Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Hormone Replacement Therapy Warnings Removed
By: Astraea Ballinger and Beverly Thomassian

Hormone Replacement Therapy (HRT) is an important topic of conversation due to its vast untapped benefits for women and people with uteruses. Due to a two decade misinterpretation of study results and black box warnings, HRT has been mostly denied as an intervention for individuals who could benefit from treatment.
Flaws in the Women’s Health Initiative Study
In the early 2000s, prescriptions for HRT products dropped significantly due to the FDA’s addition of black box warnings. The application of the black box warnings stemmed from a Women’s Health Initiative (WHI) study that warned of a significantly increased risk of breast cancer diagnosis for those using HRT. These findings were later shown to be inaccurate or overstated, but the initial conclusions caused long-lasting caution, leading to many years of limited progress and underutilization of HRT therapy.
Say goodbye to the Black Box Warning and Hello to HT
There is a renewed recognition of the benefits of hormone therapy. According to the recent press release on November 10th, the FDA is removing the boxed warnings following a comprehensive review of the scientific literature by an expert panel. The FDA is working with companies to update language in product labeling to remove references to risks of cardiovascular disease, breast cancer, and probable dementia. The FDA is not seeking to remove the boxed warning for endometrial cancer for systemic estrogen-alone products.² Of course, ongoing studies are needed to monitor long term safety and efficacy of hormone therapy.*
Of note, many menopause specialists are now using the term Hormone Therapy (HT) instead of HRT. The reason being that the goal is not to replace hormones to premenopausal levels – just to add back enough hormones to reduce symptoms and prevent other chronic conditions. HT is also a broader term that includes replacement of hormones or using hormones to treat a disease.
Benefits of Hormone Therapy (HT)*
- Randomized studies show that individuals who initiate HT within 10 years of the onset of menopause (generally before age 60) have a reduction in all-cause mortality and fractures.
- FDA-approved HT containing estrogen and progesterone (or estrogen alone as indicated for postmenopausal individuals) can restore declining hormones, and relieve symptoms such as hot flashes, night sweats, sleep disturbances, and bone loss.²
- Estrogen is a key hormone for women and people with uteruses’ health. Every single part of the body depends on estrogen to operate at optimal levels—including the brain, bones, heart, and muscles.
- Women and people with uteruses who use HT reduce their risk of:
- Cardiovascular diseases by as much as 50%,
- Cognitive decline and Alzheimer’s disease by 35%.*
- Bone fractures by 50 to 60%.
- Estrogen also helps collagen production, and collagen disappears from the vulva by up to 30% in the five years after menopause. ³
- Vaginal estrogen can be used by most breast cancer survivors, too, and it’s a win-win on the physical intimacy front.
- Vaginal estrogen can be used alongside HT.³
- Oral vs. Transdermal: Transdermal estrogen is associated with a lower risk of venous thromboembolism (blood clots) compared to oral HT because it avoids first-pass metabolism in the liver.
Cancer Considerations with Hormone Therapy
For individuals with a history of hormone-sensitive conditions like certain breast cancers, non-hormonal options are often recommended. While the general recommendation is to avoid systemic HT for people with breast cancer history, some experts are calling for a more personalized approach, suggesting that for certain individuals with severe symptoms, a risk-benefit assessment might be considered, especially if non-hormonal treatments have failed.
*Limitations & Uncertainties:
Due to the longstanding limited use of HRT, data from ongoing and future longitudinal studies will provide additional evidence about the risks/benefits of long term HT treatment. Careful consideration of individual factors need to go into making decisions to pursue HT (including, age, comorbidities, health history, current medication etc.) As with any therapy there can be potential risks associated with HT use.
More upcoming approvals for HT
In addition to the removal of boxed warnings, the FDA is also approving two new drugs to expand treatment options for menopausal symptoms. The first is the approval of a generic version of Premarin (conjugated estrogens), the first such approval in more than 30 years for this widely used form of hormone replacement therapy. The new generic product is expected to improve affordability and access while maintaining the same quality, safety, and effectiveness as the brand-name drug.
The second approval is for a non-hormonal treatment for moderate to severe vasomotor symptoms, such as hot flashes, associated with menopause. This option provides relief for women who cannot or choose not to use hormone therapy. ²
HT and Urinary Tract Infections (UTI)
More than half of people with uteruses will have at least one UTI in their lifetime. One in four women and people with uteruses have a UTI strain resistant to certain common antibiotics. Younger women and people with uteruses do suffer from infections, dehydration and post-sex cystitis, but the brunt is borne by older women. UTI rates shoot upwards when women hit 45 and are perimenopause. Plus, lack of estrogen means the lactobacilli and other good bacteria in the vaginal microbiome are at risk of being replaced by pathogenic ones.
SGLT-2 Reduction of UTI with estrogen
Estrogen deficiency after menopause is an important predisposing factor for reoccurring UTIs (r UTI). Another recent study in 2020 was designed to observe the risk and frequency of UTI due to SGLT2 Inhibitors among post-menopausal individuals with T2DM and the preventive effect of vaginal e HRT for r UTI among them.
Study Design: Forty-two, post-menopausal individuals with type 2 diabetes, using vaginal e HRT were selected as cases whereas controls were 38 matched individuals not using e HRT. Subjects in both groups were prescribed SGLT2 I considering eligibility and simultaneously adjusted the doses of other OHA’s or insulin to maintain the glycemic targets. They were targeted to follow for 12 months and evaluated periodically for symptomatic UTI and maintenance of glycemic targets. Diagnosis of symptomatic UTI was made using standard definition and guidelines.
The results? The 42 participants who were using vaginal e HRT compared to the 38 who did not use e HT, demonstrated significantly lesser frequency of UTIs. Estrogen HT after menopause significantly reduces the frequency of UTI among people with type 2 diabetes using SGLT2 I. Or said in another way, not using eHT for those with diabetes on SGLT-2I may significantly increase risk of complicated UTI.¹
Genitourinary Syndrome of Menopause (GSM)
The estrogen hormone deficiency associated with menopause has been renamed Genitourinary Syndrome of Menopause (GSM). This describes the chronic decrease in estrogen levels, resulting in a combination of genital, sexual, and urinary symptoms. While most common after menopause, GSM can affect premenopausal women experiencing low estrogen levels due to other medical conditions or treatments. This syndrome is associated with the hormone estrogen leaves the vulva dry in menopause (and sometimes post-pregnancy), a condition previously called “vaginal atrophy.”
Case Study Highlighting HT Benefits for GSM
In a recent 2020 case study, a 64-year-old woman (MS) was referred for recurrent urinary tract infections (UTIs). She presented with progressive complaints of vaginal dryness, sensitivity, and pain at the introitus with associated dyspareunia despite the use of over-the-counter vaginal lubricants. MS was offered treatment with vaginal estrogen therapy for her GSM.
For relief, MS was initiated on a 2-week course of nightly estradiol cream followed by maintenance therapy twice weekly. She returned for a 3-month follow-up and reported significant improvements in vaginal dryness, with resolution of her introital irritation and dyspareunia. She had not had a UTI in this time frame. MS also reported significant improvements in her quality of life and sexual function. 4
Both the lower urinary tract in women and the vaginal and introital tissues are rich in estrogen receptors. We can prevent GSM in perimenopause and menopause by giving individuals a safe, low dose of vaginal estrogen, which plumps the tissue, feeds the vaginal microbiome and reduces UTIs by 50%.²
Effective care of women and people with uterus’s is enhanced by gaining knowledge and being aware of current recommendations for treating both menopausal symptoms in general and GSM. 4
There are currently 7 FDA-approved vaginal estrogen products for the treatment of GSM. Shared decision making to determine the best choice of vaginal estrogen product is important and can improve satisfaction with therapy. ¹
Let’s Get the Word Out!
As healthcare professionals caring for people with diabetes, we can discuss the benefits for HT for individuals in perimenopause and menopause. We can also advocate for use of vaginal estrogen for individuals experiencing frequent UTIs, especially for those taking SGLT-2 inhibitors.
References
- ASHISH GAUTAM, PRABHAT K. AGRAWAL, NIKHIL PURSNANI, RUCHI RANI; 140-LB: Effect of Vaginal Estrogen as Hormone Replacement Therapy for Menopause on SGLT2 Inhibitor–Associated Urinary Tract Infection: A Prospective Cohort Study. Diabetes 1 June 2020; 69 (Supplement_1): 140–LB. https://doi.org/10.2337/db20-140-LB
- FDA. (2025, November 10). HHS advances women’s health, removes misleading FDA warnings on hormone replacement therapy. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy
- Muir, K. (2023, December 17). “Millions of women are suffering who don’t have to”: Why it’s time to end the misery of UTIs. The Guardian. https://www.theguardian.com/society/2023/dec/17/millions-of-women-are-suffering-who-dont-have-to-why-its-time-to-end-the-misery-of-utis
- Rosenblum, N. (2020, December). Update in female hormonal therapy: What the urologist should know: NYU case of the month, December 2020. Reviews in urology. https://pmc.ncbi.nlm.nih.gov/articles/PMC8058921/
Learn More From Our Expert:
Dr. Jill Schramm, DNP, FNP-C, BC-ADM, CDCES
Level 5 | Hot Flashes & Hyperglycemia
Recorded and Ready For Viewing!
Beta Bionics iLet Bionic Pancreas: Celebrating Freedom from Carb Counting

In May 2023, the FDA approved the Beta Bionics iLet Bionic Pancreas insulin pump for individuals 6 years and older. This is the first automated insulin delivery (AID) system to eliminate the need to enter carbohydrate (carb) counts for meals or snacks.
With over 1 million people worldwide utilizing insulin pump therapy, removing the intricate skill of carb counting has grabbed the attention of the diabetes community.¹
Diabetes is a disease that can be overwhelming, causing a substantial risk of distress and burnout. As a diabetes health care professionals, you help individuals living with diabetes choose technology to enhance their self-management and reduce some of the associated burdens.
Key Features
The iLet Bionic Pancreas is a continuous subcutaneous insulin infusion (CSII) system, also commonly referred to as an insulin pump. Like other tubed insulin pumps on the market, it features a small cartridge that holds insulin, an operating system that delivers the insulin, integration with a continuous glucose monitor (CGM), and is connected to the body via tubing with an insertion set.
CGM compatibility includes:
☑️ Dexcom G6
☑️ Dexcom G7
☑️ Libre 3+
The Bionic Circle app enables iLet users to invite up to 10 friends or family members to view alerts, blood glucose trends, meal announcements, and insulin doses. Healthcare providers utilize the Healthcare Provider Bionic Portal to download iLet data for review during office visits or for remote patient monitoring.
But How Is iLet Different?
The most significant difference with the iLet is that there are NO traditional pump settings. The only initial settings used are the individual’s weight and target range. Because there are no traditional settings, there is no user input for corrections or carb counting.
Three different algorithms drive insulin delivery. Let’s look at each algorithm²:
Basal Algorithm
- The original basal profile is developed based on the individual’s weight; however, over time, the system continually adapts the basal profile using continuous glucose monitor (CGM) data.
Corrections Algorithm
- Based on CGM data, the algorithm adds additional insulin beyond the basal requirements every 5 minutes, aiming to maintain blood glucose within the predetermined target rang.
Meal Announcement Algorithm
- When the individual announces a meal, the system customizes the insulin delivery based on dosing history for similar-sized meals.
- It determines and adapts meal types separately (breakfast, lunch, or dinner). Initially, the meal dose is calculated, just like the basal rate, and then postprandial corrections are applied if necessary. Based on this data, the system will continuously adapt to individualize the insulin needs based on the size of meals.
- The only decisions made at meal announcements are:
- Choosing the meal: breakfast, lunch, or dinner
- Choosing the size of the meal: If the meal is the usual amount of carbs, smaller, or larger
The only adjustable setting is the glucose target range. There are three different glucose targets to choose from. Two different blood glucose targets can be set within a 24-hour period.³
- 🩸Higher (130 mg/dL)
- 🩸Usual (120 mg/dL)
- 🩸Lower (110 mg/dL)
The Educator’s Perspective
When using the iLet there are a few crucial points to consider:
🥖 Carbohydrate education is not gone! Although no carb counting is required, clients must be aware of carbs. They will still need a basic understanding of which foods contain carbs to accurately determine the size of the meal.
📲 There are no traditional pump settings to manage. The only setting that can be changed is the target range. Education is key for clients who would self-adjust pump settings with previous insulin pumps.
🏃♂️ Managing exercise has changed. There is no exercise mode, activity mode, or temp basal setting to adjust insulin delivery for physical activity. Please see tips from Beta Bionics on managing physical activity with the iLet at https://www.betabionics.com/articles/exercise/.
As a diabetes healthcare professional, you support individuals living with diabetes in setting personalized goals and developing tailored treatment plans. After assessing the client’s needs and barriers, you may find that they are overwhelmed or distressed by the constant need for carb counting. You may also find those who prefer to be ‘hands-off’ with their diabetes for many reasons. These individuals may find that an AID system like the iLet can improve glycemic control without increasing treatment burden.
If you’re looking for more information on diabetes technology or identifying barriers to self-management, join our 2-Day Training Seminar in San Diego to help those living with diabetes continue to thrive.
References
Association of Diabetes Care and Education Specialists. (n.d.). The DCES and pump therapy. Danatech Diabetes Technology. https://www.adces.org/education/danatech/insulin-pumps/pumps-in-professional-practice/dces’s-and-pump-therapy
Beta Bionics. (n.d.). HCP webinars. https://www.betabionics.com/hcp/hcp-webinars/
- Beta Bionics (n.d.). Healthcare provider resources. https://www.betabionics.com/hcp/hcp-resources/
Live in San Diego
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements. See Training Schedule Here >>
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rediscover the Implanted CGM: A Closer Look at Eversense 365
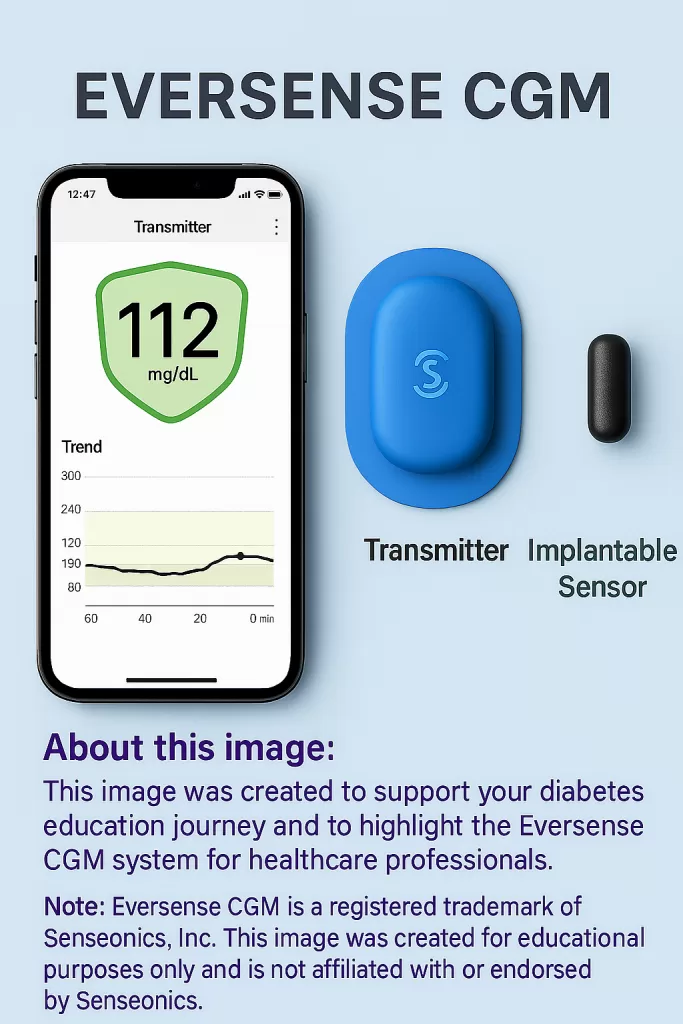
Do your clients accidentally knock off their continuous glucose monitor (CGM) or complain about how frequently they need to be replaced? If so, did you know there is an implanted CGM option available?
According to the ADA 2025 Standards of Care, CGMs are now the standard of care for individuals using insulin therapy or experiencing hypoglycemia.¹ There are many similarities between the available CGMs, but the Eversense CGM by Senseonics stands out due to some striking differences. As the diabetes education specialist, you can highlight the similarities and differences between CGMs so people can make a personalized and informed decision about which device works best for them.
Get to Know Eversense 365
The Eversense 365 is an implanted CGM (iCGM) used to monitor glucose in individuals 18 or older with diabetes. It is currently the only FDA-approved implantable glucose sensor in the United States. The Eversense system has launched the current 365-day sensor, which was approved for use in October 2024.
This system consists of a small sensor implanted into the subcutaneous tissue of the outer upper arm. A smart transmitter is placed over the inserted sensor to transmit data to a compatible smartphone. Glucose accuracy is similar to other prescription CGMs on the market.²
This system requires initial calibrations when starting a new transmitter. Calibrations must be completed within 36 hours.³
Initial calibration schedule:
- #1 – After the 24-hour warm-up phase
- #2 – 2-12 hours after the first calibration (Glucose readings will then begin to display on the app)
- #3 – 2-12 hours after the second calibration
- #4 – 2-12 hours after the third calibration
Ongoing calibration schedule:
- 1 calibration every 24 hours for 13 days
- 1 weekly calibration for the life of the sensor
Key Components of Eversense 365
The three key components of the Eversense 365 iCGM system are an implantable sensor, a smart transmitter, and a phone app that displays and shares data.
Implantable Sensor
- Sensor has a 365-day lifespan.
- Subcutaneous placement by trained provider.
- Sensor precautions:
- Do not inject insulin or insert an insulin pump infusion site within 4 inches of the iCGM sensor.
- Do not use lithotripsy, diathermy, electrocautery, or receive vaccinations near the inserted sensor, as this may cause damage to the sensor.
- The sensor can be worn in an MRI under specific conditions (see Eversense 365 Glucose Monitoring System User Guide for more information).
Smart Transmitter
- The transmitter is removable and rechargeable.
- Glucose data is transmitted every 5 minutes to the Eversense 365 app after the second calibration.
- Creates vibration alerts for high and low glucose readings.
- The transmitter must be removed before MRI, CT, or x-ray.
Mobile App & Data Sharing:
- Eversense 365 app displays real-time glucose trends.
- The app allows individuals to share glucose data with family, friends, and healthcare providers.
Eversense 365 Eligibility, Benefits, & Risks
The Everesense iCGM is approved for adults aged 18 and older with diabetes. This is available by prescription only. Medicare coverage for CGM requires a diagnosis of diabetes and being treated with insulin, or having two or more level 2 hypoglycemic episodes (<54 mg/dL).⁴ Coverage with commercial insurance varies, and Medicaid coverage varies from state to state.
Eversense 365 Benefits
- Decreased adhesive allergies
- The silicone-based adhesive on the transmitter can result in fewer skin reactions.
- Less frequent sensor changes
- The sensor is placed only once a year.
- Decreased wasted sensors falling off or failing early
- The transmitter is removable and can be replaced easily if knocked off.
- Decreased rate of compression lows
- Fewer compression lows have been noted⁵
- No worry about vitamin C or acetaminophen interfering with CGM readings
- These do not interfere with iCGM glucose readings like with other CGMs.
Contraindications & Precautions
- Do not use in individuals with known allergy to:
-dexamethasone or dexamethasone acetate
-any component of the sensor, transmitter, or adhesive - Mannitol or sorbitol (intravenous, irrigation, or peritoneal dialysis solution, but not sorbitol in the diet) can cause falsely elevated glucose levels.
- The tetracycline antibiotic class can cause falsely low glucose readings
- Always check fingerstick blood glucose for very high or very low glucose readings before making a treatment decision
- The system has not been tested on:
-Those who are pregnant
-Those under 18 years old
-Those taking certain medications: chemotherapy, anticoagulant therapy, or immunosuppressive therapy
-Those with active implantable devices (such as a cardiac defibrillator)³
Role of the Diabetes Education Specialists
Diabetes care and education specialists (DCES) are an essential source of information for those living with diabetes to help achieve glycemic goals with a personalized approach to technology. Individualized education and training on the Eversense 365 iCGM ensure the proper use of the system, including calibration and interpretation of the glucose data. Understanding the details of the Eversense 365 allows the DCES to efficiently help troubleshoot problems, leading to long-term adherence and maximizing the benefits of an iCGM to improve diabetes outcomes.
Ready for a closer look at how technology integrates into successful diabetes outcomes? Check out the Diabetes Ed Training Conferences for technology updates and more!
References
- American Diabetes Association Professional Practice Committee. (2025). Diabetes technology: Standards of care in diabetes – 2025. Diabetes Care, 48 (supplement 1), S146-S166. https://doi.org/10.2337/dc25-S007
- Danatech. (n.d.). Find & compare continuous glucose monitors. https://www.adces.org/education/danatech/glucose-monitoring/continuous-glucose-monitors-(cgm)/view-compare-cgms
- Senseonics. (2025) Eversense 365 Continuous Glucose Monitoring System User Guide.https://www.eversensecgm.com/user-guides/
- American Diabetes Association. (n.d.). FAQs on CGM coverage criteria changes in Medicare. https://diabetes.org/advocacy/cgm-continuous-glucose-monitors/faqs-medicare-coverage#:~:text=Medicare%20now%20allows%20people%20to,day%20to%20access%20a%20CGM.
- Christiansen, M. P., Klaff, L. J., Brazg, R., Chang, A. R., Levy, C. J., Lam, D., Denham, D. S., Atiee, G., Bode, B. W., Walters, S. J., Kelley, L., & Bailey, T. S. (2018). A prospective multicenter evaluation of the accuracy of a novel implanted continuous glucose sensor: PRECISE II. Diabetes Technology & Therapeutics, 20(3), 197. https://pmc.ncbi.nlm.nih.gov/articles/PMC5867508/
ReVive 5 Diabetes Training Program: A Person-Centered Approach to Diabetes Distress & Glucose Management
Join us live on July 15th and July 22nd, 2025 at 9:00 am PST
6+ CEs with Expanded Accreditation!
Join experts Larry Fisher, Ph.D., ABPP, Susan Guzman, Ph.D., and Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM, for this transformative two-part training on the ReVive 5 framework—an evidence-based approach that integrates emotional well-being and glucose data into person-centered diabetes care.
Grounded in the results of the EMBARK Trial, this program emphasizes the urgent need to assess and address diabetes distress, now recognized in the ADA Standards of Care as a critical component of care. You’ll gain practical tools and strategies used in the trial to support emotional well-being, meet clinical standards, and empower individuals on their diabetes journey.
Program Objectives:
Upon completion of this activity, participants will be able to:
- Identify the key differences between diabetes distress and depression and explain their impact on self-care behaviors.
- Apply evidence-based communication strategies to respond to diabetes distress screening results.
- Demonstrate how to analyze glucose patterns using meter and sensor data.
- Utilize the ReVive 5-step approach to integrate emotional and glucose management into diabetes care.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:



Lawrence Fisher, Ph.D., ABPP
Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
CEO of DiabetesEd Services
Faculty Bios & Disclosures
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Consultant, advisor, and speaker for Eli Lilly
Speaker Interview:
Bio:
Dr. Fisher has been a professor in the Department of Family & Community Medicine at the University of California, San Francisco for over 25 years, and he is the Director of The Behavioral Diabetes Research Group at UCSF.
He has a Diplomate in Clinical Psychology from the American Board of Professional Psychology and is a former Associate Editor of Diabetes Care. He has conducted multiple cross-sectional and longitudinal NIH- and ADA-supported clinical research with adults with diabetes and their families.
His recent work focuses on diabetes distress and depression, disease management, and how adults and families struggle over time to manage chronic health conditions. He has won two major UCSF School of Medicine teaching awards, was nominated for the UCSF Postdoctoral Scholars Association Outstanding Mentorship Award, and has received a certificate from the American Psychological Association in “Recognition for Substantial Contributions to the Field of Family Psychology and Health.”
In 2012 he received the Richard Rubin Award from the American Diabetes Association. He maintains an active clinical practice at UCSF, has published over 190 peer-reviewed articles on diabetes and related topics, and frequently speaks to both professional and lay groups at local, national, and international meetings and workshops.
 Susan Guzman, PhD
Susan Guzman, PhD
- Consultant, advisor, and speaker for Abbot Labratories and Embecta
Dr. Guzman is a clinical psychologist specializing in diabetes. In 2003, Dr. Guzman co-founded the Behavioral Diabetes Institute (BDI), the first non-profit organization devoted to the emotional and behavioral aspects of living with diabetes.
At BDI, she serves as the Director of Clinical Education, developing and leading programs for people with diabetes and healthcare professionals. She has helped develop and facilitate diabetes distress group interventions for two NIH-funded research studies for adults with type 1 diabetes.
Dr. Guzman is passionate about helping to change the conversations in diabetes away from shame, blame, and judgment to those based on facts, empathy, and engagement. She has been part of a joint ADA/ADCES effort to address problematic language and messages in diabetes.
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADMBeverly Thomassian has no financial disclosures
Speaker Interview:
Bio:
Expanded Accreditation
Activity Start and End Date: 7/15/2025 to 7/22/2027
Estimated time to complete the activity: 6 hours and 15 minutes
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 6.25 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 6.25 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 6.25 contact hour(s) (.625] CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – UAN JA4008073-9999-25-198-H01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 6.25 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 6.25 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 6.25 Interprofessional Continuing Education (IPCE) credit for learning and change.
Disclosure of Unlabeled Use:
This educational activity may contain discussion of published and/or investigational uses of agents that are not indicated by the FDA. The planners of this activity do not recommend the use of any agent outside of the labeled indications. The opinions expressed in the educational activity are those of the faculty and do not necessarily represent the views of the planners. Please refer to the official prescribing information for each product for discussion of approved indications, contraindications, and warnings.
Disclaimer:
Participants have an implied responsibility to use the newly acquired information to enhance patient outcomes and their own professional development. The information presented in this activity is not meant to serve as a guideline for patient management. Any procedures, medications, or other courses of diagnosis or treatment discussed or suggested in this activity should not be used by clinicians without evaluation of their patient’s conditions and possible contraindications and/or dangers in use, review of any applicable manufacturer’s product information, and comparison with recommendations of other authorities.
Instructions for Credit
Participation in this self-study activity should be completed in approximately 6 hours and 15 minutes. To successfully complete this activity and receive CE credit, learners must follow these steps during the period from 7/15/2025 to 7/22/2027.
- Review the objectives and disclosures
- Study the educational content in Online University
- After review of content, a module within the course in the Online University will list a link to Partners for Advancing Clinical Education’s website
- Visit Partners for Advancing Clinical Education website listed in course in the Online University
- Complete the activity evaluation through Partners for Advancing Clinical Education website
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Why Actos May Be Reemerging in the Diabetes Landscape
By: Beverly Thomassian

In the ever-evolving world of diabetes care, medications come in and out of favor based on new research, shifting safety data, and individual needs. Pioglitazone (Actos), once a go-to medication for improving insulin sensitivity, fell out of favor in the early 2010s due to concerns about bladder potential side effects and newer medications.
Now, pioglitazone is gaining renewed interest, especially for individuals with increased cardiovascular risk and steatosis, who may benefit from its unique profile. Even though pioglitazone only lowers A1C by 0.5 – 1.0%, this medication’s properties compel us to consider reintroducing it into the medical management of diabetes, especially in the presence of liver and heart disease. Plus, as a generic medication, its price tag of less than $5.00 a month makes it affordable for most people.
Potent Insulin Sensitizer
Pioglitazone is one of the thiazolidinedione (TZD) class of medications that work by enhancing insulin sensitivity, primarily through activation of PPAR-γ receptors in adipose and muscle tissue.
In a recent podcast, Banting Award Recipient, Dr. Ralph DeFronzo, provides an Insulin Resistance Master Class. He notes that pioglitazone, an insulin-sensitizing medication, improves cardiometabolic health, in part, by shifting fat distribution from visceral to subcutaneous areas. This redistribution of fat, may be associated with some weight gain. But, Dr. DeFronzo explains that this weight gain is actually a sign that the pioglitazone is working to improve insulin sensitivity. Compared to other oral agents, pioglitazone remains one of the most effective insulin sensitizers, especially useful in those with significant insulin resistance.
Why the Renewed Interest?
1. Cardiovascular Benefits – Decrease stroke and MI
The IRIS trial demonstrated that pioglitazone reduced the risk of stroke and myocardial infarction in insulin-resistant patients with a history of cerebrovascular events (Kernan et al., 2016). This benefit is being re-evaluated in the context of cardiometabolic risk, especially in people with atherosclerotic disease or metabolic syndrome.
The ADA Standard #3 states, “In people with a history of stroke and evidence of insulin resistance and prediabetes, pioglitazone may be considered to lower the risk of stroke or myocardial infarction. However, this benefit needs to be balanced with the increased risk of weight gain, edema, and fractures. Lower doses may mitigate the risk of adverse effects but may be less effective.”
2. Role in MASLD and MASH
Pioglitazone has shown promise in improving liver histology in people with metabolic-associated steatohepatitis (MASH), making it one of the few medications with such benefits (Cusi et al., 2017). Studies demonstrate it improves hepatic insulin sensitivity, reduces liver fat, and may slow fibrosis progression.
The ADA Standards of Care #4, include recommendations to start pioglitazone and GLP-1’s for individuals with diabetes and steatosis to prevent progression and slow fibrosis. “In phase 2 clinical trials, pioglitazone and some GLP-1 RAs have been shown to be potentially effective to treat steatohepatitis and to slow fibrosis progression. They may also decrease CVD, which is the number one cause of death in people with type 2 diabetes and MASLD.
3. Re-Evaluating Safety Concerns
Initial concerns about the risk of bladder cancer stemmed from observational studies; however, more recent analyses suggest that the risk is low or not statistically significant (Lewis et al., 2015). Furthermore, thoughtful prescribing—avoiding use in individuals with heart failure or active bladder cancer risk—helps mitigate potential harm. In addition, this medication is not recommended for those at risk of falls and fractures.
Comparative Benefits of Diabetes Medications
Here is a visual summary comparing the relative effects of pioglitazone versus other common medications:
Clinical Considerations
When considering pioglitazone (Actos), carefully assess:
- Cardiovascular history
- benefit for those with insulin resistance
- caution in heart failure
- Liver function and history of MASLD/MASH – recommended
- Bladder cancer history – avoid
- Fracture Risk – avoid
Pioglitazone may also be especially helpful in combination with agents like metformin or GLP-1 receptor agonists, balancing out each other’s side effects and mechanisms of action.
Conclusion
Pioglitazone (Actos) may never regain its former status as a front-line diabetes treatment, but it has a clear and valuable role in today’s therapeutic landscape. For select individuals—especially those with insulin resistance, cardiovascular risk, or liver disease—pioglitazone offers an underutilized tool backed by strong evidence and decades of experience.
In diabetes care, what’s old can be new again—especially when paired with clinical wisdom and person-centered decision-making.
📚 References
Want to learn more about ADA Standards?
Enroll in our upcoming webinar
Join us live on April 8, 2025, at 11:30 am PST

This course provides the need-to-know information regarding the microvascular complications of diabetes. It includes a brief overview of pathophysiology & clinical manifestations along with prevention strategies & screening guidelines. This straightforward program will provide participants with the information they can use in a clinical setting & also provides critical content for certification exams.
Letting Go of Judgment – Embracing Curiosity
Letting Go of Judgement & Embracing Curiosity
by Beverly Thomassian
As healthcare professionals, I believe we can let go of the assumptions and judgments that so often cloud our perception of the very person we are trying to care for and lean into curiosity.
Feelings of judgment are more commonplace than you may think – almost like an unconscious thought pattern. These feelings can block the creation of a meaningful connection and leave the healthcare professional and the person in our care feeling …disconnected, misunderstood, or unseen. When judgment takes the lead, it builds a quiet wall that can prevent trust from forming and healing from taking root.
But when we become aware of these unconscious patterns and intentionally set them aside, we create space for empathy, curiosity, and genuine connection. It’s in that space that the healthcare professional and the person in our care can feel respected, valued, and heard.
You can become more aware of feelings of judgment and notice what they are saying to you. This awareness is the first step to showing up for the people in our care with deeper authenticity and compassion.
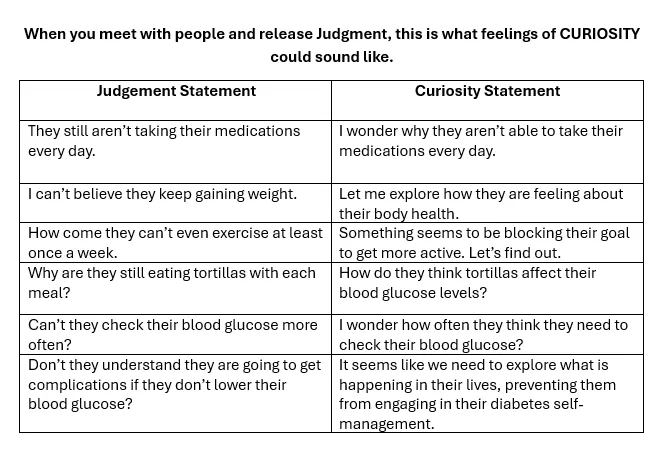
When you meet with people, this is what feelings of judgement sound like.
- “They still aren’t taking their medications every day”
- “I can’t believe they keep gaining weight”
- “How come they can’t exercise at least once a week”
- “Why are they still eating tortillas with each meal”
- “Can’t they check their blood glucose more often”
- “Don’t they understand they are going to get complications if they don’t lower their blood glucose”
If you hear yourself thinking these thoughts or something similar, at first, simply commit to noticing it. Don’t beat yourself up for having these thoughts and feelings. As healthcare professionals, we have a whole trunk full of biases and lived experiences. It’s okay; we are actively working on releasing the shackles of judgment from ourselves and the people in our care. Now, take a deep breath and see if you can reframe this thought through the lens of curiosity.
By exchanging judgment with curiosity, you actively engage in more mindful practice and start meeting people where they are – with compassion. Curiosity does not judge; it leans in with openness, seeking to understand rather than to label. It invites connection, discovery, and the possibility of seeing things, especially people—in a new and compassionate light.
After all, we all signed up for this profession to make a positive impact in people’s lives. Meeting people with the lens of curiosity brings out the best in us, matching the reason we entered health care in the first place – to help with healing.
The goal is give yourself permission to set those feelings of judgment aside so you can show up as your best self and make the difference you want.
This approach has numerous benefits for the caregiver and the person receiving care.
When you provide nonjudgmental care infused with curiosity and compassion, you honor the strengths of the people you’re serving. You’re also infusing your consciousness with kindness in place of judgment. This approach, based on curiosity and compassion, leads to more effective care and healing that flows both ways.
Join our Group – Healing Through Connection
We know these unconscious feelings can get in the way, yet no one talks about them. Let’s start an open and honest dialogue about these feelings. The best caregiver in the world experiences moments of judgment that can get in the way of how they show up for people. The solution is to talk about these feelings with colleagues and friends in a safe space.
We’ve developed a community to do just that. It’s a community for healthcare professionals involved in caring for people with chronic diseases. We all want the same things – which is to provide more effective care based on compassion. When you meet other people in this community, you’re going to realize that you’re not alone and that other people experience the same feelings you do. And instead of you dealing with it by yourself, there is going to be an entire community of healthcare professionals supporting each other.
Benefit of this “Healing Through Connection” FaceBook Group
– Professionals can share authentic feelings around caregiving and find connection
– Give permission to these common feelings that you and other people experience
– Know that you’re not alone in this – you don’t need to feel bad or judge yourself
– these are normal human feelings that caregivers have and it’s time that we acknowledge them

Ignite your passion & prepare for Diabetes Certification!
Join our Expert Team at our dynamic Virtual DiabetesEd Training Conference April 16-18th, 2025

Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more! If you’re preparing for the CDCES or BC-ADM exam, this conference—paired with free bonus courses—serves as the ideal study companion!
With interactive co-teaching, we keep sessions engaging, relevant, and fun. Let’s learn and grow together!

Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun! The faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Christine Craig, MS, RD, CDCES
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 11 Bonus Online Courses: As a course attendee, you automatically receive a bonus online course bundle of 11 online courses valued at over
Diabetes Mentorship Program Kicks-Off in Northern Cal
 Dignity Health Mercy Medical Center Redding Steps Up with a Diabetes Mentorship Program!
Dignity Health Mercy Medical Center Redding Steps Up with a Diabetes Mentorship Program!
We are thrilled to announce the launch of the Diabetes Mentorship Program at Mercy Medical Center in Redding, designed to support and guide the next generation of diabetes educators. This unique opportunity is tailored for eight motivated mentees who are eager to gain hands-on experience in diabetes care, all while learning from Janelle Revnak, MS, RDN, CDCES, an experienced diabetes care and education specialist, with 10 years practicing as an RDN and 5 years as a CDCES. Janelle is passionate about sharing her expertise with the next generation of diabetes professionals. Her extensive background in both outpatient and inpatient diabetes education will ensure that mentees receive comprehensive training and valuable insights into the world of diabetes care.
Over the course of the program, mentees will attend monthly educational sessions led by Janelle, coupled with didactic learning sessions and job shadowing, providing an immersive experience in the inpatient setting. As part of our mentoring partnership, the trainees will also have access to our Diabetes Boot Camp series. Janelle decided to start this program after realizing that the need for diabetes education in her rural community was larger than what one person could realistically deliver. She reached out and identified colleagues in her hospital who were interested upping their diabetes knowledge and improving care.
“I alone cannot change the world, but I can cast a stone across the waters to create many ripples.” – Mother Teresa
Increasing Demand for Diabetes Care and Education Specialists
As the number of people living with diabetes continues to rise, the demand for skilled diabetes educators is paramount. According to the latest CDC Data, the prevalence of diabetes has increased dramatically over the past decade, with more than 37 million Americans now living with diabetes—an increase of nearly 30% over the past 10 years. This growing population needs more than just medical care; they require specialized education and support to effectively manage their condition. Current diabetes care and education specialists (DCES) are uniquely positioned to assist in equipping future professionals with the knowledge and experience needed to meet the needs of this expanding patient population.
The mentorship program will be held once a month and is designed to create a balanced approach to learning. Mentees will dive deep into didactic topics, such as advanced diabetes management, behavior change strategies, and innovative approaches to diabetes care. In addition to classroom-style learning, they will have the opportunity to job-shadow Janelle, gaining firsthand experience in how diabetes education is applied in real-world inpatient clinical settings. This combination of theory and practice ensures mentees are well-equipped to make an impact in the field.
Participants will also have the chance to engage with a wide range of diabetes-related cases during their job shadowing. From inpatient diabetes clinical management to individualized patient education, they will develop a well-rounded understanding of the crucial role diabetes educators play in improving care outcomes while helping individuals feel emotionally supported through this challenging disease. This hands-on approach allows for active learning and real-time feedback, which is vital for shaping confident and competent DCES.
The mentorship program is not just about learning—it’s about making connections, fostering growth and building a community of passionate diabetes care professionals. We are excited to offer this incredible opportunity to those who are committed to advancing their skills and knowledge in diabetes education. Together, we can make a real difference in the lives of those living with diabetes. In the spirit of Mother Teresa, it is not one person alone that can impact the growing population affected by diabetes, but working together, we can achieve meaningful change.
If you have questions, you can reach Janelle at [email protected].
Are you Interested in Starting a Mentorship Program?
As part of our Bridge Program, Coach Beverly wants to support YOUR efforts to mentor a new generation of Diabetes Care and Education Specialists. If you are a mentor, we are offering significant discounts off of our Diabetes Boot Camp or Virtual 3 Day Program for groups of mentees who are practicing in underserved regions of our country. Please email us for more information at [email protected]
Want more expert insights & hands-on learning?
A perfect program for healthcare professionals entering the field of diabetes!
Join us for our 2025 Virtual Conference!!!

🎉 Join Our Virtual DiabetesEd Training Conference! 🎉
🗓️ Date:April 16th-18th, 2025
⏰ Time: 8:00am PST
Get ready for 2.5 days of engaging sessions on the latest in person-centered diabetes care, covering ADA Standards, medications, technology, and more! Learn from Diana Isaacs, Coach Beverly, and other experts.
💡 Can’t attend live? Access recordings, podcasts, and resources for 1 full year.
🎉 Special Offer: Register 3 or more and save $50 each!
Register now and take your diabetes expertise to the next level!
January 2025 E-Newsletter
At the beginning of each year, Coach Beverly excitedly scans the new ADA Standards to discover updates and advances in diabetes care. She then integrates these new findings into our courses and web content to ensure we accurately reflect the latest guidelines.
In our first newsletter of 2025, we are excited to share our library of annually reviewed Cheat Sheets that integrate the 2025 Standards! They are available on our website and CDCES Coach App for easy access, with the option to download and share with your colleagues and people living with diabetes alike.
We are thrilled to recognize a trailblazer in Northern California who is mentoring eight new diabetes care and education specialists. Janelle Revnak, MS, RDN, CDCES, realized that more educators were needed to meet the needs of her rural community and took action. Read more about her story and bold plan below.
Christine Craig, MS, RD, CDCES, highlights the importance of sleep in improving health and suggests actions that diabetes care and education specialists can take to address sleep health as a vital component of diabetes care.
Coach Beverly addresses commonly asked questions for those taking the CDCES Exam, including information on our practice hours tracker and which ADA Standards year to study.
We encourage you to test your knowledge with our Question and Rationale of the Week. January kicks off our Level 1 Fundamental Series, followed by our annual ADA Standards of Care update and Level 3 Mastery Course Series in February. We hope to see you there!
Here is to a 2025 filled with self-compassion and moments of awe.
Coach Beverly, Bryanna, Tiffany, and Christine
Announcements ___________________________ |
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Bold Front-of-Food Labeling Proposal

Clarifying “Healthy” on Food Labels
To address nutrition’s role in chronic disease, the FDA proposes a bold new front-of-package nutrition labeling law aimed at helping consumers make healthier food choices.
The proposed nutrition label is intended to complement the nutrition facts label and would categorize saturated fat, sodium, and added sugars as low, medium, or high. This proposal comes on the heels of the December 2024 definition update of the nutrition claim “healthy.”
To be labeled as “healthy”, products must contain fruit, vegetables, protein, dairy, or grains and meet certain nutrient limits. As diabetes care and education specialists, it is essential to be aware of this FDA initiative, since it aligns with the 2025 ADA Standards of Care nutrition therapy recommendations3 and global efforts to address diet-related health issues.
Front-of -Package Food Labeling decreased High Sugar Purchases
In Fall 2023, my family and I spent five months in Chile, offering a firsthand view of the impact of front-of package policies on the grocery landscape. Similar to global trends, over the past twenty years, Chilean diet patterns have shifted toward packaged and fast-food consumption.
Recognizing the connection between diet and chronic disease, Chile implemented ambitious food policies. Key measures included increased taxation on sugar-sweetened beverages, front-of-package warning labels, restrictions on child-targeted food marketing, and bans on unhealthy food sales in schools.4 In 2016, Chile became the first country to require front-of-package warning labels for foods high in calories, saturated fat, added sugars, and sodium. Outcomes from these measures significantly reduced purchases of sugar-sweetened beverages by nearly 24% within two years and reduced overall purchases of “high in sugar” food and beverage-labeled foods.4 Countries throughout South America, Israel, and Canada have followed suit with required front-of-package warning or stop light labeling.5 They have all shown improved consumer awareness and changes to diet intake, which has also influenced manufacturers’ food reformulation.
Unintended Consequences – More Non-Caloric Sweeteners
Despite the progress in Chile’s nutrition policy efforts, unintended consequences emerged. To avoid warning labels, food companies reformulated products, especially those “high in sugar.” By 2020, Chile’s total percentage of non-caloric sweeteners increased to be within over 50% of all products.6
The FDA is encouraged that its’ proposed front-of-package nutrition labeling system will encourage product reformulation to align with new policies.2 While reformulations can be beneficial, they also raise concerns about continued reliance on low nutrient-density processed food consumption and additives such as non-nutritive sweeteners, which the World Health Organization and the American Diabetes Association discourage.3
It will be important to monitor behavioral purchasing changes along with the long-term health benefits or implications of reformulated products to ensure U.S. new labeling guidance actually achieve healthier dietary patterns.
Advocate for Whole Food-Based Eating Patterns
As we embark on a new era of food and chronic care policy efforts, diabetes educators can learn from other countries’ successes and challenges while advocating for policies that foster healthier dietary and socioeconomic environments. Where appropriate, we can encourage a shift toward whole food-based eating patterns and reduced reliance on processed food consumption. We can stay abreast and advocate for policy and action alerts impacting nutrition and diabetes care.
By complementing front-of-package labeling proposals with educational campaigns, community-level interventions, and policies that address quality food access, we can improve population health and address the root causes of health disparities.

Learn More:
Get Involved in Advocacy:
- American Diabetes Association Advocacy Overview
- Association of Diabetes Care and Education Specialists Advocacy
- American Dietetic Association Advocacy
References:
- CDC: Diabetes. Download on January 18th, 2025 from https://www.cdc.gov/diabetes/communication-resources/1-in-3-americans.html
- Food Labeling: Front-of-Package Nutrition Information (Proposed Rule). Downloaded on January 19th 2025 from Source.
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2024. Diabetes Care1 January 2024; 47 (Supplement_1): S77–S110. https://doi.org/10.2337/dc24-S005
- Taillie LS, Reyes M, Colchero MA, Popkin B, Corvalán C. An evaluation of Chile’s Law of Food Labeling and Advertising on sugar-sweetened beverage purchases from 2015 to 2017: A before-and-after study. PLoS Med. 2020 Feb 11;17(2):e1003015.
- Front-of-package labeling. Downloaded on 1/18/2025 from https://www.globalfoodresearchprogram.org/resource/front-of-package-label-maps/
- Sambra V, López-Arana S, Cáceres P, Abrigo K, Collinao J, Espinoza A, Valenzuela S, Carvajal B, Prado G, Peralta R, Gotteland M. Overuse of Non-caloric Sweeteners in Foods and Beverages in Chile: A Threat to Consumers’ Free Choice? Front Nutr. 2020 Jun 17;7:68