3 Ways Companion Pets Can Support People with Diabetes
What Do I Do with These Needles? Sharps Disposal Resources

MR arrived at the clinic last week with a bag full of stuff. To be honest, my imagination conjured that they had a bag of fresh peaches or other fruits from their local farm to share with the staff. I laughed when they pulled out bleach and coffee containers filled with lancets and needles. When we first met they had been tossing their used sharps in the trash. After I explained that those sharps can harm the sanitation workers plus they can mess up recycling equipment, they were more than happy to start tossing used needles and syringes in used bleach bottles and coffee cans. MR is not alone, many people living with diabetes use sharps such as lancets or needles to manage their diabetes and disposing of used sharps safely is important for all of us.
We want to share this helpful website, SafetyIsThePoint.org that gives instructions for how to safely dispose of household-used sharps. This website has videos, cheatsheets, and a search function for drop-off locations available by zip code.
Household Sharps Management
On their Household Sharps Management page, they outlined the steps for how to safely dispose of sharps in their household trash, along with an instructional video.
Finding Local Disposal Locations
Across the U.S. people living with Diabetes can enter their zip code and find disposal centers in their regions.
Cheatsheets
They also provide handy posters and cheatsheets on best practices for household sharps disposal.
- Used Household Sharps Disposal Poster
- Used Household Sharps Disposal Rack Card
- Household Sharps Fact Sheet
- Social Media Material
Check out their website, SafetyIsThePoint.org to read more.
Join us for our upcoming FREE webinar
3 Steps to Save Feet; Assess, Screen, and Report
Airs live on August 10, 2023, at 11:30 am PST
Coach Beverly walks participants through the 3 Step Process to Save Feet; Assess, Screen and Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment and action steps. We will share free teaching tools, strategies, and documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting.
Objectives:
- Describe steps involved in effective foot assessment made easy.
- Demonstrate how to use a monofilament to assess sensation.
- Discuss the use of screening forms to report findings
Two Ways to Register
Intended Audience: This course is designed for all health care providers and educators, who are interested in learning more about assessing and saving feet in people living with diabetes.
All hours earned count toward your CDCES Accreditation Information
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
FreeStyle Libre 3 Sensor
People with diabetes are very interested in learning about the newest and smallest FreeStyle Libre 3 sensor produced by Abbott Laboratories. This sensor, approved for people with diabetes 4 years and older offers significant improvements. Here is a summary of features that we hope you find helpful when advising people on the best choice based on their needs.
This latest FreeStyle Libre 3 version offers a smaller sensor that is the size of two stacked pennies. With this upgraded sensor, users no longer have to scan the sensor at least every eight hours to prevent data loss. This 14-day sensor automatically transmits glucose values to their smartphones every minute. There is no reader associated with this sensor, so users will need to have a newer android or iPhone that can support the FreeStyle Libre 3 app. It’s a good idea to download the Freestyle 3 app in the office before the person leaves, to make sure their phone supports the app. If not, they might be better suited to the FreeStyle Libre 2 CGM system that does have a reader in addition to the app.
Sensor insertion is fairly simple. The most important teaching points include making sure the insertion site is washed thoroughly, cleaned with alcohol, and allowed to dry combined with a good site location. Avoid overwrap that is not ‘breathable’ and would occlude the sensor hole, since moisture can accumulate and affect adhesion. In addition, glucose notifications can only be transmitted to phones when they are within 33 feet of the sensor.
The accuracy of this sensor has a MARD rating of sub-8% (lower is better), and demonstrates accuracy during intense blood sugar fluctuations, which can be reassuring for people making insulin adjustments based on results. Alarms settings can be customized with the exception of the default urgent low glucose alarm which alarms when glucose levels hit 55 mg/dl.
No calibration is needed with the Libre 3 Sensor, but there is a one-hour warm-up period. Sharing data is made easy with this sensor. Clinicians can log onto Freestyle Libre View Portal to receive data and support people can use the LibreLinkUp to keep track of blood sugar trends.
Unfortunately, in order for Medicare to cover sensors under DME, there needs to be an associated glucose “reader” in addition to the person taking at least one injection of insulin a day. Given this stipulation, people with Medicare may want to opt for the FreeStyle Libre 2 version that comes with a glucose reader.
With insurance, the cost for 2 sensors is about $65 a month. For those without insurance coverage, the out-of-pocket expense is $130-160.
For more information, you can visit the Abbott website and you are invited to purchase our Virtual Conference with Dr. Diana Isaacs, which provides a detailed review of diabetes technology.
Want to learn more about this question? Join us for our
Meds for Type 2 Update; New ADA/EASD Consensus Statement
Level 2 | 1.25 CEs
Airs live on Wednesday, December 1st at 11:30 am PST

Plan on joining this exciting webinar that walks participants through the newly released, “Management of Hyperglycemia in Type 2 Consensus Report by the ADA and EASD”. These updated guidelines will be incorporated into the 2023 ADA Standards of Care, but you can get a early sneak peak by joining Coach Beverly on December 1st, 2022. She will highlight the revised guidelines with a focus on new elements and exciting changes on how we approach medication management for type 2 diabetes. Together, we will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection and addressing clinical inertia.
Objectives:
- Describe the role of Diabetes Care and Education Specialists in advocating for optimal therapeutic approaches.
- Discuss the application of the new ADA/EASD Guidelines to improve glucose and reduce CV and renal risk.
- List strategies to initiate and adjust oral and injectable therapy using a person-centered approach
Intended Audience: A great course for health care professionals seeking evidence-based information that improves the quality of life and outcomes.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Uvalde T-Shirt Installation Connects Art to Heart

After the Uvalde shooting, a group of mothers who belonged to a monthly book club, decided not to talk about their book of the month. Instead they dedicated their gathering to sharing their deep grief and feelings of powerlessness about the senseless loss of 19 beautiful children in Uvalde, Texas. Children, just like their own, who were excited to learn, hang out with friends and wrap up school for the summer.
I am one of the book club mothers.
We committed to shine a light on this tragedy and connect to our common humanity through art. We are often afraid to talk about gun violence because it is such a fraught conversation. However, we know one thing we all have in common regardless of our political affiliation or upbringing.
We all want our school aged children to be safe and free of death from gun violence in their schools, homes and communities.
Let’s start our conversation with this belief in mind.
To express our grief and touch the hearts of others, we created an art installation featuring 21 orange t-shirts of different sizes, with the hand-painted names of the children and teachers who died that day in May. We call it the “Uvalde T-shirt Clothesline”.
The Uvalde T-Shirt Clothesline speaks of the empty shirts left behind: shirts that will never be played in, worn to school, or hugged at night.
We displayed this at our local Farmer’s Market where many people stopped, looked up and reflected on the loss. It now it hangs at the entrance of the museum of northern california, monca.



Uvalde T-Shirt Clothesline Story
On May 24, 2022, in the small town of Uvalde, Texas, nineteen innocent children and two teachers were gunned down at school by an 18-year-old with an automatic weapon. Out of our grief and dismay over this tragic loss of life arose this installation of 21 orange t-shirts, hand-painted with the names of the children and teachers who died that day.
The Uvalde T-Shirt Clothesline speaks of the empty shirts left behind: shirts that will never be played in, worn to school, or hugged at night. Shirts whose young owners will never reach their full potential. We chose orange shirts since orange is the commemorative color of gun violence prevention.
Empty orange shirts on a clothesline serves as a metaphor for the ordinary act of hanging our family’s clothes to dry, a commonplace fixture of household routine. It connects to the tragic reminder that gun violence in our schools is also becoming routine.
Firearms are the leading cause of death for children in the United States. Every two and a half-hours, a child loses their life due to firearm violence, accidents, or suicide. We hope this display touches hearts and shines a light on the senseless loss of these beautiful souls. Through connection and conversation, we can make a difference.
Please share any questions or comments regarding this blog with [email protected]. Thank you.
T-Shirt Clothesline Tribute makes local paper front page.
Maybe other communities could create their own clothesline? Read Enterprise Record Article here.
Resources
Download a List of Gun Violence Prevention Organizations
Nurses Union Addresses Gun Violence
Art Displays
Uvalde mural honors Robb Elementary School shooting
Know someone with Type 1 Diabetes? We can offer help!
Attention Diabetes Educators and Specialists:
Do you know an adult living with Type 1 Diabetes and an A1c of 7.5% or greater?
Please invite them to join the EMBARK Study, Participants receive payment plus group classes and one-on-one coaching from diabetes experts as part of this NIH Study. We need to enroll 70 ,more participants by the end of the year and we so appreciate your help!
What participant’s are saying about their EMBARK experience
“I feel a lot more empowered in my diabetes care”
“I have learned so much about how to make insulin and carb adjustments to improve blood sugars.”
“This is the first time in 10 years that I have had an A1c less than 7%.”
As an instructor and coach for the past year with the EMBARK study, I can attest that participants greatly benefit from their experience. They comment on how much they love the virtual group classes and swapping stories with others living with Type 1 Diabetes. Many participants have shared that they don’t feel so alone with their diabetes because of these group sessions. They also appreciate how much they learn about self-managing their diabetes during the individual coaching sessions with a diabetes expert.
EMBARK Info Sheet to Share with Participants
Benefits of joining the EMBARK Study
- EMBARK is a national, entirely virtual program to help adults with T1D reduce diabetes distress and improve management.
- EMBARK addresses the emotional side of diabetes: the often neglected part of diabetes care called “diabetes’ distress.” This refers to the expected stresses, worries, burdens, and concerns that are part of living with diabetes over time and that impacts many aspects of diabetes management.
- Participants get paid $250. Because it is a University-based, NIH-supported clinical trial, EMBARK pays participants for brief assessments over 12 months ($250 total), including free A1C testing.
- EMBARK includes live, interactive, small group education and training, plus personal coaching over three months.
- EMBARK provides an easily accessible personal resource to help with management and living with diabetes during the pandemic, when many people with diabetes lack access to care and support.
- EMBARK includes randomization to three different evidenced-based programs – there is no non-intervention control group, so everyone receives an active intervention.
- Because EMBARK includes ongoing evaluation, the information gained will be passed on to diabetes clinicians to enhance care.
- EMBARK is delivered by highly experienced, licensed educators and behavioral psychologists.
Sign up Today
It is so easy to get started. Just click this link or call: 1-855-850-3599 (toll-free) or email us at: [email protected].
Learn more about EMBARK- Click Here!
EMBARK Info Sheet to Share with Participants
Thank you,
UCSF EMBARK Team
Diabetes in the US: Could we be doing better?

I felt pretty discouraged reading through the New England Journal of Medicine (NEJM) summary of the state of diabetes treatment and control in the U.S. from 1999-2018. We have stalled in improving diabetes outcomes in spite of exciting new therapies and dazzling technologies.
Based on this “Diabetes Report Card” for the U.S it seems pretty clear that changes in our care delivery system are urgently needed. First, let me share the data, then we consider how Diabetes Care Specialists (you and me) can drive the improvement arrow in the right direction.
The data summarized below is extracted from the National Health and Nutrition Examination Survey (NHANES) which assesses national trends in diabetes care and outcomes for the past decade.
Summary of the major findings of the Diabetes ABC’s. A1C, Blood Pressure and Cholesterol.
Data is compared from the 2007 -2010 period to the 2015-2018 time period.
Reaching A1c Target of less than 7%?
- The percentage of people with diabetes and an A1c of less than 7%, declined from:
- 57.4% in 2007-2010 to
- 50.5% in 2015 to 2018
Coach Bev’s Report Card Comment: Blood glucose levels trended up. GRADE C-
Reaching LDL target of less than 130 mg/dL?
- The percentage of people with diabetes and an LDL of less than 130 leveled off, with slight movement in the right direction.
- 52.3% in 2007-2010 to
- 55.7% in 2015 to 2018
Coach Bev’s Report Card Comment: Lipid levels improved slightly. GRADE B-
Reaching blood pressure goal of less than 140/90 mm Hg?
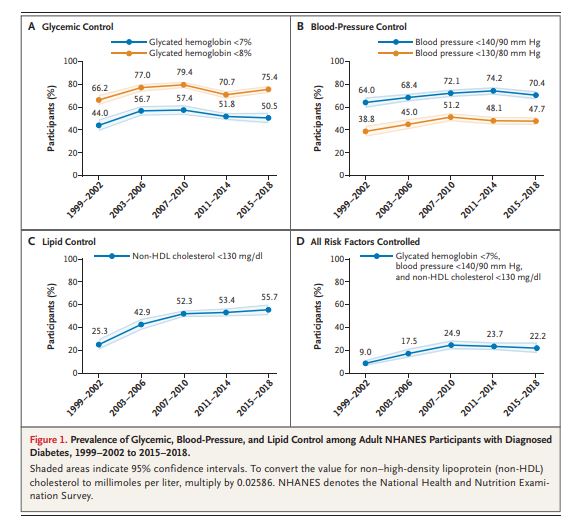
- The percentage of people with diabetes and blood pressure below the target of 140/90 worsened.
- 74.2% in 2007-2010 to
- 70.4% in 2015 to 2018
Coach Bev’s Report Card Comment: Blood pressure control achievement dropped slightly. GRADE C-
The percent of participants who achieved all 3 targets of A1C, BP, and lipids?
- The percentage of people who reached all 3 targets declined slightly.
- 24.9 % in 2007-2010 to
- 22.2% in 2015 to 2018
Coach Bev’s Report Card Comment: ABC’s of diabetes control dropped slightly. GRADE C-
Data and Graph from Trends in Diabetes Treatment and Control in U.S. Adults, 1999–2018 | NEJM
What are the barriers and how can Diabetes Care and Education Specialists help improve the grade?
The year 1999 got off to a good start with improved diabetes control but stalled and declined as the decade moved forward. There are several possible reasons as cited by the authors.
Sluggish initiation of first-line therapies. In 2015–2018, only 56.3% of adults with diabetes were using statins, 59.5% were using metformin, and 60.3% were using an ACE inhibitor or ARB.
These results are consistent with those of previous studies and point to clinical inertia as a potential culprit.
In addition, achieving glycemic and blood-pressure control often entails the use of multiple agents. However, the study found that only 60.6% of participants with an A1C level of 7% or higher and 52.8% of those with a blood pressure of 140/90 mm Hg or higher were treated with more than one glucose-lowering or blood-pressure-lowering medication, respectively.
Coach Beverly suggested action: Diabetes Care and Education Specialists can continue to raise awareness of the ADA Standards of Care for Diabetes and advocate for initiating first-line and add-on therapies in their work settings. Plus, we can encourage a streamlined referral process to facilitate participant access to DSMES and to RD/RDN for initial and ongoing lifestyle and nutrition counseling.
Care Gaps for Young People, Ethnic Groups and Uninsured Populations
The study found that younger people, Mexican Americans, and persons without health insurance were more likely to be untreated when risk-factor targets were not achieved. These gaps are especially magnified in under-resourced areas.
In addition, given that the rates of diabetes-related complications are higher in people of color and uninsured populations and that type 2 diabetes discovered in young adulthood have a more aggressive clinical course than diabetes, immediate action is required to improve outcomes.
Coach Beverly suggested action: Diabetes Care and Education Specialists continue to take a leadership role in intentional and unrelenting outreach to provide DSMES and MNT to under-resourced communities using novel and evidenced-based approaches. Since prediabetes rates are also higher in many of these communities, establishing easily accessed Diabetes Prevention Programs and networking with community health workers and leaders can contribute to improved health outcomes.
Medications are too expensive for many people
Even though we have a slew of new and highly effective classes of diabetes medications, they are out of the financial reach for many. As patents expire and the medications are available as generics, access and affordability will increase. In the meantime, a realistic approach to providing affordable diabetes treatment is needed.
Coach Beverly suggested action:
Diabetes Care and Education Specialists can help craft a medication plan that is realistic and affordable. For people with no insurance or large co-pays, consider using available generic diabetes medications. These medications often cost $10 or less for a 3-month prescription. They include: metformin, sulfonylureas, and pioglitazone. In addition, Walmart offers Reli-On insulins including Regular, NPH, and 70/30 insulin for $25 a vial. There are also online resources like GoodRx.com that help people find discounts on their usual medications and the different pharmaceutical companies also offer discount programs based on need.
See Insulin Cost Savings Guide for an abundance of resources and useful links.
In conclusion, Diabetes Care and Specialists are perfectly positioned to influence health delivery systems and advocate for best clinical practices. We can be catalysts for establishing DPP and DSMES programs in under-resourced communities and advocate for access to affordable medications and technologies to help participants reach their targets for A1C, Blood Pressure, and Cholesterol while improving quality of life.
With a concentrated effort, maybe our next report card will be a little bit better!
With hope, Coach Beverly
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
A Radical New Approach to Diabetes Care – Vayu Health
Delivering person-centered high quality diabetes care to high-risk individuals with diabetes is no easy task in our current complicated health environment. We are excited to share our interview with Dr. Avni Shah, Founder of Vayu Health, and her vision to provide equitable diabetes care delivery for our most vulnerable populations. Dr. Shah and her team are proposing a radical new equity focused-approach to diabetes care. To learn more, read our interview below.
“Our vision is to transform the lives of under served Medicaid members living with multiple chronic conditions, behavioral health needs, and social determinants of health (SDOH) through a team-based approach to care that places people at the center of decisions about their own health. We are passionately driven to improve health, equity, and experiences for every person we work with, while also lowering costs,” said Dr. Avni Shah.
Dr. Shah says their care model is rooted in trusting relationships with patients, and also with the providers, community partners and health plans that they work with. To sustain vibrant, patient-centered programs they are designing a payment model that rewards their care team for doing the right thing at the right time for these vulnerable populations.
They believe that a major shift is needed in the way care is delivered for under resourced people living with chronic conditions, especially sub optimally managed diabetes, and are currently looking to build out their clinical team, including a Certified Diabetes Care and Education Specialist (CDCES) and a Licensed Clinical Social Worker (LCSW).
Interview with Dr. Avni Shah
1. What motivated you to leave a traditional work setting as a Peds Endo and take the risk to create a new health care model for Medicaid members living with diabetes?

- It is really about who the traditional healthcare work setting failed that motivated me to leave: 1) patients and families living with chronic conditions, especially the underserved 2) my teammates and 3) my conscience (ie my moral injury).
- We need something different and I believe it can be different. What we all need and strive for are: trusting relationships, joy in work and life, and direct translation of our work to better health and equity. We want to do what we know works, which is often not what can be supported and billed/paid in the traditional work setting.
2. What do you consider the biggest shortcomings in our current approach to providing diabetes care?
- Shortcomings that create barriers to doing what we know work are:
1) the lack of alignment of what success looks like between a patient, the health system, and the health plan plus
2) the lack of payment for your time (ie phone calls, home visits), needed innovations (ie virtual care, community integrations), and integrated team based resources (ie educators, coaches, behavioral specialists) to enable a personalized method for empowering patients to meet their goal(s).
3. Describe your future vision and model of diabetes care provision.
We believe that it is past time for a seismic change in chronic care management, especially for diabetes. Our primary-care based model is what is needed right now for people with diabetes and will include the following key components:
- Whole-person care, integrating medical, behavioral, social, and self-management care
- Team based approach including a local coach, CDCES, LCSW, and PCP
- High-touch and flexible interactions, both in-person and virtual
- Trauma-informed and culturally sensitive approach
- Focus on building trust and engagement by identifying a person’s self-identified goals and helping achieve them
- Utilize local community assets to address social determinants of health
- Read more below
4. Do you have a favorite quote?
I have many quotes I love, but none that are a favorite. So here are a few:
- You must be the change you want to see in the world. – Mahatma Gandhi
- What you do makes a difference, and you have to decide what kind of difference you want to make. -Jane Goodall
- I have found the paradox, that if you love until it hurts, there can be no more hurt, only more love. – Mother Teresa
- Seek first to understand, then to be understood. – Stephen Covey
What is Vayu’s Goal? To Spark a Fundamental Change in Diabetes Care Delivery
Vayu Health was started by physicians who work extensively with adults and children with not only diabetes, but other chronic conditions, behavioral health issues and social risk factors. Vayu’s team recognized that despite best efforts of providers and patients, of new drugs and technologies, and of increased spending, population health outcomes have not improved significantly over the last 20 years for individuals living with chronic conditions such as diabetes, especially for those with low incomes. COVID-19 has only intensified the call for change as it has disproportionately impacted individuals already marginalized by our healthcare system failures.
To address this urgent crisis, fundamental change in the healthcare system is needed and Vayu Health is poised to create this change.
Identifying System Failures and Building Solutions
To successfully build their model, Vayu first identified the healthcare system failures, cataloging the barriers to people with diabetes receiving the right care. They identified four key barriers that needed to be addressed:
- Right care at the right time: The healthcare system is not always known for flexibility or quick response time, and when serving large volumes of patients, can default to a one-size-fits-all approach. Individuals with chronic conditions however have a wide variety of needs depending on lifestyle, disease severity and the environment in which they live. The system must be able to match patients with the right care when and where they need it.
- Treating the disease, not the person: A person with diabetes likely also has other clinical, behavioral and/or social needs, yet the delivery system frequently treats just the diabetes. To effectively support people with diabetes, programs must also address social issues, self-management needs, behavioral care, looking at the whole person instead of just the condition.
- Lack of timely, accurate data: The healthcare system is composed of multiple parts and people, which commonly do not interact smoothly with each other. People with diabetes can see primary care providers, specialists, be admitted to hospitals and get lab work and prescriptions, and data from all of these entities are vital to tracking and managing their health and making informed decisions about their care.
- Payment for some things, not always the right things: Treatment for people with diabetes works best when a team works together, each person contributing to the top of their license. However, payment for services does not always cover the cost of each staff member, requiring providers and their teams to make tough choices about how much they can invest in a team-based model.
Vayu Health’s Innovative Model
Vayu Health is taking on each of these systemic barriers, and addressing them in a cohesive, person-centered care model. As Medicaid members disproportionately experience care failures, Vayu is focusing on Medicaid managed care patients, living with diabetes and other chronic conditions.
They are collaborating with one of California’s largest Medicaid managed care health plans and a California community health center to develop and integrate Vayu Health’s unique systems approach, including a new value-based payment that will incentivize doing the right thing at the right time for patients. This collaboration is the first step in a systematic shift in the way community primary care providers and patients experience care and the way that Medicaid managed health plans cover the costs.
In addition to the best practice chronic condition care model, a healthcare ecosystem will be developed which will incorporate the following system elements:
- Alignment across providers, health plans and providers on care model and payment
- Value-based payment to support the best practice care model (i.e. population based prospective)
- Appropriate target population
- Linkage of appropriate outcome and cost data
- Continuous improvement driven by quality improvement methodology
- Infrastructure/business financing needs
- Technology required to enable effective team care
Equity-focused start-up is looking for innovators to launch a new diabetes care model:
Vayu Health is a California non-profit set to launch a completely different care model for people with diabetes living in under served communities, and is looking for like-minded people passionate about equity, person-centered care, and reducing barriers to accessing high-caliber diabetes care.
If you love working in an innovative team environment, are excited by participating in creative programming for patients, and are an independent thinker and self-starter, this just might be the perfect opportunity for you.
The Vayu Team is looking for a CDCES and LCSW
The team is made up of people that are excited about building something new, and every team member regardless of role has a voice in creating the company. Vayu believes passionately in reducing barriers to care for vulnerable populations, and has a strong focus on equity. The care team includes local community coaches, certified diabetes educators, licensed clinical social workers, and community clinic physicians. With this multidisciplinary team, care delivery will be a combination of coordinated, proactive in-person and virtual care, delivered when and where the patient needs it.
Vayu has the commitment of the community clinic and Medicaid healthcare plan, as well as national experts in diabetes care, Medicaid managed care healthcare payment reform, and chronic care system design and optimization.
CORE TEAM:
- Avni Shah, MD, Pediatric Endocrinologist: Previous diabetes director at Stanford Children’s and faculty leader for T1D national quality improvement collaboration. Currently volunteer faculty at UCSF. She had gestational diabetes requiring insulin, has pre-diabetes, and has a strong family history of Type 2 Diabetes.
- Margie Powers, MSW, MPH: Design and implement population health initiatives for provider groups, health plans and self-insured employers across the country, with focus on serving Medicaid populations at Federally Qualified Health Centers in California. Previously Director of Medically Complex Patients Program at Purchaser’s Business Group on Health in San Francisco.
- Alan Glaseroff, MD, Family Practitioner (pro bono): Designed and led Stanford Coordinated Care (SCC) and Humboldt Diabetes Project which both showed significant improvement in outcomes, patient experience, patient activation, utilization, and costs. He has lived with Type 1 Diabetes since 1983.
- John Bertko, F.S.A., M.A.A.A. (pro bono): Actuarial consultant serving as the Chief Actuary with Covered California (California’s Insurance Marketplace). Past Director of Special Initiatives and Pricing in the Center for Consumer Information and Insurance Oversight at the Centers for Medicare and Medicaid Services (CMS) and Chief Actuary of Humana Inc.
This is an incredible opportunity to join a dynamic mission-driven company with visionary leadership and a bold and inclusive culture. Interested people should directly contact Margie ([email protected] or 415-225-4787).
See Full Calendar for upcoming webinars and Virtual Courses.
Can’t make it live? All paid registrants are guaranteed access to the video presentation, handouts and podcasts.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Living with Type 1 can be Tough. Embark can Help!
Managing diabetes can be tough! Something that people rarely talk about is how tough type 1 diabetes can be and how many people find diabetes to be stressful and challenging.
That’s why we are excited to share an opportunity for people living with type 1 diabetes to join a new NIH-supported study that is part of a collaboration between T1D Exchange and the University of California, San Francisco (UCSF).
Note from Coach Beverly
I have had the pleasure of working as an Embark facilitator for the past year.
I can personally share with you that this program offers so much meaningful hands-on problem solving and support for those who join. Participants not only receive practical information but gain valuable insights into approaches for self-care.
I highly recommend this program to anyone with type 1 diabetes who is feeling frustrated and tired and ready to make changes with the help of a supportive team!
Embark Program Details
The program begins with a group workshop (8-12 adults with type 1 diabetes) (held virtually online on a Saturday), followed by online video group meetings and/or individual phone calls with either a psychologist or Certified Diabetes Educator.
The program interventions are strictly behavioral, meaning that participants will not be asked to change or try any new medications or devices.
Participants will receive gift cards for their time and there are no costs to you or to your insurance. There is no age limit to taking part, you just need to be 19 years or older!
If you know people living with type 1 diabetes, please share this information with them. Our hope is that they will be interested in learning more about this exciting new program.
Research Participants Needed:
Are you…
– An adult (19 years +)
– Diagnosed with Type 1 Diabetes for at least 1 year
– Unhappy with your recent Hemoglobin A1C of 7.5% or higher
– Feeling overwhelmed, frustrated, “burned out” with living with diabetes
If you answered YES to the above questions, you may qualify to participate in EMBARK. The purpose of this study is to work compassionately to help you better manage your distress with diabetes and to reach your management goals.
More info on Embark Website
Or you can call: 1-855-850-3599 (toll free) or email us at: [email protected]. Thank you, UCSF EMBARK Team
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.












