take a close look at the impact of alcohol on the effectiveness of glucagon rescue medications. As an educator for many years, I was not aware of alcohol’s impact on glucagon efficacy. Through increased knowledge, I am hopeful we can enhance the safety of people living with type 1 diabetes.
Our next article celebrates the abundance and deliciousness of summer fruit. Sadly, so often, people with diabetes are told not to eat fruit because it is “full of sugar.”
I reassure them that fruit is loaded with nutrients, fiber and decreases inflammation. In a new study, researchers highlight clear evidence that eating a portion of fruit is far better for our mental health than eating other sweet treats like cookies and snack foods. Plus, the study demonstrated that snacking on fruit not only boosts mood it can also improve cognition and decrease stress.
We also take a close look at the impact of those pesky dates on our food packaging. Almost 40% of food waste happens in our kitchen when consumers think food is too old to eat based on package dates. But, are we wasting food unnecessarily? Read more to gain clarity on what these dates signify. Let’s share this information with our communities to help decrease food waste and save money.
Lastly, we celebrate our special scholarship recipient, Judith, who recently earned her CDCES. Please join me in congratulating this dedicated, kind and enthusiastic individual.
We hope you enjoy our question and rationale of the week and we invite you to join our upcoming webinars and Virtual Conference.
Thank you in advance for your actions and advocacy on behalf of people living with diabetes.
Beverly, Bryanna, Robert, and Amanda
Featured Articles
- Does Alcohol Intake Blunt Impact of Glucagon?
- Food Dates Can Lead to Unnecessary Waste
- Does Snacking on Food Improve Mood?
- Scholarship Recipient Receives CDCES!
- Question of the Week
- Rationale of Week
Upcoming Webinars
- Virtual DiabetesEd Specialist Conference | Oct. 12-14th
- CDCES Exam Prep | Aug. 10th
- Solving Glucose Mysteries for Type 1 | Aug. 9th
- Solving Glucose Mysteries for Type 2 | Aug. 11th
- Insulin Calculation Workshop | Aug. 23rd
ADCES Book Bundle
Starting your journey to becoming a CDCES?
Join us live August 10th at 11:30 am PST for our
Preparing for the CDCES Exam FREE Webinar
This course will transform your test anxiety into calm self-confidence and test taking readiness.
Can’t join us live?
Don’t worry, register and we will send you a link to the recorded version.
Webinar Topics
Read More: Preparing for CDCES Exam Webinar TopicsPreparing for the CDCES Exam |
FREE Webinar
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Best treatment for abrasion?

For last week’s practice question, we quizzed test takers on the best treatment for abrasions 65% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 38 years old and takes insulin twice a day. They mention they went to the bathroom at night, lost their balance, and scraped their shin. They put a band-aid on it, but want you to take a look.
What is the best approach to treat the abrasion?
Answer Choices:
- Clean carefully with sanitizing gel, apply topical antibiotic and observe for signs of infection.
- Discuss creating a safe path to the bathroom at night and assess the abrasion for severity.
- Replace the band-aid with gauze and suggest they make an appointment with podiatry.
- Take a photo of the abrasion, wash with soap and water, and apply iodine around the perimeter.
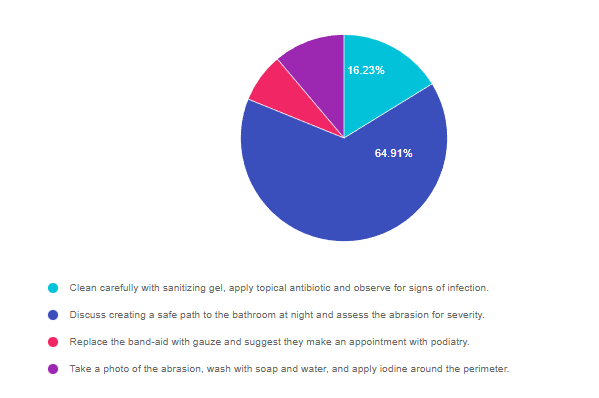
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 4, and finally option 3.
Getting to the Best Answer
Answer 1 is incorrect. 16.23% chose this answer, “Clean carefully with sanitizing gel, apply topical antibiotic and observe for signs of infection.” This is a juicy answer, but not the best answer for this situation for two main reasons. Applying topical antibiotic is a great idea, but generally, abrasions are cleansed with soap and water instead of sanitizing gel. In addition, this answer did not address the core issue, of improving safety when going to the bathroom at night.
Answer 2 is correct. 64.91% of you chose this answer, “Discuss creating a safe path to the bathroom at night and assess the abrasion for severity.” YES, GREAT JOB, this is the best answer. Many lower extremity falls, scrapes and injuries happen on the way to the bathroom when it is dark. It is important to make sure people have a safe path, including night lights and removal of any potential fall risks, especially for older people with balance issues.
Answer 3 is incorrect. 7.71% of respondents chose this answer, “Replace the band-aid with gauze and suggest they make an appointment with podiatry.” It is important to evaluate and treat the abrasion, but it does not warrant an automatic referral to the podiatrist, especially since it is on the shin. Also, this question does not provide enough details about the severity of the wound to determine if further treatment is required.
Finally, Answer 4 is incorrect. 11.16% chose this answer, “Take a photo of the abrasion, wash with soap and water, and apply iodine around the perimeter.” Of course it is a great idea to evaluate an abrasion, but iodine can cause skin irritation and not usually recommended as an antiseptic. In addition, this answer did not address the core issue, of improving safety when going to the bathroom at night.
Announcing our Special Scholarship Recipient – Judith Paul

When Judith reached out to us for guidance to achieve her dream of becoming a CDCES, her sincerity and passion for improving diabetes care were immediately evident.
Judith contacted us last winter as she was preparing to take the CDCES exam. Through our phone conversations, her passion for Diabetes Care stood out.; she is inquisitive, enthusiastic, and has a strong desire to provide the best diabetes care possible.
Through our conversations, I got to know Judith very well. She had moved here several years ago from Haiti with a goal to become an RN, and eventually a Diabetes Educator. For Judith, diabetes is very dear to her heart as she has close family members who live with diabetes. She saw firsthand the devastating effects it can have when someone doesn’t receive adequate care.
Judith Paul embodies what it means to be a Diabetes Advocate
Becoming a CDCES is not an easy journey for anyone. A health care professional has to demonstrate 1000 hours of diabetes self-management work experience, earn CE’s, apply online and pay the testing fee of $350. Then there is the grueling four-hour exam, with complicated questions that use precise and nuanced language. Preparing for the exam requires months of dedicated study and preparation.
Making a Difference Scholarship
As I got to know Judith more, I felt should we be a great candidate for our “Making a Difference” Scholarship. We usually only offer this award once a year in the Spring to candidates who are making significant contributions to improving diabetes care in their community, but Judith’s desire and determination won our hearts. We awarded Judith free access to our CDCES Prep Bundle, to support her dream to become a Certified Diabetes Care and Education Specialist. Judith fully immersed herself in her studies. Over time, I could hear the changes in her language as she moved towards a more person-centered approach.
After months of dedicated studying, she passed her CDCES Exam this June!
We are so proud of you, Judith, and know that you are going to continue being a fantastic model for your colleagues to provide outstanding care for people living with diabetes!
Judith’s Story in Her Own Words
I am so excited to let Diabetes Education Services know that I recently passed the CDCES exam! I have dreamed of becoming a CDCES since 2017 and my thanks go to coach Beverly and Bryana for helping me make my dream a reality. My passion about diabetes education and those living with the disease drove me, along with my desire to share accurate and compelling information with patients and colleagues to help improve care.
I heard about Diabetes Education Services from a co-worker in December 2021 when I spoke with Bryanna. She was very professional, intelligent, kind, and helpful. She explained the program in detail and answered all of my questions and she provided me with information about the classes, online courses, free resources, App access, and much more. I am beyond grateful for all the support I received from coach Beverly and Bryanna. Coach Beverly made learning so fun and easy to understand. She teaches exactly the way I learn. I always looked forward to attending classes, listening to the webinar, podcast, and taking the quizzes. Her passion, knowledge and love for people living with diabetes are exceptional and she has inspired me even more. I have become more passionate, caring, and knowledgeable and I found myself talking to patients more effectively thanks to her example. Where I used to say “diabetic”, “obesity”, or “blood glucose not in control”, now I use phrases like “people with diabetes”, “participant with excess weight”, “blood glucose above target”, etc.
I found the CDCES exam so EASY because of the coaching program and your teaching style was exactly what I needed to be successful. You provided me with all the tools and resources that I needed. Coach Beverly’s program has the WHOLE package for people like me who need to learn about special situations such as pregnancy or pediatric, and also about diabetes technology. I learned test-taking strategies like choosing the best answers by using a process of elimination. I have attended other diabetes courses in the past, but I had never felt ready for the exam until I attended your program. During the exam I felt ready, confident, calm, and well prepared and I smiled as I heard Coach Beverly’s voice in my head. Coach Beverly not only teaches what you need to know to be successful in the CDCES exam, but also, she teaches how to be an excellent diabetes educator. Throughout the entire program, I felt like I had my own, personal coach and tutor. Beverly and Bryanna always responded to my emails and my last-minute questions in a timely manner.
Again, THANK YOU Coach Beverly, Bryanna, and all of the Diabetes Education Services staff for helping me make my dream a reality. As a person with a strong family history of diabetes, passing the CDCES exam is a HUGE personal accomplishment for me, and I could NOT have earned this certification without the Diabetes Education Services program. I plan to use Diabetes Education Services to obtain my CEUs and to polish my skills.
If someone is considering becoming a CDCES, they should absolutely consider this program. The designations CDCES after my name came from hard work and with help and support from Diabetes Education Services. Thank you, and I highly recommend you.
Judith Paul, BSN, RN, CCM, CDCES
Starting your journey to becoming a CDCES?
Join us live August 10th at 11:30 am PST for our
Preparing for the CDCES Exam FREE Webinar
This course will transform your test anxiety into calm self-confidence and test taking readiness.
Can’t join us live?
Don’t worry, register and we will send you a link to the recorded version.
Webinar Topics
Read More: Preparing for CDCES Exam Webinar TopicsPreparing for the CDCES Exam |
FREE Webinar
What is a Certified Diabetes Care and Education Specialist?
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | Premeal Glucose is Too Low

RL carb counts and takes 1 unit of insulin for every 10 gms of carbohydrate. RL also uses a correction ratio and takes 1 unit for every 40 points above their glucose target of 120. RL’s asks you what to do if their premeal glucose is less than 70 before their lunch meal at work. RL often has blood sugar drops right before lunch and usually eats a sandwich, chips, berries and some sparkling water for lunch.
Given the situation, what is the best recommendation for JL to do if their pre-lunch glucose is less than 70 mg/g?
- Immediately eat 15gms of berries and recheck glucose in 15 minutes.
- Decrease usual insulin carb coverage for this meal by 1 or 2 units.
- Encourage JL to eat lunch immediately and give insulin afterward.
- Discuss which strategies would work best for RL in this situation.
Click Here to Test your Knowledge
Want to learn more about this question?
Enroll in our upcoming webinar
Solving Glucose Mysteries for Type 1
Airs live on August 9th at 11:30 am PST
Why do the blood sugars keep dropping after meals? Is the basal insulin set correctly? What adjustments are needed for exercise?
During this webinar, Coach Beverly addresses each of these glucose mysteries and more, using a person-centered approach. She describes a stepwise approach to evaluate glucose patterns and correct common issues encountered by people living with type 1 diabetes.
Objectives:
- Describe common glucose mysteries encountered by people with type 1 diabetes.
- Using a stepwise approach, evaluate factors affecting glucose patterns.
- State interventions to increase time-in-range and improve quality of life.
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.

Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Uvalde T-Shirt Clothesline on display at Museum of Northern California Art (monca)
Installation Connects Common Humanity Through Art

CHICO, CA, Sept 19, 2022—**Dismayed over the horrific school shooting that occurred in Uvalde, Texas on May 24, a group of local mothers organized an art installation featuring 21 orange t-shirts, hand-painted with the names of the children and teachers who died. The Uvalde T-Shirt Clothesline was displayed at the Chico Farmer’s Market on July 2nd and now graces the front arches of the Museum of Northern California Art (monca). Orange is the commemorative color of gun violence prevention. Since 2020, firearms have become the leading cause of death for children in the United States, surpassing motor vehicle accidents.[1] Every 2 hours and 36 minutes, a child loses their life due to firearm violence, accidents, or suicide.[2]
“The Uvalde T-Shirt Clothesline speaks of the empty shirts left behind: shirts that will never be played in, worn to school, or hugged at night. Shirts whose young owners will never reach their full potential.” – Beverly Thomassian
“Hanging shirts to dry on a line is a common household activity. The fact that our kids are growing up in a culture of gun violence and school shootings, that they do drills in school to practice how to respond in case of an actual violent attack, that this has become so routine, so commonplace–as ordinary as doing laundry–is why this installation of empty shirts hung on a clothesline has such an immediate, powerful effect.” – Amy Antongiovanni
Be SMART – Gun Safety Alliance of Northern California is a newly formed local chapter of the national Be SMART for Kids campaign. Our goals are:
- to shine a light on the problem of gun violence against children
- to connect our common humanity through art
- to raise awareness that secure gun storage—storing guns locked, unloaded and separate from ammunition—can save children’s lives
Contact – Beverly Thomassian, Be SMART Advocate, [email protected]
[1] Current Causes of Death in Children and Adolescents in the United States, N Engl J Med, May 19 2022; 386:1955-1956, DOI: 10.1056/NEJMc2201761
[2] https://www.childrensdefense.org/policy/policy-priorities/gun-violence-prevention/
Press Release
Download Press Release here
T-Shirt Clothesline Tribute makes local paper front page.
Read Enterprise Record Article here.
Resources
Nurses Union Addresses Gun Violence
Art Displays
Uvalde mural honors Robb Elementary School shooting
More information here
Rationale of the Week | Best action to treat a corn?

For last week’s practice question, we quizzed test takers on why diabetes foot care is important. 93% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: A person with diabetes has small corn on their pinky toe and it bothers them when walking.
What is the best first action?
Answer Choices:
- Instruct them on to how to safely use a liquid corn remover.
- Encourage them to buy a shoe size larger than their usual shoe size.
- Carefully trim the corn with a sterile instrument and cover with gauze padding.
- Refer the person to a foot specialist.
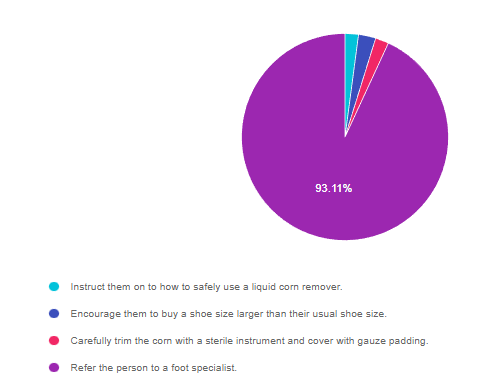
As shown above, the most common choice was option 4, the second most common answer was option 2, then a tie for options 1 and 3.
Getting to the Best Answer
Answer 1 is incorrect. 2.10% chose this answer, “Instruct them on to how to safely use a liquid corn remover.” The problem with corn and callus liquid or patch treatments, is that they contain salicylic acid, which can remove the callus/corn, but also damage the healthy tissue underneath. This disruption in skin integrity can lead to ulcerations and increase the risk of skin infections, especially if the person with diabetes is experiencing blood glucose elevations. We have created foot care education sheets in English and Spanish that you are invited to print and share. Let’s prevent the agony of “DeFeet”. Foot Care Teaching Sheet – Steps to Healthy Feet. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Answer 2 is incorrect. 2.69% of you chose this answer, “Encourage them to buy a shoe size larger than their usual shoe size.” While it is important to make sure there is plenty of room to wiggle toes and avoid rubbing from tight fitting shoes, it is also important to avoid ill fitting shoes. Wearing too large of shoes can lead to slippage and increased friction resulting in blisters and ulcers. These teaching sheets demonstrate an easy strategy to make sure that people are wearing the best size shoes for their foot shape. Foot Care Teaching Sheet – Steps to Healthy Feet. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Answer 3 is incorrect. 2.10% of respondents chose this answer, “Carefully trim the corn with a sterile instrument and cover with gauze padding.” People diabetes are strongly discouraged from performing any “bathroom surgery” to self-treat foot problems. Approved foot care tools for foot care include, nail clippers, nail file, soap and water, washcloth, gentle scrub brush, lotions, socks and shoes. We have created foot care education sheets in English and Spanish that you are invited to print and share. Let’s prevent the agony of “DeFeet”. Foot Care Teaching Sheet – Steps to Healthy Feet. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Finally, Answer 4 is incorrect. 93.11% chose this answer, “Refer the person to a foot specialist.” GREAT JOB. Most people chose this answer for good reason, the action of referring a person with foot problems to a Podiatrist significantly reduces the risk of ulceration, infection and amputation. By identifying and referring people with high risk feet to specialists, we can reverse the trend of increasing amputations and improve quality of life. We are happy to share these free lower extremity education handouts with you. Please feel free to print and share! Foot Care Teaching Sheet – Steps to Healthy Feet. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Want to learn more about this question?
Enroll in our Foot Screening Bundle, now on Sale!
This bundle includes our 3 Steps to Save Feet; Assess, Screen, and Report Webinar + 20-pack of Monofilament + ADA Foot Screening Chart
People with diabetes are at increased risk of foot complications. Basic foot care education and intervention can reduce the risk of amputation by over 50 percent.
This bundle comes with our:
We have included instructions on assessing and inspecting feet, risk assessment, and action steps. We enhanced the teaching tools and forms from the Lower Extremity Prevention Program (LEAP) and are excited to share them with our community of diabetes advocates.
FREE Resources for Health Care Professionals and People with Diabetes
3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings.
Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language.
Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language.
FREE Handouts and Resources
Read More: FREE Handouts and Resources 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. JR is 38 years old and takes insulin twice a day. They mention they were going to the bathroom at night, lost their balance and scraped their shin. They put a band-aid on it, but want you to take a look. What is the best approach to treat the abrasion? Click Here to Test your Knowledge 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. Question of the Week | Best treatment for abrasion?

Want to learn more about this question?
Foot Screening Bundle – Purchase Now and save $15!
3 Steps to Save Feet Webinar + Monofilament 20-Pack + ADA Foot ChartCan’t join us live?
Don’t worry, we will send you a link to the recorded version.FREE Handouts and Resources









