
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

For last week’s practice question, we quizzed test takers on glucose monitoring in the inpatient setting. 60% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JL is a new nursing graduate and asks you questions about glucose monitoring in the inpatient setting. Which of the following statements is most accurate regarding providing diabetes care in the hospital setting?
Answer Choices:
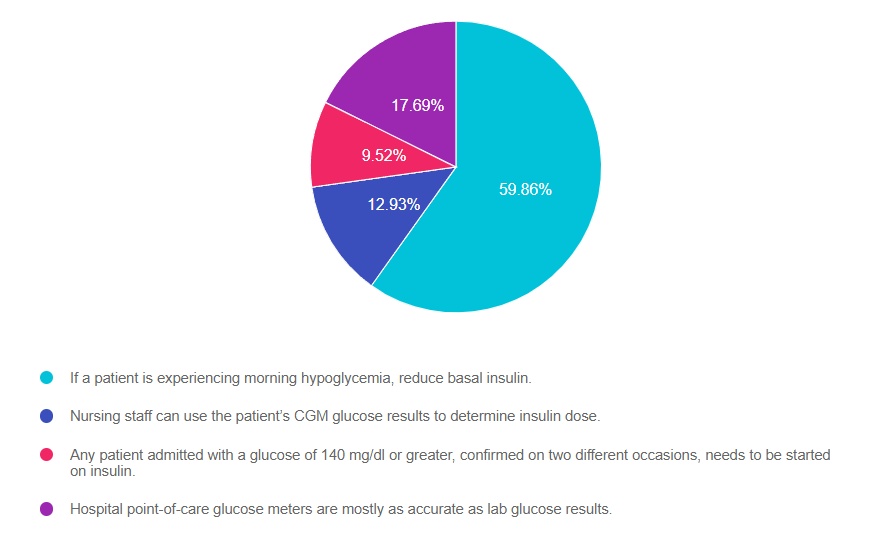
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 2, and finally 3.
Answer 1 is correct. 59.86% chose this answer, “If a patient is experiencing morning hypoglycemia, reduce basal insulin.” YES, GREAT JOB! During hospitalization, keeping glucose levels on target improves outcomes and decreases the length of stay. This includes preventing hypoglycemia, which can be life-threatening. The most common cause of morning hypoglycemia is basal insulin. Treating hypoglycemia rapidly with carbs and rechecking to make blood sugar is increasing is critical. However, to prevent future hypoglycemic events, determining the cause of the low blood sugar and taking corrective action is just as important. Reducing basal insulin by 20% or more when morning blood sugars are less than 100 mg/dL in the hospital setting makes a big difference in protecting against hypoglycemia.
Answer 2 is incorrect. 12.93% of you chose this answer, “Nursing staff can use the patient’s CGM glucose results to determine insulin dose.” This is a juicy answer, however, the FDA has not approved the dosing of insulin based on CGM results in the hospital setting. Inpatients with adequate cognition are allowed to use their CGM to monitor their blood sugar and keep an eye on trends based on the hospital’s policy. However, insulin dosing is based on the hospital-approved point-of-care glucose meter results.
Answer 3 is incorrect. 9.52% of respondents chose this answer, “Any patient admitted with a glucose of 140 mg/dl or greater, confirmed on two different occasions, needs to be started on insulin.” If a person is admitted with a glucose of 140 or greater, this would certainly catch our attention and require ongoing monitoring. They may have undiagnosed prediabetes or diabetes (depending on if the glucose was fasting or random). However, this glucose level of 140 does not meet the criteria to start insulin. According to the ADA Standards, insulin therapy is initiated when the admitting glucose is 180 or greater.
Finally, Answer 4 is incorrect. 17.69% chose this answer, “Hospital point-of-care glucose meters are mostly as accurate as lab glucose results.” This is another juicy answer. The lab glucose is the most accurate. Approved hospital glucose meters can read 15% higher or lower than the actual lab glucose. At home glucose meters, can be up read up to 20% higher or lower than lab glucose and still be within FDA approval parameters. For more info, see our blog, How Accurate are Glucose Meters?
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control and outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest ADA Standards and provide links to resources and inpatient management templates.
Objectives:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
As a Diabetes Specialist at a local Native Health Services Clinic, I assess a lot of feet every day. I believe this simple act of looking, touching, questioning, caring, and referring has saved many lower extremities.
Last month, a client arrived who was excited to report that they were able to walk for over an hour without getting short of breath. We celebrated this accomplishment and then I asked them to take off his shoes, knowing this person had already lost all of the toes on their left foot due to diabetes. The client wasn’t wearing custom shoes to accommodate this foot, just regular tennis shoes.
When the socks came off, I discovered an angry-looking ulcer that the person wasn’t too concerned about, saying, “it’s not really bothering me.” We sent this client to the emergency department, and they were immediately started on antibiotics to stop this very dangerous infection.
That’s just one example of how the simple act of assessing feet at during a wellness visit can make a big difference in outcomes.
A study conducted by researchers at the University of Virginia School of Medicine reviewed data on the impact of Wellness Visits on amputation rates in the “Diabetes Belt”.
The “Diabetes Belt,” refers to 644 counties in the southeastern and Appalachian regions of the U.S. with higher rates of diabetes including the state of Mississippi as well as portions of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, North Carolina, Ohio, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and West Virginia.
People living in the Diabetes Belt had 27% greater odds of requiring a lower-extremity amputation compared to residents of counties surrounding the belt.
This ten-year study at the University of Virginia found that people with diabetes who participated in a free Annual Wellness Visit covered by Medicare were 36% less likely to need an amputation compared to those who did not attend an Annual Wellness Visit regardless of where they lived.
“Our results confirmed our hypothesis that Annual Wellness Visits are associated with a reduced risk of major lower-extremity amputations, highlighting the importance of connecting patients to preventive care services,” said Jennifer Lobo, PhD, a researcher in UVA’s Department of Public Health Sciences.
The research also revealed significantly higher rates of diabetes-related amputations among Black participants compared with non-Hispanic White participants, both inside and outside the Diabetes Belt.
Based on these research results, more resources and changes in our health care system are needed to decrease amputation rates in the Diabetes Belt. As health care providers, we can take an active role in reaching out to Black community members to determine systemic barriers. Then, through community collaboration, we can start building bridges to improve inclusivity and access to healthcare.
To learn more about addressing racial disparities to reduce amputation, click here and click here.
The researchers concluded that people with diabetes who participated in their Annual Medicare Wellness Visit may have had their foot complications diagnosed sooner, helping prevent amputations. Also, given the effectiveness of wellness visits to prevent future problems, the authors suggest incentivizing people with Medicare to use their annual wellness visits to evaluate lower extremities and provide education and foot care training.

AR has type 1 diabetes and is in shock because they just discovered they are 6 weeks pregnant. AR uses a CGM and insulin pump to manage their diabetes and their most recent A1C is 8.3%. Which of the following is a potential complication associated with hyperglycemia during the first 10 weeks of pregnancy?
Click Here to Test your Knowledge

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, and understanding. This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Objectives:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed test takers on pregnancy and diabetes. 63% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR says they just found out they are pregnant. AR has type 2 diabetes and polycystic ovary syndrome and takes metformin 1000mg BID, semaglutide (Ozempic) 1.0mg weekly, and 30 units glargine insulin for diabetes management. Her most recent A1C was 8.2%. What is the most important action to take?
Answer Choices:
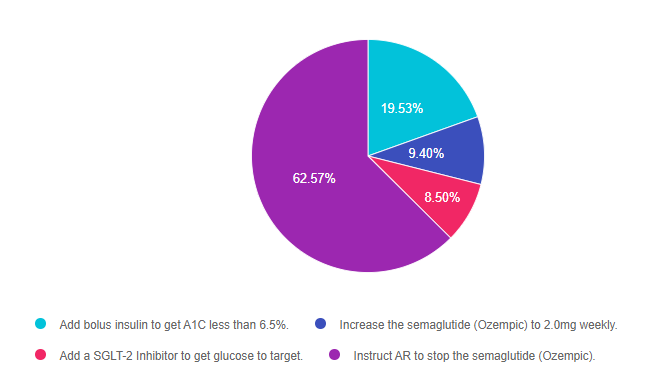
As shown above, the most common choice was option 4, the second most common answer was option 1, then option 2, and finally 3.
Answer 1 is incorrect. 19.53% chose this answer, “Add bolus insulin to get A1C less than 6.5%.” This answer is accurate, but it is not the best answer. The A1C goal during pregnancy is less than 6.5% and in this case, AR will need to manage their diabetes using basal bolus insulin therapy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 2 is incorrect. 9.40% of you chose this answer, “Increase the semaglutide (Ozempic) to 2.0mg weekly.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA.
Answer 3 is incorrect. 8.50% of respondents chose this answer, “Add a SGLT-2 Inhibitor to get glucose to target.” AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Insulin is safe during pregnancy. However, SGLT-2s are not approved for pregnancy and the GLP-1 RA, semaglutide would also need to be discontinued.
Finally, Answer 4 is correct. 62.57% chose this answer, “Instruct AR to stop the semaglutide (Ozempic).” YES, GREAT JOB! AR’s blood glucose levels are above the A1C pregnancy target of 6.5%, which means insulin intensification is needed. Basal bolus insulin therapy is safe during pregnancy. However, since semaglutide is not approved for pregnancy, the most important action is to stop the administration of this GLP-1 RA. Metformin can be continued through the first trimester and the insulin would need to be intensified to get A1C to target.

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, and understanding. This course reviews those special needs while focusing on Gestational Diabetes and Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, and prevention of complications during pregnancy. A helpful review for the CDCES Exam and for those who want more information on people who are pregnant and live with Diabetes.
Objectives:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

JL is a new nursing graduate and asks you questions about glucose monitoring in the inpatient setting. Which of the following statements is most accurate regarding providing diabetes care in the hospital setting?
Click Here to Test your Knowledge
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control and outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest ADA Standards and provide links to resources and inpatient management templates.
Objectives:
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Research clearly demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control and outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest ADA Standards and provide links to resources and inpatient management templates.
Objectives:
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM 
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
The injectable GLP-1 semaglutide (Ozempic) can now be dosed up to 2.0mg a week. This higher maximum dose provides greater reductions in body weight (6.9kgs vs 6.0kgs) and A1c (2.2 vs 1.9% ) when compared to 1.0 semaglutide dose. There was a comparable safety profile with both doses. However, more people experienced negative gastrointestinal side effects when receiving the higher dose (34% compared to 30.8%).
This is good news for people with type 2 diabetes who would like to benefit from both A1C and weight reduction. Plus, semaglutide lowers the risk of cardiovascular events.
Without insurance coverage, this medication costs about $1000 for a month’s supply. However, since semaglutide (Ozempic) is an established diabetes medication covered by many insurance plans, we are hopeful that people who would benefit from this therapy will have access to this higher dose.
The SUSTAIN FORTE trial lasted for 40-weeks and enrolled 961 patients with type 2 diabetes with an A1C of 8.0-10.0%. All patients in the trial initiated treatment with a 0.25 mg dose of semaglutide that was doubled every 4 weeks until the target dose was achieved.
In addition to reduction in A1C and body weight, the semaglutide 2.0 mg arm of the trial saw a greater proportion of patients achieve an A1C less than 7% (67.6% vs 57.5% [OR, 1.60; 95% CI, 1.21-2.13; P=.001]) or a body weight reduction greater than 5% (59.2% vs 51.3% [OR, 1.41; 95% CI, 1.08-1.84]) than the semaglutide 1.0 mg arm.
We have updated our Diabetes Medication PocketCard with this higher maximum dose or our website, CDCES Coach App, and printed PocketCards.
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
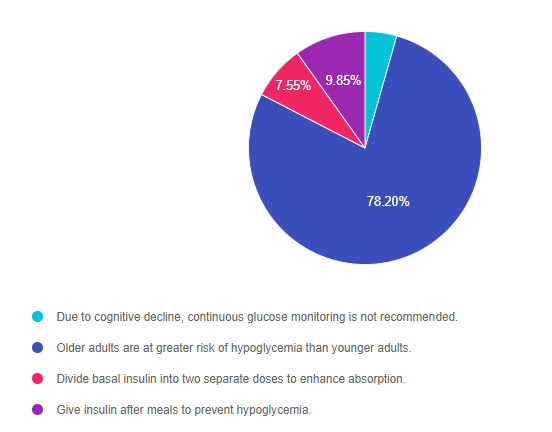
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.“ Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company. For last week’s practice question, we quizzed test takers on if insulin is safe for older adults. 78% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success! Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question Question: For older adults with diabetes using insulin therapy, which of the following is the most accurate statement? Answer Choices: As shown above, the most common choice was option 2, the second most common answer was option 4, then option 3, and finally 1. Answer 1 is incorrect. 4.40% chose this answer, “Due to cognitive decline, continuous glucose monitoring is not recommended for older adults.” Many older adults on intensive insulin therapy with a history of hypoglycemia can benefit from CGM technology to prevent low blood sugars and fine tune carb intake and insulin dosing. Each older adult needs a individualized assessment to determine if a CGM is right for them. The rate of cognitive decline is complex and is a result of genetics, other chronic conditions and overall health combined with aging. Answer 2 is correct. 78.20% of you chose this answer, “Older adults are at greater risk of hypoglycemia than younger adults. GREAT JOB, almost 80% of you chose this best answer. As people with diabetes age, they are at higher risk for low blood sugars for many reasons, especially if they are taking insulin or a secretagogue. Older individuals may have diminished renal function, which increases the duration of the action of insulin and secretagogues. Some can experience lower calorie intake due to decreasing appetite, trouble chewing, lack of resources, forgetfulness or depression and feelings of isolation. Others may have difficulty administering their insulin or medications accurately or may forget to eat after injections. For this reason, the ADA Standards recommends that older adults are assessed for hypoglycemia risk at each visit coupled with problem solving as needed. Answer 3 is incorrect. 7.55% of respondents chose this answer, “Divide basal insulin into two separate doses to enhance absorption.” This is a juicy answer. For older adults at risk for hypoglycemia, the ADA does recommend scheduling the basal insulin for the morning instead of evening. Finally, Answer 4 is incorrect. 9.85% chose this answer, “Give insulin after meals to prevent hypoglycemia.” Another juicy answer. This answer implies that all older people should take their insulin after meals. Some individuals might benefit from post-meal insulin, especially if they are not sure how much they are going to eat and they have a history of hypoglycemia. However, insulin works best when given before the meal so it peaks at the same time the post meal glucose is peaking. This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.” Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company. Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. 
Why become a CDCES?
Three Reasons from Coach Beverly Rationale of the Week | Insulin safe for older adults?

Getting to the Best Answer
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
What is a Certified Diabetes Care and Education Specialist?

Why become a CDCES?
Three Reasons from Coach Beverly