
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Why did 16 year old stop taking meds?
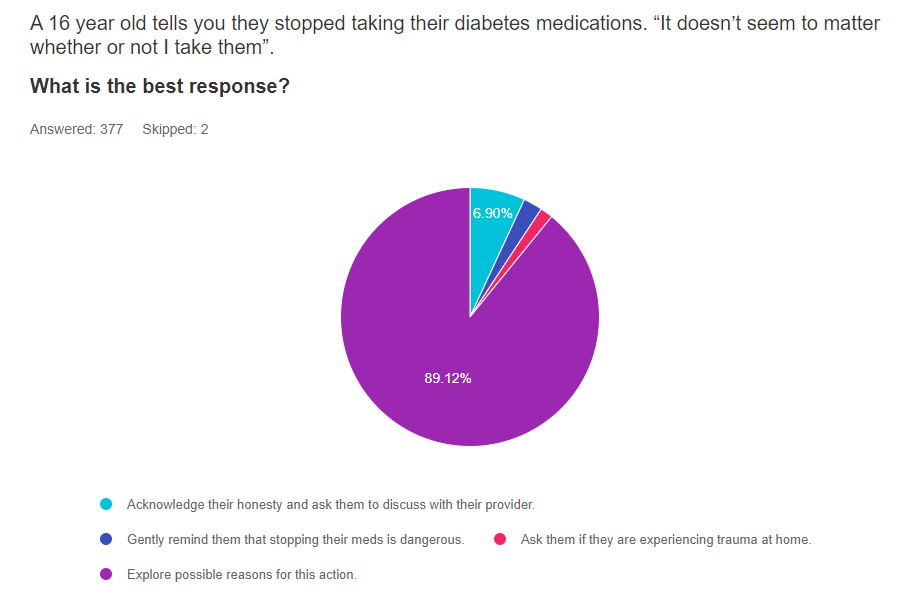
For last week’s practice question, we quizzed participants on Why a 16 year old stopped taking their medication. 88% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: A 16 year old tells you they stopped taking their diabetes medications. “It doesn’t seem to matter whether or not I take them”.
What is the best response?
Answer Choices:
- Acknowledge their honesty and ask them to discuss with their provider.
- Gently remind them that stopping their meds is dangerous.
- Ask them if they are experiencing trauma at home.
- Explore possible reasons for this action.
Getting to the Best Answer
Answer 1 is incorrect. 6.9% chose this answer. “Acknowledge their honesty and ask them to discuss with their provider.” The first part of this answer is correct. We want to acknowledge their honesty and provide a non-judgmental environment. However, we want to explore their feelings further as part of this current appointment instead of stopping the conversation and deferring to the provider. For more information on this topic, you are invited to our Language and Diabetes Webinar. We hope you can join us. See below for more info!
Answer 2 is incorrect.2.39% of you chose this answer. “Gently remind them that stopping their meds is dangerous.” This person is experiencing diabetes distress, so we want to acknowledge their feelings and explore strategies to decease distress. When people with diabetes are experiencing distress, approaching the situation with curiosity and non-judgment is always the best approach. For more information on this topic, you are invited to our Language and Diabetes Webinar. We hope you can join us. See below for more info!
Answer 3 is incorrect. About 1.59% of respondents chose this. “Ask them if they are experiencing trauma at home.” While trauma at home can cause significant distress, this individual has stopped taking their diabetes medications since they are not sure if they actually work. Asking about trauma at home doesn’t match the concern they are verbalizing at this moment. When people with diabetes are experiencing distress, approaching the situation with curiosity and non-judgment is always the best approach. For more information on this topic, you are invited to our Language and Diabetes Webinar. We hope you can join us. See below for more info!
Finally, Answer 4 is correct. 89% chose this answer. “Explore possible reasons for this action.” YES, this is the best answer and almost 90% of respondents chose this answer. GREAT JOB. When people with diabetes are experiencing distress, approaching the situation with curiosity and non-judgment is always the best approach. For more information on this topic, you are invited to our Language and Diabetes Webinar. We hope you can join us. See below for more info!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on July 11th at 11:30 am PST for our
Language and Diabetes FREE Webinar
What we say matters.
As educators, advocates, spouses, friends, and providers, our use of language can deeply affect the self-view of people living with diabetes every day.
Intentional communication is a powerful tool that can uncover trauma, identify barriers, and move both the provider and person with diabetes toward a greater understanding of the issues involved.
The language used in the health care setting is immensely important in determining trust, mutual respect, and meaningful long-term relationships.
Topics covered include:
- Learn phrases, words, and approaches that can be left behind.
- Describe diabetes language that is respectful, inclusive, person-centered, and imparts hope.
- Discuss how to evaluate for ACE and provide trauma-informed care
- Practice communicating about diabetes using phrases free from judgment with a focus on a strength-based approach
This webinar is free and you can view it at any time, on any device. To earn CEs, you can purchase this course at our online university store.
Coach Beverly Thomassian, RN, MPH, BC-ADM, CDCES
Author, Nurse, Educator, Clinician, and Innovator, Beverly has specialized in diabetes management for over twenty years. As president and founder of Diabetes Educational Services, Beverly is dedicated to optimizing diabetes care and improving the lives of those with diabetes.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | What does Medicare Cover?
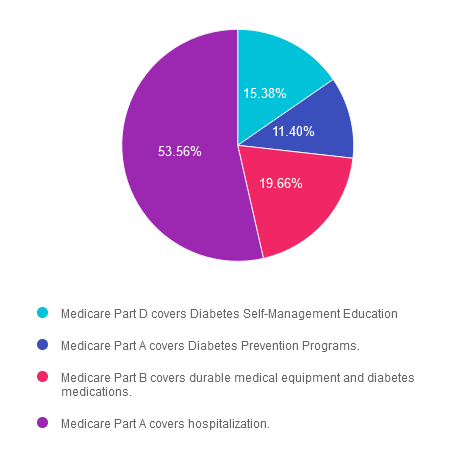
For last week’s practice question, we quizzed participants on what Medicare will cover. 54% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KT just turned 65 and asks you about Medicare Insurance Coverage for Diabetes.
Which of the following is accurate regarding Medicare Coverage for people living with diabetes?
Answer Choices:
- Medicare Part D covers Diabetes Self-Management Education
- Medicare Part A covers Diabetes Prevention Programs.
- Medicare Part B covers durable medical equipment and diabetes medications.
- Medicare Part A covers hospitalization.
Getting to the Best Answer
Answer 1 is incorrect. 15.38% chose this answer. “Medicare Part D covers Diabetes Self-Management Education.” Actually, medicare Part D helps cover the cost of prescription drugs. Part D is optional and only provided through private insurance companies approved by the federal government. However, Part D is offered to everyone who qualifies for Medicare. Costs and coverage may vary from plan to plan
Answer 2 is incorrect. 11.4% of you chose this answer. “Medicare Part A covers Diabetes Prevention Programs.” Actually, medicare part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
Answer 3 is incorrect. About 19.66% of respondents chose this. “Medicare Part B covers durable medical equipment and diabetes medications.” Part B doesn’t help cover diabetes medications, but Part B does cover:
- Services from doctors and other health care providers
- Diabetes Self-Management Education
- Outpatient care, Home health care
- Durable medical equipment (like meters, CGMs, wheelchairs, walkers, hospital beds, and other equipment)
- Many preventive services (like screenings, shots or vaccines, and yearly “Wellness” visits)
Finally, Answer 4 is correct. 53.56% chose this answer. “Medicare Part A covers hospitalization.” YES, GREAT JOB. This is the best answer.
Medicare Part A covers:
- Inpatient care in a hospital
- Skilled nursing facility care
- Nursing home care (inpatient care in a skilled nursing facility that’s not custodial or long-term care)
- Hospice care
- Home health care
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 2 | Setting up a Successful DSME Program awards 1.5 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Inpatient didn’t get bolus insulin before lunch. What is best action?
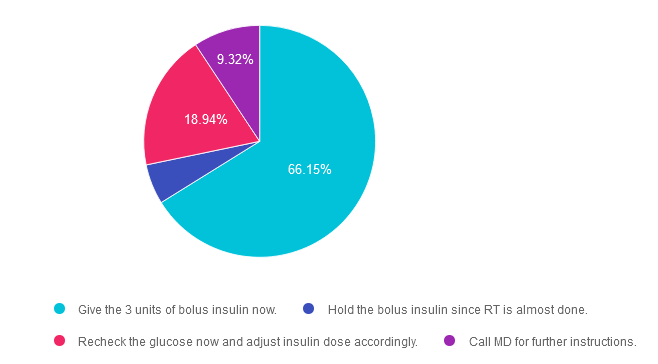
For last week’s practice question, we quizzed participants on missing bolus insulin before lunch, how should you follow up? 66% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: RT is in the hospital with pneumonia. Based on pre lunch glucose check, RT needs 3 units bolus insulin for lunch. RT’s blood glucose before lunch (20 minutes ago) was 173. You walk in room and RT is almost done with lunch.
What is best action?
Answer Choices:
- Give the 3 units of bolus insulin now.
- Hold the bolus insulin since RT is almost done.
- Recheck the glucose now and adjust insulin dose accordingly.
- Call MD for further instructions.
Getting to the Best Answer
Answer 1 is correct. 66.15% chose this answer. “Give the 3 units of bolus insulin now.” YES, this is the BEST answer. Since RT just checked their blood glucose 20 minutes ago, even though they have consumed most of their meal, it is best to give the bolus insulin now so the insulin can help blunt the post prandial increase. It also provides a great teaching moment to encourage individuals to give insulin before eating, to allow the insulin to start working to match the post meal increase from food.
Answer 2 is incorrect. 5.59% of you chose this answer. “Hold the bolus insulin since RT is almost done.” If we hold the bolus insulin, RT’s blood glucose level will go above target since there would be no insulin available to store the incoming carbohydrates in muscle and liver cells as glycogen.
Answer 3 is incorrect. About 18.94% of respondents chose this. “Recheck the glucose now and adjust insulin dose accordingly.” Unfortunately, this is not a good time to determine insulin needs based on glucose. Since RT is eating, the blood sugars are rising and we might end up giving too much insulin based on this temporary increase. It is best to determine insulin dose on premeal glucose and anticipated carb consumption.
Finally, Answer 4 is incorrect. 9.32% chose this answer. “Call MD for further instructions.” No need to call for instructions in this situation. If a person with diabetes experienced this situation at home, they would simply give their insulin mid-meal. In this situation, it won’t cause any harm to give the recommended dose now. It also provides a great teaching moment to encourage individuals to give insulin before eating, to allow the insulin to start working to match the post meal increase from food.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on [Air Date] for our
Hospitals & Hyperglycemia
Level 2 Standards of Care Intensive
Research demonstrates the importance of glucose control during hospitalization to improve outcomes not only in the inpatient setting but after discharge. This course reviews the evidence that supports inpatient glucose control & outlines practical strategies to achieve targets in the inpatient setting. We incorporate the latest American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provide links to resources & inpatient management templates.
Objectives:
- Describe the impact of hyperglycemia in the hospital setting.
- Discuss the importance of inpatient glucose control.
- List three strategies to get glucose to the goal in the hospital setting.
Learning Outcome:
The diabetes care team will gain insights and knowledge of special considerations, individualized goals, and standards for inpatients with diabetes that they can include in their practice.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.6.7
- 9.6.8
- 10.3.1
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | ADA Standards for Gestational Diabetes
For last week’s practice question, we quizzed participants on ADA standards for gestational diabetes. 43% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS has type 1 diabetes and is here for the first visit after confirmation of pregnancy. LS has been using non-adjunctive continuous glucose monitoring (CGM) along with insulin pump therapy to manage diabetes. Previous visits have focused on preconception counseling and last A1c was 6.4%.
According to the 2024 ADA Standards of Care, what do we recommend regarding glucose monitoring during pregnancy?
Answer Choices:
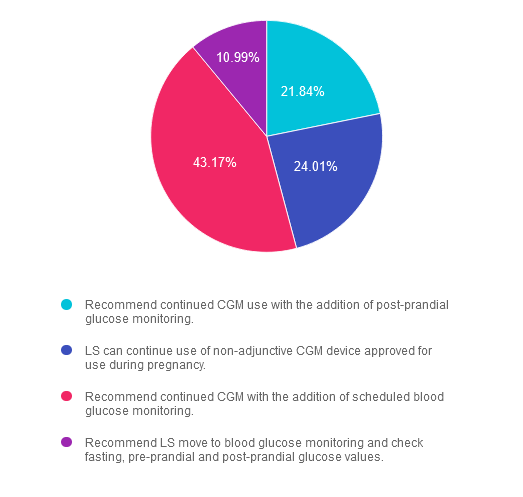
Getting to the Best Answer
Answer 1 is incorrect. 21.84% chose this answer. “Recommend continued CGM use with the addition of post-prandial glucose monitoring.” The 2024 ADA Standards of Care do recommend CGM use for individuals with type 1 diabetes during pregnancy but simply monitoring post-prandial glucose is insufficient. Keep reading below.
Answer 2 is incorrect. 24.01% of you chose this answer. “LS can continue use of non-adjunctive CGM device approved for use during pregnancy.” We can continue use of CGM devices during pregnancy, but blood glucose monitoring is recommended in addition to CGM.
Answer 3 is correct. About 43.17% of respondents chose this. GREAT JOB! “Recommend continued CGM with the addition of scheduled blood glucose monitoring.” The 2024 Standards of Care recommends CGM for individuals with type 1 diabetes during pregnancy but also recommends that it not replace pre-prandial and post-prandial blood glucose monitoring. Fasting, pre-prandial and post-prandial blood glucose monitoring is recommended for individuals with diabetes in pregnancy.
Finally, Answer 4 is incorrect. 10.99% chose this answer. “Recommend LS move to blood glucose monitoring and check fasting, pre-prandial and post-prandial glucose values.” We will recommend LS add blood glucose monitoring, but LS does not need to transition off CGM therapy.
Reference:
American Diabetes Association Professional Practice Committee; 15. Management of Diabetes in Pregnancy: Standards of Care in Diabetes—2024. Diabetes Care 1 January 2024; 47 (Supplement_1): S282–S294. https://doi.org/10.2337/dc24-S015
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Now Recorded & Ready to Watch
Pregnancy & Diabetes
Level 2 Standards of Care Intensive

Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Learning Outcome:
Participants will gain knowledge of special considerations, individualized goals, and standards for people experiencing diabetes during pregnancy to improve outcomes.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.6.7
- 9.6.8
- 10.3.1
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | What is the cause of this emergency room visit?
For last week’s practice question, we quizzed participants on what is the cause of LS’ ER visit based on lab results. 61% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS is a 29-year-old who arrives in the emergency room with known history of type 2 diabetes. BMI is 23.9 and they are on basal insulin therapy and an oral medication to help “clear extra sugar”. On admission, their blood glucose is 189, pH is 7.2 and LS has 3+ betahydroxybyturate.
What is the most likely cause of these lab results?
Answer Choices:
- LS is omitting insulin to lose weight.
- There is a lab error in the glucose reading.
- LS is taking a SGLT-2 Inhibitor
- New onset gastroparesis.
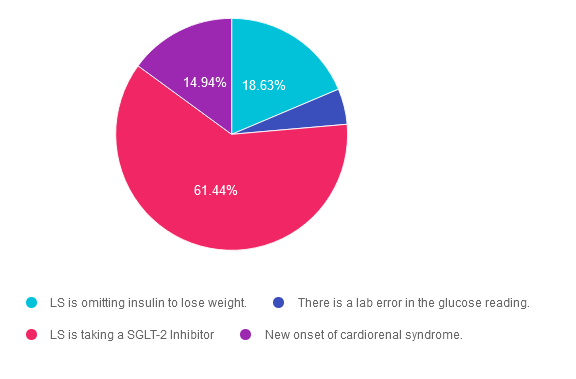
Getting to the Best Answer
Answer 1 is incorrect. 18.63% chose this answer. “LS is omitting insulin to lose weight.” Although this answer is tempting since LS has ketosis and acidosis, it doesn’t explain why the glucose level is so low. With insulin omission, the person would present in ketoacidosis with a blood sugar of 200 or greater. In addition, the question mentions that LS is taking a diabetes pill to help release the sugar through her urine. This is an important clue to get to the best answer.
Answer 2 is incorrect. 4.98% of you chose this answer. “There is a lab error in the glucose reading.” Since LS has ketosis and acidosis, it is confusing as to why the glucose level is so low. With insulin omission, the person would present in ketoacidosis with a blood sugar of 200 or greater. The question also mentions that LS is taking a diabetes pill to help release the sugar through her urine. This is an important clue to get to the best answer.
Answer 3 is correct. About 61.44% of respondents chose this. “LS is taking a SGLT-2 Inhibitor.” GREAT JOB. This is the best answer. LS has ketosis and acidosis, with a glucose level less than 200. Given her history, this meets the criteria for euglycemic DKA. Since the question mentions that LS is taking a diabetes pill to help release the sugar through her urine, this important clue gets us to the best answer. LS is taking a SGLT-2 inhibitor, which can lead to euglycemic DKA, especially during periods of illness or if they are not taking adequate insulin.
Finally, Answer 4 is incorrect. 14.94% chose this answer. “New onset gastroparesis.” This answer doesn’t really explain why LS is experiencing acidosis and ketosis. Many people with new onset gastroparesis struggle with post meal hypoglycemia and erratic blood sugar levels, but they do not generally struggle with euglycemic DKA. The question also mentions that LS is taking a diabetes pill to help release the sugar through her urine. This is an important clue to get to the best answer.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us Live in Sunny San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
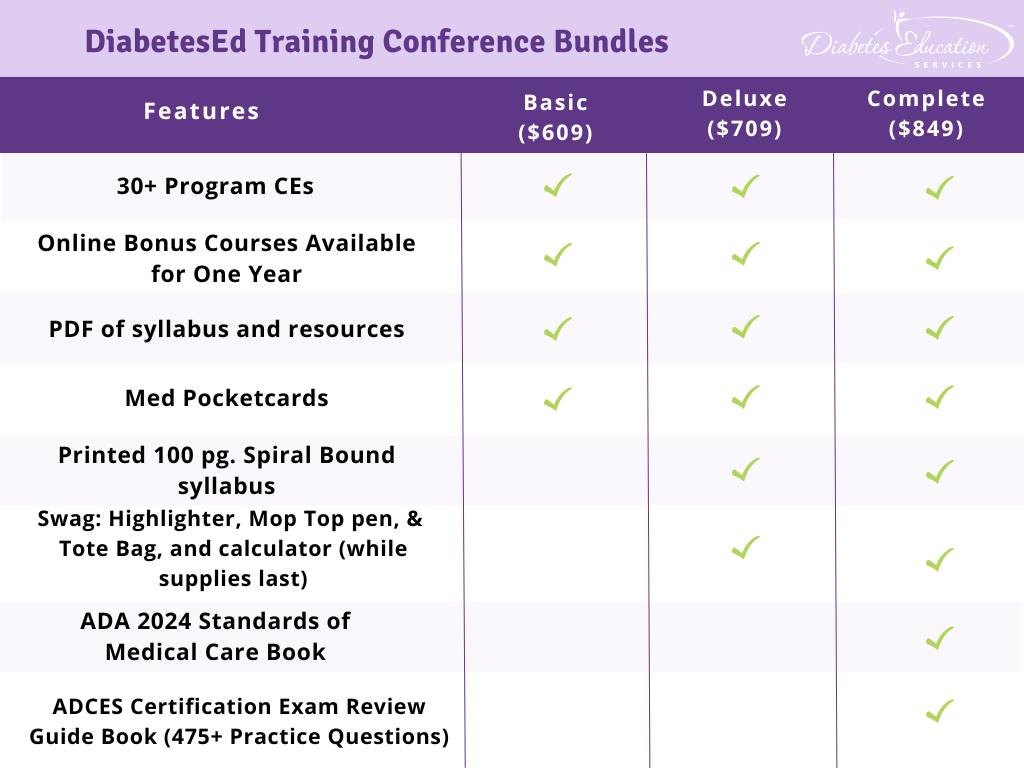
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | KR is on Metformin & 4 Weeks Pregnant. Best action?
For last week’s practice question, we quizzed participants on ADA recommendations for metformin while pregnant. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KR has polycystic ovary syndrome and takes metformin 850mg twice daily. KR just discovered they are 4 weeks pregnant. Fasting glucose is 103 mg/dl.
According to ADA Guidelines, if prediabetes diagnosis is confirmed, what is the next step?
Answer Choices:
- Continue metformin through first trimester.
- Start basal insulin, stop metformin.
- Add human basal bolus insulin.
- Stop metformin, start sulfonylurea.
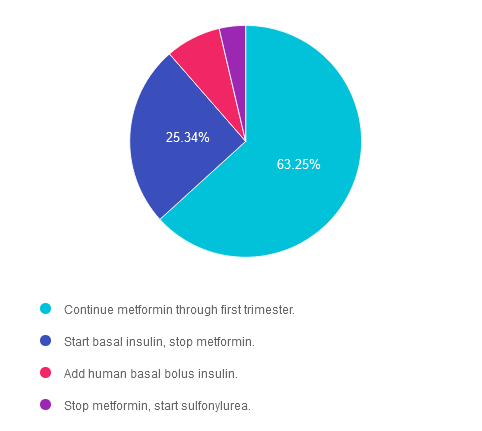
Getting to the Best Answer
Answer 1 is correct. 63.25% chose this answer. “Continue metformin through first trimester.” YES, this is the best answer. According to ADA Standard 15, “Metformin, when used to treat polycystic ovary syndrome and induce ovulation, should be discontinued by the end of the first trimester.” Standard 15 goes on to say, “Insulin is the preferred medication for treating hyperglycemia in GDM. Metformin and glyburide, individually or in combination, should not be used as first-line agents, as both cross the placenta to the fetus. Other oral and noninsulin injectable glucose-lowering medications lack long-term safety data.” Given that KR has a fasting glucose in the prediabetes range, basal insulin is not indicated at this time. KR needs referral to an RDN for nutrition therapy and ongoing evaluation of glucose levels.
Answer 2 is incorrect. 25.34% of you chose this very tempting answer. “Start basal insulin, stop metformin.” However, according to ADA Standard 15, “Metformin, when used to treat polycystic ovary syndrome and induce ovulation, should be discontinued by the end of the first trimester.” Given that KR has a fasting glucose in the prediabetes range, basal insulin is not indicated at this time. KR needs referral to an RDN for nutrition therapy and ongoing evaluation of glucose levels.
Answer 3 is incorrect. About 7.74% of respondents chose this. “Add human basal bolus insulin.” According to ADA Standard 15, “Metformin, when used to treat polycystic ovary syndrome and induce ovulation, should be discontinued by the end of the first trimester.” Given that KR has a fasting glucose in the prediabetes range, basal bolus insulin is not indicated at this time. KR needs referral to an RDN for nutrition therapy and ongoing evaluation of glucose levels.
Finally, Answer 4 is incorrect. 3.68% chose this answer. “Stop metformin, start sulfonylurea.” According to ADA Standard 15, “Metformin, when used to treat polycystic ovary syndrome and induce ovulation, should be discontinued by the end of the first trimester.” Standard 15 goes on to say, “Insulin is the preferred medication for treating hyperglycemia in GDM. Metformin and glyburide, individually or in combination, should not be used as first-line agents, as both cross the placenta to the fetus. Other oral and noninsulin injectable glucose-lowering medications lack long-term safety data.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on June 11th at 11:30 am PST for our
Pregnancy & Diabetes
Level 2 Standards of Care Intensive
Pregnancy with diabetes is confronted with a variety of issues that require special attention, education, & understanding. This course reviews those special needs while focusing on Gestational Diabetes & Pre-Existing Diabetes. Included are the most recent diagnostic criteria, management goals, & prevention of complications during pregnancy. This is a helpful review for Certification Exams & those who want more information on people who are pregnant & live with diabetes.
Objectives:
- List three issues that affect pregnancy with diabetes.
- Describe the unique attributes of pre-existing diabetes in pregnancy & gestational diabetes.
- State the diagnostic criteria & management goals for gestational diabetes.
- Potential short-term & long-term complications of fetal exposure to hypoglycemia.
- Prevention measures to keep mother & baby healthy.
Learning Outcome:
Participants will gain knowledge of special considerations, individualized goals, and standards for people experiencing diabetes during pregnancy to improve outcomes.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.6.7
- 9.6.8
- 10.3.1
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Are statins indicated for Peds with Diabetes?
For last week’s practice question, we quizzed participants on when to start statin therapy for pediatrics with diabetes. 50% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Based on the ADA Standards, in addition to dietary intervention, lifestyle and glucose management, when is it indicated to consider starting statin therapy for pediatrics with diabetes?
Answer Choices:
- When LDL is greater than 100 with a BMI of 25 or more.
- After age 10, if LDL is still greater than 130 at 6 months.
- Only if LDL and triglycerides are greater than 90thpercentile.
- Statins are only indicated for individuals 18 years and older.
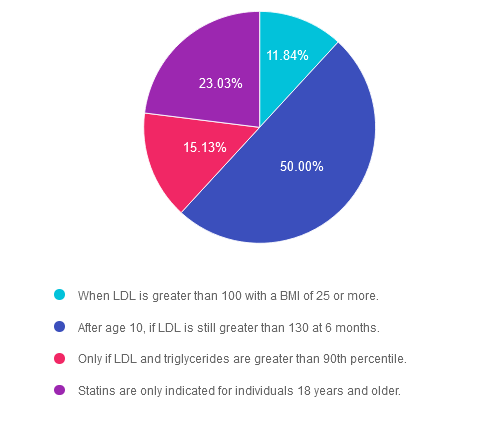
Getting to the Best Answer
Answer 1 is incorrect. 11.84% chose this answer. “When LDL is greater than 100 with a BMI of 25 or more.” This is a tempting answer. However, according to ADA Standards, if after 6 months of intensive lifestyle intervention, the LDL is still greater than 130mg/dL and the child is 10 years or older, statin therapy is indicated to prevent cardiovascular complications.
Answer 2 is correct. 50% of you chose this answer. “After the age of 10 if LDL is 130 or greater.” Great job, this is the BEST answer. According to ADA Standards, if after 6 months of intensive lifestyle intervention, the LDL is still greater than 130mg/dL and the child is 10 years or older, statin therapy is indicated to prevent cardiovascular complications.
Answer 3 is incorrect. About 15.13% of respondents chose this. “Only if LDL and triglycerides are greater than 90thpercentile.” According to ADA Standards, if after 6 months of intensive lifestyle intervention, the LDL is still greater than 130mg/dL and the child is 10 years or older, statin therapy is indicated to prevent cardiovascular complications.
Finally, Answer 4 is incorrect. 23.03% chose this answer. “Statins are only indicated for individuals 18 years and older.” According to ADA Standards, if after 6 months of intensive lifestyle intervention, the LDL is still greater than 130mg/dL and the child is 10 years or older, statin therapy is indicated to prevent cardiovascular complications.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on May 30th at 11:30 PST for our
From Tots to Teens
Level 2 Standards of Care Intensive
This course includes updated goals & guidelines for children living with type 1 or type 2 diabetes. This course discusses the special issues diabetes educators need to be aware of when working with children with diabetes & their families. We discuss the clinical presentation of diabetes, goals of care, & normal growth & development through the early years through adolescence. Strategies to prevent acute & long-term complications are included with an emphasis on positive coping for families & children with diabetes.
Objectives:
- Discuss the goals of care for Type 1 and Type 2 Kids with Diabetes.
- State Strategies to prevent acute and chronic complications.
- Discuss the importance of positive psychosocial adjustment & resources.
Learning Outcome:
Attendees will have comprehensive knowledge of special considerations, individualized goals and standards for children with diabetes to include in their practice.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.6.7
- 9.6.8
- 10.3.1
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working diabetes specialist and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Best treatment for Hypoglycemia with Gastroparesis
For last week’s practice question, we quizzed participants on how to treat hypoglycemia while dealing with gastroparesis. 73% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JR has type 1 diabetes and was recently diagnosed with gastroparesis. JR is a runner and has not been able to exercise recently due to nausea, vomiting, bloating, and intestinal pain. They experience hypoglycemia about 3 times a week.
Based on this information, what is the best treatment for hypoglycemia?
Answer Choices:
- Glucose tabs or gels.
- Skittles or gummies.
- High carb, low fiber snack bar.
- Peanut butter crackers.
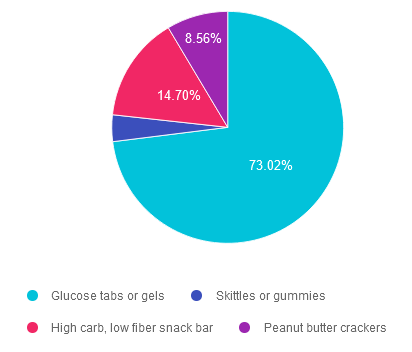
Getting to the Best Answer
Answer 1 is correct. 73.02% chose this answer. “Glucose tabs or gels.” Great job! Since JR has gastroparesis with slowed gastric emptying and delayed absorption of nutrients, we need to provide a fast acting carb that can instantly raise blood sugar. Fast absorption of sugar from glucose tabs and gels begins in the mouth, to quickly raise blood sugar levels.
Answer 2 is incorrect. 3.72% of you chose this answer. “Skittles or gummies.” Since JR has gastroparesis with slowed gastric emptying and delayed absorption of nutrients, we need to provide a fast acting carb that can instantly raise blood sugar. Gummies and skittles are more challenging to chew and need to be broken down in the stomach, which would delay the blood sugar from increasing to a safe level. Another consideration is that the ability to chew can be impaired when someone is experiencing significant hypoglycemia. Glucose tabs and gel, are quickly absorbed and require minimal chewing and are the best choice.
Answer 3 is incorrect. About 14.70% of respondents chose this. “High carb, low fiber snack bar.” Since JR has gastroparesis with slowed gastric emptying and delayed absorption of nutrients, we need to provide a fast acting carb that can instantly raise blood sugar. A snack bar, even though it is low fiber, is more challenging to chew and needs to be broken down in the stomach, which would delay the blood sugar from increasing to a safe level. Another consideration is that the ability to chew can be impaired when someone is experiencing significant hypoglycemia. Glucose tabs and gel, are quickly absorbed and require minimal chewing and are the best choice.
Finally, Answer 4 is incorrect. 8.56% chose this answer. “Peanut butter crackers.” Since JR has gastroparesis with slowed gastric emptying and delayed absorption of nutrients, we need to provide a fast acting carb that can instantly raise blood sugar. Peanut butter crackers are more challenging to chew and need to be broken down in the stomach, which would delay the blood sugar from increasing to a safe level. Another consideration is that peanut butter is a protein and fat combination food that would delay the absorption of the carbs from the crackers. Glucose tabs and gel, are quickly absorbed and would be the best choice!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity
Unlock insights for managing diabetes distress with the experts!
Join us live on June 17th & 24th, 2024 for our
ReVive 5 Diabetes Training Program:

The 2024 ADA Standards of Care now recommends annual screening for diabetes distress. If you are wondering how to screen for distress and tailor education based on the results, we encourage you to join this unique training program.
This two-session training provides the essential steps to address diabetes distress combined with an innovative approach to helping people make sense of their glucose data.
The first session is team-taught by experts in the field of diabetes distress and effective communication approaches. Dr. Larry Fisher kicks off the program by describing the difference between depression and distress and interpreting Diabetes Distress screening results. Dr. Susan Guzman uses a case study approach and step-by-step communication strategies to address responses from the Diabetes Distress screening tool. This session includes an abundance of evidence-based approaches that you can apply in your clinical setting.
Coach Beverly leads the second session. During this three-hour program, Beverly describes insulin dosing strategies, meter and sensor data interpretation, and common issues encountered by people using diabetes technology. Case studies include tools to help individuals discover what changes are needed to get glucose to target, coupled with the communication skills discussed in the first session. In conclusion, the team of instructors review a case study that pulls together all the ReVive 5 elements.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
Can’t join live? That’s okay. Your registration guarantees you access to the recorded version of the series, along with podcasts and resources for one full year.
Accredited Training Program:
- 15+ CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
Team of Experts:
ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Speakers Interviews – Learn more about the ReVive 5 Team
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- February 2026 eNews
- Rationale of the Week | Best Response for Facilitating Positive Health Behavior Change?
- Question of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- Rationale of the Week | What Does J.C.’s Family History & Lab Work Reveal?
- Red Flags for Low Digital Literacy in Diabetes Care
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.








