
Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Clinical Clues to Hypercortisolism
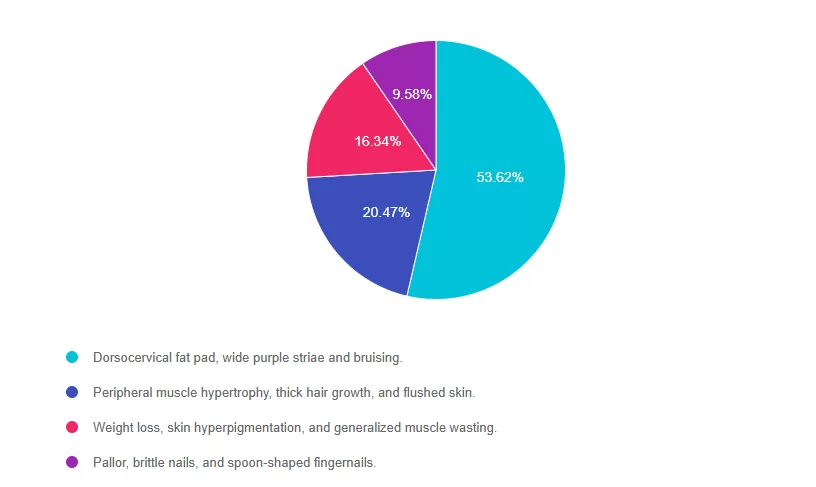
For last week’s practice question, we quizzed participants on clinical clues to hypercortisolism. 53% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

AJ is a 52-year-old with type 2 diabetes presents with worsening hyperglycemia despite taking three diabetes medications. AJ says, “No matter what I do, I can’t seem to get my blood sugars down”.
Which of the following clusters of physical findings would increase your suspicion that AJ is struggling with hypercortisolism?
- Dorsocervical fat pad, wide purple striae and bruising.
- Peripheral muscle hypertrophy, thick hair growth, and flushed skin.
- Weight loss, skin hyperpigmentation, and generalized muscle wasting.
- Pallor, brittle nails, and spoon-shaped fingernails.
Getting to the Best Answer
Answer 1 is correct. 53.62% chose this answer, “Dorsocervical fat pad, wide purple striae and bruising.” YES, GREAT JOB! These are classic physical features of hypercortisolism. Dorsocervical fat pad, wide purple striae and easy bruising along with proximal muscle weakness, and poor wound healing, should prompt evaluation for hypercortisolism in people with elevated glucose and hypertension, despite being on several medications for blood glucose and blood pressure.
Answer 2 is incorrect. 20.47% of you chose this answer, “Peripheral muscle hypertrophy, thick hair growth, and flushed skin.” These features are not characteristic of hypercortisolism; thick hair growth and muscle hypertrophy point to other conditions.
Answer 3 is incorrect. 16.34% of respondents chose this, “Weight loss, skin hyperpigmentation, and generalized muscle wasting.” These features are more consistent with Addison’s disease (adrenal insufficiency) or chronic illness, not hypercortisolism.
Finally, Answer 4 is incorrect.9.58% chose this answer, “Pallor, brittle nails, and spoon-shaped fingernails.” These findings are typically seen in iron-deficiency anemia, not hypercortisolism.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Diabetes Distraction in the Clinic
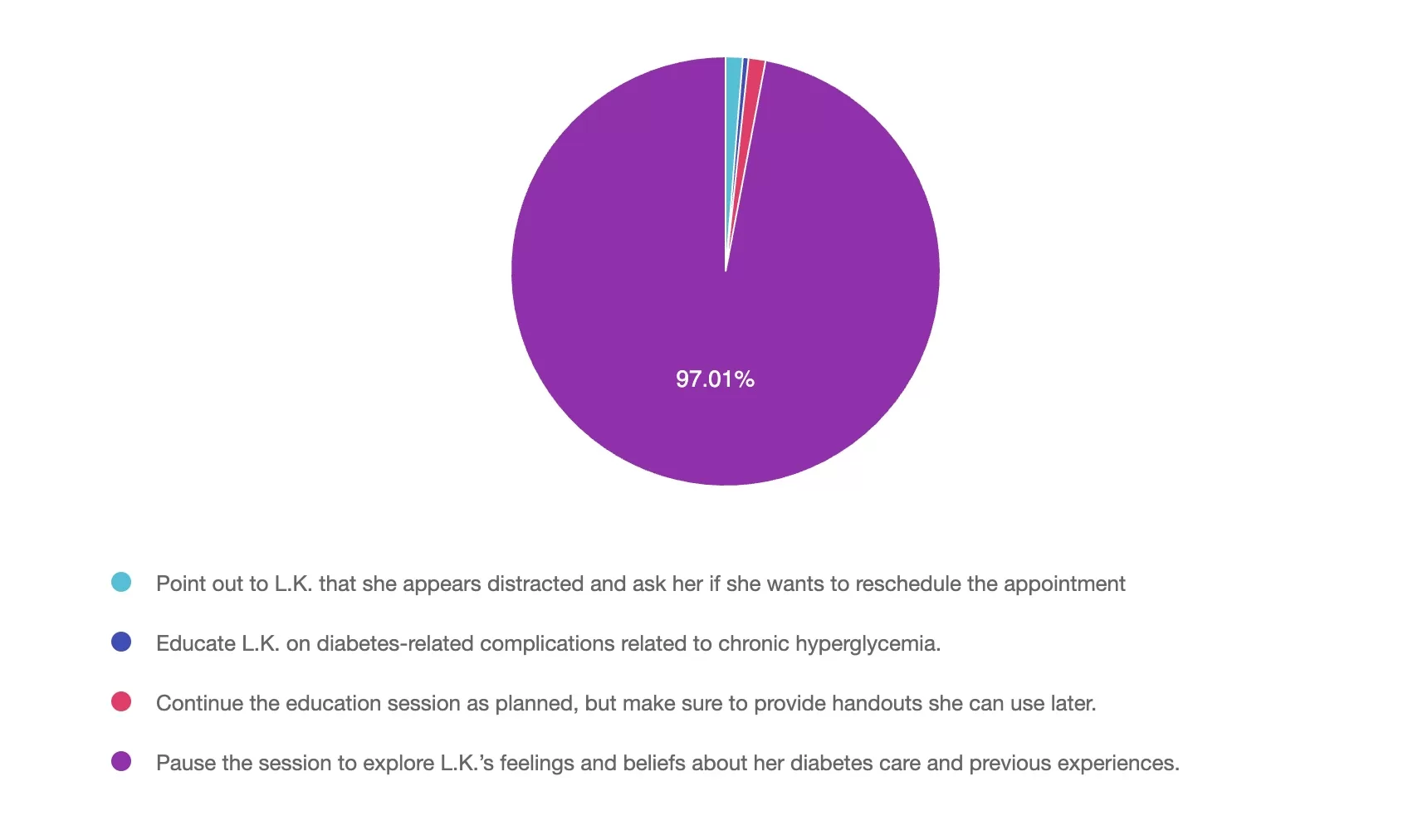
For last week’s practice question, we quizzed participants on Diabetes Distraction in the Clinic. 97% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

In the clinic today, you are seeing L.K., a 28-year-old with type 1 diabetes who was diagnosed at the age of 10. She was referred by the healthcare team for carb counting education and to discuss insulin pump options. During the session, L.K. appears preoccupied with her phone, avoids eye contact, and appears disinterested. When you ask what L.K.’s goals are for today’s session, she reports, “No matter how hard I try, no one is ever happy with my readings. Going on a pump isn’t going to change that”.
As a diabetes care and education specialist, what would you do?
- Point out to L.K. that she appears distracted and ask her if she wants to reschedule the appointment.
- Educate L.K. on diabetes-related complications related to chronic hyperglycemia.
- Continue the education session as planned, but make sure to provide handouts she can use later.
- Pause the session to explore L.K.’s feelings and beliefs about her diabetes care and previous experiences.
Getting to the Best Answer
Answer 1 is incorrect. 1% chose this answer, “Point out to L.K. that she appears distracted and ask her if she wants to reschedule the appointment.” L.K. verbalized her frustration with her diabetes and the healthcare system. As the diabetes healthcare provider, you are poised not only to provide information, but also to build a trusting relationship using person-centered approach. Stopping the session and rescheduling might derail collaboration and forward movement.
Answer 2 is incorrect. 1% of you chose this answer, “Educate L.K. on diabetes-related complications related to chronic hyperglycemia.” Although educating clients about the potential health outcomes of chronic hyperglycemia is essential, it does not constitute a person-centered approach in this situation. L.K. has made it clear that she is frustrated with her diabetes and healthcare experience.
Answer 3 is incorrect. About 1% of respondents chose this, “Continue the education session as planned, but make sure to provide handouts she can use later.” Continuing the education session with L.K. after she has verbalized her frustration is not a person-centered approach to care. She will not be engaged and an active participant in her care if she does not feel heard and validated.
Finally, Answer 4 is correct. 97% chose this answer, “Pause the session to explore L.K.’s feelings and beliefs about her diabetes care and previous experiences.” Every client has both positive and negative experiences in their diabetes journey that will influence their diabetes self-management and health outcomes. The statement she made in the diabetes education session must be addressed and discussed to build trust and understand her specific concerns. This approach is person-centered, leading to a shared decision-making approach to her personal diabetes goals.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Diabetes Type 3c: Misdiagnosis and Clarification
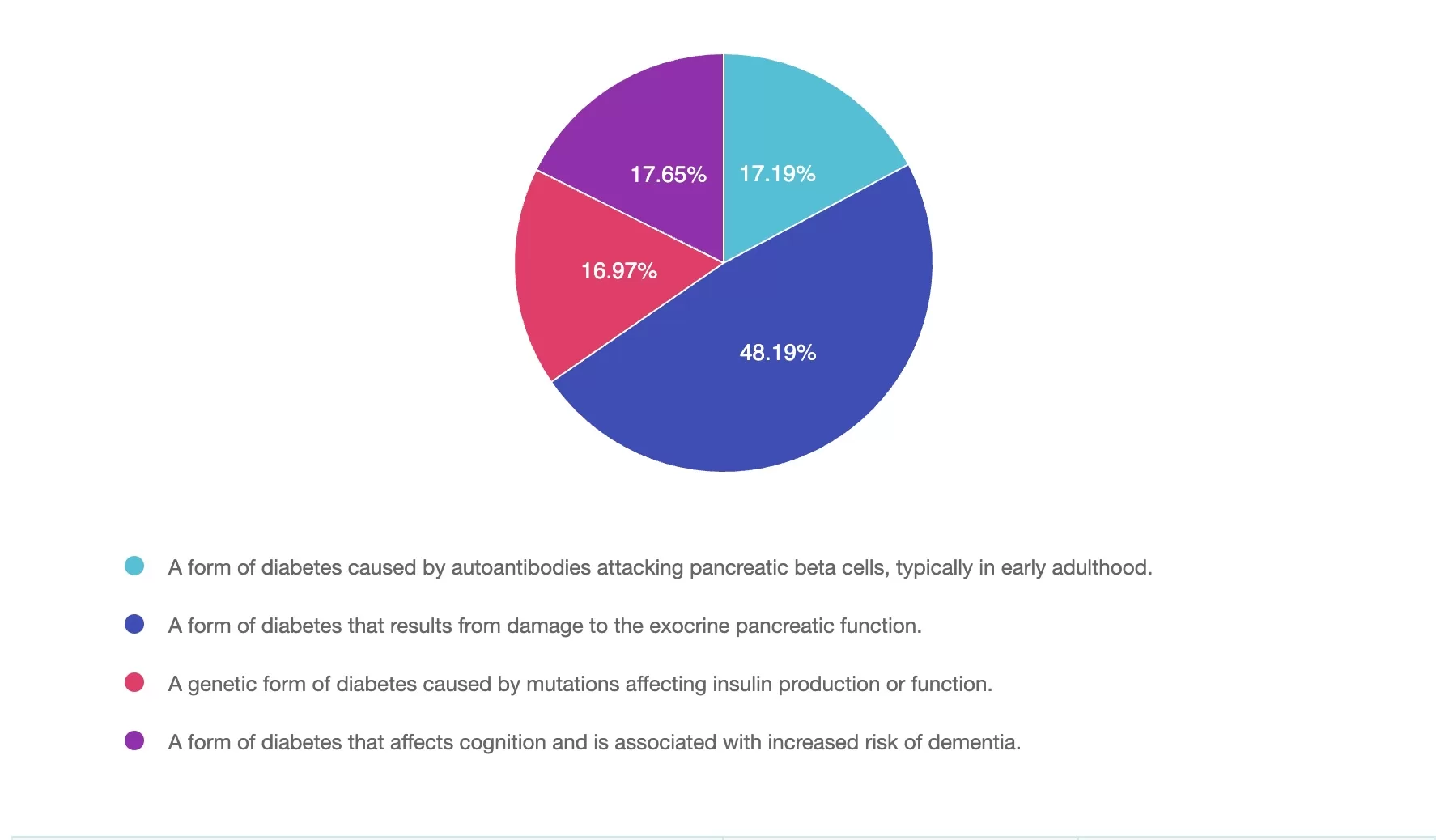
For last week’s practice question, we quizzed participants on Diabetes Type 3c: Misdiagnosis and Clarification 48% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Diabetes Type 3c is often misdiagnosed as type 2 diabetes. A colleague asks you to clarify what is meant by Diabetes Type 3c.
What is the most accurate response?
- A form of diabetes caused by autoantibodies attacking pancreatic beta cells, typically in early adulthood.
- A form of diabetes that results from damage to the exocrine pancreatic function.
- A genetic form of diabetes caused by mutations affecting insulin production or function.
- A form of diabetes that affects cognition and is associated with increased risk of dementia.
Getting to the Best Answer
Answer 1 is incorrect. 17.19% chose this answer, “A form of diabetes caused by autoantibodies attacking pancreatic beta cells, typically in early adulthood.” This answer describes the autoimmune Type 1 diabetes or LADA.
Answer 2 is correct. 48.19% of you chose this answer, “A form of diabetes that results from damage to the exocrine pancreatic function.” Great Job! This answer correctly describes Type 3c (pancreatogenic diabetes), which results from pancreatic exocrine dysfunction like pancreatitis, pancreatic surgery, or cystic fibrosis.
Answer 3 is incorrect. About 16.97% of respondents chose this, “A genetic form of diabetes caused by mutations affecting insulin production or function.” This description refers to monogenic diabetes, such as MODY.
Finally, Answer 4 is incorrect.17.65% chose this answer, “A form of diabetes that affects cognition and is associated with increased risk of dementia.” This describes type 3 diabetes, or cognitive impairment due to ongoing hyperglycemia.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Navigating Diabetes Care on the Road?
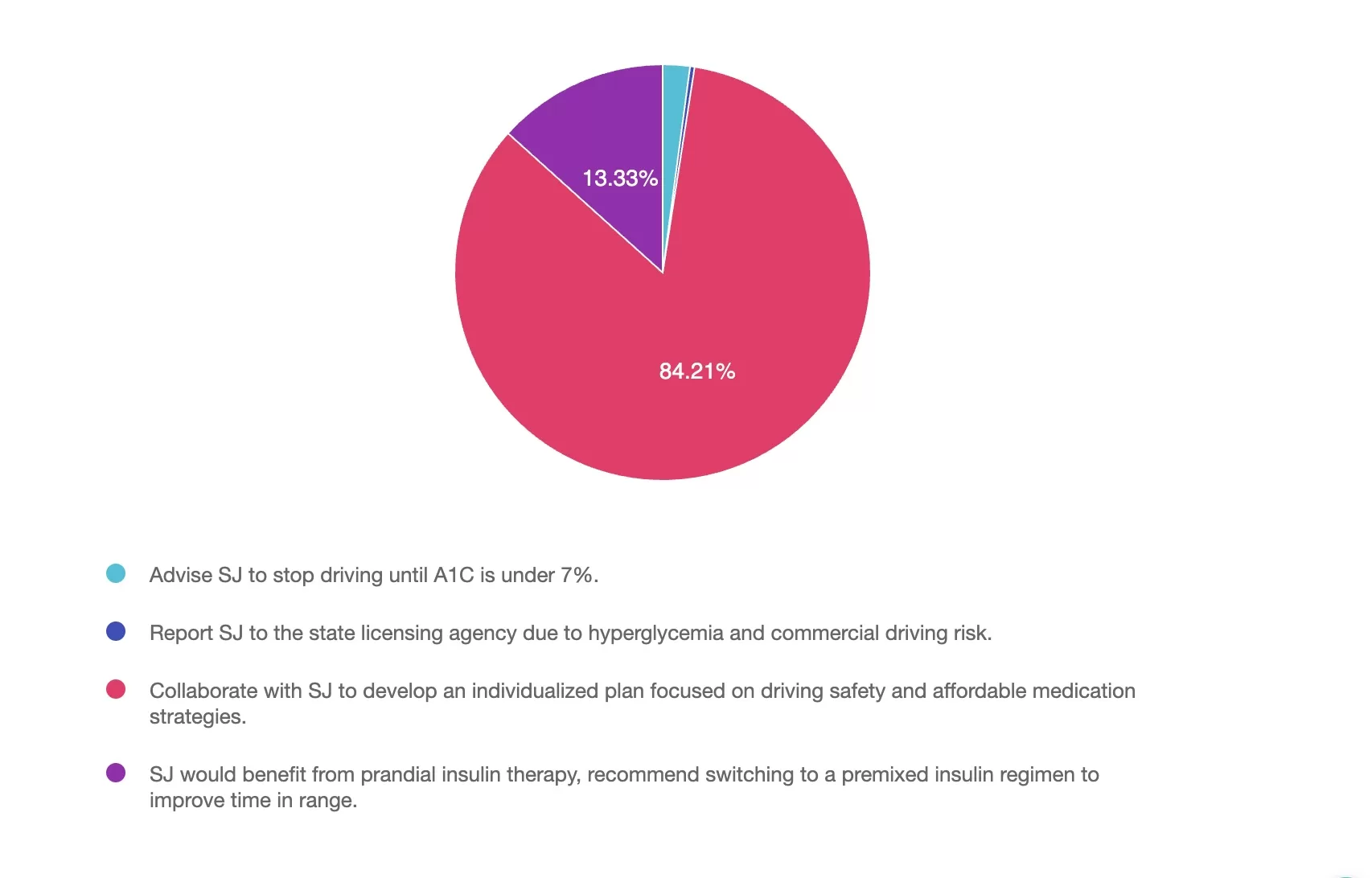
For last week’s practice question, we quizzed participants on Navigating Diabetes Care on the Road. 84% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

SJ is a 62-year-old long-haul truck driver with type 2 diabetes for the past 18 years. They take basal insulin nightly and metformin twice daily. Despite consistency of medications and a recent focus on lifestyle changes, Time in Range remains at 5% with a GMI of 9.2%. Last A1c was 9.7%. No history of hypoglycemia nor signs of retinopathy or neuropathy are documented. Incretin therapy or SGLT-2 inhibitor has been recommended but SJ shares that the insurance share of cost makes those medications unaffordable. SJ has an erratic schedule and drives across multiple states for work. They report fatigue during long drives but denies difficulty with driving nor any episodes of low blood glucose. SJ is motivated to improve diabetes management but is concerned about their livelihood if license were to be impacted.
As the diabetes care and education specialist, which of the following is the most appropriate next step in SJ’s care plan?
- Advise SJ to stop driving until A1C is under 7%.
- Report SJ to the state licensing agency due to hyperglycemia and commercial driving risk.
- Collaborate with SJ to develop an individualized plan focused on driving safety and affordable medication strategies.
- SJ would benefit from prandial insulin therapy, recommend switching to a premixed insulin regimen to improve time in range.
Getting to the Best Answer
Answer 1 is incorrect. 2% chose this answer, “Advise SJ to stop driving until A1C is under 7%.” Stopping driving based on an elevated A1C or Time in Range not at target is not recommended unless there is a clear safety risk. Hyperglycemia alone, without symptoms or complications, does not justify driving restrictions. Further assessment is needed before recommending driving cessation.¹
Answer 2 is incorrect. 1% of you chose this answer, “Report SJ to the state licensing agency due to hyperglycemia and commercial driving risk.” There is no legal or clinical basis to report SJ at this time. Reporting should occur if it is believed SJ poses a risk to public safety, such as recurrent severe hypoglycemia or functional impairments1 affecting driving ability.
Answer 3 is correct. About 84% of respondents chose this, “Collaborate with SJ to develop an individualized plan focused on driving safety and affordable medication strategies.” Individualized care should be emphasized, particularly in cases where cost limits access to newer therapies. We can explore medication cost saving resources, cost-effective oral agents, titration of basal insulin if not already optimized, or addition of prandial insulin support glycemia. SJ has been driving for many years, ensure driving safety strategies and ensure SJ knows the Federal Motor Carrier Safety Administration rules, which allow individuals with insulin-treated diabetes to drive commercially, as long as safety is maintained.²
Finally, Answer 4 is incorrect. 13% chose this answer, “SJ would benefit from prandial insulin therapy, recommend switching to a premixed insulin regimen to improve time in range.” Premixed insulin may not be the best option for someone like SJ with an unpredictable schedule. It increases the risk of hypoglycemia and limits flexibility. While it may help improve A1C, other options should be considered first, including more flexible insulin regimens or cost-conscious oral therapies.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Insulin Pump Inquiry for Rising A1C on MDI?
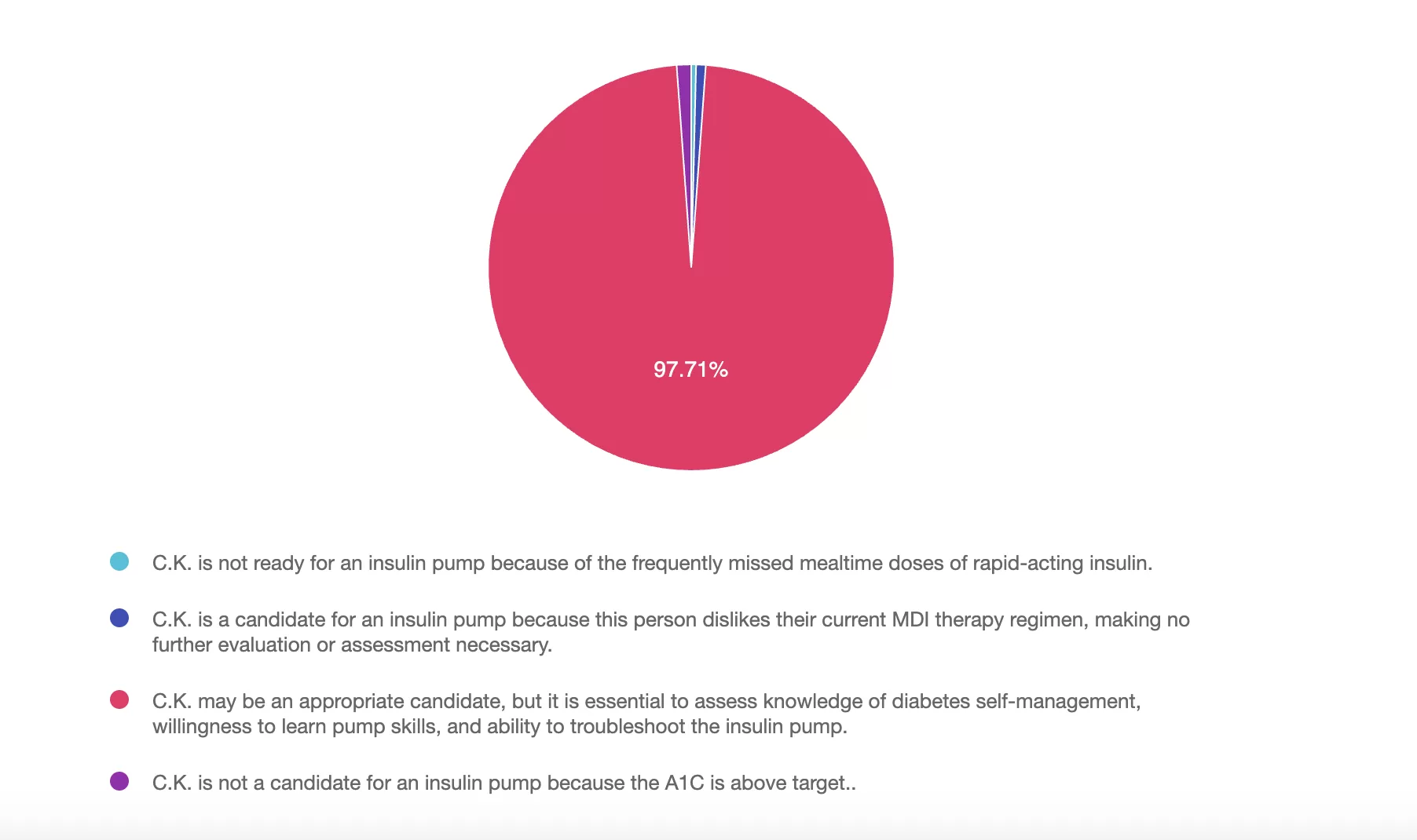
For last week’s practice question, we quizzed participants on Insulin Pump Inquiry for Rising A1C on MDI. 97% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

C.K. is a 55-year-old elementary school teacher diagnosed with type 1 diabetes ten years ago and is managing glycemic control with multiple daily injections (MDI) and a CGM. You are seeing C.K. for diabetes education due to an increasing hemoglobin A1c from 7.0% to 9.9%. During the appointment, C.K. reports missing mealtime doses due to being “too busy to get all that stuff out” at both work and home. C.K. notes that a friend from church has an insulin pump and asks if an insulin pump would help improve their A1c.
As the diabetes care and education specialist, what factors do you need to assess before determining if C.K. is ready for insulin pump therapy?
Answer Choices:
- C.K. is not ready for an insulin pump because of the frequently missed mealtime doses of rapid-acting insulin.
- C.K. is a candidate for an insulin pump because this person dislikes their current MDI therapy regimen, making no further evaluation or assessment necessary.
- C.K. may be a appropriate candidate, but it is essential to assess knowledge of diabetes self-management, willingness to learn pump skills, and ability to troubleshoot the insulin pump.
- C.K. is not a candidate for an insulin pump because the A1C is above target.
Getting to the Best Answer
Answer 1 is incorrect. 1% chose this answer, “C.K. is not ready for an insulin pump because of the frequently missed mealtime doses of rapid-acting insulin.” Missing insulin doses will not keep C.K. from starting an insulin pump. The use of an insulin pump can make it easier to bolus for meals, particularly with mobile bolusing features. By using an insulin pump, C.K. can bolus without stopping to get out all the supplies needed to give an injection, which may improve his success with bolus doses.
Answer 2 is incorrect. 1% of you chose this answer, “C.K. is a candidate for an insulin pump because this person dislikes their current MDI therapy regimen, making no further evaluation or assessment necessary.” The fact that C.K. dislikes the current MDI regimen is a conversation starting point to explore insulin pump therapy. When determining appropriateness for insulin pump therapy, the diabetes healthcare professional needs to evaluate for other factors, such as the physical and cognitive ability to operate and troubleshoot an insulin pump. More evaluation, including social determinants of health and CK’s goals and needs, are necessary to determine if pump therapy is right for C.K.
Answer 3 is correct. About 97% of respondents chose this, “C.K. may be a appropriate candidate, but it is essential to assess knowledge of diabetes self-management, willingness to learn pump skills, and ability to troubleshoot the insulin pump.” This client is frustrated with their regimen and their A1C is elevated. This could be a valid reason to start the discussion of insulin pump therapy for those using insulin therapy to manage diabetes. The diabetes healthcare professional needs to first evaluate and assess the clinical factors, lifestyle, and goals, of the individual to set them up for maximum success while reducing frustration in their diabetes self-management.
Finally, Answer 4 is incorrect. 1% chose this answer, “C.K. is not a candidate for an insulin pump because the A1C is above target.” An elevated A1C level is not a reason to dismiss insulin pump therapy. CK might actually benefit from using an insulin pump based on his goals and consideration of his social determinants of health.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
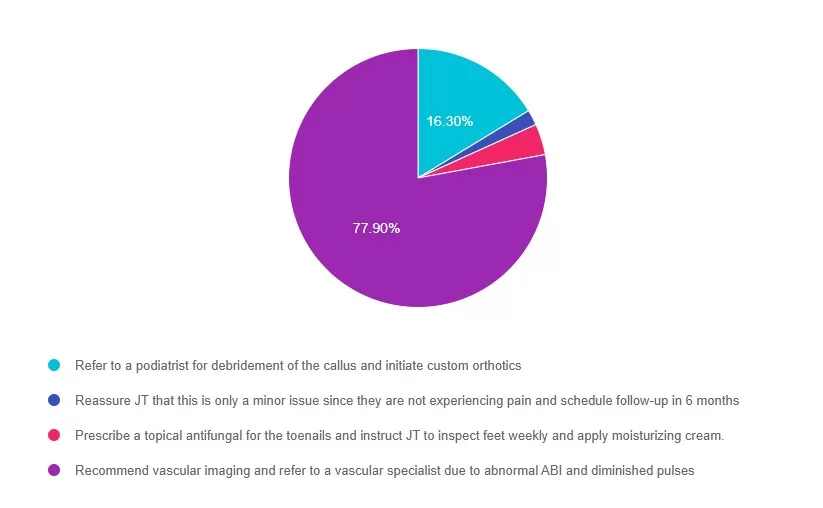
Rationale of the Week | Lower Extremity Recommendation for JT?
For last week’s practice question, we quizzed participants on Lower Extremity Recommendation for JT? . 77% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
JT is a 58-year-old with type 2 diabetes presents for a routine exam. Has a 20-year history of diabetes, hypertension, and peripheral neuropathy. Reports no foot pain, but partner notes they have been walking with a slight limp. On exam, you note dry skin, thickened toenails, a callus on the plantar aspect of the first metatarsal head, and diminished monofilament sensation at multiple sites on both feet. Pedal pulses are diminished bilaterally, and ABI (Ankle-Brachial Index) is 0.6 on the right and 0.7 on the left.
Which of the following is the most appropriate next step in managing this JT’s foot care?
Answer Choices:
- Refer to a podiatrist for debridement of the callus and initiate custom orthotics.
- Reassure JT that this is only a minor issue since they are not experiencing pain and schedule follow-up in 6 months.
- Prescribe a topical antifungal for the toenails and instruct JT to inspect feet weekly and apply moisturizing cream.
- Recommend vascular imaging and refer to a vascular specialist due to abnormal ABI and diminished pulses.
Getting to the Best Answer
Answer 1 is incorrect. 16% chose this answer, “Refer to a podiatrist for debridement of the callus and initiate custom orthotics.” While podiatry referral is important, vascular compromise must be evaluated first. Debridement in a patient with peripheral arterial disease (PAD) could lead to poor healing or ulceration.
Answer 2 is incorrect. 1% of you chose this answer, “Reassure JT that this is only a minor issue since they are not experiencing pain and schedule follow-up in 6 months.” Absence of pain does not exclude serious pathology, especially in individuals with neuropathy.
Answer 3 is incorrect. About 3% of respondents chose this, “Prescribe a topical antifungal for the toenails and instruct JT to inspect feet weekly and apply moisturizing cream.” This addresses a minor issue (onychomycosis), but ignores signs of ischemia and neuropathy.
Finally, Answer 4 is correct. 77% chose this answer, “Recommend vascular imaging and refer to a vascular specialist due to abnormal ABI and diminished pulses.” ABI values <0.9 indicate PAD; values <0.5 are considered severe. Given the ABI of 0.6 and 0.7, along with diminished pulses and gait change, vascular referral is necessary to assess perfusion and prevent future ulceration or amputation.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on August 12th @ 11:30am PST for Level 4 | 3 Steps to DeFeet Amputation

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. This course is free to attend without earning CEs, or you can choose the paid option if you wish to receive CE credits.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Recent Blog Bytes
- The Healing Shift: How a Chinese Restaurant Became My Refuge
- Question of the Week | TIR (Time of Range) of 89% – What Is Your Concern?
- Rationale of the Week | Which Feature Most Strongly Supports a Diagnosis of HHS Rather Than DKA?
- How Not Winning Motivated Me to Write A Book
- Question of the Week | What Not to Say to Overwhelmed Individual
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
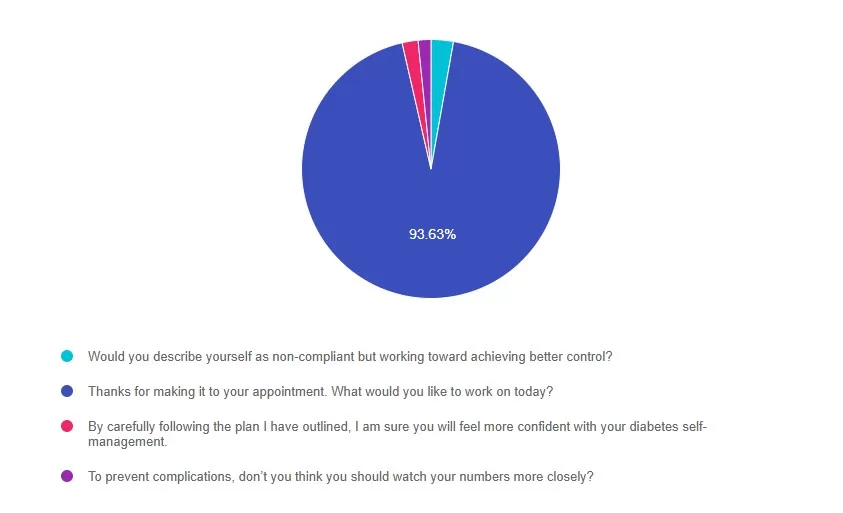
Rationale of the Week | Best example of Person-Centered Question?
For last week’s practice question, we quizzed participants on Best example of Person-Centered Question. 93% of respondents chose the best answer – GREAT JOB! We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: RJ is entering the field of diabetes care and education and has heard about the new language movement but isn’t sure how to apply it to their clinical practice. Which of the following is the best example of using person-centered language when speaking to someone with diabetes?
Answer Choices:
- Would you describe yourself as non-compliant, but working toward achieving better control?
- Thanks for making it to your appointment. What would you like to work on today?
- By carefully following the plan I have outlined, I am sure you will feel more confident with your diabetes self-management.
- To prevent complications, don’t you think you should watch your numbers more closely?
Getting to the Best Answer
Answer 1 is incorrect. 2% chose this answer, “Would you describe yourself as non-compliant but working toward achieving better control?” This response uses outdated judgmental terms like “non-compliant” and “control”.
Answer 2 is correct. 93% of you chose this answer, “Thanks for making it to your appointment. What would you like to work on today?” This uses respectful, person-first language and invites collaboration by focusing on the individual’s goals.
Answer 3 is incorrect. About 1% of respondents chose this, “By carefully following the plan I have outlined, I am sure you will feel more confident with your diabetes self-management.” This non-collaborative approach doesn’t include the individual in creating a plan.
Finally, Answer 4 is incorrect. 1% chose this answer, “To prevent complications, don’t you think you should watch your numbers more closely?” This uses a negative tone and the outdated “should” word. It can lead to shame or resistance.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
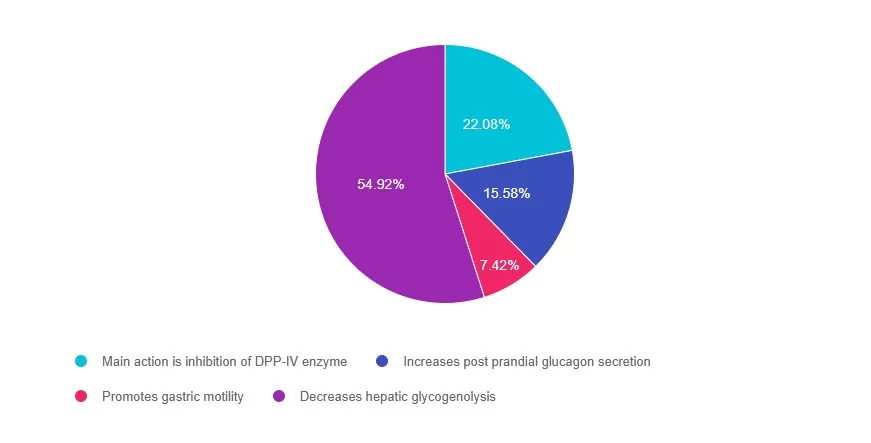
Rationale of the Week | What best describes the action of GLP-1 Receptor Agonists?
For last week’s practice question, we quizzed participants on What best describes the action of GLP-1 Receptor Agonists? 54% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which of the following is accurate statement regarding Glucagon Like Peptides (GLP-1)?
Answer Choices:
- Main action is inhibition of DPP-IV enzyme
- Increases post prandial glucagon secretion
- Promotes gastric motility
- Decreases hepatic glycogenolysis
Getting to the Best Answer
Answer 1 is incorrect. 22% chose this answer, “Main action is inhibition of DPP-IV enzyme.” The GLP-1’s do not inhibit the action of the DPP-IV enzyme (that is the DPP-IV inhibitor class). GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 2 is incorrect. 15% of you chose this answer, “Increases post prandial glucagon secretion.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon, slow gastric emptying and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 3 is incorrect. About 7% of respondents chose this, “Promotes gastric motility.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Finally, Answer 4 is correct. 54% chose this answer, “Decreases hepatic glycogenolysis.” YES – GREAT JOB! GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon which decreases hepatic glycogenolysis. They also slow gastric emptying, stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
For more information, download our Medication PocketCard for more information.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.






