
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

As we continue to navigate this long-lasting pandemic there has been so much loss and heartache.
Years ago I went to a conference on preventing burnout in healthcare providers with Dr. J. Bryan Sexton, associate professor in psychiatry and behavioral sciences at Duke’s School of Medicine and an expert in the idea of resilience. He impressed me and I have talked about his conference to many colleagues over the years.
I loved sharing his wisdom with my clients, because of studies that link resilience to better diabetes self management. (1)
Lately, as I have been struggling with overwhelming feelings of sadness, I have remembered to practice some of his tools to cultivate resilience. Cultivating resiliency is something that takes daily focus. To cultivate means to nurture, grow, and encourage resilient behaviors.
Three Good Things
Humans are hard-wired to remember the negative aspects of our day, but flipping around the natural inclination is simple.
Building resilience is possible by focusing on positive emotions – joy, serenity, hope gratitude, inspiration, pride, love, awe, and amusement.
Promoting positive thoughts and building resilience can be as easy as taking notes each night before bed. Think of three things that happened during the day that went well and your role in the positive outcome, then jot down those three things. Best results for this exercise come after 14 consecutive days. Empirical evidence shows that this elevates brain serotonin with positive effects on our mood that last for months. (2)
Show Gratitude
Grab a pen and paper and write a letter of appreciation to someone- anyone. Take five minutes to explain something they did, how it impacted you and the benefits you received. Whether you share the letter or not, Dr. Sexton said it can have lasting impacts, increasing happiness while lowering depressing thoughts because focusing on benefits forces us to linger on positive thoughts.
Rediscover Awe
Through an “awe intervention,” you can create a sense of slowed down time, which offers a calming sensation and a feeling of having more time available.
Awe also helps us to feel inspired. I call awe intervention, “joyful thanksgiving”. It is a practice that I am doing in which I acknowledge and give a little extra gratitude for the many amazing sights, sounds, tastes, relationships, information, and emotions that excite me and create awe right from the moment when I wake up.
I began to feel grateful for this medicinal food. Oats, blueberries, banana, and nuts contain water soluble fiber which slow the absorption of sugar and fat from food, and therefore help prevent spikes in blood sugar and blood fat, possibly reducing the inflammatory response to food. (3)(4)
Fiber is a super food which provides important nutrition for our intestinal bacteria to live and prosper, that’s why fiber is called a pre-biotic. Vegetables, fruit, whole grains, nuts and legumes remain the single best sources of fiber in the diet. High-fiber vegetables include many of the green leafy vegetables like kale, collard greens, chard, arugula, and even lettuces. Whole-grain sources of fiber include oats, quinoa, barley and rye. Legumes include beans like peas, soy, black, pinto and lentils.
Encouraging our clients to consider adding more fiber rich dishes to the holiday meals this season and perhaps telling them about Dr. Sexton’s tools for cultivating resilience may help them to feel happier and more hopeful and contribute to better blood sugar control.
½ cup unsweetened coconut milk beverage
½ cup old-fashioned oats
½ TB chia seeds
½ banana
1 tsp maple syrup
½ cup blueberries
2 TB chopped walnuts
1/8 tsp cinnamon
Combine coconut milk, oats, chia, banana, maple syrup in a pint-sized jar and stir. Top with blueberries and coconut. Cover and refrigerate overnight. Heat up and sprinkle with walnuts and cinnamon in the morning.
285 calories, 6 gm protein, 57 gms carbohydrate, 7 gms fiber 6 gm fat
Meta-Analysis. Nutrients. 2015 Dec; 7(12): 10369-10387p. 1392:8
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
The holidays are upon us in the midst of a pandemic.
In past holiday seasons, I would check in with my clients to see how the holiday season was affecting their health. We would talk about getting enough sleep and adapting exercise routines to adjust for cold weather and shorter days.

We would talk about stress management tools to help cope with the pressures to overeat and the pressures to eat foods that we have been attempting to avoid.
This year is challenging because we are already taxed by the unbelievable stress of living in a pandemic.
I have found that I am already struggling with insomnia and less exercise. I have been overeating and craving sweets. In fact, I think that I have developed a sugar addiction during these last 7 months. I have been substituting ice cream, donuts, and chocolate for the hugs that I used to take for granted. I am missing gatherings, parties, and shared dinners with friends.
Sugar is a powerful stimulant of serotonin that is lacking in my brain these days. I thought that I was developing a cavity and this woke me up.
I had to make a commitment to cut back on sugar.
I thought about the World Health Organization’s sugar recommendation of lowering our free sugar intake to less than 5% of our total daily calories. This works out to about 6 teaspoons a day, depending on the person.
Free sugar applies to
Whole fruit and milk sugar are not included in free sugar.
I started to look at the total amount of free sugar that I was consuming. On some days it added up to over 12 teaspoons per day! And I am a dietitian.
The average American consumes 17 teaspoons of sugar daily. This translates to 57 pounds of sugar consumed each year.
Many people don’t realize that a lot of the sugar they take in are “hidden” in processed foods, according to the World Health Organization.

Research does show that for some people eating sugar produces characteristics of craving and withdrawal, along with chemical changes in the brain’s reward center, the limbic region. These changes are linked to a heightened craving for more sugar.
I am grateful to be able to consciously choose to lower my sugar intake to improve my health.
I am grateful that the whole fruit can be used as a sweet substitute for my sugar cravings.
I love the new fall crop of apples, pears, kiwi, and persimmons.
Below are my recipes for baked apples and poached pears that are a delicious holiday dessert.
Mix the melted butter or coconut oil, walnuts, and cinnamon together and pour over the apples. Bake in the preheated oven until the apples are soft, about 20 – 30 minutes. Stir once during the baking.
Enjoy!

Pour the wine into a small saucepan along with the orange zest and juice and all of the spices
Bring almost to a boil and add the pear halves. Turn down the heat and let the pears simmer gently for 20 – 30 minutes, or until they have slightly softened. Carefully turn the pears over a few times throughout the cooking time to ensure they color evenly. When the pears are cooked remove them from the wine and place them on plates. Add a tablespoon of yogurt to each plate and sprinkle with toasted almonds.
Visit our Joy of 6 Page for sugar info and resources to share with your clients!
Written by Dawn DeSoto RD, CDCES, our resident Nutrition Content Writer
This time of year is my favorite. Seeing the beautiful colors of the fall harvest soothes and invigorates me. Being outdoors with my community is especially healing during this unusual and stressful time of isolation due to the pandemic.

I especially adore shopping and gathering fresh produce and other goodies from our local Farmers’ Market!
The farmer’s market is also a special place for me because my daughter works there. Her booth is overflowing with all the pumpkins and winter squash they have harvested. Last week, at the market, my daughter introduced me to her friend as they were talking about a pumpkin pie he had made from the pumpkin that he had purchased from her.
“Unfortunately, I can’t eat the pumpkin pie anymore because I was just diagnosed with having Type-2 Diabetes,” he explained.
I couldn’t help but tell him that I was a Dietitian and Diabetes Specialist.
We started talking about modifying the recipe using sugar substitutes or low carbohydrate crusts. We discussed portion control and going for a walk after eating a piece of the pie. He was intrigued.
Pumpkin and other winter squash do contain carbohydrates but are nourishing food. Benefits include:
It is important to take away the judgment around food choices, to encourage thoughtful choices, and find joy in our food. At this difficult time, every effort to empower ourselves with choice and joy is highly recommended.
Choose a pie pumpkin and wash it’s exterior. Cut in half lengthwise and remove the seeds and pulp. Roast in your oven for about 45 minutes at 350 degrees F.
Simply peel away the skin from the flesh and toss the pumpkin pulp into your food processor or blender.
Ingredients:
In a large bowl, whisk eggs and pumpkin puree together. Add the rest of the ingredients and whisk together while slowly pouring in the evaporated milk.
Pour mixture into pie crust.Bake in the oven for 20 minutes at 390 degrees, reduce oven to 350 degrees and bake for another 45 – 60 minutes until inserted toothpick comes out clean. Store in the refrigerator overnight.
Written by Dawn DeSoto RD, CDCES, our resident Nutrition Content Writer

Meet Dawn Desoto, our resident Nutrition content expert. Dawn has specialized in diabetes care for over twenty years.
As a diabetes specialist, Dawn provides individual and group coaching. Dawn launched a Diabetes Prevention Program in her community and provided plant-based cooking classes coupled with take-home recipes. The participants loved the helpful, delicious, easy-to-understand food demonstrations and recipes. But, a big motivation to keep coming to classes, was the fact that they felt celebrated and supported by the kind wisdom of Dawn’s approach.
In addition to her diabetes and nutrition expertise, Dawn loves to garden, cook, swim, bike and hike with her son and daughter. She also enjoys reading, traveling, and star gazing!
Please join me in welcoming my friend and colleague, Dawn Desoto, RD, CDCES

Ireland’s Supreme Court announced that Subway’s sandwich “bread” cannot be legally labeled as bread.
After a Subway franchise in Ireland attempted to claim tax breaks for some of their items on the menu, a ruling was made that the bread Subway uses isn’t bread but more of a confectionary baked good.
“Subway’s bread is, of course, bread. We have been baking fresh bread in our restaurants for more than three decades and our guests return each day for sandwiches made on bread that smells as good as it tastes,” a Subway spokesperson said in a statement. The company says it’s reviewing the ruling.
Subway’s bread recipe has 10% of sugar to the weight of flour, which means their bread cannot be considered a staple food of bread and therefore ineligible for tax breaks.
This decision is in accordance with the Value-Added Tax Act of 1972 which states that “tax-exempt bread can’t have sugar, fat and bread improver exceed 2% of the weight of flour.”
This isn’t the first time Subway’s bread recipe has been questioned. In 2014 a petition went viral to remove azodicarbonamide, a chemical found in shoe rubber and items like yoga mats.
Overall, Subway, often revered as one of the healthier fast food options, may need to reevaluate its bread recipe and consider decreasing added sugar content.
To read more, click here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Over 50% of people living with diabetes have fatty liver disease.
Over the next 20 years, non-alcoholic steatohepatitis (NASH) and type 2 diabetes will account for 65,000 transplants, 1.37 million cardiovascular-related deaths, and 812,000 liver-related deaths.
These statistics are from a 2020 article in Diabetes Care, Economic and Clinical Burden of Non-alcoholic Steatohepatitis in Patients With Type 2 Diabetes in the U.S.
Fatty liver disease is increasingly recognized as the hepatic manifestation of metabolic syndrome. Currently, there is no effective approved medical therapy to fix the fatty liver disease, management depends on lifestyle changes, such as weight loss and increased exercise.
About 34 million people in the U.S. have type 2 diabetes. Of those, over half are also living with liver disease.
In the U.S. in 2019:
Given the high rate of liver disease in people with diabetes, I have been paying more attention to our client’s liver enzymes levels, including alanine aminotransferase (ALT) or aspartate aminotransferase (AST). Elevated levels of these liver enzymes indicate inflammation and a potential pathway to liver disease progression.
After discovering elevated enzymes, we send them for further diagnostic testing to evaluate the extent of liver disease. The question is, should we make liver health screening a part of our usual diabetes practice?

According to a recent article in Gastroenterology, screening for non-alcoholic fatty liver disease (NAFLD) followed by lifestyle modification among people with type 2 diabetes can be cost effective.
In a recent study, a team of researchers used a hypothetical cohort of people age 55 years with type 2 diabetes and developed a model that compared screening and treatment with no such protocol.
For the virtual intervention group, they measured ALT or AST and provided an ultrasound scan. If these tests came back positive for NAFLD, the participants underwent further screening with liver biopsies and transient elastography.
People found to have NASH with Stage 2 entered a year-long behavior program to help them with weight loss and lifestyle changes. They found the for participants with stage 2 fibrosis or higher, the screening and lifestyle intervention was just as cost-effective compared to the group with no screening.
“Our results indicate the potential value and cost-effectiveness of NAFLD screening” in people with type 2 diabetes, wrote the study authors. “Given the increasing burden of NAFLD/NASH and the expected rapid increase in approved medications, we recommend screening patients with type 2 diabetes for NAFLD.”
Click this link to read more about Screening People with Type 2 for Liver Disease.
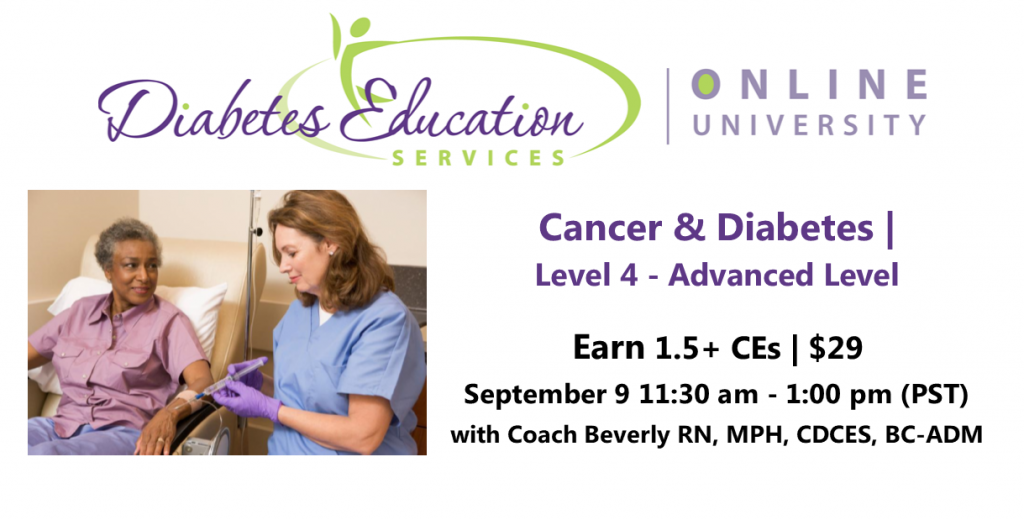
People with cancer often experience hyperglycemia secondary to treatment, which can increase risk of infection and compromise their nutritional status. In addition, recent research has identified the link between diabetes and cancer. Join us to learn more about this unexpected link and treatment strategies for steroid-induced hyperglycemia using a case study approach.
Topics Include:
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
[yikes-mailchimp form=”1″]Food insecurity in the United States has doubled over the past 20 years.

Food insecurity “exists whenever the availability of nutritionally adequate and safe foods or the ability to acquire acceptable foods in socially acceptable ways is limited or uncertain” as defined by S. A. Anderson.
According to a recent study published by JAMA Network:
Food deserts, socioeconomic status, ability, and other factors impact one’s access to nutritionally healthy foods.
“Food insecurity in North America is consistently more prevalent among households with a person living with diabetes, and similarly, diabetes is also more prevalent in food-insecure households,” states Enza Gucciardi in “The Intersection between Food Insecurity and Diabetes.”
For people living with diabetes who experience food insecurity, adhering to diabetes self-management (DSM) regimens can be more challenging.
Often this can put a person living with diabetes in a situation in which they have to decide between healthy foods, prescriptions, or other expenses.
As Diabetes Specialists, we can create person-centered, realistic plans that are coupled with accessible resources to better support those living with diabetes.
The USDA has created a list of Food Assistance programs that may be able to help those experiencing food insecurity.
Written by Bryanna, our Director of Operations & Customer Happiness
For more information on the JAMA published study click here. Additionally, read more from “The Intersection between Food Insecurity and Diabetes” by clicking here.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Can cinnamon help maintain glucose in those with prediabetes?

There have been several studies over the past decade to determine the efficacy of using cinnamon supplements to regulate blood sugars. Most of the studies found either no significant change or slight changes.
For example, a 2013 study of 70 different participants found that those who took 1 gram of cinnamon daily showed no significant changes over 30 or 60 days.
However, a recent study found that cinnamon supplements may be beneficial over time for improving glucose homeostasis in prediabetes.
This study, conducted by Giulio R. Romeo, MD, from the Joslin Diabetes Center in Boston, and Dr. Romeo’s colleagues spanned over 12 weeks across 45 participants who met the criteria for prediabetes. These participants, who were not taking a placebo, took 500mg of cinnamon supplements a day to see the impact on glucose control.
From a similar baseline, FPG rose after 12 weeks with placebo but remained stable with cinnamon, leading to a mean between-group difference of 5 mg/dL (P<0.05). When compared to the respective baseline, cinnamon, but not placebo, resulted in a significant decrease of the AUC PG (P<0.001) and of the 2-hr PG of the OGTT (P<0.05). There were no serious adverse events in either study group.
Their study found that fasting plasma glucose (FPG) rose for those who took the placebo. For those who took cinnamon supplements, their area over the curve (AUC) plasma glucose (PG) decreased along with their 2 hour PG by oral glucose tolerance test (OGTT).
The results suggest that over time, a cinnamon supplement of 500mg a day may help blood glucose levels for those with prediabetes.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

A committee of experts provides recommendations for healthy eating twice every decade. These final recommendations are sent to the US Department of Health and Human Services and the US Department of Agriculture, which use them to create the final 2020 dietary guidelines for Americans.
For the first time ever, the panel is including nutrition guidelines for infants 2 years and younger, with a pointed focus on reducing sugar consumption.
On average, infants consume a teaspoon of added sugar a day while toddlers consume about 6 teaspoons a day.
“Nutritional exposures during the first 1,000 days of life not only contribute to long-term health but also help shape taste preferences and food choices.”
2020 Dietary Guidelines Report
The committee also recommended further reductions in sugar intake for those age 2 and beyond. They also suggested less alcohol for men.
Read more about the 2020 Dietary Recommendations

Visit our Joy of Six Resource Page which has handouts and other helpful info on strategies to decrease sugar intake.