Rationale of the Week | Why is Diabetes Foot Care So Important?

For last week’s practice question, we quizzed test takers on why diabetes foot care is important. 91% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Why is it important that people with diabetes pay special attention to taking care of their feet?
Answer Choices:
- Years of insulin injections can increase risk of lower extremity complications.
- People with diabetes often experience changes in lower extremity sensation and circulation.
- Unusual skin growths are associated with diabetes unless preventative measures are routinely used.
- Everyone with diabetes needs a referral to a Podiatrist to prevent foot problems from starting.
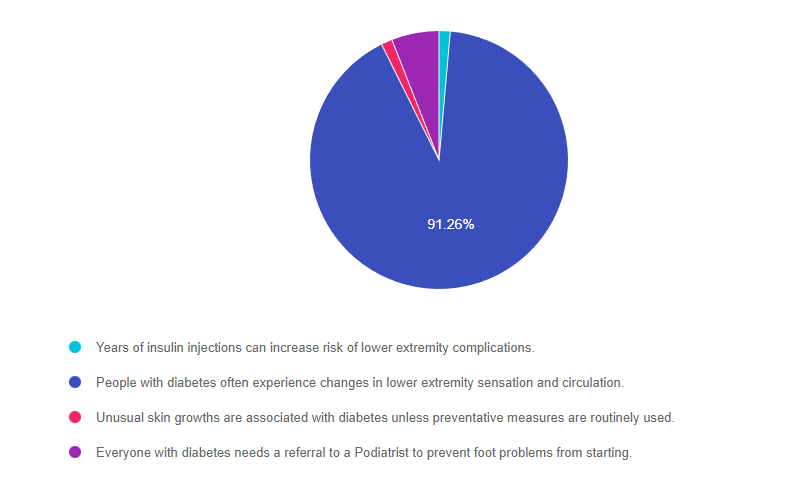
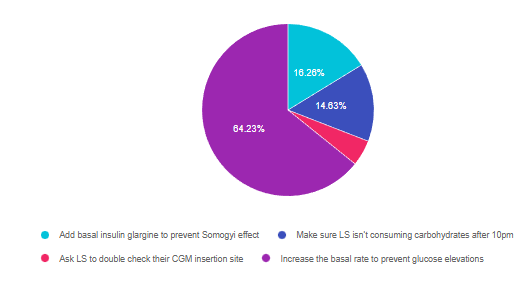
As shown above, the most common choice was option 2, the second most common answer was option 4, then a tie for options 1 and 3.
Getting to the Best Answer
Answer 1 is incorrect. 1.39% chose this answer, “Years of insulin injections can increase risk of lower extremity complications.” Insulin injections don’t increase the risk of lower extremity problems and they might even reduce the risk of vascular disease by improving blood glucose levels.
Answer 2 is correct. 91.29% of you chose this answer, “People with diabetes often experience changes in lower extremity sensation and circulation.” YES, GREAT JOB. Diabetes can contribute to increased risk of vessel disease and neuropathy if blood glucose levels and blood pressure readings are chronically above target. Of course, genetics and environment also play a role in increasing or decreasing the risk of lower extremity complications. By providing people with diabetes strategies to protect lower extremities and care for their feet, health care professionals make a big dent in improving outcomes. We have free patient education handouts that you are welcome to share with the clients you serve. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language and is also available in Spanish, Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Answer 3 is incorrect. 1.39% of respondents chose this answer, “Unusual skin growths are associated with diabetes unless preventative measures are routinely used.” People with diabetes are not at increased risk of skin growths, however they are at risk for fungal infections, especially if blood sugars are elevated. Keeping feet clean and dry, especially in between toes can help ward off infections and interdigit maceration. We have free patient education handouts that you are welcome to share with the clients you serve. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language and is also available in Spanish, Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos.
Finally, Answer 4 is incorrect. 5.92% chose this answer, “Everyone with diabetes needs a referral to a Podiatrist to prevent foot problems from starting.” A person with diabetes, well managed glucose levels, who can safely provide their own foot care does not need a referral to a Podiatrist. However, people with neuropathy, vascular disease, foot deformities, thick toenails, or a history of foot problems, usually benefit from being referred to a Podiatrist for assessment and care. You can download or free 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings.
Want to learn more about this question?
Enroll in our Foot Screening Bundle, now on Sale!
This bundle includes our 3 Steps to Save Feet; Assess, Screen, and Report Webinar + 20-pack of Monofilament + ADA Foot Screening Chart
People with diabetes are at increased risk of foot complications. Basic foot care education and intervention can reduce the risk of amputation by over 50 percent.
This bundle comes with our:
We have included instructions on assessing and inspecting feet, risk assessment, and action steps. We enhanced the teaching tools and forms from the Lower Extremity Prevention Program (LEAP) and are excited to share them with our community of diabetes advocates.
FREE Handouts and Resources
Read More: FREE Handouts and Resources 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. A person with diabetes has small corn on their pinky toe and it bothers them when walking. What is the best first action? Click Here to Test your Knowledge 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. We have created a Foot Care Toolkit! This toolkit includes a Handout on how to perform a 10-minute foot assessment, a patient education handout, plus a webinar detailing how to use these tools. Plus, we now offer discounted monofilaments that you can use in your practice setting. 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Webinar: Coach Beverly will walk participants through the 3 Step Process to Save Feet; Assess, Screen and Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment and action steps. We will share free teaching tools, strategies, and documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. No matter your profession, learning the basics of lower extremity assessment can help you to identify when people with diabetes are in jeopardy of serious foot problems. Basic foot care assessment and education can reduce the risk of amputation by over 50%. According to a 2019 article published in Diabetes Care, the rate of amputations in the U.S. is increasing. Each year, people with diabetes experience over 100,000 non-traumatic amputations. In the United States, every 17 seconds someone is diagnosed with diabetes, and every day 230 Americans with diabetes will suffer an amputation. There are also major health disparities in people at the highest risk of losing their lower extremities. African Americans are 4 times more likely to experience diabetes-related amputation than whites. If each one of us reading this article prevented ONE amputation, we could prevent 40, 000 amputations. By assessing and screening for feet at risk, including using a monofilament to detect loss of protective sensation, diabetes healthcare professionals can immediately identify high-risk feet and take steps to protect lower extremities. Learn how to take an active role in decreasing this devastating loss of limb and often life. For last week’s practice question, we quizzed test takers on the best use of monofilament to check feet. 60% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success! Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question Question: ADA Standards of Care recommend using a 5.07 monofilament to evaluate for loss of protective sensation in lower extremities in people with diabetes. Which of the following statements is most accurate regarding using a monofilament to assess lower extremities? Answer Choices: As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally 3. Answer 1 is correct. 60.00% chose this answer, “When using the monofilament, test above or below thickened or callused skin.” YES, GREAT JOB. Many people with diabetes have calluses and thickened skin that will block the sensation of 10gms of linear pressure delivered by the monofilament. For this reason, avoid areas with thickened insensate skin and test for sensation above or below the callused location. Answer 2 is incorrect. 11.27% of you chose this answer, “Be careful not to bend the monofilament when testing for sensation.” Actually, to deliver 10gms of linear pressure using a monofilament, the examiner needs to slightly bend the 5.07 filament into a “C” position. This will deliver the correct amount of pressure to evaluate if the person is experiencing loss of sensation. Answer 3 is incorrect. 4.13% of respondents chose this answer, “Alternate between hot and cold testing with monofilament testing to enhance accuracy.” Hot and cold testing is a strategy to determine if the person has decreased temperature sensation. However alternating between these two assessment techniques won’t enhance the testing accuracy of the monofilament. Finally, Answer 4 is incorrect. 24.60% chose this answer, “Rotate monofilament testing between the medial malleolus and distal phalanges for best results.” This is a juicy answer with some cool foot terms. The medial malleolus is actually the bump that protrudes on the inner ankle and the distal phalanges are the tips of the toes. The inner ankle is not one of the points of assessment using a monofilament. The large toe, the foot pad and heel are locations included in a foot assessment using a 5.07 monofilament. All health care professionals are invited to join us to learn strategies to protect lower extremities during this FREE Webinar. Coach Beverly will walk participants through the 3 Step Process to Save Feet; Assess, Screen and Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment and action steps. We will share free teaching tools, strategies, and documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. CEs: 1.0 CEs for $19 or No CEs for FREE Topics include: Read More: FREE Handouts and Resources 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes. People with diabetes are at increased risk of foot complications. By using a 5.07 monofilament (delivers 10gms of linear pressure) to assess for loss of sensation, diabetes health care professionals can immediately identify high-risk feet and take steps to protect lower extremities. Basic foot care education and intervention can reduce the risk of amputation by over 50 percent. We are excited to provide these single-use 5.07 monofilaments in packs of 20. We have included instructions on how to assess and inspect feet, along with risk assessment and action steps. We enhanced the teaching tools and forms from the Lower Extremity Prevention Program (LEAP) and are excited to share them with our community of diabetes advocates. Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. Download Course Flyer | Download Schedule If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan. Team of expert faculty includes: Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University. All hours earned count toward your CDCES Accreditation Information Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. Why is it important that people with diabetes pay special attention to taking care of their feet? Click Here to Test your Knowledge All health care professionals are invited to join us to learn strategies to protect lower extremities during this FREE Webinar. Coach Beverly will walk participants through the 3 Step Process to Save Feet; Assess, Screen and Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment and action steps. We will share free teaching tools, strategies, and documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. CEs: 1.0 CEs for $19 or No CEs for FREE Topics include: 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet – Steps to Healthy Feet. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Foot Care Teaching Sheet in Spanish– Pasos Para Tener Pies Sanos. This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes. People with diabetes are at increased risk of foot complications. By using a 5.07 monofilament (delivers 10gms of linear pressure) to assess for loss of sensation, diabetes health care professionals can immediately identify high-risk feet and take steps to protect lower extremities. Basic foot care education and intervention can reduce the risk of amputation by over 50 percent. We are excited to provide these single-use 5.07 monofilaments in packs of 20. We have included instructions on how to assess and inspect feet, along with risk assessment and action steps. We enhanced the teaching tools and forms from the Lower Extremity Prevention Program (LEAP) and are excited to share them with our community of diabetes advocates. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. July 2022 eNews | 3 Steps to”DeFeet” Amputations in People with Diabetes It’s officially summer. What better season to celebrate feet and lower extremities! My passion for lower extremity advocacy began with my work at Stanford Hospital over 25 years ago. A kind-hearted man was admitted to the vascular unit with an infected foot ulcer and osteomyelitis. Despite days of antibiotic therapy and wound care, a partial foot amputation was required. He was devastated by this loss and so was I. Here is the real tragedy. I am sure this amputation could have been prevented with some simple foot care education. For this newsletter issue, we have put together a toolkit full of foot care resources that we are excited to share with you, including a FREE Webinar on 3 Steps to Save Feet. Amputation rates are on the rise. We hope by sharing these tools and information, we reverse this trend and save limbs. The great thing about foot care education is that all health care professionals can engage in sharing the prevention strategies outlined in our free handouts. Just think of all the unnecessary suffering we can prevent by looking at feet, providing education, and taking action on any unusual foot findings. I think our foot care motto from Stanford Hospital says it best, “Lift the Sheets and Look at the Feets”. Let’s just start with this first step. We are also overjoyed to announce that we are providing two Flower Scholarships that cover the cost of our Fall Virtual DiabetesEd Course. Applications are now being accepted. Thank you in advance for your actions and advocacy on behalf of people living with diabetes. Beverly, Bryanna, Robert, and Amanda Featured Articles Upcoming FREE Webinars All health care professionals are invited to join us to learn strategies to protect lower extremities during this FREE Webinar. Coach Beverly will walk participants through the 3 Step Process to Save Feet; Assess, Screen and Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment and action steps. We will share free teaching tools, strategies, and documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. CEs: 1.0 CEs for $19 or No CEs for FREE Topics include: 3 Steps to Save Feet – Assess, Screen, Report Handout. This handout walks health care professionals through the steps involved in a 10-minute foot assessment and monofilament screening. Also includes a Screening Form to document and report findings. Foot Care Teaching Sheet: This handout covers the important elements of foot care for people living with diabetes with simple and straightforward language. Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES Author, Nurse, Educator, Clinician and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes. People with diabetes are at increased risk of foot complications. By using a 5.07 monofilament (delivers 10gms of linear pressure) to assess for loss of sensation, diabetes health care professionals can immediately identify high-risk feet and take steps to protect lower extremities. Basic foot care education and intervention can reduce the risk of amputation by over 50 percent. We are excited to provide these single-use 5.07 monofilaments in packs of 20. We have included instructions on how to assess and inspect feet, along with risk assessment and action steps. We enhanced the teaching tools and forms from the Lower Extremity Prevention Program (LEAP) and are excited to share them with our community of diabetes advocates. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. For last week’s practice question, we quizzed test takers on Mounjaro, a new medication. 82% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success! Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question Question: The FDA recently approved the new ‘twincretin” dual incretin hormone therapy called Tirzepatide (Mounjaro). The provider wants to start a person with type 2 diabetes on this new medication and asks for your consultation. The person’s current medications for type 2 diabetes include metformin, empagliflozin (Jardiance), semaglutide (Ozempic), and Pravachol. What is the best response to the provider? Answer Choices: As shown above, the most common choice was option 2, the second most common answer was option 4, then option 1, and finally 3. Answer 1 is incorrect. 6.53% chose this answer, “Inform provider that Tirzepatide (Mounjaro) is contraindicated in people taking SGLT-2 Inhibitors.” According to the Package Insert, Tirzepatide can be used in combination with SGLT-2 Inhibitors and other approved diabetes medications. However, since Tirzepatide is a combination of GLP-1 and GIP Incretins, it is not recommended to use in combination with a GLP-1 RA or the DPP-IV class of medications. Read more on our blog here. Answer 2 is correct. 82.13% of you chose this answer, “Recommend stopping the semaglutide (Ozempic) before starting the Tirzepatide (Mounjaro).” YES, GREAT JOB! Since Tirzepatide is a combination of GLP-1 and GIP Incretins, it is not recommended to use in combination with a GLP-1 RA or the DPP-IV class of medications. Answer 3 is incorrect. 4.12% of respondents chose this answer, “Reinforce the importance of prescribing a CGM before starting Tirzepatide (Mounjaro).” Since this person is not on insulin or any medications that would cause low blood sugar, a CGM is not required to monitor blood sugars. Blood glucose monitoring combined with regular A1C testing will be important to determine the efficacy of this new “twincretin”. Read more on our blog here. Finally, Answer 4 is incorrect. 7.22% chose this answer, “Request provider also prescribes Glucagon rescue med in case of severe hypoglycemia.” Since this person is not on insulin or any medications that would cause low blood sugar, a glucagon rescue med is not required to treat severe hypoglycemia. Blood glucose monitoring combined with regular A1C testing will be important to determine the efficacy of this new “twincretin”. Read more on our blog here. The FDA just approved a novel, dual incretin hormone therapy called Tirzepatide (Mounjaro). This new twin incretin injectable includes not only a GLP-1 Receptor Agonist, but also a Glucose-dependent insulinotropic polypeptide (GIP), which magnifies the therapeutic effectiveness. The SURPASS studies indicate that study participants experienced an A1C drop of up to 2.5% and weight loss of up to 10kg or more. Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. Download Course Flyer | Download Schedule If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan. Join us LIVE for this Virtual Course and enjoy a sense of community! Team of expert faculty includes: Deluxe Option for $499: Virtual Program includes: Deluxe Version includes Syllabus, Standards and Swag*: Basic Option for $399: Virtual Program includes: Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University. All hours earned count toward your CDCES Accreditation Information Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. For last week’s practice question, we quizzed test takers on the best blood sugar fix. 64% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success! Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question Question: LS wears an insulin pump and uses lispro insulin. LS has an average basal rate of 0.6 units and hour, a 1:15 carb ratio and a 1:50 correction ratio. Based on the ambulatory glucose profile, LS is experiencing elevated glucose levels from 4am to 7am. To get glucose to target, what is the best next step? Answer Choices: As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally 3. Answer 1 is incorrect. 16.26% chose this answer, “Add basal insulin glargine to prevent Somogyi effect.” Since LS uses an insulin pump, they don’t need to inject additional basal insulin (glargine) to get overnight blood sugars to target. With an insulin pump, the bolus insulin (lispro) acts as the basal insulin, delivering background insulin at 0.6 units an hour. In addition, Simogyi is defined as rebound hyperglycemia, or the sudden increase in blood sugars, due to stress hormones, after a significant hypoglycemic event. There is no symptoms in the question that indicate that LS is experiencing a Somogyi event. This is a juicy answer, but on closer inspection, not the best one. Answer 2 is incorrect. 14.63% of you chose this answer, “Make sure LS isn’t consuming carbohydrates after 10pm.” Based on the glucose profile, LS blood sugars are increasing around 4am, which is most likely due to the Dawn Phenomena, not late night snacking. In the middle of the night, the body starts releasing growth hormone cortisol, and catecholamines, which causes an increase in blood sugars around 4am for many people with type 1 diabetes. This is referred to as the Dawn Phenomena. The best way to manage this is to slightly increase basal rate during the period when blood sugar is on the rise. Answer 3 is incorrect. 4.88% of respondents chose this answer, “Ask LS to double check their CGM insertion site.” While it’s always good to check to make sure devices are working properly, this isn’t the case for this question. LS is having consistent glucose elevations from 4am to 7am, which is commonly referred to as the Dawn Phenomena. In the middle of the night, the body starts releasing growth hormone cortisol, and catecholamines, which causes an increase in blood sugars around 4am for many people with type 1 diabetes. The best way to manage this is to slightly increase basal rate during the period when blood sugar is on the rise. Finally, Answer 4 is correct. 64.23% chose this answer, “Increase the basal rate to prevent glucose elevations.” YES, GREAT JOB. LS is having consistent glucose elevations from 4am to 7am, which is commonly referred to as the Dawn Phenomena. In the middle of the night, the body starts releasing growth hormone cortisol, and catecholamines, which causes an increase in blood sugars around 4am for many people with type 1 diabetes. The best way to manage this is to slightly increase basal rate during the period when blood sugar is on the rise. Learn Test-Taking Secrets with Coach Bev – Option to add on 200+ Computerized Practice Test Questions for $49 During this webinar, Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test-taking tips based on her experience taking the certification exam six times. To provide plenty of practice, Coach Beverly will sample 20 test questions that have been plucked from our Test Taking Toolkit during this live webinar. She will explain how to dissect the question, eliminate wrong answers and avoid getting lured in by juicy answers. Includes a review of 20 sample test questions with test taking strategies. This includes access to the recorded version of this webinar on your Online University Student Portal. Plus, the Test Taking Toolkit provides you with over 200+ sample online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test-taking confidence. Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. Download Course Flyer | Download Schedule If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan. Join us LIVE for this Virtual Course and enjoy a sense of community! Team of expert faculty includes: Deluxe Option for $499: Virtual Program includes: Deluxe Version includes Syllabus, Standards and Swag*: Basic Option for $399: Virtual Program includes: Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University. All hours earned count toward your CDCES Accreditation Information Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. Question of the Week | Best action to treat a corn?

Want to learn more about this question?
Foot Screening Bundle – Purchase Now and save $15!3 Steps to Save Feet Webinar Airs live today, July 19th at 11:30 am PST
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.FREE Handouts and Resources

Foot Care Toolkit: A 3-Step Process to Save Feet
All health care professionals are invited to learn how to assess feet.
Foot Care Toolkit
Rationale of the Week | How to use a Monofilament to Check Feet

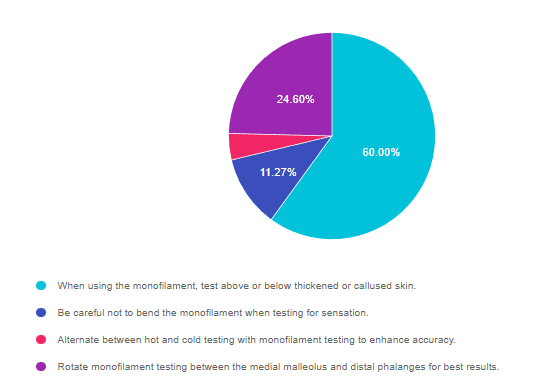
Getting to the Best Answer
Want to learn more about this question?
Join us for our new FREE Webinar
3 Steps to Save Feet; Assess, Screen, and ReportAirs live July 19th at 11:30 am PST (45 to 60 minutes)
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.FREE Handouts and Resources

NEW! Order Monofilament (5.07) for Diabetes Foot Screening 20-Pack

Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Specialist Conference
30+ CEsAirs October 12-14th, 2022

Join us LIVE for this Virtual Course and enjoy a sense of community!
Two Registration Options
Question of Week | Why is Diabetes Foot Care So Important?

Want to learn more about this question?
Join us for our new FREE Webinar
3 Steps to Save Feet; Assess, Screen, and ReportAirs live July 19th at 11:30 am PST (45 to 60 minutes)
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.FREE Handouts and Resources

NEW! Order Monofilament (5.07) for Diabetes Foot Screening 20-Pack

July 2022 eNews | 3 Steps to”DeFeet” Amputations in People with Diabetes

Happy July
Want to learn more about this question?
Join us for our new FREE Webinar
3 Steps to Save Feet; Assess, Screen, and ReportAirs live July 19th at 11:30 am PST (45 to 60 minutes)
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.FREE Handouts and Resources

NEW! Order Monofilament (5.07) for Diabetes Foot Screening 20-Pack

Rationale of the Week | Best advice on adding new med, Mounjaro

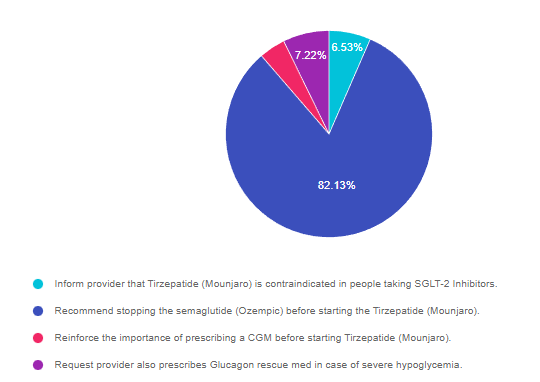
Getting to the Best Answer
Want to learn more about this question?
New Dual Incretin Injectable – “TwinCretin”

Want to learn more about Diabetes Care? View our
Virtual DiabetesEd Specialist Conference
30+ CEsAirs October 12-14th, 2022
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Rationale of the Week | Best blood sugar fix?

Getting to the Best Answer
Want to learn more about this question? Join us for our upcoming webinar
Test Taking Practice Exam Toolkit | FREE Webinar
Are You Ready for Exam Success?
Join us live Thursday, June 30th at 11:30 am PST
Two Ways to Join
Want to learn more about Diabetes Care? View our
Virtual DiabetesEd Specialist Conference
30+ CEsAirs October 12-14th, 2022
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs








