
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

According to a NIH systematic literature review, there is clear evidence that diabetes and climate change are interconnected. Which of the following situations are due to the impact of a changing climate?
Click Here to Test your Knowledge
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
Deluxe Option for $499: Virtual Program includes:
Deluxe Version includes Syllabus, Standards and Swag*:
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Research published in The Lancet Diabetes & Endocrinology this month confirmed the same findings as a growing number of studies. COVID-19 increases a person’s risk of diabetes, even months after being infected.
In this latest robust study, researchers reviewed the medical records of over 180,000 US Veterans who survived the first 30 days of COVID-19 infection between March 2020 and September 2021 and compared them with 2 large control groups—a contemporary cohort of more than 4.1 million non-infected participants who used VA services during the same time period and a historical cohort of another 4.28 million non-infected participants who used VA services during 2017.

Over 40% of study participants infected with COVID-19 were more likely to develop diabetes or be prescribed diabetes medication within a year compared to the control group. Simply translated, 2 in 100 COVID-19 patients were more likely to develop diabetes than those who did not get infected.
People older than 65 years and those with cardiovascular disease, high blood pressure, high cholesterol, or prediabetes had a higher risk of diabetes than younger individuals or those without underlying conditions. Additionally, Black participants had higher risks of developing diabetes than White participants.
Most of the post-COVID diabetes cases (over 99%) developed type 2 diabetes. In addition, the severity of the COVID-19 infection impacted the risk. People with COVID-19 admitted to intensive had the highest risk of developing develop diabetes, compared to those not infected.
Some limitations of the study include that the findings may not translate to other populations, since the US Veterans study group consisted of mostly older white men, many of whom had risk factors for diabetes, including hypertension and extra weight. The risk of getting diabetes post-COVID-19 seems to be much lower in younger people. Another limitation is that some people in the control group might have had an asymptomatic missed COVID-19 diagnosis.
These startling findings have significant implications for the 80 million people in the U.S. known to be infected with COVID-19, especially for people living with long-haul covid.
People who have experienced a COVID-19 infection need to know the symptoms of hyperglycemia and be encouraged to report suspicions of diabetes symptoms to their providers right away. In addition, regular glucose testing of people who were infected with COVID-19 may now be recommended to detect those who may not be aware of the signs of diabetes.
Now, more than ever, we need to increase access to Diabetes Prevention Programs and Diabetes Self-Management Education, to make sure this expanding population of people with new diabetes gets the information they need to successfully manage glucose levels and maintain optimal quality of life.
For more information:
Washington Post Article and The Lancet Diabetes & Endocrinology
This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking certification exams or considering setting up a DSME program, this program is designed for you. We highlight the newly revised and simplified 2022 Standards and provide strategies on program implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Download Course Schedule | Download Course Flyer
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
Download Course Schedule | Download Course Flyer
Deluxe Option for $449: Virtual Program includes:
Deluxe Version includes Syllabus, Standards and Swag*:
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

For last week’s practice question, we quizzed test takers on which produce has the most pesticide residue. 82% of respondents chose the best answer, GREAT JOB. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: Each year, the Environmental Working Group (EWG) publishes the Shopper’s Guide to Pesticides in Produce™, which ranks the pesticide contamination of 46 popular fruits and vegetables based on test results by the Department of Agriculture and the Food and Drug Administration of around 45,000 samples of produce. Based on their 2022 analysis, which three fruits and vegetables listed are included in the “dirty dozen” (produce that is highest in pesticide residue)?
Answer Choices:
A. Strawberries, tomatoes, pears
B. Kale, asparagus, mangoes
C. Avocados, onions, sweet corn
D. Sweet potatoes, watermelon, cherries
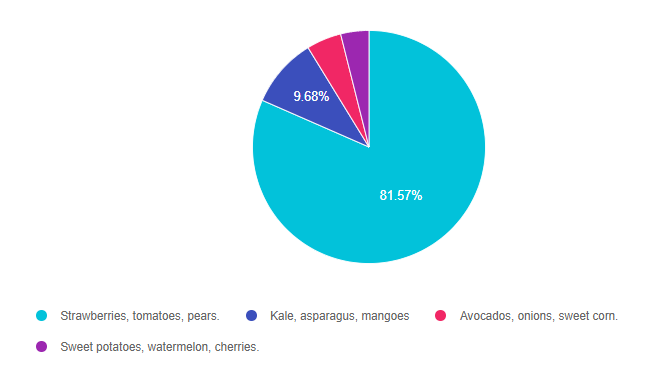
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 3, and finally 2.
Answer 1 is correct. 81.57% chose this answer, “Strawberries, tomatoes, pears.” YES, this is the best answer. The complete list of fruits and vegetables with the highest pesticide levels include:
These fruits and veggies are still healthy choices since they are packed with fiber and phytonutrients. However, given their higher amount of pesticide, try to purchase from the Organic Section of your local store or farmer’s market.

Answer 2 is incorrect. 9.68% of you chose this answer, “Kale, asparagus, mangoes.” Kale is included on the dirty dozen list, while asparagus and mangoes are part of the Clean 15.
Answer 3 is incorrect. 4.84% of respondents chose this answer, “Avocados, onions, sweet corn.” All of these vegetables and fruits have the lowest amount of pesticide and a part of the Clean 15.
These Clean 15 healthy fruits and veggies are safe to purchase in the non-organic or organic section. It’s always a good idea to wash fruit and veggies before eating.
Finally, Answer 4 is incorrect. 3.92% chose this answer, “Sweet potatoes, watermelon, cherries.” Sweet potatoes and watermelon are part of the Clean 15 while cherries are included in the dirty dozen.
Please visit the Environmental Working Groups Web page here
Dirty Dozen List
Clean 15 List
Info on how this list is created each year
We hope you appreciate this week’s rationale!

Free PocketCard and Wildflower Seed Postcard
We have created a list of 10 Actions to Celebrate Earth Day and printed these actions on wildflower seed postcards, that are ready for planting. To thank you for your pledge to commit to one or more actions that invest in the well-being of our planet, we will mail you a Free PocketCard and Wildflower Seed PostCard.
It’s easy! Just pick your action(s) on this survey and provide a mailing address where to send these gifts of appreciation. Each action, no matter how small, matters.
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
Deluxe Option for $449: Virtual Program includes:
Deluxe Version includes Syllabus, Standards and Swag*:
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

JR’s mom has type 1 diabetes and JR’s dad has type 2 diabetes. JR is 21 years old and in the emergency room with a glucose of 482 mg/dl. Besides checking glucose, ketones and A1C levels, which of the following lab test can be used to determine if someone has autoimmune diabetes?
Click Here to Test your Knowledge
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
Deluxe Option for $499: Virtual Program includes:
Deluxe Version includes Syllabus, Standards and Swag*:
Deluxe Option for $499: Virtual Program includes:
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Like me, you might feel overwhelmed and powerless with all the news about global warming, habitat loss and planetary suffering.
There is HOPE. After listening to many experts, I have come to the conclusion that our actions CAN MAKE A DIFFERENCE, no matter how small. As a diabetes specialist, I also know that rates of diabetes have increased dramatically over the past 20 years as the microbial diversity of humans (and the planet) is in sharp decline.
I am acutely aware that the health of our people is inextricably linked to the health of our planet.
As a diabetes leader and CEO, I have a tremendous opportunity and obligation to speak up and support my community in making positive changes to promote the well-being of humans and our planet.
We came up with a list of 10 Simple Steps we can take to improve planetary health. I am committing to making all 10 of these changes in my personal and professional life, starting today.
Change isn’t easy. We aren’t going for perfect, we are starting with intention and slowly moving to action, giving ourselves lots of grace along the way. I am excited to share my successes and wrong turns with you on this journey and we would love to hear from you too!
In celebration of Earth Day, we are excited to highlight the importance of plants and their role in supporting wildlife. The biggest secret to success is choosing Native Plants for your outdoor pots, balcony, yard or garden this year.
By choosing plants that originated from your geographic area, you help support your regional ecosystem and offer pollinators, birds, butterflies and other healthy critters needed food, pollen and building materials for their survival.
Read more on our blog, Earth Day Secrets to Improving Planet Health
Stay tuned and we share details and resources on each of these 10 Steps over the next few months. And, please send us your stories too at [email protected]. We want to hear from you!
We came up with a list of 10 simple steps you can take to improve planetary health. Just pick your action(s) on this survey or come up with your own, and we will send you two gifts of appreciation, for free.
To thank you for taking action, we will mail you (while supplies last) our world-famous Medication PocketCard and a Wildflower Seed Post Card, complete with 10 simple action steps printed on it, that you can read, review and then plant.
Like you, I have a deep appreciation for all the earth has given me and I want to give back to this beautiful blue planet. Each intention and action matters.
We are excited to celebrate Earth Day on April 22 and everyday. We will be posting blogs and resources to expand on actions we can all take to protect this precious earth we have the privilege to live on.
Each action, no matter how small, matters. We can do this!
With wishes for improved planetary health,
Beverly, Bryanna, Jackson, and Amanda
We have a favor to ask.
In celebration of Earth Day, could you commit to taking just one action to protect the planet? We made it super easy and came up with a list of 10 simple steps you can take to improve planetary health. Just pick your action(s) on this survey or come up with your own, and we will send you two gifts of appreciation, for free.
To thank you for taking action, we will mail you our world-famous Medication PocketCard and a Wildflower Seed Post Card, complete with 10 simple action steps printed on it, that you can read, review and then plant.
The health of our people is inextricably linked to the health of our planet.
Like you, I have a deep appreciation for all the earth has given me and I want to give back to this beautiful blue planet. Each intention and action matters.
We are excited to celebrate Earth Day on April 22 and everyday. We will be posting blogs and resources to expand on actions we can all take to protect this precious earth we have the privilege to live on.
Free PocketCard and Wildflower Seed Postcard
We have created a list of 10 Actions to Celebrate Earth Day and printed these actions on wildflower seed postcards, that are ready for planting. To thank you for your pledge to commit to one or more actions that invest in the well-being of our planet, we will mail you a Free Medication PocketCard and Wildflower Seed PostCard.
It’s easy! Just pick your action(s) on this Earth Action survey and provide a mailing address where to send these gifts of appreciation. Each action, no matter how small, matters. We can do this!
With wishes for improved planetary health,
Beverly, Bryanna, Jackson, and Amanda
We have a favor to ask.
In celebration of Earth Day, could you commit to taking just one action to protect the planet? We made it super easy and came up with a list of 10 simple steps you can take to improve planetary health. Just pick your action(s) on this survey or come up with your own, and we will send you two gifts of appreciation, for free.
To thank you for taking action, we will mail you our world-famous Medication PocketCard and a Wildflower Seed Post Card, complete with 10 simple action steps printed on it, that you can read, review and then plant.
The health of our people is inextricably linked to the health of our planet.
Like you, I have a deep appreciation for all the earth has given me and I want to give back to this beautiful blue planet. Each intention and action matters.
We are excited to celebrate Earth Day on April 22 and everyday. We will be posting blogs and resources to expand on actions we can all take to protect this precious earth we have the privilege to live on.
Free PocketCard and Wildflower Seed Postcard
We have created a list of 10 Actions to Celebrate Earth Day and printed these actions on wildflower seed postcards, that are ready for planting. To thank you for your pledge to commit to one or more actions that invest in the well-being of our planet, we will mail you a Free Medication PocketCard and Wildflower Seed PostCard.
It’s easy! Just pick your action(s) on this Earth Action survey and provide a mailing address where to send these gifts of appreciation. Each action, no matter how small, matters. We can do this!
With wishes for improved planetary health,
Beverly, Bryanna, Jackson, and Amanda

For last week’s practice question, we quizzed test takers on the link between oral health & hyperglycemia. 73% of respondents chose the best answer. We want to share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: Diabetes is associated with an increased risk of oral disease. Which of the following statements is true regarding people living with diabetes and hyperglycemia?
Answer Choices:
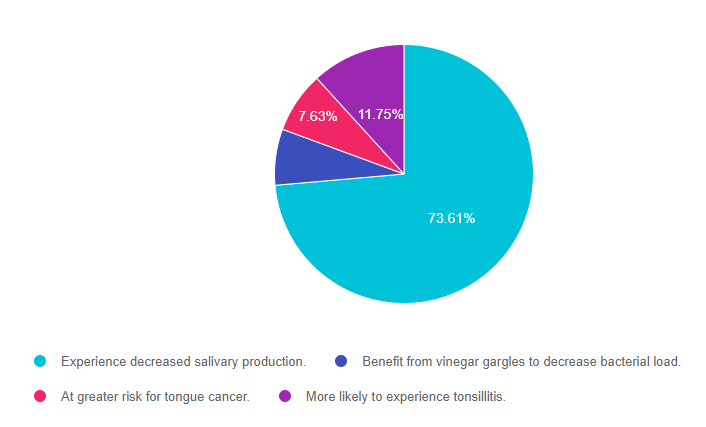
As shown above, the most common choice was option 1, the second most common answer was option 4, then option 3, and finally 2.
Answer 1 is correct. 73.61% chose this answer, “Experience decreased salivary production.” YES, GREAT JOB, this is the best answer. When a person is experiencing hyperglycemia, this leads to dehydration due to the chronic diuresis. When dehydrated, people with hyperglycemia produce less saliva and they saliva they do produce is laden with glucose. These 2 factors contribute to a higher risk of dental caries and can make mastication more difficult. There are products to increase salivary production, but the best treatment is to improve blood glucose levels.
Answer 2 is incorrect. 7.01% of you chose this answer, “Benefit from vinegar gargles to decrease the bacterial load.” Actually, gargling with vinegar can be harmful to your mouth if it is dry. Without the proper amount of saliva, the acid can break down enamel and decrease ability to fight off infection. There are products to increase salivary production, but the best treatment is to improve blood glucose levels.
Answer 3 is incorrect. 7.63% of respondents chose this answer, “At greater risk for oral cancers.” People with diabetes and chronic hyperglycemia have a higher risk for oral carries, gingivitis and periodontitis due to increased levels of sugar in the saliva that supports bacterial growth. However, do not have an increased risk of oral cancers.
Finally, Answer 4 is incorrect. 11.75% chose this answer, “More likely to experience tonsillitis.” People with diabetes and chronic hyperglycemia have a higher risk for oral carries, gingivitis and periodontitis due to increased levels of sugar in the saliva that supports bacterial growth. However, do not have an increased risk of tonsillitis.
More information from the American Dental Association.
We hope you appreciate this week’s rationale!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Join us LIVE for this Virtual Course and enjoy a sense of community!
Team of expert faculty includes:
Deluxe Option for $499: Virtual Program includes:
Deluxe Version includes Syllabus, Standards and Swag*:
Deluxe Option for $499: Virtual Program includes:
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.