
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Why is JR’s blood glucose elevated?
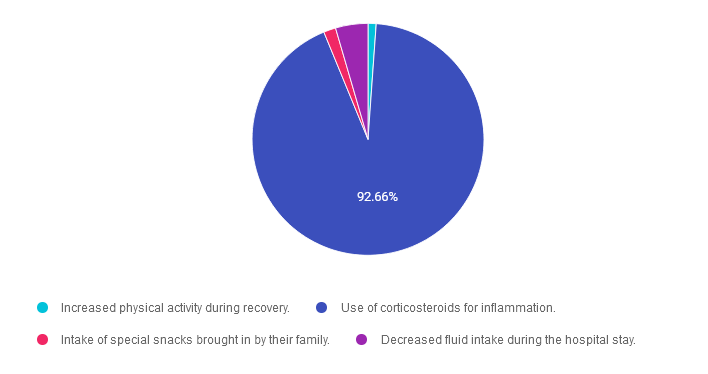
For last week’s practice question, we quizzed participants on why JR’s blood glucose is elevated. The majority of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: During a hospital stay, JR, who has no prior history of diabetes experiences elevated blood glucose levels.
Which of the following factors is the most likely cause of this hyperglycemia during hospitalization?
Answer Choices:
- Increased physical activity during recovery.
- Use of corticosteroids for inflammation.
- Intake of special snacks brought in by their family.
- Decreased fluid intake during the hospital stay.
Getting to the Best Answer
Answer 1 is incorrect. 1.13% chose this answer. “Increased physical activity during recovery.” Physical activity would most likely contribute to lowering glucose levels.
Answer 2 is correct. 92.66% of you chose this answer. “Use of corticosteroids for inflammation.” GREAT JOB. The vast majority of you chose this best answer. Steroids are notorious for increasing insulin resistance and contributing to hyperglycemia.
Answer 3 is incorrect. About 1.69% of respondents chose this. “Intake of special snacks brought in by their family.” While snacks may cause an increase in blood glucose, steroids pack a much more potent glucose raising punch.
Finally, Answer 4 is incorrect. 4.52% chose this answer. “Decreased fluid intake during the hospital stay.” While dehydration is often co-associated with hyperglycemia, it is not likely to cause extreme hyperglycemia. The better answer is steroid therapy as the cause of elevated blood sugars.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
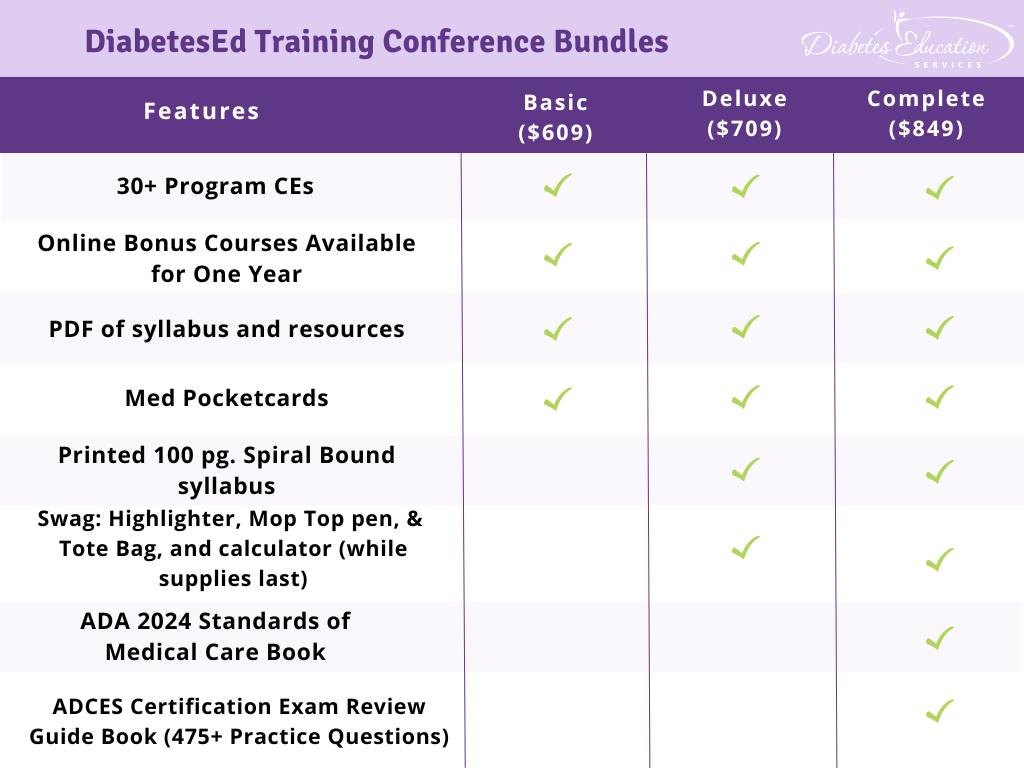
Join us Live in Beautiful San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

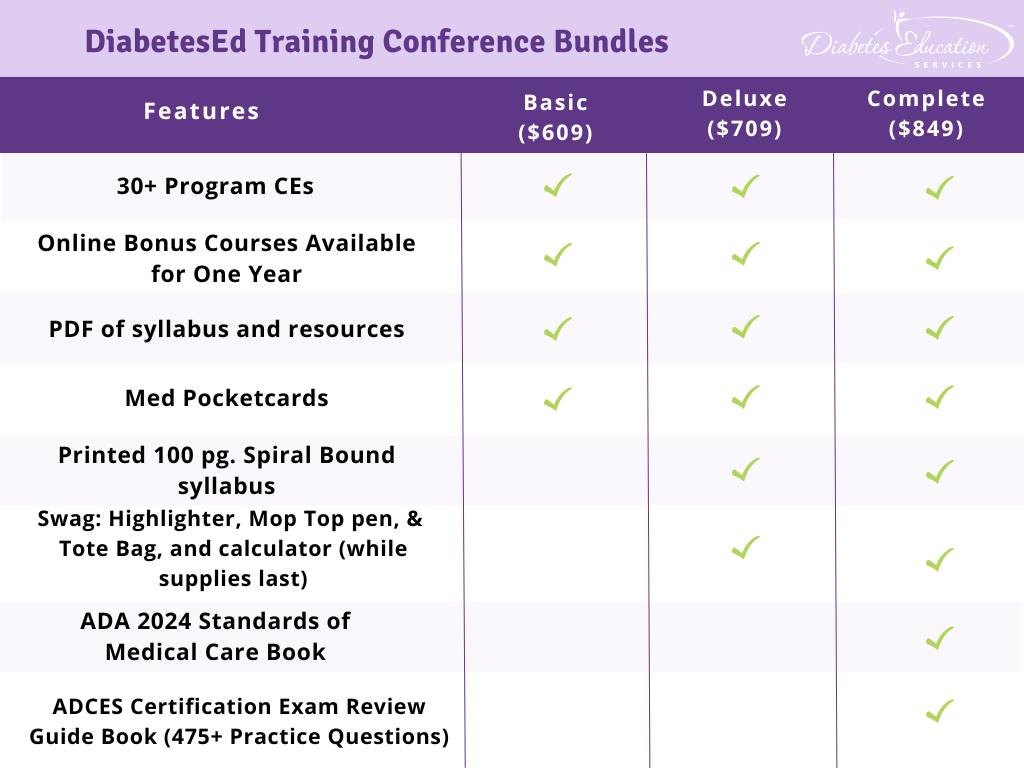
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
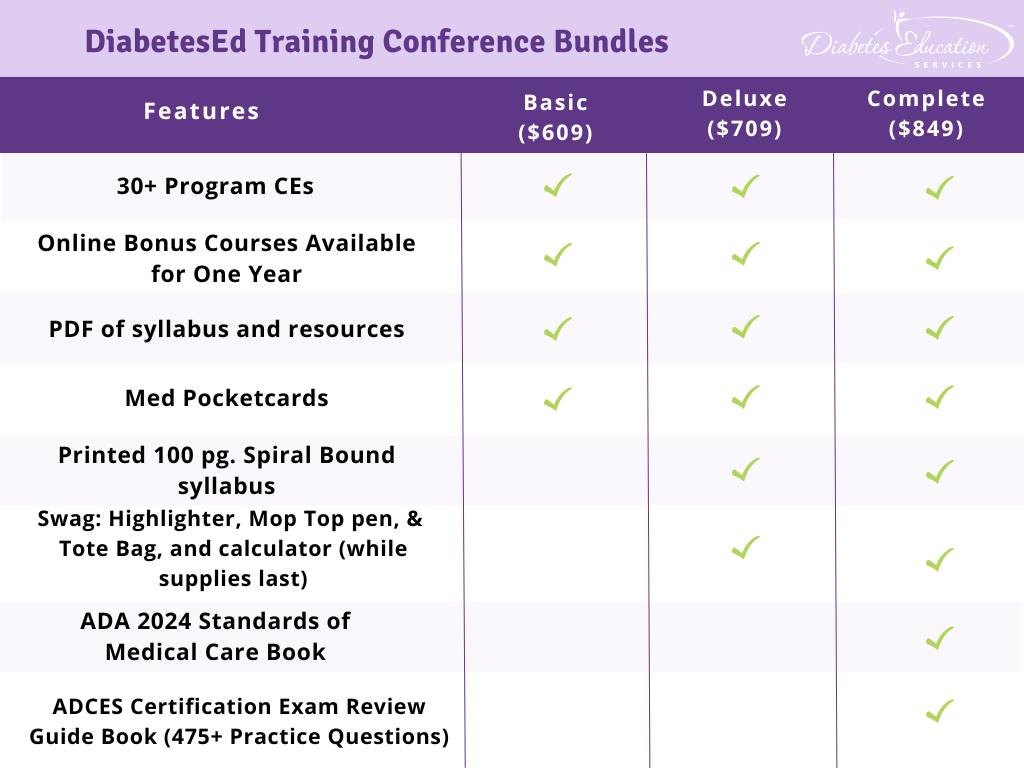
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Hypoglycemia and Hospitalization: Is there a Connection?
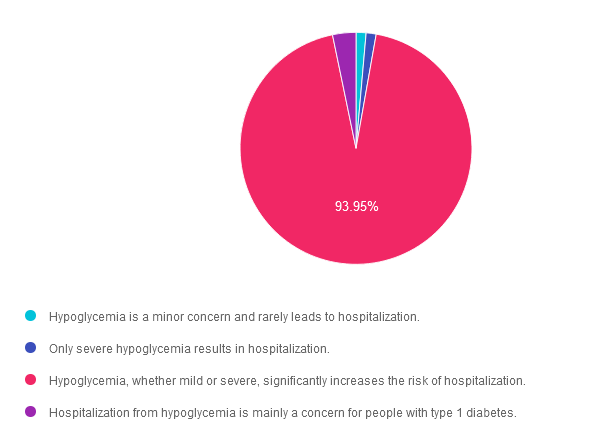
For last week’s practice question, we quizzed participants on the connection with hypoglycemia and hospitalizations. Almost all of the respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JR is 79 years old and takes insulin 3 times daily. Lately, they have been experiencing increased episodes of hypoglycemia.
Which of the following statements is true regarding hypoglycemia and the risk of hospitalization?
Answer Choices:
- Hypoglycemia is a minor concern and rarely leads to hospitalization.
- Only severe hypoglycemia results in hospitalization.
- Hypoglycemia, whether mild or severe, significantly increases the risk of hospitalization.
- Hospitalization from hypoglycemia is mainly a concern for people with type 1 diabetes.
Getting to the Best Answer
Answer 1 is incorrect. 1.4% chose this answer. “Hypoglycemia is a minor concern and rarely leads to hospitalization.” Hypoglycemia can lead to falls, confusion and loss of consciousness, all of which can precipitate hospitalization.
Answer 2 is incorrect. 1.4% of you chose this answer. “Only severe hypoglycemia results in hospitalization.” Even mild hypoglycemia can lead to falls and confusion, and if not treated, can worsen and result in loss of consciousness and hospitalization.
Answer 3 is correct. About 93.95% of respondents chose this. “Hypoglycemia, whether mild or severe, significantly increases the risk of hospitalization.” GREAT JOB! This is the best answer. Creating a collaborative plan to PREVENT hypoglycemia is especially important for people taking secretagogues or using insulin therapy.
Finally, Answer 4 is incorrect. 3.26% chose this answer. “Hospitalization from hypoglycemia is mainly a concern for people with type 1 diabetes.” Older people with type 2 diabetes and diminished renal function, who use insulin or secretagogues to lower glucose levels, are at risk of severe hypoglycemia and require close glucose monitoring.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us Live in Beautiful San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

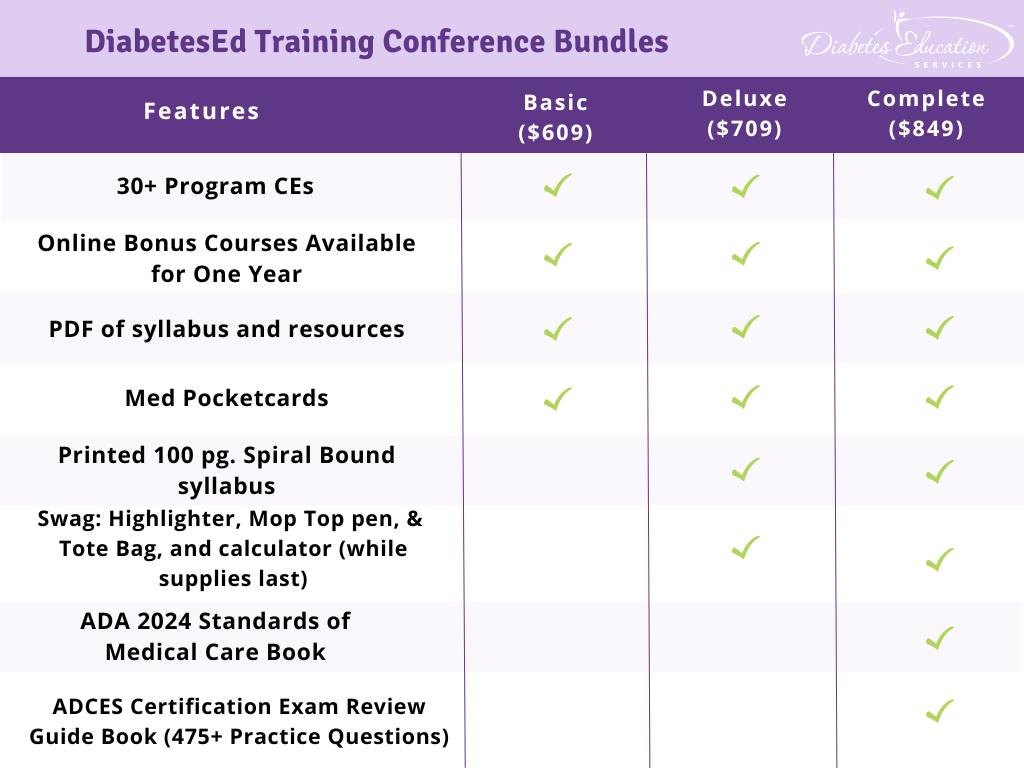
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
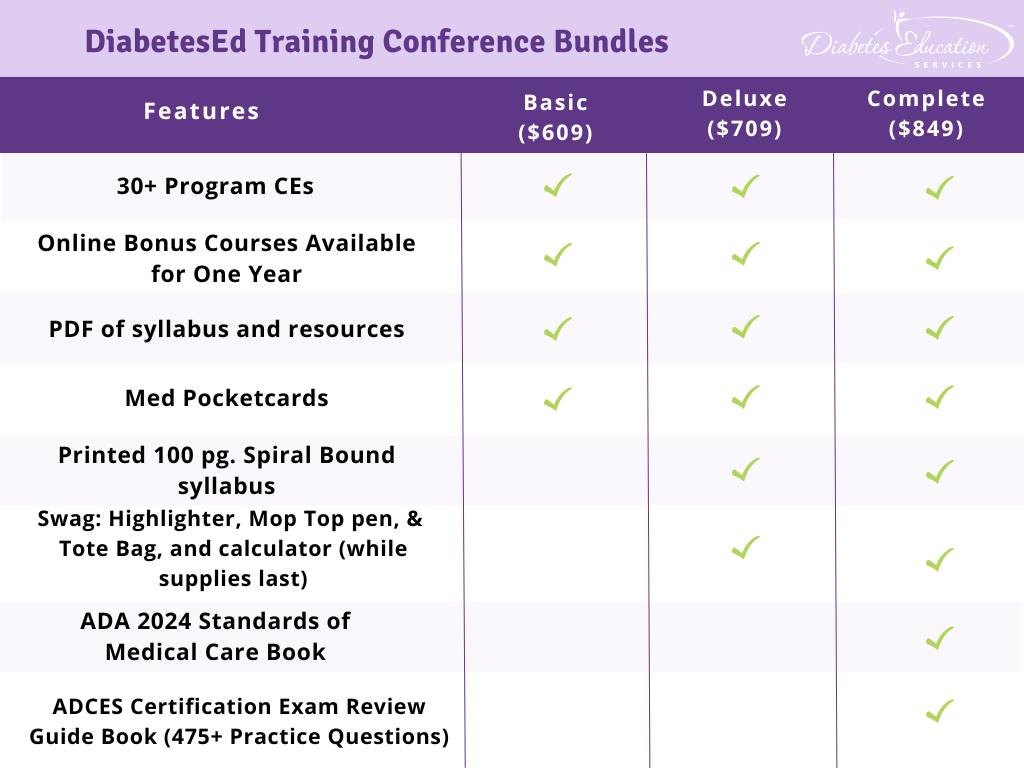
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Older Adults & Goals for Care
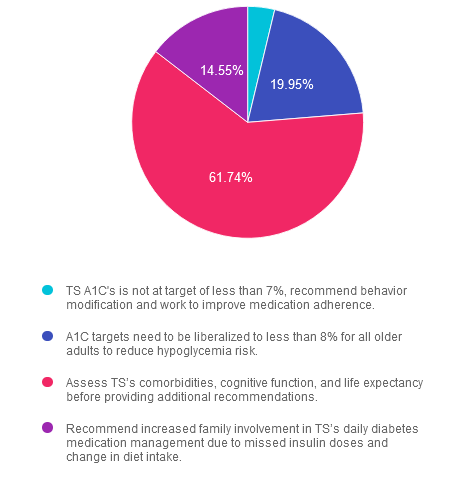
For last week’s practice question, we quizzed participants on older adults and goals for care. 62% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: TS is 82 years old, living with type 1 diabetes for the past 56 years. They present to the clinic with their family for diabetes care and education. TS’s last A1c was 7.6%, with a Time in the Range of 64% and Time below the Range of 1%. TS lives alone and self-manages their medications, and the family reports concern of potential missed insulin doses and dietary intake patterns are less consistent over the past few months.
Considering diabetes management in older adults, what recommendations would you give TS and his family?
Answer Choices:
- TS’s A1C is not at target of less than 7%, recommend behavior modifications and work to improve medication adherence.
- A1C targets need to be liberalized to less than 8% for all older adults to reduce hypoglycemia risk.
- Assess TS’s comorbidities, cognitive function, and life expectancy before providing additional recommendations
- Recommend increased family involvement in TS’s daily diabetes medication management due to missed insulin doses and change in diet intake.
Getting to the Best Answer
Answer 1 is incorrect. 3.76% chose this answer. “TS’s A1c is not at target of less than 7%, recommend behavior modifications and work to improve medication adherence.” Answer 1 is incorrect. The American Diabetes Association 2024 Standards of Care recommends personalizing glycemic targets for adults over 65 depending on comorbidities, cognitive and functional status, and living situations. An A1c of less than 7% may not be appropriate.
Answer 2 is incorrect. 19.95% of you chose this answer. “A1c targets should be liberalized to less than 8% for all older adults to reduce hypoglycemia risk.” Answer 2 is incorrect. While it is true we may liberalize A1c targets for older adults to prevent hypoglycemia, it is not the best answer. Older adults over 65 who are otherwise healthy, have stable coexisting chronic conditions, and have intact functional and cognitive status may benefit from lower glycemic goals (less than 7 to less than 7.5%).
Answer 3 is correct. About 61.74% of respondents chose this. “Assess TS’s comorbidities, cognitive function, and life expectancy before providing additional recommendations.” Answer 3 is the correct action. In older adults with diabetes, assessing comorbidities, cognitive function, and life expectancy is important to allow for the personalization of diabetes management recommendations and care goals.
Finally, Answer 4 is incorrect. 14.55% chose this answer. “Recommend increased family involvement in TS’s daily diabetes medication management due to missed insulin doses and change in diet intake.” Answer 4 is incorrect. We need more information to conclude that TS needs additional family support today. Completing a comprehensive evaluation, including cognitive function screening, is essential before providing recommendations.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us Live in Sunny San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
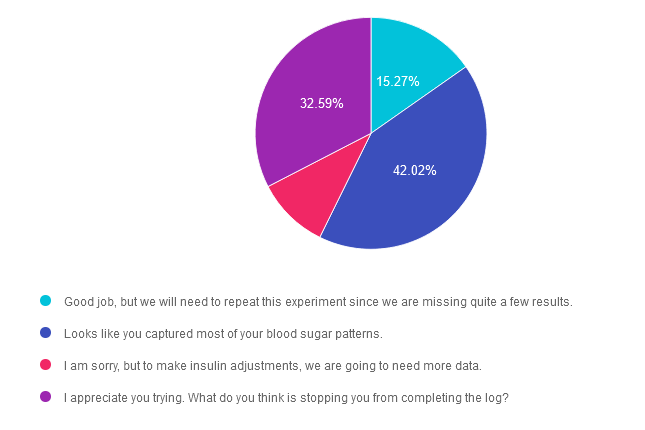
Rationale of the Week | Blood Glucose Data Missing – Best Response?
For last week’s practice question, we quizzed participants on best response for missing blood glucose data. 42% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JR returns to clinic after trying to keep a three day 7-point data log. Looking at log, the diabetes specialists notice several blood sugar readings are missing.
What is the best response?
Answer Choices:
Good job, but we will need to repeat this experiment since we are missing quite a few results.
Looks like you captured most of your blood sugar patterns.
I am sorry, but to make insulin adjustments, we are going to need more data.
I appreciate you trying. What do you think is stopping you from completing the log?
Getting to the Best Answer
Answer 1 is incorrect. 15.27% chose this answer. “Good job, but we will need to repeat this experiment since we are missing quite a few results.” A 7-point log means that we are asking a person with diabetes to document their before and after meal glucose levels 3 times a day in addition to a middle of the night blood glucose. If we ask them to do this for 3 days, that means they are documenting 21 blood sugars over a 3 day period. If they are only missing several readings, we would consider that a success. We can certainly use the data they have collected to collaborate on problem solving and strategizing to support their future goals.
Answer 2 is correct. 42.02% of you chose this answer. “Looks like you captured most of your blood sugar patterns.” Yes, GREAT JOB! If they are only missing several readings, we would consider that a success. We can certainly use the data they have collected to collaborate on problem solving and strategizing to support their future goals.
Answer 3 is incorrect. About 10.12% of respondents chose this. “I am sorry, but to make insulin adjustments, we are going to need more data.” A 7-point log means that we are asking a person with diabetes to document their before and after meal glucose levels 3 times a day in addition to a middle of the night blood glucose. If we ask them to do this for 3 days, that means they are documenting 21 blood sugars over a 3 day period. If they are only missing several readings, we would consider that a success. We can certainly use the data they have collected to collaborate on problem solving and strategizing to support their future goals.
Finally, Answer 4 is incorrect. 32.59% chose this answer. “I appreciate you trying. What do you think is stopping you from completing the log?” If they are only missing several readings, we would consider that a success. We can certainly use the data they have collected to collaborate on problem solving and strategizing to support their future goals.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us Live in Beautiful San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | How much bolus insulin at each meal?
For last week’s practice question, we quizzed participants on how much basal bolus insulin at each meal. 50% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Answer Choices:
- 3 units
- 5 units
- 6-7 units
- More information is needed to determine bolus dose.
Question: KT weighs 60 Kgs and is newly diagnosed with diabetes and needs to start insulin therapy.
Based on the 50/50 rule for determining insulin dosing, which of the following is the most accurate bolus dose for each meal?
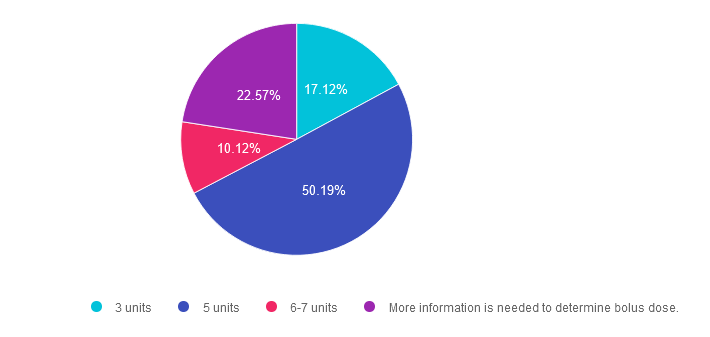
Getting to the Best Answer
Answer 1 is incorrect. 17% chose this answer. “3 units.” The 50/50 rule for insulin is a dosing strategy based on body weight. The formula looks like this; Take body weight is kg times 0.5 to get total daily needs per day. Then give 50% as basal and 50% as bolus insulin. The last step is to divide the bolus insulin by 3 meals to get the meal time bolus dose. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal.
Answer 2 is correct. 50% of you chose this answer. “5 units.” Yes, this is the BEST answer. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal. Super easy.
Answer 3 is incorrect. About 10% of respondents chose this. “6-7 units.” The 50/50 rule for insulin is a dosing strategy based on body weight. The formula looks like this; Take body weight is kg times 0.5 to get total daily needs per day. Then give 50% as basal and 50% as bolus insulin. The last step is to divide the bolus insulin by 3 meals to get the meal time bolus dose. Since KT weighs 60kg, here is how you do the math; 60kg x 0.5 = 30 units total insulin a day. 50% or 15 units is dedicated to basal insulin and 50% or 15 units is dedicated to bolus insulin. Now, divide the 15 units bolus insulin by 3 meals, which equals 5 units per meal.
Finally, Answer 4 is incorrect. 22.57% chose this answer. “More information is needed to determine bolus dose.” Although this is a tempting answer, it’s not the best answer since this is a straight forward dosing calculation problem. There is no information about their social determinants of health or any barriers. Given those facts, answer B is the best answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Recorded & Ready to Watch
Insulin Calculation Workshop | From Pumps & Beyond
Level 4 | Advanced Level & Specialty Topics
Determining basal & bolus rates for multiple daily injections or insulin pumps can seem overwhelming. This course provides participants with a step-by-step approach to determining basal rates, bolus ratios & how to problem-solve when blood glucose levels aren’t on target. During this course, Coach Beverly provides abundant case studies to give participants hands-on practice & build confidence when calculating insulin doses for a variety of situations.
Objectives:
- Describe using formulas to determine appropriate insulin dosing.
- Discuss strategies to determine & fine-tune basal insulin dose.
- Describe how to determine & fine-tune bolus rates including coverage for carbs & hyperglycemia.
- Using a case study approach, utilize calculations to determine the best insulin dosing strategy.
Learning Outcome:
Participants will have an increased knowledge of how to calculate bolus/basal insulin therapy based on person-specific factors and will be able to recommend insulin adjustments based on individual needs.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 10.3.1
- 10.5.3
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best Move to Get Glucose to Goal?
For last week’s practice question, we quizzed participants on getting glucose to goal. 60% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS wears an insulin pump and uses lispro insulin. LS has an average basal rate of 0.6 units and hour, a 1:15 carb ratio and a 1:50 correction ratio. Based on the ambulatory glucose profile, LS is experiencing elevated glucose levels from 4am to 7am.
To get glucose to target, what is the best next step?
Answer Choices:
- Add basal insulin glargine to prevent Somogyi effect.
- Increase the basal rate to prevent glucose elevations.
- Make sure LS isn’t consuming carbohydrates after 10pm.
- Ask LS to double check their CGM insertion site.
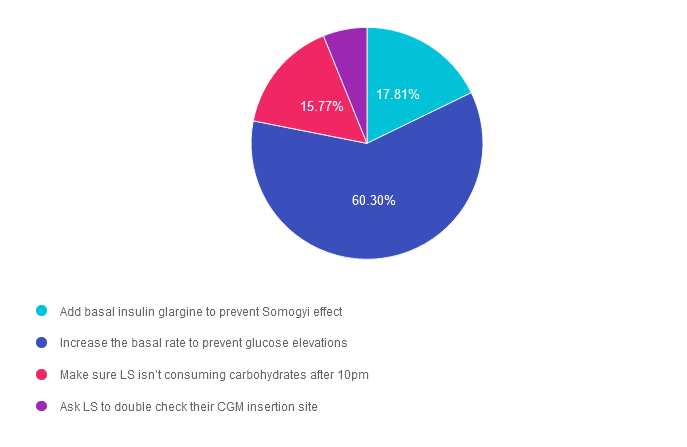
Getting to the Best Answer
Answer 1 is incorrect. 17.81% chose this answer.” Add basal insulin glargine to prevent Somogyi effect.” If a person is using insulin pump therapy, glargine injections would not be added in addition to the pump therapy. In addition, no basal insulins (like glargine) are used in pump therapy, only bolus insulins. Lastly, Somogyi effect is defined as a hypoglycemic event that triggers a burst of counterregulatory hormones that causes a substantial increase in blood glucose. There is no evidence that the person is experiencing hypoglycemia in this scenario.
Answer 2 is correct. 60.30% of you chose this answer. “Increase the basal rate to prevent glucose elevations.” YES, this is the best answer. LS is most likely experiencing Dawn Phenomena, which if the natural rise in blood sugars starting around 3-4 am due to the early morning release of cortisol and growth hormones. By increasing the pump’s basal rate to match this insulin resistant phase, we can help LS get blood glucose closer to target.
Answer 3 is incorrect. About 15.77% of respondents chose this. “Make sure LS isn’t consuming carbohydrates after 10pm.” This juicy answer does not explain why LS’s blood glucose always rises at 4am. Also, people with diabetes have the freedom to eat carbohydrates throughout the day and evening, they would just need to provide adequate bolus insulin coverage for late night carbs.
Finally, Answer 4 is incorrect. 6.12% chose this answer. “Ask LS to double check their CGM insertion site.” Since we can see a pattern of blood glucose levels rising each day at 4am, we assume that the CGM working correctly (we can always double check using a glucose meter to confirm)
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Now Recorded & Ready to Watch
Insulin Calculation Workshop | From Pumps & Beyond
Level 4 | Advance Level & Specialty Topics

Determining basal & bolus rates for multiple daily injections or insulin pumps can seem overwhelming. This course provides participants with a step-by-step approach to determining basal rates, bolus ratios & how to problem-solve when blood glucose levels aren’t on target. During this course, Coach Beverly provides abundant case studies to give participants hands-on practice & build confidence when calculating insulin doses for a variety of situations.
Objectives:
- Describe using formulas to determine appropriate insulin dosing.
- Discuss strategies to determine & fine-tune basal insulin dose.
- Describe how to determine & fine-tune bolus rates including coverage for carbs & hyperglycemia.
- Using a case study approach, utilize calculations to determine the best insulin dosing strategy.
Learning Outcome:
Participants will have an increased knowledge of how to calculate bolus/basal insulin therapy based on person-specific factors and will be able to recommend insulin adjustments based on individual needs.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 10.3.1
- 10.5.3
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | Insulin Calculation Workshop | From Pumps & Beyond awards 1.5 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Medical Nutrition Therapy Coverage
For last week’s practice question, we quizzed participants on medical nutrition therapy coverage. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: SJ is a 68-year-old recently referred for medical nutrition therapy (MNT). They are on a fixed income and are concerned about their out-of-pocket expense for their upcoming visit. SJ has Medicare (CMS) as their primary insurance.
What can we tell SJ about Medicare’s coverage for MNT services?
Answer Choices:
- Medicare provides full coverage and no cost share for all Medical Nutrition Therapy referrals.
- Medicare provides 3 hours of MNT services for the initial referral and calendar year and 2 hours after referral in subsequent years.
- Medicare provides coverage for diagnosis of diabetes, non-dialysis CKD stage 3- 5, and post-kidney transplants.
- Both B and C.
- All of the Above.
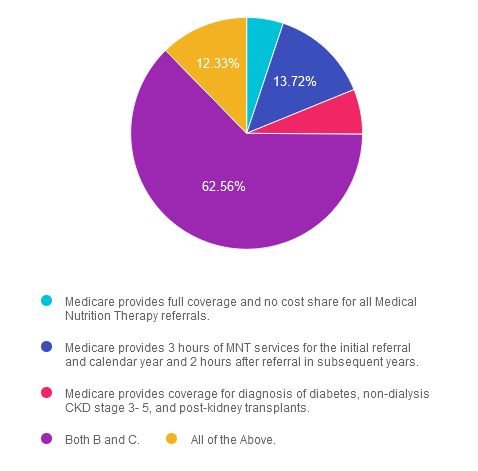
Getting to the Best Answer
Answer 1 is incorrect. 5.12% chose this answer. “Medicare provides full coverage and no cost share for all Medical Nutrition Therapy referrals.” While it is true that Medicare provides full coverage and no out-of-pocket cost share, not ALL MNT referrals are covered. Despite continued work towards increasing MNT access, currently, Medicare only provides coverage for specific diagnoses. Referrals must also come from a physician (MD and DO). Medicare does not accept referrals from an NP or PA. Keep reading for more information.
Answer 2 is incorrect. 13.72% of you chose this answer. “Medicare provides 3 hours of MNT services for the initial referral and calendar year and 2 hours after referral in subsequent years.” This answer is true but not the best answer. Medicare will provide coverage of up to 3 hours of MNT services for the first year of referral and 2 hours every calendar year thereafter with physician referral. If a provider determines medical necessity, most often from a change in diagnosis, treatment regimen, or medical condition, a second referral will allow additional hours of MNT services.
Answer 3 is incorrect. About 6.28% of respondents chose this. “Medicare provides coverage for diagnosis of diabetes, non-dialysis CKD stage 3- 5, and post-kidney transplants.” This answer is true but not the best answer. Medicare provides coverage for diabetes diagnoses, non-dialysis CKD stages 3-5, and post-kidney transplants within the last 36 months.
Answer 4 is correct. 62.56% chose this answer. “Both B and C.” Answer D is correct and the best answer.
Finally, Answer 5 is incorrect. 12.33% chose this answer. “All of the Above.” Answer E is incorrect and not the best answer. While advocacy for expansion of MNT services to cover other diagnosis is an active effort, at the time of writing, coverage remains for only the prior mentioned diagnoses.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us Live in Sunny San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Understanding Ankle Brachial Index – What is True?
For last week’s practice question, we quizzed participants on understanding ankle brachial index. 68% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: People of color living with diabetes are at increased risk of lower extremity complications and amputations. Ankle-Brachial Index (ABI) measures lower extremity vessel disease in individuals with diabetes and is an important tool to evaluate risk of future complications.
Which of the following is true regarding ABI?
Answer Choices:
- ABI result of less than 0.90 indicates peripheral arterial disease.
- ABI compares brachial systolic blood pressures between left and right arms.
- People with bounding pulses in lower extremities benefit from ABI testing.
- ABI testing can only be conducted by a vascular specialist.
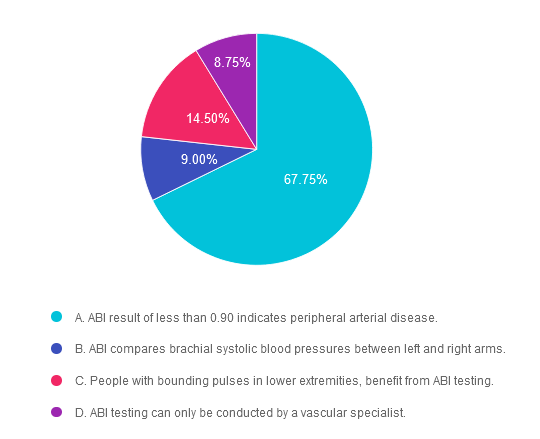
Getting to the Best Answer
Answer 1 is correct. 67.75% chose this answer. “ABI result of less than 0.90 indicates peripheral arterial disease.” GREAT JOB. The ABI is a ratio that measures arterial perfusion in the upper extremities compared to the lower extremities. In brief, the ABI compares the systolic brachial pressure in the arm to the systolic pressure of the lower extremity (using the posterior tibial or dorsalis pedis pressure). To indicate adequate arterial circulation, the lower extremity pressure should be equal to the brachial pressure, or a ratio of 0.99 or better. Therefore, an ABI of less than 0.99 indicates decreased arterial circulation in lower extremities; an alert of peripheral arterial disease (PAD) People with peripheral arterial disease may also complain of pain in calves, legs or buttocks when walking that is relieved by stopping movement. Discovery of PAD requires referral to a specialist to determine next steps to treat PAD and to mitigate future risk of lower extremity complications and heart disease. For more info, we offer a FREE webinar called 3 Steps to DeFeet Amputation. Assess, Screen Report.
Answer 2 is incorrect. 9.0% of you chose this answer. “ABI compares brachial systolic blood pressures between left and right arms.” The ABI is a ratio that measures arterial perfusion in the upper extremities compared to the lower extremities. In brief, the ABI compares the systolic brachial pressure in the arm to the systolic pressure of the lower extremity (using the posterior tibial or dorsalis pedis pressure). For more info, we offer a FREE webinar called 3 Steps to DeFeet Amputation. Assess, Screen Report.
Answer 3 is incorrect. About 14.5% of respondents chose this. “People with bounding pulses in lower extremities benefit from ABI testing.” Bounding pulses in the lower extremity is a positive sign of adequate lower extremity circulation. For more info, we offer a FREE webinar called 3 Steps to DeFeet Amputation. Assess, Screen Report.
Finally, Answer 4 is incorrect. 8.75% chose this answer. “ABI testing can only be conducted by a vascular specialist.” ABI can be conducted in a variety of medical settings as long as the health care professional has completed training on how to perform an accurate ABI, For more info, we offer a FREE webinar called 3 Steps to DeFeet Amputation. Assess, Screen Report.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
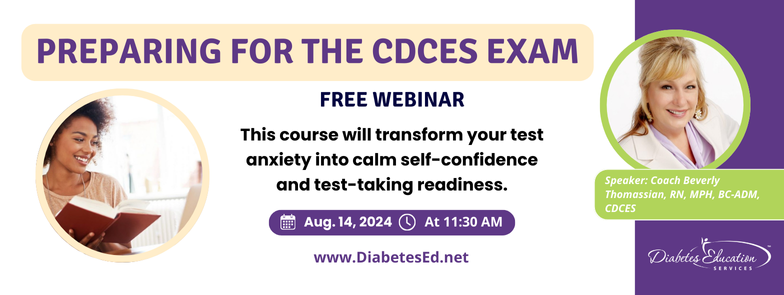
Why become a CDCES?
Three Reasons from Coach Beverly
Read More: 3 Reasons to Become a CDCES “The best part of becoming a CDCES is working with my colleagues and people living with diabetes. As diabetes educators, we hear compelling and beautiful life stories. I am astounded by the barriers they face and inspired by their adaptability, problem-solving skills, and resilience.“ Reason 1: CDCES is a widely recognized certification by employers and health care professionals throughout the U.S. This credential demonstrates a specialized and in-depth knowledge in the prevention and treatment of individuals living with pre-diabetes and diabetes. Reason 2: Currently, 13% of people in the U.S. have diabetes and another 36% have pre-diabetes which means 49% of Americans are running around with elevated blood glucose levels. Given this epidemic, there will be plenty of future job opportunities. Reason 3: Having my CDCES along with my nursing degree, has opened many doors of opportunity; from working as an inpatient Diabetes Nurse Specialist in a hospital to working as a Manager of Diabetes Education in the outpatient setting to starting my own consulting company.
- Exam requirement updates and eligibility
- New test format starting in July 2024
- Strategies to succeed along with a review of study tips and test-taking tactics.
- We will review sample test questions and the reasoning behind choosing the right answers.
- Learn how to focus your time and prepare to take the CDCES Exam.
- We provide plenty of sample test questions and test-taking tips!
Can’t join us live?
Don’t worry, we will send you a link to the recorded version.
Instructor

Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician, and Innovator, Beverly has specialized in diabetes management for over twenty years and has successfully passed the CDCES exam six times. As president and founder of Diabetes Education Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
“Becoming a Certified Diabetes Care and Education Specialist (CDCES) is one of the best professional and personal decisions I have ever made.” – Coach Beverly Thomassian
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.






