Virtual DiabetesEd Specialist Conference | 30+ CEs
Join our Virtual DiabetesEd Specialist Program!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Deluxe Virtual Program for $459 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2021 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs
Basic virtual program for $359 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of Week – | Which One is Autonomic Neuropathy? We made an oops!

For our August 17th Question of the Week, 39% of respondents chose the best answer. This is due in part to our error. We mis-keyed the best answer for the first 96 respondents (we quickly fixed it as soon as we discovered the error). So, you may want to retake this question before you read on to discover the answer. Coach Bev sincerely apologizes if this caused any of you distress! But today, we are making it right. Thanks for your patience and ongoing participation!
Before we start, if you don’t want any spoilers and you tried the question on Tuesday morning, you can answer below: Answer Question
Question 1: Which of the following are considered diabetes autonomic neuropathies?
- Decreased sexual arousal, pins and needles sensations in lower extremities.
- Loss of protective sensation and urinary incontinence.
- Resting tachycardia and esophageal dysmotility.
- Hypoglycemia unawareness and insensate feet.
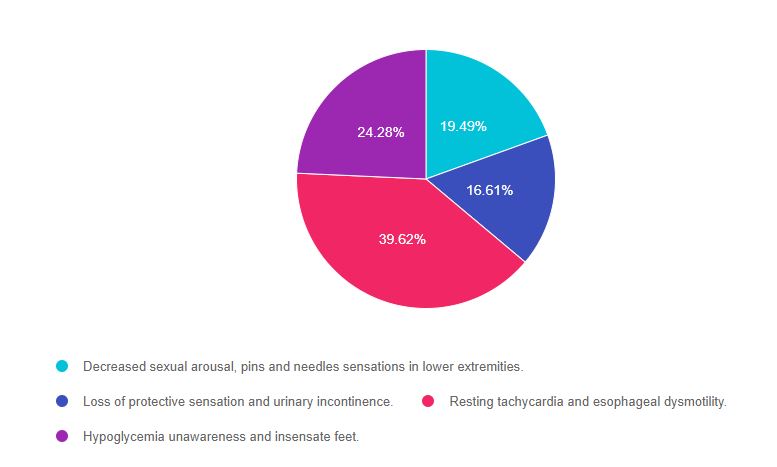
As shown above, the most common choice was option 3, the second most common answer was option 4, then option 1, and finally option 2.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for specialty topics like microvascular disease. Be familiar with nerve disease presentation and screening as listed in the ADA Standards of Care on Microvascular health and treatment options. We also invite you to join our webinar (see below). Also, the tests will often provide a 2 part answer, one part being correct and the other part incorrect. Of course, if any part of the answer is incorrect, it is not the best answer. A great test taking tip to hold onto to when your sympathetic nervous system is in full gear. You got this, Coach Beverly
A note on Autonomic Neuropathy. This condition causes nerve damage to the autonomic nervous system which is in charge of digestion, sexual function, heart rate, and the adrenergic flight or fight response. The autonomic nervous system also “oversees” the energy-conserving parasympathetic response including bladder control, heart rate slowing, eye pupil constriction, and more.
Answers & Rationale
Answer 1 is incorrect, 19.49% chose this answer, “Decreased sexual arousal, pins and needles sensations in lower extremities.” This is a juicy answer. Autonomic dysfunction can affect sexual function, but it doesn’t affect libido or sexual desire. In addition, the pins and needles sensation is due to the nerve damage associated with peripheral neuropathy. Since both parts of this answer aren’t correct, this answer is false.
Answer 2 is incorrect, 16.61% of you chose this answer, “Loss of protective sensation and urinary incontinence.” Loss of protective sensation is associated with peripheral neuropathy. However, urinary incontinence is often a result of autonomic neuropathy. Since both parts of this answer aren’t correct, this answer is false.
Answer 3 is correct, 39.62% of you chose this answer, GREAT JOB! “Resting tachycardia and esophageal dysmotility.” Elevated heart rate while resting is a concerning sign and is often associated with cardiac autonomic neuropathy and increased risk of a cardiac event. Autonomic neuropathy can affect the motility of the entire GI track, including the esophagus. The more commonly recognized GI autonomic neuropathy is gastroparesis. Since both conditions, resting tachycardia and esophageal dysmotility, are associated with autonomic neuropathy, this is the best answer.
Answer 4 is incorrect, 24.28% of you chose this juicy answer “Hypoglycemia unawareness and insensate feet.” Since hypoglycemia unawareness is associated with a diminished adrenergic response to low blood glucose levels, it is considered an autonomic neuropathy. However, insensate feet are due to peripheral nerve damage associated with ongoing hyperglycemia. Since both parts aren’t correct, this answer is false.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic?
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
We are Celebrating DiabetesEd Specialist Scholarship Recipients
We are so excited to announce our DiabetesEd Specialist Scholarship Recipients!
We received dozens of applications for our annual Making a Difference Scholarship and the Flower Scholarship gifted from an anonymous donor! It was a great personal joy for our team to read these scholarship applications. Each applicant is serving communities with a great need and going “above and beyond” to promote and provide accessible diabetes care and education. It is always a very difficult decision for all of the judges, and we read each application in careful detail considering the financial need, impact, volunteerism, and readiness to take the CDCES exam.
We greatly appreciate the good work of all the applicants and thank them for their service!
This year we are offered 3 Scholarship Options for our Virtual DiabetesEd Specialist Conference, October 6-8, 2021.
Congratulations Chantel Wade, his year’s Flower Scholarship Recipient!
Chantel Wade is the recipient of our “Flower Scholarship.” Chantel is an ambulatory RN and the lead in the Patient Education Department at her local health center. There she serves a diverse population of individuals from different socioeconomic backgrounds, seeing many people who are on Medicare, Medi-Cal or are uninsured. She uses a hands-on, interactive approach with those she works with; she is committed to meeting people where they are by creating custom care plans that meet their individual needs. Outside of work, she is active in her local Fellowship Church and other organizations where she volunteers her time and expertise to offer pre-diabetes and diabetes education.
Congratulations Keira McCrary, “Making a Difference Exemplar Scholarship” Recipient!
Keira McCrary is the recipient of our “Making a Difference Exemplar Scholarship” because of her dedication to her community. Keira works as a Registered Dietician who provides direct care services to Native American tribal communities in her area. In her work, she supports people living with diabetes through all stages of life with programs such as home meal delivery for elder tribal members and the Native Youth Preventing Diabetes Organization. Through Native Youth Preventing Diabetes Organization Keira assists in the education of tribal youth in the areas of diabetes prevention, nutritional education, physical activity, behavioral health, and more. She also creates user-friendly tools for those she works with such as informational “how-to” diabetes-friendly recipe videos and a weekly newsletter.
Congratulations Logan Mumphrey, “Making a Difference Scholarship” Recipient!
Logan Mumphrey is our second recipient of our “Making a Difference Scholarship” for many reasons! Logan is currently working towards his MSN/FNP and has worked as the primary nurse and clinical coordinator for transgender health services helping to build the program from the ground up. This program provides gender-affirming care that goes beyond hormone therapy including care navigation, surgery coordination, assistance with identity document changes, peer support, and much more. Logan is passionate about diabetes care and education and hopes that by becoming a CDCES, it will allow him to provide more support for those he works with so they can manage their diabetes with a gender-affirming lens.
This year we are offered 3 Scholarship Options which include:
- Flower Scholarship valued at $1000 for a diabetes nurse educator who comes from an under-served community and is providing care and education to communities that lack access to Diabetes Specialists and health care resources. The nurse applicant taking their CDCES exam within a year. The donor of this scholarship is generously providing funds to cover course registration plus enrollment in our Ultimate Online Bundle, Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages, ADA 2021 Standards of Care Book DiabetesEd Services highlighters, PocketCard and Pen.
- Making a Difference Exemplar Scholarship valued at $1000 for a diabetes educator who exemplifies advocacy and compassionate care in their community and is pursuing their CDCES. This top-tier scholarship provides funds to cover course registration plus enrollment in our Ultimate Online Bundle, Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages, ADA 2021 Standards of Care Book DiabetesEd Services highlighters, PocketCard and Pen.
- Making a Difference Scholarship valued at $900 for a diabetes educator who exemplifies advocacy and compassionate care in their community and is pursuing their CDCES. This scholarship provides funds to cover course registration plus enrollment in our Ultimate Online Bundle.
The goal of these scholarships are three-fold:
- To support U.S. health care professionals who are going above and beyond to improve diabetes care in their community; and
- To support applicants’ effort to become a Certified Diabetes Care and Education Specialist (CDCES) and
- To provide financial assistance with the DiabetesEd Course registration fee and or sleeping rooms
Question of Week | Thick calluses coupled with leg pain?

JR has lived with type 1 diabetes for over twenty years. JR arrived in the clinic with thick calluses on both feet and complaints of calf pain when walking for more than 10 minutes. JR’s pulses are difficult to palpate.
What diagnosis best matches JR’s presentation?
- Peripheral polyneuropathy.
- Diabetes venous stasis syndrome.
- Peripheral arterial disease.
- Charcot foot.
Click here to test your knowledge!
Want to learn more about this topic and more?
Join our Virtual DiabetesEd Specialist Program!
Airs live October 6-8, 2021
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!

CEs: Includes over 30 CEs
Program Info: 2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Speakers: View Conference Faculty.
Dates: October 6-8. Don’t worry if you can’t make it live. YourRegistration fee includes access to FREE podcast and all recorded webinars for one year.
Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | Oct. 6-8 | 30+ CEs
Deluxe Virtual Program for $499 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
+Plus Syllabus, Standards and Swag:
- Diabetes Educator Course 2021 Syllabus Hard Copy – over 100 pages -This spiral-bound workbook contains the printed version of all of the instructor’s slides.
- ADA 2021 Standards of Care Book -The ADA Standards of Medical Care in Diabetes is a key resource for healthcare professionals involved in diabetes care, education, and support.
- DiabetesEd Services highlighters, Medication PocketCard and Pen
Syllabus and Bonus Items Shipping Notice for Deluxe Virtual Conference: Our company is based in California, so if you live toward the east coast it can take more than 5 business days for the book to arrive. Please purchase the conference with syllabus no later than Tuesday, Sept 28th to ensure delivery in time for the conference.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Virtual DiabetesEd Specialist Conference Basic | Oct. 6-8 | 30+ CEs
Basic virtual program for $399 includes:
- Presentations by our team of experts
- Q & A Session with the instructor after each webinar
- State-of-the-art review of current diabetes care and technology.
- Resources for each session
- Access to FREE podcast and recorded webinars within a week of each live session for one full year.
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Team of Experts: Our team of expert faculty has been fine-tuning this course for over fifteen years and we know what you need to succeed! In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Bonus Courses worth 12+ CEs, FREE
When you register for our Virtual Course, you have immediate access to these Bonus DiabetesEd University Online Courses – for FREE!
- Test Taking Toolkit – Over 200 sample test questions!
- Level 2 – Assessing and Promoting Well-Being: From Population Health to a Person-Centered Approach 1.5 CEs
- Level 2 – Hospital and Hyperglycemia 1.5 CEs
- Level 2 – Hyperglycemic Crisis, DKA and HHS Standards 1.0 CEs
- Level 2 – Meds Management Update for Type 2 – 1.5 CEs
- Level 2 – Setting up a Successful Diabetes Program 1.5 CEs
- Level 2 – Pregnancy and Diabetes 1.5 CEs
- Level 2 – From Tots to Teens – Diabetes Standards 1.5 CEs
- Level 2 – Older Adults and Diabetes 1.5 CEs
- Mindfulness and Compassion in the Diabetes Encounter – 1.0 CE
2021 Diabetes Educator Course Flyer & Schedule (subject to change)
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Eye Check Necessary?

For our August 10th Question of the Week, 37% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: AL is 24 with newly diagnosed type 1 diabetes. AL is very worried about going blind because an Aunt with Type 1 diabetes lost her vision due to living with type 1 diabetes.
Which of the following matches the ADA guidelines for diabetes eye care?
- An eye examination is recommended before pregnancy.
- Get eye exam immediately at type 1 diabetes diagnosis, then yearly thereafter.
- If no retinopathy found on initial exam, refer to trained retinal expert for thorough exam.
- Only trained ophthalmologist can screen for type 1 diabetes eye disease.
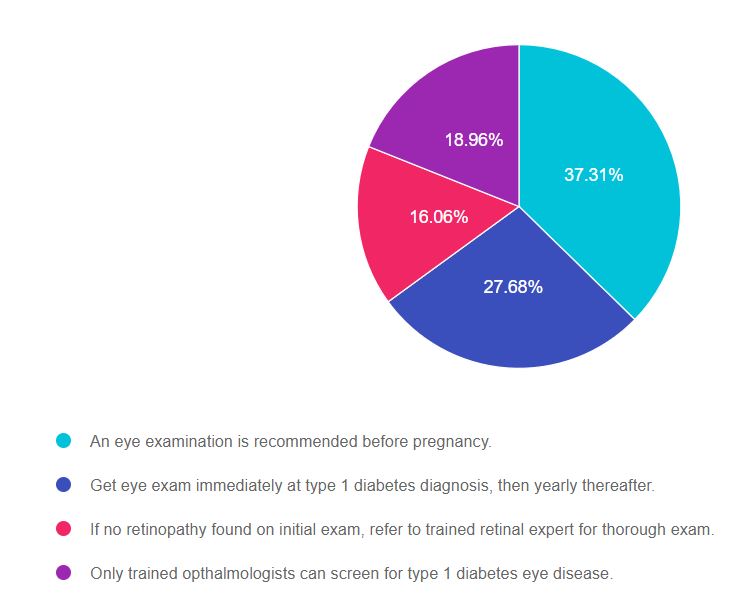
As shown above, the most common choice was option 1, the second most common answer was option 2, then option 4, and finally option 3.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for specialty topics like microvascular disease. Be familiar with screening guidelines for eye disease as listed in the ADA Standards of Care on Microvascular health and treatment options. We also invite you to join our webinar (see below). You got this, Coach Beverly
Answers & Rationale
Answer 1 is correct, 37.31% chose this answer, “An eye examination is recommended before pregnancy.” Great Job! Yes, this is the best answer. All people living with diabetes considering pregnancy need to get a baseline eye exam to evaluate retinal health. In addition, the ADA Standards recommend eye exams each trimester of pregnancy and after birth to monitor retinal changes.
Answer 2 is incorrect, 27.68% of you chose this answer, “Get eye exam immediately at type 1 diabetes diagnosis, then yearly thereafter.” This is the juicy answer. According to the ADA Standards for people with type 1 diabetes, they need an eye exam within in 5 years of diagnosis, then an eye exam every 1-2 years. The reason they don’t require an immediate eye exam is because type 1 diabetes is quickly identified and this short span of hyperglycemia does not increase risk of retinopathy. The reason we check people with type 2 eyes immediately, is because they could have had diabetes for an average of 6 years before diagnosis, allowing for the possibility of undetected eye damage.
Answer 3 is incorrect, 16.06% of you chose this answer, “If no retinopathy found on initial exam, refer to trained retinal expert for thorough exam.” ‘All people with diabetes do not need to be referred to a retinal expert. An ophthalmologist or optometrist can screen for type 1 diabetes eye disease. If retinopathy is discovered, depending on the severity, they may advise referral to a retinal specialist as needed.
Answer 4 is incorrect, 18.96% of you chose this answer “Only a trained ophthalmologists can screen for type 1 diabetes eye disease.” An ophthalmologist or optometrist can screen for type 1 diabetes eye disease. Programs that use retinal photography (with remote reading or use of a validated assessment tool) are also appropriate screening strategies for diabetes retinopathy. Such programs need to provide pathways for timely referral for a comprehensive eye examination when indicated.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic?
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
Enroll Now | 1.5 CEs | $29
Join us for our
Level 2 | Setting up a Successful DSME Program Standards | 1.5 CEs

This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking the CDCES Exam or considering setting up a DSME program, this program is designed for you. We review the 10 standards and provide strategies on implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- The steps involved in setting up a Diabetes Program
- List program essentials
- Discuss marketing strategies for success
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | Which One is Autonomic Neuropathy?

Which of the following are considered diabetes autonomic neuropathies?
- Decreased sexual arousal, pins and needles sensations in lower extremities.
- Loss of protective sensation and urinary incontinence.
- Resting tachycardia and esophageal dysmotility.
- Hypoglycemia unawareness and insensate feet.
Click here to test your knowledge!
Want to learn more about this topic? Enroll in our
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
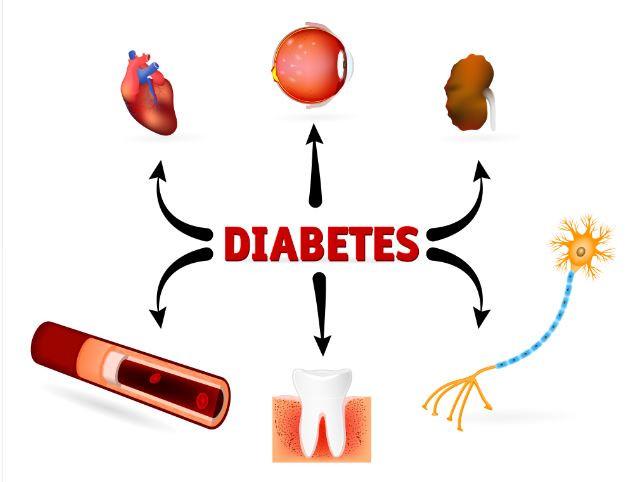
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Protecting Kidney Function, Best Strategy?

For our August 3rd Question of the Week, 53% of respondents chose the best answer. We want to “take a closer look” at this question and determine strategies to choose the best response.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question 1: JR is 53 years old with type 2 diabetes for the past 7 years. JR’s BMI is 32, GFR is more than 60, blood pressure is 128/76, Urinary Albumin Creatinine Ratio (UACR) is 17mg/g.
According to the ADA Standards, which of the following is the most accurate recommendation to continue to protect JR’s kidney function?
Answer Choices:
- Initiate low dose ACE Inhibitor or ARB
- Focus on lifestyle changes
- Maintain protein intake to ~0.7 g/kg
- Reduce sodium intake to 1000 mg per day
As shown above, the most common choice was option 2, the second most common answer was option 3, then option 4, and finally option 1.
Getting to the Best Answer
If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. Don’t forget to leverage your common sense and vast health care knowledge to get the best answer for these specialty topics like diabetes kidney disease. Be familiar with MNT guidelines and guidelines for best therapeutic intervention based on careful assessment of microvascular health. You got this, Coach Beverly
Answers & Rationale
Answer 1 is incorrect, 32% chose this answer, “Initiate low dose ACE Inhibitor or ARB.” This is a juicy answer, however, based on the ADA Standards on Microvascular Complications, medication is not required.
Here are 3 reasons why JR does not need an ACE or ARB:
- JRs GFR is more than 60, indicating acceptable kidney function.
- His B/P is below the most stringent target of 130/80.
- His UACR is normal, at less than 30.
Since all three of these indicators are below target range, blood pressure medication is not warranted and could even cause unwanted side effects like orthostatic hypotension. About a decade ago, there was a recommendation to start people with type 1 on an ACE or ARB to protect the kidney function, but it is NO longer recommended because it did not improve outcomes.
Answer 2 is correct, 53% of you chose this answer, “Focus on lifestyle changes.” YES, GREAT job. To help JR to keep his vessels healthy and improve his overall nutrition, we are going to encourage regular activity and an evidence based nutrition approach (DASH diet, Mediterranean, Plant Based eating etc.). We will make sure JR has an appointment with a diabetes care and education specialist and RD/RDN. No medications needed for JR, just ongoing self-care support and encouragement.
Answer 3 is incorrect, 9% of you chose this answer, “Maintain protein intake to ~0.7 g/kg.” In the old days, we used to recommend restricting protein intake to less than 0.8g/kg for people with diabetes kidney disease. We no longer make this recommendation since it didn’t improve outcomes! Plus, JR’s kidney function is fine and there is no diabetes kidney disease based on the information provided.
Answer 4 is incorrect, 6% of you chose this answer “Reduce sodium intake to 1000 mg per day.” For people with diabetes, the sodium recommendation is 2,300 mg per day, regardless of their blood pressure, since there is no evidence that a lower sodium intake reduces risk of complications.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this topic? Enroll in our
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
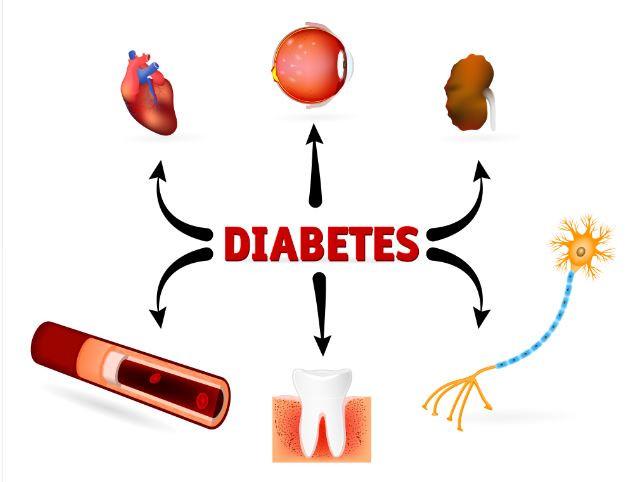
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of Week | What is Best Eye Care Guideline?

AL is 24 with newly diagnosed type 1 diabetes. AL is very worried about going blind because an Aunt with Type 1 diabetes lost her vision due to living with type 1 diabetes.
Which of the following matches the ADA guidelines for diabetes eye care?
- An eye examination is recommended before pregnancy.
- Get eye exam immediately at type 1 diabetes diagnosis, then yearly thereafter.
- If no retinopathy found on initial exam, refer to trained retinal expert for thorough exam.
- Only trained opthalmologists can screen for type 1 diabetes eye disease.
Click here to test your knowledge!
Want to learn more about this topic? Enroll in our
Join us for our
Level 2 | Microvascular Complications, Eye Kidney, & Nerve Disease Standards | 1.5 CEs
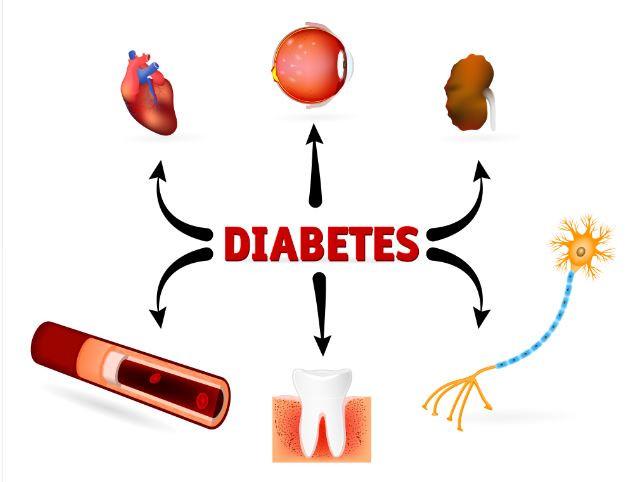
This course provides you with the need-to-know information regarding the microvascular complications of diabetes. We start with a brief overview of the pathophysiology and clinical manifestations then sum up with prevention strategies and screening guidelines. This straight-forward program will provide you with information you can use in your clinical setting and also provides critical content for the diabetes educator exam.
Objectives:
- Eye, kidney and nerve disease
- Modifiable and non-modifiable risk factors for diabetes complications
- Screening guidelines and prevention strategies.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Want to learn more about this topic? Enroll in our
Join us live on August 26th from 11:30 am to 1:00 pm for our
Level 2 | Setting up a Successful DSME Program Standards | 1.5 CEs

This course provides you with a succinct overview of the latest standards for Diabetes Self-Management Education (DSME) and Support Programs. If you are taking the CDCES Exam or considering setting up a DSME program, this program is designed for you. We review the 10 standards and provide strategies on implementation. In addition, we discuss Medicare Reimbursement and covered benefits. This course provides insights into the exam philosophy and also highlights critical content areas.
Objectives:
- The steps involved in setting up a Diabetes Program
- List program essentials
- Discuss marketing strategies for success
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
See Full Calendar for upcoming webinars and events.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








