Why adding GLP-1 RA or GIP/GLP-1 RA before Basal Insulin is Recommended
In the past, if a person with type 2 diabetes can’t get blood glucose to target on oral meds, the next action would be to add basal insulin. However, the latest guidelines, found in the ADA 2023 Standard 9, encourages providers to consider adding a GLP-1 RA or GIP/GLP-1 RA before writing that prescription for basal insulin.
Diabetes pharmacologic management has dramatically changed over the past few years with the addition of Incretin Mimetics (GLP-1 RA and GIP/GLP-1 RAs) and SGLT2i’s to the medication landscape. The pathways and algorithms have been adjusted to incorporate these newer medication options, which significantly lower glucose without the risk of low blood sugar or weight gain like insulin or sulfonylureas.
GLP-1 RA or GIP/GLP-1 RA versus Insulin Therapy
The truth is, insulin will always lower blood glucose levels, but users may experience the side effects of hypoglycemia and unwanted weight gain. However, for some people, adding insulin is still the next best step. According to the ADA Standard 9, “health care professionals should consider insulin as the first injectable when there is evidence of ongoing catabolism, symptoms of hyperglycemia and when A1C levels >10% or blood glucose levels are 300mg/dL or very high, or a diagnosis of type 1 diabetes is a possibility.”
Insulin can be easily titrated up or down, depending on glucose profile and users can fine tune dosing to match carb intake and other factors. Insulin has been around for over 100 years and has been extensively studied and it’s action and side effects are well understood.
In spite of these benefits, insulin does have some disadvantages. Insulin doesn’t have the same cardiovascular benefits as the GLP-1 RA’s or GIP/GLP-1 RA’s, nor does it contribute to weight loss. Let’s explore some of the benefits of starting with these “Incretin Agonists” before adding insulin therapy.
Benefits of starting Incretin Mimetics; GLP-1 RA’s or GIP/GLP-1 RA’s, before adding insulin therapy
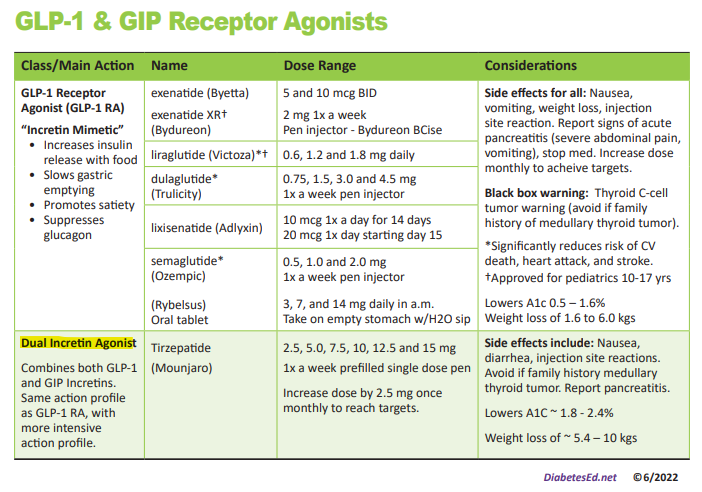
These 2 classes of incretin mimetics lower A1C from 1.6% to 2.4% when used at maximum dose, a significant glucose improvement. In addition, people experience weight loss that ranges from 6% to 13% when on maximum doses. (Please see PocketCard to the right and package inserts for more information)
Data from the CVOTs (Cardiovascular Outcomes Trials) demonstrate that three of the GLP-1 RAs (liraglutide, dulaglutide, semaglutide ) significantly reduce the risk of cardiac death, heart attack and stroke.
Given that the most people living with type 2 diabetes have elevated BMI’s and a high risk for CV disease, it makes sense, when feasible and clinically indicated, to start with GLP-1 RAs or GIP/GLP-1 RAs before initiating insulin therapy. Of course, when selecting GLP-1 RAs or GIP/GLP-1 RAs, we need to consider individual preference, insurance coverage, A1C lowering and weight-lowering effect and frequency of injection. In addition, for those on GLP-1 RA and basal insulin combination, we can consider using a fixed-ratio combination product (iDegLira or iGlarLixi) For more info on dosing and considerations for these two combination products, you can Download FREE Combo Injectable PocketCards.
For a step-by-step approach, please see the 2023 ADA Algorithm for Intensifying Injectable Therapy for People with Type 2 from ADA Standard 9. This algorithm provides a roadmap for health care professionals working to improve glucose levels for those living with type 2 diabetes.
When people with type 2 are not at their glucose targets using oral medications, we are encouraged to thoughtfully consider the next best pharmacologic injectable addition. Given the benefits listed above, the GLP-1RA and GIP/GLP-1 RA therapies may be the best choice for many people living with type 2 diabetes.
Thank you for collaborating with individuals to determine the next best step when needing to add injectables to their management plan. To learn more, you can view our recorded program, Meds for Type 2 Update; New ADA/EASD 2023 Consensus Statement.
We retyped this ADA Standards algorithm in a larger font and on 2 pages, to make it easier to read for studying and so you can post on the wall of your clinical practice.
View ADA 2023 Standard 9, Pharmacological Approaches to Glycemic Treatment here.
Celebrating Martin Luther King Jr. – A Day of Service and Reflection
“Everyone can be great, because everyone can serve”
While the celebration of Dr. King is global, its spirit is local. As Dr. King said, “Everyone can be great, because everyone can serve” and there is no better way to honor his legacy than through individual and community service.
As Diabetes Specialists, we honor Dr. King’s words by serving people living with prediabetes and diabetes. We advocate for affordable diabetes care, medications, and access to nutritious foods.
We are fully aware that people with diabetes are more likely to struggle with food insecurity, social and financial inequities and lack adequate resources to pay for medications and diabetes supplies. We know that there is still much work to be done. During these challenging times, I am comforted by Dr. King’s resonant statement “The arc of the moral universe is long, but it bends toward justice.”
On this day of national celebration and service, we thank Dr. King for being a beacon of light and clarity with his call to action that still resonates today.
With Gratitude,
Coach Beverly
Sign up for Diabetes Blog Bytes – . It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]New Lipid Goals for Higher Risk Individuals
If you are taking the CDCES or BC-ADM exam in 2023, these new lipid targets for high risk individuals and treatment interventions are important to know.

For all of us who serve people with diabetes, evidence from many trials demonstrated that these more intensive LDL cholesterol targets will save lives and decrease CV disease. By sharing this information with our colleagues and teams, we can be a part of improving outcomes and quality of life.
The following content summarizes the 2023 updated ADA guidelines as outlined in Standard 10 – Cardiovascular Disease and Risk Management.
New LDL Treatment Targets for Higher Risk Individuals
Primary Prevention – People without ASCVD
The guidelines have remained the same for lower risk individuals with diabetes aged 40–75 years without atherosclerotic cardiovascular disease, “Start moderate-intensity statin therapy in addition to lifestyle therapy”. They also are the same for people with diabetes aged 20–39 years with additional atherosclerotic cardiovascular disease risk factors, “Based on individual assessment, initiate statin therapy in addition to lifestyle therapy.”
More Intensive LDL for High Risk Individuals
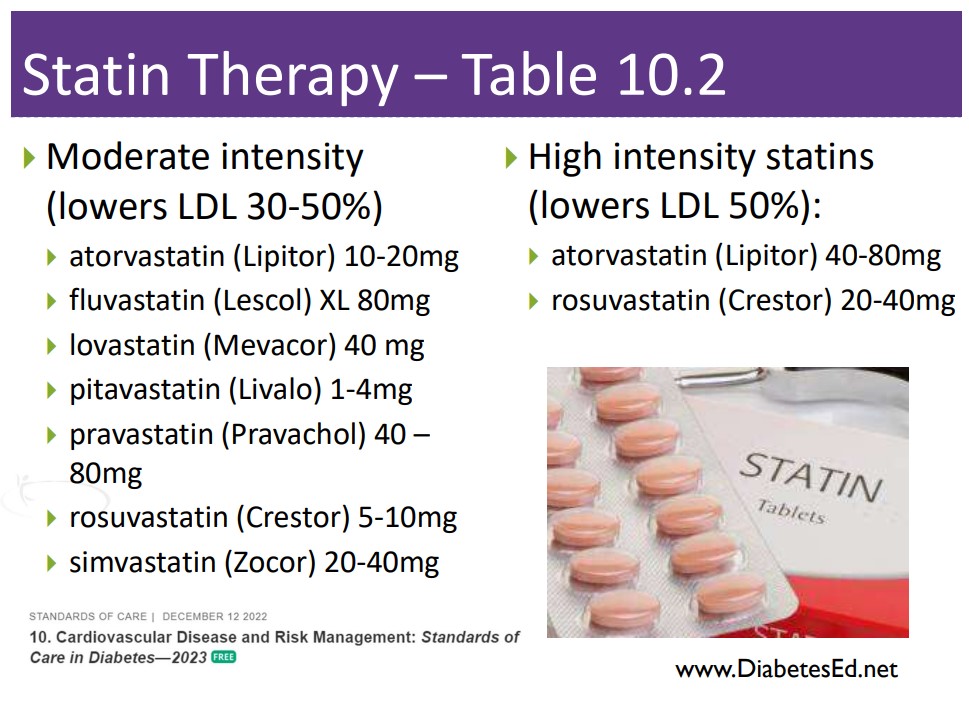
In the category of primary prevention for people with diabetes aged 40–75 at higher cardiovascular risk (LDL >100, HTN, Smoke, CKD, albuminuria, family hx ACSVD), the goals have been intensified.
- High-intensity statin therapy is recommended to reduce LDL cholesterol by at least 50% of baseline and to target an LDL cholesterol goal of <70 mg/dL.
- For people with diabetes aged 40–75 years at higher cardiovascular risk, especially those with multiple atherosclerotic cardiovascular disease risk factors and an LDL cholesterol of 70 mg/dL or greater, it may be reasonable to add ezetimibe or a PCSK9 inhibitor to maximum tolerated statin therapy.
More Intensive LDL Goals for People with Atherosclerotic Cardiovascular Disease:
Secondary Prevention goals have also been intensified.
For people of all ages with diabetes and atherosclerotic cardiovascular disease:
- Add high-intensity statin to lifestyle therapy.
Target LDL cholesterol reduction of 50% or greater from baseline and an LDL cholesterol goal of <55 mg/dL.
Addition of ezetimibe or a PCSK9 inhibitor with proven benefit in this population is recommended if goal is not achieved on maximum tolerated statin therapy.
In 2022, the ADA Standards did not include specific LDL targets for people with diabetes. However, based on recent study results, the committee updated the 2023 guidelines to reflect the latest research findings. To learn more about the study findings, Standard 10 – Cardiovascular Disease and Risk Management.
Cholesterol Medication Cheat Sheets
Keeping track of medications for hypertension and cholesterol can seem daunting. We have put together a Lipid Medication Cheat Sheet along with summary information for each class that is important to know for certification exams and is very useful in clinical practice.
Lipid and Hypertension Medication Cheat Sheet
Getting LDL to Target Matters
Together, we can improve the quality of life and outcomes for people living with diabetes. Getting LDL cholesterol levels to target is an important interventions to maintain health. Thank you for reading this article and advocating for the best evidence-based care.
Want to learn more about this question? Join us for our
Level 2 | ADA Standards of Care CE Course | 2.0 CEs
Updates air live between Feb. 2, 2023, at 11:30 am PST
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
- List significant changes and updates to the 2023 ADA Standards of Medical Care.
- State 3 updates on new blood pressure and lipid goals.
- Identify 5 key elements of the position statement.
- Discuss how to apply the Standards in the clinical setting and in preparation for exam success.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Studying for the CDCES Exam? Enroll in our
CDCES Deluxe Prep Bundle | 30+ Online Courses + Bonus Items | 47 CEs
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Included in this bundle
- Level 1 focuses on the fundamentals and introduces each topic area for the exam.
- Level 2 deep dives into the ADA Standards of Care,
- Level 3 AKA Boot Camp is a more accelerated level that focuses on test simulation for finding the best answer to get you to the finish line of your study path.
- Technology Toolkit which gives information on pumps, sensors, and calculations,
- Test Taking Toolkit includes over 220 practice questions for test simulation plus a webinar where Coach Beverly provides test-taking tips based on her experience taking the certification exam six times.
- ADCES Review Guide for the Diabetes Care and Education Specialist Exam – 5th Edition – Revised – The ADCES Review Guide is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam. This book includes 480 + multiple-choice questions and strategies for preparing for and taking the exam with an answer key with rationales for all questions!
- Medication PocketCard – Our four-sided medication accordion Pocketcards were designed by Coach Beverly Thomassian to assist in clinical practice and exam preparation.
- Tote Bag
Enroll now | $499
Can’t afford Insulin? Strategies that can help
The cost of insulin is a real problem. According to an analysis of data from the CDC’s 2021 National Health Interview Survey, 1.3 million Americans with diabetes, or 16.5% of insulin users in the U.S. rationed their insulin in the past year due to the high costs of this life-saving hormone.
Insulin rationing is more common in adults under the age of 65, middle-income individuals, and Black Americans. This lack of insulin results in chronic hyperglycemia, intensifying the risk of diabetes-related complications, worsening quality of life, and can even lead to hospitalization and death.
In the 2021 National Health Survey, 16.5% of respondents living in the US, rationed insulin in the past year.
The retail price for a box of insulin pens (1,500 units) is about $500. A vial of insulin (1000 units) varies from $160 to $400. For this reason, many insulin companies offer coupons or biosimilar versions of certain insulins. However, these cost savings aren’t enough for many individuals.
Hopefully, the 2022 Inflation Reduction Act, will at least improve insulin access for seniors with Medicare by limiting insulin copays to $35 per month. However, a similar cap for the privately insured was removed from the bill, and copay caps do not aid the uninsured. Further reform is needed to improve access to insulin for all Americans.
Why is insulin so expensive?
According to a very compelling article published by USC, the insulin distribution intermediaries, or Pharmacy Benefits Managers (PBMs), are significantly contributing to increasing insulin costs.
A USC cross-sectional study of the U.S. insulin market was conducted in 2020 using 2014-2018 data from multiple sources. The study analyzed the flow of funds throughout the insulin distribution system which includes manufacturers, drug wholesalers, pharmacies, health plans, and (PBMs).
According to the USC study, in 2014, 70% percent of insulin revenue was going to the manufacturers and 30% of the insulin revenue went to the PBM middlemen, but by 2018, only 47% was going to the manufacturers. The intermediaries—mostly PBM’s and pharmacies–were pocketing the rest, a whopping 53% share of the revenue from insulin sales.
In light of this complicated insulin distribution system, more needs to be done to uncover these issues and get to the root of unaffordable insulin for the millions of people who rely on it every day.
Here are different strategies to access affordable insulin.
Until we get a handle on the cost of insulin, here is some helpful information and programs that can make insulin more affordable.
Insulin Affordability Guide from ADCES
Insulin Affordability Guide helps make navigation easier ADCES Access & Affordability page with Insulin Cost-Savings Resource Guide. Insulin Cost Savings Guide
ReliOn Insulins $25 a Vial
Walmart and some other pharmacies also offer ReliOn insulins. These include Novolin R, Novolin N, and Novolin 70/30. For people with type 2 diabetes and some with type 1, these insulins offer an affordable option. They are only $25/vial or $44/5 pack of pens and do not require a prescription in most states. Access to these insulins can be truly life-saving in some circumstances. Every person with diabetes needs to be aware that they can purchase these insulins without a prescription if they are ever out of insulin.

Other Options
Generic Insulins
Because insulin is a biologic drug, a true generic must come from the same manufacturer. Recently Lilly and Novo Nordisk have created generic insulins.
Lilly offers generics of insulin lispro, insulin lispro mix 75/25, and insulin lispro junior kwik pen.
Novo Nordisk offers generics of their insulin, which they are calling a “follow on Brand” and includes insulin apart and insulin Aspart mix 70/30.
Both Lilly and Novo offer approximately 50% cost savings from the original insulin product and the pharmacist can make an automatic substitution if you ask.
Co-Pay Cards
Most insulins offer a co-pay card which can bring down the price of insulin most commonly to $0 to $25/month depending on the manufacturer and type of insulin. For any person with a commercial insurance plan, it’s good to check if a co-pay card is available for the insulin before picking it up from the pharmacy.
The things to be aware of about these cards are that they have maximum savings and sometimes that is much less than the total cost of the insulin. Also, they only work for people with commercial insurance meaning they won’t for people without health insurance or that have a government insurance plan like Medicare. They also do not always work if the drug is not covered by the insurance plan. In that case, it would be preferable to switch to insurance covered by the insurance plan.
Assistance Plans
These are programs offered through pharmaceutical companies for people without health insurance or that have Medicare but still struggle to pay for medications. There are various income requirements to be eligible, but depending on the program it can be 250-400% above the Federal poverty line. Many people are surprised to find that they are eligible, so this is a good option to look into which can make insulin completely free. There is typically a packet of information that needs to be completed and then if eligible, the insulin is shipped to the prescriber’s office for the patient to pick up.
In summary, more needs to be done to make insulin more affordable. As diabetes specialists, we can write to our congresspeople and advocate on behalf of people living with diabetes, to ensure that people no longer have to ration insulin.
References
- ADA Standards of Care – Standard 9, the chart on Average Wholesale Price of Insulin
- Annals of Internal Medicine – Prevalence and Correlates of Patient Rationing of Insulin in the United States: A National Survey, Adam Gaffney, MD, MPH, David U. Himmelstein, MD, Steffie Woolhandler, MD, MPH
- CNN Report on Insulin Rationing
Insulin prices are skyrocketing, but just who is driving the rise in costs? Hint: it’s not the drug manufacturers – USC - For a summary of all this information, see the ADCES Insulin Cost Savings Resources Page.
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Warning – Alcohol can Blunt Impact of Glucagon Rescue Meds
LS tells you that they frequently attend company mixers where they feel compelled to have at “least a few drinks”, to fit in and network. The tricky part of this scenario is that LS lives with type 1 diabetes. Since they don’t have a working pancreas, their circulating levels of insulin and glucagon are often mismatched to their body’s needs.
When discussing the situation, LS says they feel confident they can handle alcohol and prevent lows since they have lived with type 1 diabetes for over ten years. LS shares, “I feel comfortable recognizing when both arrows are pointing down and I am heading for a glucose crash”.
As educators, we are committed to taking person-centered approach while encouraging safe practices.
In regards to LS, we realize alcohol’s impact on the thought process and blood glucose levels. We know that alcohol can affect critical thinking and possibly impair recognition of an impending hypoglycemic event. Inebriation also has many symptoms in common with hypoglycemia. Plus, alcohol consumption slows glycogen breakdown in the liver, which increases the risk of hypoglycemia. Lastly, based on a study published in Endocrinology Advisor, higher levels of alcohol in the blood can delay and blunt the effectiveness of glucagon rescue medications.
In the worst-case scenario, if LS experiences severe low blood sugar and passes out, alcohol ingestion can blunt the effectiveness of the glucagon rescue medications.
Alcohol and Glucagon Pathophysiology Review
The body considers alcohol a toxin and as soon as it reaches the bloodstream, the liver prioritizes metabolizing the alcohol and breaking it down. During this clean-up process, the liver is distracted from responding to endogenous glucagon, the hormone that signals the liver to break down glycogen for energy and liberate glucose into the bloodstream. This clean-up can last for up to 8 hours, making delayed hypoglycemia a real possibility.
When a person with type 1 diabetes drink alcohol, they at increased risk of hypoglycemia because the liver isn’t breaking down stored glycogen to increase blood glucose levels.
Let’s get back to LS. What if LS is drinking gin and diet tonics and only munching on low-carb vegetables and cheeses during the mixer? LS is not ingesting many carbohydrates, so glycogen stores may be low and the liver is busy cleaning up the alcohol and blood sugars start dropping. By the 4th drink, LS isn’t thinking very clearly, says they “feel funny” and passes out.
A colleague of LS carries a glucagon emergency kit and provides LS with a dose and calls 911. After 15 minutes, LS still hasn’t regained consciousness, so a second dose is administered. The paramedics arrive and check the glucose, it is 53.
Simply put, glucagon rescue medications may not work if the person drinks too much alcohol.
After reviewing the package inserts of all available US manufactured Glucagon Rescue Meds, there are no warnings for alcohol intake decreasing the effectiveness of glucagon rescue meds. So, I dug a little deeper and found a decent study on the topic which describes the impact of alcohol ingestion on glucose-regulating hormones.
I also found a very helpful monograph published by Lilly Baqsimi in Canada. Baqsimi is a powdered glucagon rescue medication that is delivered nasally. The Baqsimi monograph clearly states several warnings, “Alcohol can suppress hepatic gluconeogenesis and chronic alcoholism can deplete liver glycogen stores. Therefore BAQSIMI may be less effective in presence of acute or chronic alcohol ingestion. Alcohol-induced hypoglycemia is associated with a failure of blood glucose levels to rise normally after glucagon administration. BAQSIMI may not work if the person drinks too much alcohol.“.
Keeping it Real and Safe
In conclusion, having a conversation with people with type 1 about the suppressive nature of alcohol on glycogen release for many hours after consuming alcohol is very important. Another important teaching point is that glucagon rescue meds may not be as effective and timely in raising glucose to safe levels.
As a general rule of thumb, encouraging people with type 1 to eat 15gms of carbs with each drink and have a glass of water in between, may help make sure they have enough circulating carbs and slow the pace of alcohol consumption to help the liver with processing. They may also consider decreasing their insulin dose in association with alcohol intake to prevent this serious side effect.
Download our Glucagon Rescue Med PocketCard for more information here.
Want to learn more about Diabetes Care? Join us for our
Virtual DiabetesEd Specialist Conference
30+ CEs
Airs October 12-14th, 2022
Join us LIVE for this Virtual Course and enjoy a sense of community!
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice.
Download Course Flyer | Download Schedule
If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
Two Registration Options
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
New Injectable – “TwinCretin” on Printed PocketCards
We have just added this novel, first in class, dual incretin hormone therapy, Tirzepatide (Mounjaro), to our printed version of our Diabetes Medication PocketCard.
This new twin therapy includes not only a GLP-1 Receptor Agonist, but also a Glucose-dependent insulinotropic polypeptide (GIP), which magnifies the therapeutic effectiveness. The SURPASS studies indicate that study participants experienced an A1C drop of up to 2.5% and weight loss of up to 10kg or more.
How does it work?

Incretins (GLP-1 and GIPs) play a major role in glucose regulation post prandially. Incretins are gut hormones that stimulate insulin release from the pancreas when glucose rises in response to food ingestion. They keep blood sugars in check as well as activating the satiety center, to increase the sense of fullness. Incretins slow gastric emptying and also curb post-meal glucagon release, decreasing post prandial glucose spikes. Unfortunately, people with type 2 diabetes, make less than half of the usual amount of the GLP-1 and GIP hormones, which contributes to chronically elevated glucose levels.
To date, therapies that have only included the Glucagon-Like Peptide-1 (GLP-1) have demonstrated major success in managing Type 2 DM.
By creating a formulation with BOTH the GIP and GLP incretin hormones, the A1C lowering and weight loss effectiveness has been significantly amplified.
First in Class – Dual Incretin Injectable Therapy
Tirzepatide is a novel synthetic peptide, engineered to provide a once-weekly injectable medication that acts on glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptors.
Tirzepatide has been granted FDA approval for treatment of type 2 diabetes based primarily on a series of trials known as SURPASS. The SURPASS 1 trial compared increasing doses to evaluate dose response. The SURPASS 2-5 Trials compared tirzepatide to the GLP-1 semaglutide and to the basal insulins degludec and glargine. In all of the trials, the findings were impressive.
Summary of SURPASS Trials and Results based on Tirzepatide Package Insert.
- SURPASS -1 Dose efficacy study ranging rom 5 to 15 mg, evaluating A1C and weight loss. Up to 85% of participants on tirzepatide achieved an A1C of less than 7%. A1C drop of 1.7% with 15mg dose. Weight loss of up to 7.8kgs.
- SURPASS-2 Compared tirzepatide with patients on metformin to semaglutide. Up to 86% of participants on tirzepatide achieved an A1C of less than 7%. A1C drop of 2.3% with 15mg dose. Weight loss of up to 11.2 kgs.
- SURPASS-3 Compared tirzepatide with patients on metformin, with our without an SGLT-2 Inhibitor to Insulin degludec. Up to 83% of participants on tirzepatide achieved an A1C of less than 7%. A1C drop of 2.1% with 15mg dose and weight loss of up to 11.3kgs.
- SURPASS-4 Compared tirzepatide with people on metformin, and/or sulfonylureas and/or SGLT-2s with Insulin Glargine in people with increased cardiovascular risk. Up to 85% of participants on tirzepatide achieved an A1C of less than 7%. A1C drop of 2.4% with 15mg dose and weight loss of up to 10.6 kgs.
- SURPASS-5 Compared tirzepatide vs placebo in people taking Insulin glargine with or without metformin. Up to 90% of participants on tirzepatide achieved an A1C of less than 7%. A1C drop of 2.4% with 10mg dose and weight loss of up to 10.5kgs.
Tirzepatide (Mounjaro) Indications and Dosing
This once a week injectable is for adults with type 2 diabetes as an adjunct to diet and exercise to improve glycemic control and support weight loss. Tirzepatide is delivered with a single dose prefilled pen.
Starting Dose: 2.5 mg SC every week for 4 weeks initially; THEN increase to 5 mg SC every week. If additional glycemic improvement is needed, increase by 2.5-mg increments after at least 4 weeks at current dose.
Note: The initial 2.5-mg dose is intended for treatment initiation and is not effective for glycemic control
Maximum dose: 15 mg SC qWeek
Common Adverse Side effects: Nausea, diarrhea, abdominal discomfort and injection site hypersensitivity reactions. There is also a black box warning to avoid if family history of medullary thyroid tumor and to report any signs of pancreatitis immediately.
Cost: Tirzepatide is comparably priced to other GLP-1 RAs on the market at $974.33 for four weekly doses, regardless of dose size. Hopefully, insurance companies will recognize the long term benefits of these newer classes of agents, and increase coverage of these beneficial treatment options.
In conclusion: This new medication class substantially lowers blood sugars and body weight, with a once a week injection. Coupled with healthy eating and keeping active, people with diabetes have the opportunity to improve their health and quality of life with this novel medication class.
Author’s note: Beverly Thomassian has no conflict of interest to report and distilled the content of this article from the SURPASS study results and the tirzepatide package insert.
*PocketCardsTM are for individual use only.
High Dose Ozempic Superior at Dropping A1c & Body Weight
The injectable GLP-1 semaglutide (Ozempic) can now be dosed up to 2.0mg a week. This higher maximum dose provides greater reductions in body weight (6.9kgs vs 6.0kgs) and A1c (2.2 vs 1.9% ) when compared to 1.0 semaglutide dose. There was a comparable safety profile with both doses. However, more people experienced negative gastrointestinal side effects when receiving the higher dose (34% compared to 30.8%).
This is good news for people with type 2 diabetes who would like to benefit from both A1C and weight reduction. Plus, semaglutide lowers the risk of cardiovascular events.
Without insurance coverage, this medication costs about $1000 for a month’s supply. However, since semaglutide (Ozempic) is an established diabetes medication covered by many insurance plans, we are hopeful that people who would benefit from this therapy will have access to this higher dose.
The SUSTAIN FORTE trial lasted for 40-weeks and enrolled 961 patients with type 2 diabetes with an A1C of 8.0-10.0%. All patients in the trial initiated treatment with a 0.25 mg dose of semaglutide that was doubled every 4 weeks until the target dose was achieved.
In addition to reduction in A1C and body weight, the semaglutide 2.0 mg arm of the trial saw a greater proportion of patients achieve an A1C less than 7% (67.6% vs 57.5% [OR, 1.60; 95% CI, 1.21-2.13; P=.001]) or a body weight reduction greater than 5% (59.2% vs 51.3% [OR, 1.41; 95% CI, 1.08-1.84]) than the semaglutide 1.0 mg arm.
We have updated our Diabetes Medication PocketCard with this higher maximum dose or our website, CDCES Coach App, and printed PocketCards.
Studying for the CDCES Exam?
Enroll in CDCES Online Prep Bundle + 5th Ed ADCES Review Guide Book | 47 CEs
This bundle includes our CDCES Online Prep Bundle plus the ADCES Review Guide.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
What is a Certified Diabetes Care and Education Specialist?
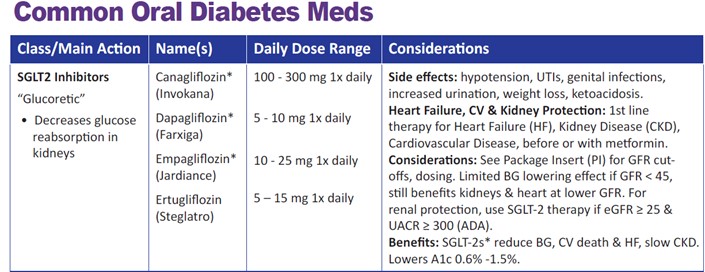
Read More: What is a CDCES? First awarded in 1986, as Certified Diabetes Educator (CDE) credential and in 2020 with a new name: Certified Diabetes Care and Education Specialist (CDCES) to more accurately reflect the specialty. CDCES has become a standard of excellence for the delivery of quality diabetes education. Those who hold this certification are known to possess comprehensive knowledge of and experience in diabetes prevention, management, and prediabetes. “Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.“ Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 10% of people in the U.S. have diabetes and another 35% have pre-diabetes which means 45% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company. Diabetes medications are not just about glucose management anymore In the past, to determine the right medication for an individual, the primary focus was placed on the glucose-lowering impact. However, with the introduction of the SGLT-2 Inhibitors and GLP-1 RA’s, there has been a tremendous leap forward and expansion of expectations for the co-benefits of diabetes medications. The SGLT2s and GLP1’s, are both associated with weight loss without the fear of hypoglycemia. They decrease the risk of cardiovascular events and also offer renal protection. In addition, the SGLT-2s are so effective at treating heart failure (HF), that they are now being used for people with HF without diabetes. Keeping close tabs on UACR and GFR A big shift in determining the optimal diabetes treatment now includes thoughtful evaluation of Urinary Albumin Creatine Ratio (UACR) and GFR. In the past, we collected UACR and GFR yearly to monitor kidney function. Now we use the results of these tests to determine not only kidney function but the risk of heart disease and the best therapy for diabetes, kidney health, and hypertension. Now, more than ever, we are compelled to evaluate urinary labs to determine the albumin to creatinine ratio and keep a close eye on GFR to determine best practices to not only extend lifespan but improve healthspan. For more info on UACR and GFR, see our blog post, “From Dipsticks to GFR – How to evaluate kidney function“. Our updated Medication PocketCards reflect these shifts In this latest version available for download and purchase, we have expanded and clarified the SGLT-2 considerations to reflect the changes in the 2022 ADA Standards of Care. We recognize that SGLT2 Inhibitors may be used as first-line therapy due to their additional benefits, “Along with metformin, SGLT-2s may be considered at first line diabetes therapy, especially for those with heart and kidney failure.” Since this class also slows the progression of chronic kidney disease, we also added, “for renal protection, use SGLT-2 Therapy if eGFR greater than or equal to 25 and UACR greater than or equal to 300.” Since the GFR cut-offs for this med class are changing frequently, we removed the GFR guidelines for individual SGLT2’s and encourage users to review the package insert for the most recent recommendations. Over the past twenty years, there has been tremendous expansion in the availability of diabetes medications that not only lower glucose but help decrease the progression of common diabetes co-comorbidities. In this evolving medication landscape, our Medication PocketCards capture the critical and current information you need for your clinical practice and certification exams. Coach Beverly will highlight the key elements of the latest Medication Guidelines by AACE and ADA. We will explore clinical factors to consider when determining the best strategy to improve glucose management in people with type 2 diabetes and other co-conditions. There will be a special focus on cardiovascular risk reduction and renal protection. Objectives: Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. If you are seeking a state-of-the-art review of current diabetes care, this course is for you. Our team has been fine-tuning this course for over fifteen years, and we know what you need. This program can also be a great addition to your CDCES or BC-ADM exam study plan. Download Course Schedule | Download Course Flyer Join us LIVE for this Virtual Course and enjoy a sense of community! Team of expert faculty includes: Download Course Schedule | Download Course Flyer Deluxe Option for $499: Virtual Program includes: Deluxe Version includes Syllabus, Standards and Swag*: Deluxe Option for $499: Virtual Program includes: Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University. All hours earned count toward your CDCES Accreditation Information Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below! The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE. 
Why become a CDCES?
Three Reasons from Coach BeverlyDiabetes Meds do more than Lower Glucose & PocketCard Updates
PocketCards Update
Want to learn more about this topic? Enroll in our
Meds Management for Type 2 Standards | 1.5 CEs
Recorded & Ready to Watch!
Join us for our Virtual DiabetesEd Specialist Conference
30+ CEs | April 13-15, 2022Two Registration Options
Virtual DiabetesEd Specialist Conference Deluxe | 30+ CEs
Virtual DiabetesEd Specialist Conference Basic | 30+ CEs