Question of Week | Can diabetes impact sexual health?

JR is a 33-year-old who is non-binary and was recently diagnosed with type 2 diabetes. During your assessment, JR asks if diabetes can affect their sexual health.
What is the best response?
- That is a complicated question that is best discussed with your provider
- Here is a pamphlet on LGBTQ issues and sexuality that explains the most frequently asked questions.
- According to the data, there is a higher rate of erectile dysfunction in people living with diabetes.
- There is a relationship between elevated blood sugars and sexual health.
Click here to test your knowledge!
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Intensive Insulin Therapy with A1c 6.2%

Our September 21st Question of the week quizzed test takers on Intensive Insulin Therapy with A1c 6.2%. Three quarters (74%) of respondents, chose the best answer. We are excited to share info so you can pass on correct info to people living with diabetes and your colleagues.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: HR is a 78-year-old with a stroke and limited cognition with diabetes for 8 years and is on intensive insulin therapy: HR takes bolus insulin at meals and basaglar at night. HR has an A1c is 6.2% and employs a part time caretaker.
What is the best response in this situation?
Answer Choices:
- Start HR on an insulin pump and CGM to prevent hypoglycemia.
- Discuss de-intensifying insulin regimen.
- Using a strength-based approach, reinforce the importance of keeping the A1c less than 7%.
- Evaluate for diabetes related distress.
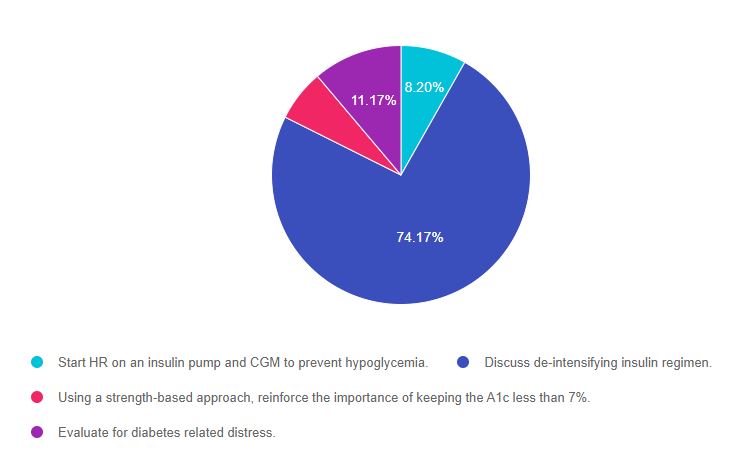
As shown above, the most common choice was option 2, the second most common answer was option 4, then option 1, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know the goals of care and considerations for people with diabetes across the lifespan. This practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 8.20% chose this answer, “Start HR on an insulin pump and CGM to prevent hypoglycemia.” This is not the best answer because we want to provide person-centered care based on the unique situation of this individual. HR has a history of a stroke, limited cognition and relies on a part time caregiver. It doesn’t seem realistic to provide pump and CGM training to HR given the cognitive limitations and the caregiver is only part-time. It is unlikely that the two of them would be comfortable enough or have the skill level to help oversee this complex technology and changing insertion sites.
Answer 2 is correct. 74.17% of you chose this answer, “Discuss de-intensifying insulin regimen.” YES. This is the best answer. Since HR is on multiple daily injections and has an A1c in the low 6% range, we know they are most likely experiencing episodes of hypoglycemia. To address this, we would need to discuss goals of care with HR and their caregivers and share our concerns about the risk and danger of hypoglycemia. We need to de-intensify this management plan. Based on the outcome of the discussion with HR, this could be accomplished by: reducing the overall insulin dose, switching to twice a day 70/30 insulin, or evaluating if oral medications could be trialed to reduce the need for insulin.
Answer 3 is incorrect. 6.46% of respondents chose this answer, “Using a strength-based approach, reinforce the importance of keeping the A1c less than 7%.” Using a strength-based approach is always a good idea, but the main issue in this question is that HR’s A1c is only 6.2%. According to the ADA Standards of Care, the A1c target in this situation would be individualized based on safety considerations, quality of life, and the goals and values of the person living with diabetes. For older, frail individuals at risk of hypoglycemia, a safer A1c target would be 7% – 8%.
Finally, Answer 4 is incorrect. 11.17% chose this answer, “Evaluate for diabetes-related distress.” Even though it is always important to consider people’s emotional response to diabetes, this answer does not address the key issue presented in this question. The first priority would be to make sure HR is safe, with a reduced risk of hypoglycemia and a realistic insulin regimen.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Best strategy to Prevent Hypo in Hospital?

As a diabetes specialist at a local hospital, one of your quality improvement goals is to prevent nocturnal hypoglycemia.
Which of the of following policy changes would most likely lower rates of overnight and morning hypoglycemia?
- Make sure the medication carts are stocked with glucagon rescue kits.
- Eliminate insulin sliding scale and encourage basal insulin therapy.
- Collaborate with dietary to make sure all people with diabetes get protein plus carb snack.
- Implement a plan to decrease basal insulin dose if morning glucose is less than 100 mg/dl.
Click here to test your knowledge!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
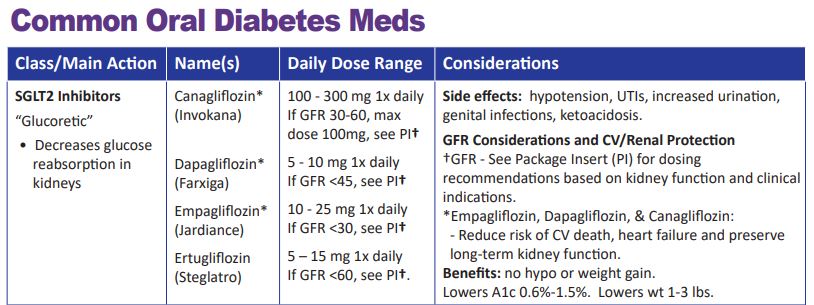
Concentrated Insulin and GFR Guidelines for SGLT2s
Did you know that Toujeo U-300 insulin pens are good for 56 days once opened? And that the max dose for Tresiba U-200 FlexTouch Pen is 160 units?
For our latest version of our printed PocketCards, we now include the number of pens in a box, max injection dose, total insulin amount per pen, and shelf life on the Concentrated Insulin Card. We also added Lyumjev KwikPen u200 insulin.
When determining the best insulin for people taking concentrated insulins, shelf life, max dosing, and total units of insulin in each device are important considerations.
We have also updated the GFR parameters for SGLT2 Inhibitors. This class of medication not only substantially lowers blood glucose but also has a profound impact on renal protection.
As more trial data become available, the GFR cutoff levels may change, so periodically refer to the package insert (PI) or our DES electronic pocket care version, for the most up-to-date information.
We update the printed version of our PocketCard once or twice a year.
We update our electronic PocketCard on an ongoing basis.
Fortunately, we can immediately update our electronic version of the PocketCard on our website and CDCES Coach App to reflect the latest medication recommendations and guidelines. In the electronic version, we also include that the GLP-1 Exenatide (Bydureon) is now approved for peds, age 10 and older and the GFR cut-off for empagliflozin is now approved for a GFR 30 or greater (please see package insert for details).
Preparing for the BC-ADM Exam Free Webinar – What you need to know

Becoming Board Certified in Advanced Diabetes Management (BC-ADM) provides an opportunity for diabetes specialists with an advanced degree in their field (plus a professional license as an advanced practice nurse, registered dietitian, registered pharmacist, or provider) to increase the breadth and depth of their diabetes knowledge. The scope of advanced diabetes practice includes management skills such as medication adjustment, medical nutrition therapy, exercise planning, counseling for behavior management, and psychosocial issues.
Attaining optimal diabetes management includes using a person-centered approach coupled with assessment, screening, management, and monitoring of acute and chronic diabetes co conditions. This webinar will review changes in requirements for this year’s exam eligibility and test format, strategies to succeed along with a review of study tips and test-taking tactics. We will review sample test questions and the reasoning behind choosing the right answers. We hope you can join us for this webinar.
See Full Calendar for upcoming webinars and Training Conferences.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | What Teaching Tip for New Med – finerenone?

Our September 14th Question of the week quizzed test takers on a new med. Less than half, 47% of respondents, chose the correct answer. This was a hard question since this finerenone was only recently FDA approved. We are excited to share info about this med along to you, so you can pass on correct info to people living with diabetes and kidney disease.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR has a GFR of 43 and lives with type 2 diabetes. JR excitedly brings you an article that talks about finerenone (Kerendia), a newly approved non-steroidal mineralocorticoid receptor antagonist which is indicated for people with chronic kidney disease (CKD) associated with Type 2 diabetes.
If JR is started on this medication, what instruction would you provide?
Answer Choices:
- Make sure to take this medication on an empty stomach
- Contact the provider if you notice ankle swelling
- Notify your provider if you experience a non-productive cough
- Avoid taking medication with grapefruit or grapefruit juice.
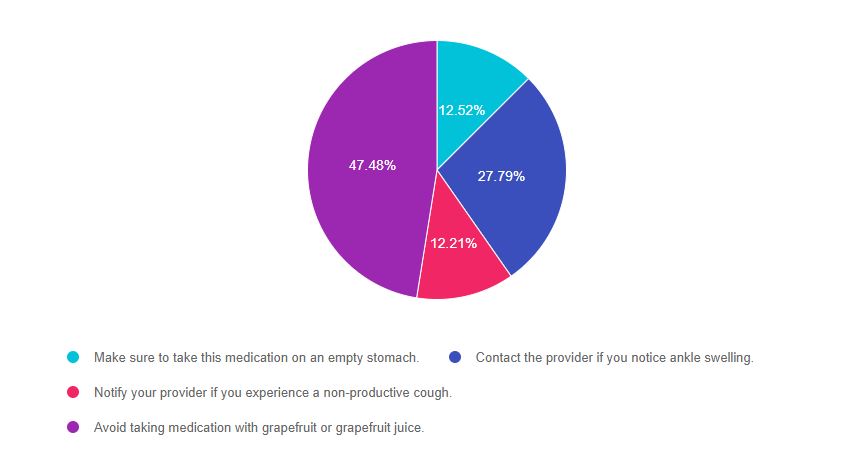
As shown above, the most common choice was option 3, the second most common answer was option 1, then option 4, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, it is helpful to know about newly approved diabetes medications, although it may take at least a year to appear in exams. However, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” that seem so familiar to you, right under your nose. Your job is to weed through the to choose the BEST answer.
Answer 1 is incorrect. 12.5% chose this answer, “Make sure to take this medication on an empty stomach.” If you don’t know anything about a particular medication and are forced to guess, this answer is pretty unlikely to be the best answer, for one reason. Most meds don’t need to be taken on an empty stomach. Two diabetes related meds, levothyroxine and oral semaglutide DO need to be taken on an empty stomach, but an empty stomach is not required for most other meds. Finerenone can be taken with or without food.
Answer 2 is incorrect. 27.8% of you chose this answer, “Contact the provider if you notice ankle swelling.” This was another juicy answer that we purposefully included. There is a class of diabetes medications, the TZDs (pioglitazone and rosiglitazone) that can cause ankle swelling, so this answer might have seemed familiar to you. Also when trying to find false answers, you may want to consider that it seems unlikely that a medication that slows kidney failure would have edema as a side effect.
Answer 3 is incorrect. 12.2% chose this answer, “Notify your provider if you experience a non-productive cough.” This juicy answer goes with a common blood pressure medication class, ACE Inhibitors, that people with diabetes are often prescribed to manage hypertension. With finerenone, the major consideration is monitoring the potassium in the first month of initiation.
Answer 4 is correct. 47.5% of respondents chose this answer, “Avoid taking medication with grapefruit or grapefruit juice.” GREAT JOB, this is the best answer. Since finerenone is a CYP3A4 substrate, the package insert recommends to avoid taking finerenone with other strong cype3A4 inhibitors. It also advises to avoid taking finerenone with grapefruit or grapefruit juice. Great job!
Want to learn more about finerenone?
Check out our New Updated Med Cheat Sheets 2021 (page 2) and consider attending our Virtual Conference with Dr. Diana Isaacs, who will speak more to this topic. You can also check out our Blog Post on New Meds for Diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
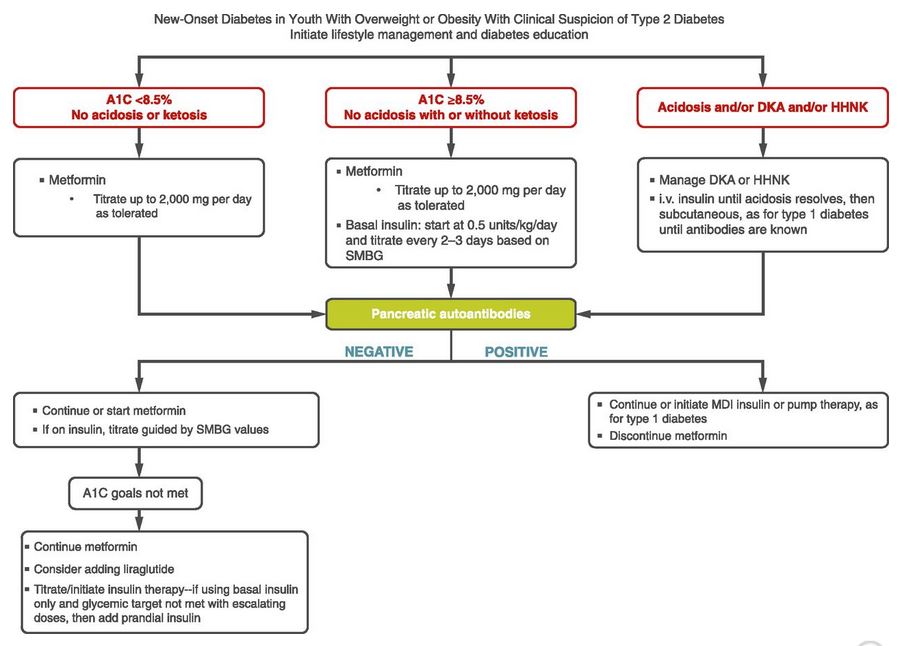
Diabetes Medication approved for Kids
The Food and Drug Administration (FDA) just approved another GLP-1 RA for use in children ages 10-17 with diabetes.
The injectable extended-release exenatide (Bydureon) is now the second glucagonlike peptide-1 receptor agonist (GLP-1 RA) approved for use in pediatric type 2 diabetes and the first with once-weekly administration. Liraglutide (Victoza) a daily injectable GLP-1 RA received approval for pediatric use in 2019 and metformin an oral biguanide has long been FDA approved for use children ten and older with type 2 diabetes.
During the annual scientific sessions of the American Diabetes Association, speakers expressed alarm about the rise in youth developing type 2 diabetes, noting that the condition typically progresses more rapidly and is less likely to respond well to metformin, compared with adults.
The approval was based on a 24-week, double-blind, placebo-controlled study in 82 children with type 2 diabetes aged 10 and older. They were randomized to 2 mg once-weekly exenatide extended release or placebo. At week 24, hemoglobin A1c in those randomized to the drug had dropped by 0.25 percentage points, compared with a 0.45 percentage point increase in the placebo group.
Based on the ADA Standards of Care for treating pediatrics with diabetes, the first treatment includes weight loss and exercise plus first line medications metformin and insulin if A1c is 8.5% or greater.
Furthermore, the initiation of any GLP-1 RA is only recommended once pancreatic antibodies are determined to be absent and if A1c goals have not met despite the initiation of metformin or insulin (see ADA standards algorithm below stating consider adding liraglutide (GLP-1 RA))
We have updated the electronic version of our Injectable PocketCard to reflect this update.
Download our Medication PocketCards today on our Website PocketCards , or CDCES Coach App (free).
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Intensive Insulin Therapy with A1c 6.2%

HR is a 78-year-old with a stroke and limited cognition with diabetes for 8 years and is on intensive insulin therapy: HR takes bolus insulin at meals and basaglar at night. HR has an A1c is 6.2% and employs a part time caretaker.
What is the best response in this situation?
- Start HR on an insulin pump and CGM to prevent hypoglycemia.
- Discuss de-intensifying insulin regimen.
- Using a strength-based approach, reinforce the importance of keeping the A1c less than 7%.
- Evaluate for diabetes related distress.
Click here to test your knowledge!
Want to learn more about this topic and more?
Enroll in our Virtual DiabetesEd Specialist Program!
Did you miss the live conference? No worries! You can register now to watch on-demand
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: Your registration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Know someone with Type 1 Diabetes? We can offer help!
Attention Diabetes Educators and Specialists:
Do you know an adult living with Type 1 Diabetes and an A1c of 7.5% or greater?
Please invite them to join the EMBARK Study, Participants receive payment plus group classes and one-on-one coaching from diabetes experts as part of this NIH Study. We need to enroll 70 ,more participants by the end of the year and we so appreciate your help!
What participant’s are saying about their EMBARK experience
“I feel a lot more empowered in my diabetes care”
“I have learned so much about how to make insulin and carb adjustments to improve blood sugars.”
“This is the first time in 10 years that I have had an A1c less than 7%.”
As an instructor and coach for the past year with the EMBARK study, I can attest that participants greatly benefit from their experience. They comment on how much they love the virtual group classes and swapping stories with others living with Type 1 Diabetes. Many participants have shared that they don’t feel so alone with their diabetes because of these group sessions. They also appreciate how much they learn about self-managing their diabetes during the individual coaching sessions with a diabetes expert.
EMBARK Info Sheet to Share with Participants
Benefits of joining the EMBARK Study
- EMBARK is a national, entirely virtual program to help adults with T1D reduce diabetes distress and improve management.
- EMBARK addresses the emotional side of diabetes: the often neglected part of diabetes care called “diabetes’ distress.” This refers to the expected stresses, worries, burdens, and concerns that are part of living with diabetes over time and that impacts many aspects of diabetes management.
- Participants get paid $250. Because it is a University-based, NIH-supported clinical trial, EMBARK pays participants for brief assessments over 12 months ($250 total), including free A1C testing.
- EMBARK includes live, interactive, small group education and training, plus personal coaching over three months.
- EMBARK provides an easily accessible personal resource to help with management and living with diabetes during the pandemic, when many people with diabetes lack access to care and support.
- EMBARK includes randomization to three different evidenced-based programs – there is no non-intervention control group, so everyone receives an active intervention.
- Because EMBARK includes ongoing evaluation, the information gained will be passed on to diabetes clinicians to enhance care.
- EMBARK is delivered by highly experienced, licensed educators and behavioral psychologists.
Sign up Today
It is so easy to get started. Just click this link or call: 1-855-850-3599 (toll-free) or email us at: [email protected].
Learn more about EMBARK- Click Here!
EMBARK Info Sheet to Share with Participants
Thank you,
UCSF EMBARK Team