Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Reluctant to Start Metformin due to Side Effects
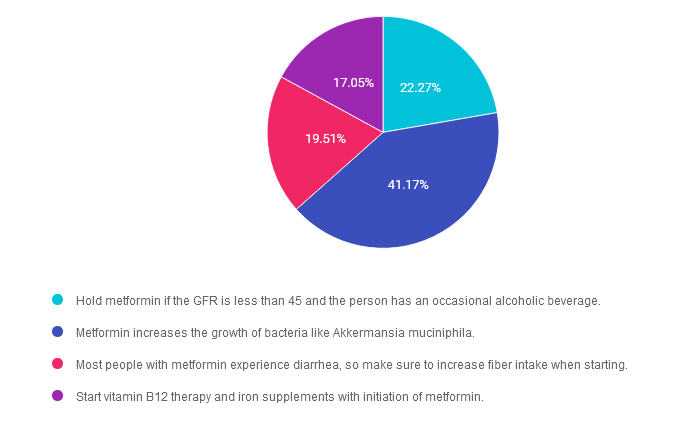
For last week’s practice question, we quizzed participants on a person’s concerns about metformin use & potential side effects. 41% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LS is reluctant to start on metformin because they heard it can cause diarrhea and kidney problems. You reassure LS that metformin doesn’t harm the kidneys and can actually improve gut health.
Based on the most recent evidence, which of the following is true?
Answer Choices:
- Hold metformin if the GFR is less than 45 and the person has an occasional alcoholic beverage.
- Metformin increases the growth of bacteria like Akkermansia muciniphila.
- Most people with metformin experience diarrhea, so make sure to increase fiber intake when starting.
- Start vitamin B12 therapy and iron supplements with initiation of metformin.
Getting to the Best Answer
Answer 1 is incorrect. 22.27% chose this answer. “Hold metformin if the GFR is less than 45 and the person has an occasional alcoholic beverage.” The guidelines state not to start metformin is the GFR is less than 45. But if someone is already on metformin their GFR drops below 45 we can continue it with caution and we might reduce the dose. We stop metformin if the GFR is less than 30. We don’t recommend metformin if someone is binge drinking due to the potential risk of lactic acidosis. An “occasional drink” would not reach the threshold to stop the metformin. Download Med PocketCards for more info.
Answer 2 is correct. 41.17% of you chose this answer. “Metformin increases the growth of bacteria like Akkermansia muciniphila.” Yes, this is the best answer. Metformin has been shown to increase gut bacterial diversity with a special nod to one of our favorite mucus protective bacteria known as “Akk”. This beneficial bacteria increase levels of butyrate and protects intestinal mucous lining, which helps to decrease inflammation. Cheers for AKK! Download Med PocketCards for more info.
Answer 3 is incorrect. About 19.51% of respondents chose this. “Most people with metformin experience diarrhea, so make sure to increase fiber intake when starting.” This is not accurate, since only a small percentage of people experience diarrhea. And, if they do, switching them to metformin extended release can decrease intestinal discomfort. Download Med PocketCards for more info.
Finally, Answer 4 is incorrect. 17.05% chose this answer. “Start vitamin B12 therapy and iron supplements with initiation of metformin.” Some, but not all individuals experience B12 deficiency on long term metformin therapy. We would only start B12 replacement therapy after confirming low B12 levels. Download Med PocketCards for more info.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Check out these upcoming class offerings!
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Diabetes Risk with Statin Use
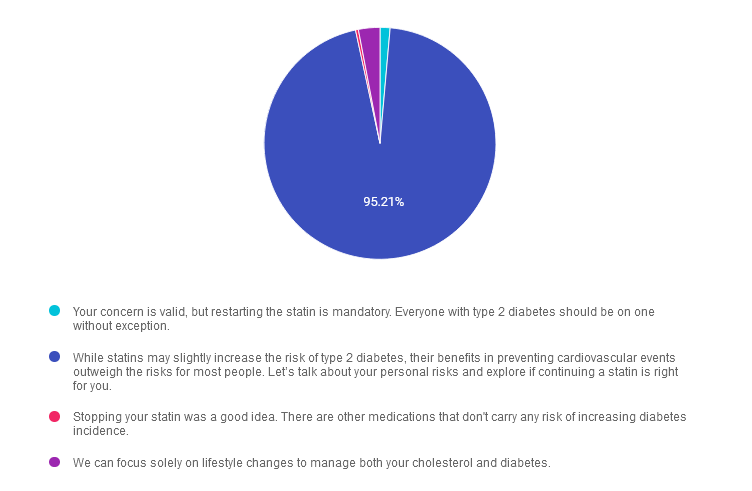
For last week’s practice question, we quizzed participants on concerns with diabetes risk and statin use. 95% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: LC is a 49-year-old living with type 2 diabetes and reports during their appointment they have stopped their statin because of concern over risk of type 2 diabetes incidence with statin use.
Using the ADA Standards of Care as a guide, what would be the best response to LC concerns?
Answer Choices:
- Your concern is valid, but restarting the statin is mandatory. Everyone with type 2 diabetes should be on one without exception.
- While statins may slightly increase the risk of type 2 diabetes, their benefits in preventing cardiovascular events outweigh the risks for most people. Let’s talk about your personal risks and explore if continuing a statin is right for you.
- Stopping your statin was a good idea. There are other medications that don’t carry any risk of increasing diabetes incidence.
- We can focus solely on lifestyle changes to manage both your cholesterol and diabetes.
Getting to the Best Answer
Answer 1 is incorrect. 1.40% chose this answer. “Your concern is valid, but restarting the statin is mandatory. Everyone with type 2 diabetes should be on one without exception.” Although statins are recommended for most people with diabetes, especially those over 40, the ADA emphasizes individualized care. There may be specific cases where statin use is not appropriate. Mandatory recommendations fail to consider individual preferences and circumstances, which are central to person-centered care.
Answer 2 is correct. 95.21% of you chose this answer. GREAT JOB! “While statins may slightly increase the risk of type 2 diabetes, their benefits in preventing cardiovascular events outweigh the risks for most people. Let’s talk about your personal risks and explore if continuing a statin is right for you.” This response acknowledges LC’s concern while addressing the evidence-based benefits of statin therapy for cardiovascular disease prevention. Statins are generally recommended for people with diabetes because cardiovascular protection outweighs the slight increase in diabetes incidence. This option promotes person-centered care by encouraging a collaborative approach.
Answer 3 is incorrect. About 0.40% of respondents chose this. Stopping your statin was a good idea. “There are other medications that don’t carry any risk of increasing diabetes incidence.” This response is misleading and may not be the best recommendation for LC. The ADA recommends considering the individual’s cardiovascular risk profile, not discontinuing statins simply because of concerns about diabetes incidence.
Finally, Answer 4 is incorrect. 2.99% chose this answer. “We can focus solely on lifestyle changes to manage both your cholesterol and diabetes.” Discontinuing statins without clinical justification could increase LC’s risk of cardiovascular events. The ADA recommends a combination of lifestyle changes and pharmacotherapy, when appropriate, for optimal outcomes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Live & On-Demand Viewing
FREE Webinars this November!!


Why Attend These Webinars?
- Accessible learning: All webinars are available online, so you can attend from the comfort of your home or office.
- Expert-led: Presentations are led by experienced diabetes educators, healthcare professionals, and researchers.
- Practical advice: Each session is designed to give you actionable strategies that can be applied in your daily life or practice.
- Up-to-date information: Stay informed about the latest research, guidelines, and technology in diabetes care.
How to Register?
Register above or simply visit DiabetesEd.net and browse the Free Resources Tab. While most webinars are available to attend at no cost, you have the option to purchase the session if you wish to earn Continuing Education (CE) credits.
For more information or any questions, please email [email protected].
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 7 times. She is a nationally recognized diabetes expert for over 25 years.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
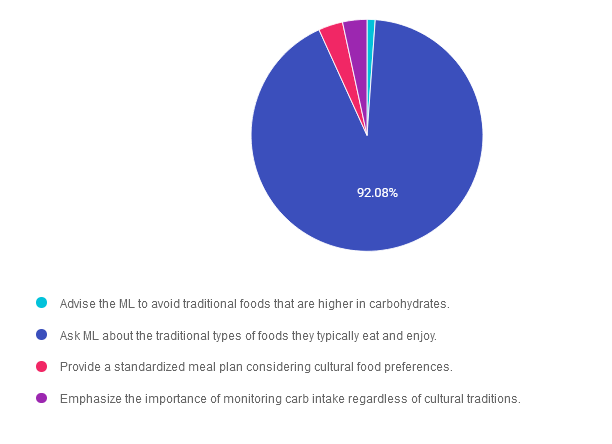
Rationale of the Week | Which Approach Considers Cultural Humility
For last week’s practice question, we quizzed participants on practicing cultural humility. 92% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: You are caring for ML, a Latinx person with newly diagnosed diabetes about lifestyle modifications. ML mentions that traditional family dinners are a central part of their daily routine.
How can the educator apply cultural humility in their approach to diabetes education to support ML’s dietary needs and preferences?
Answer Choices:
- Advise the ML to avoid traditional foods that are higher in carbohydrates.
- Ask ML about the traditional types of foods they typically eat and enjoy.
- Provide a standardized meal plan considering cultural food preferences.
- Emphasize the importance of monitoring carb intake regardless of cultural traditions.
Getting to the Best Answer
Answer 1 is incorrect. 1.13% chose this answer. “Advise the ML to avoid traditional foods that are higher in carbohydrates.” This answer was obviously incorrect to the majority of you, which highlights your knowledge of cultural humility and person-centered care. Even though it is important to monitor carbohydrates, we can’t disregard their cultural traditions. By considering the importance of cultural humility and person-centered care, we can help individuals determine a meal planning approach that works for them.
Answer 2 is correct. 92.08% of you chose this answer. “Ask ML about the traditional types of foods they typically eat and enjoy.” Yes, one of the main tenants of MNT is to “maintain the pleasure of eating.” This BEST answer highlights the importance of cultural humility and person-centered care. By considering the importance of cultural humility and person-centered care, we can help individuals determine a meal planning approach that works for them. Great job!
Answer 3 is incorrect. About 3.40% of respondents chose this. “Provide a standardized meal plan considering cultural food preferences.” One of the main tenants of MNT, is that there is NO one standardized meal plan. Our goal is to create an individualized meal plan in collaboration with the individual, based on their values, needs and preferences. By considering the importance of cultural humility and person-centered care, we can help them determine a meal planning approach that works for them.
Finally, Answer 4 is incorrect. 3.40% chose this answer. “Emphasize the importance of monitoring carb intake regardless of cultural traditions.” Our goal is to create an individualized meal plan in collaboration with the individual, based on their values, needs and preferences. Even though it is important to monitor carbohydrates, we can’t disregard their cultural traditions. By considering the importance of cultural humility and person-centered care, we can help individuals determine a meal planning approach that works for them.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
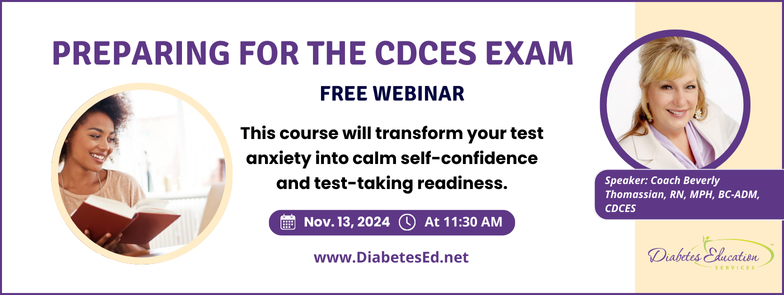
Join us live on November 13, 11:30 am PST for our
FREE Prep for CDCES Exam Webinar
Join us to get ready to succeed a the CDCES Exam. This course will transform your test anxiety into calm self-confidence and test taking readiness. Topics covered include:
- Changes in requirements for 2024
- Exam eligibility and the updated test format
- Strategies to succeed
- Review of study tips and test taking tactics.
We will review sample test questions, and the reasoning behind choosing the right answers.
After registering, you will receive a confirmation email containing information about joining the webinar.
Intended Audience: This FREE webinar is designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in achieving excellence in diabetes care and becoming Certified Diabetes Care and Education Specialists®.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 7 times. She is a nationally recognized diabetes expert for over 25 years.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Type 1 and Food Insecurity
For last week’s practice question, we quizzed participants on type 1 and food insecurity. About two thirds of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
AR is an 8 year old with type 1 diabetes who has a CGM but still uses insulin injections due to lack of insurance coverage. AR’s parents struggle with food insecurity and some days AR only has school provided breakfast and lunch. You notice he is experiencing level 1 hypoglycemia frequently around 6pm.
What is the best first intervention?
Answer Choices:
- Reassess the insulin dosing strategy.
- Double check that the family has a glucagon emergency kit.
- Reduce insulin dose and start a SGLT-2i to prevent hypoglycemia.
- Make sure AR is wearing identification that says they have type 1 diabetes.
Getting to the Best Answer
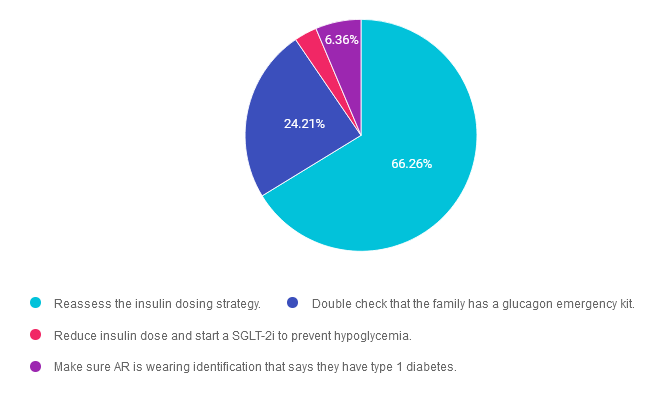
Answer 1 is correct. 66.26% chose this answer. “Reassess the insulin dosing strategy.” YES, this is the BEST answer. GREAT JOB! It appears that JR may not have adequate food intake on some days in the early evening hours. To compensate for this decreased food intake, the insulin dose will most likely need to be lowered to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
Answer 2 is incorrect. 24.21% of you chose this answer. “Double check that the family has a glucagon emergency kit.” Although it is important for all people living with type 1 diabetes to have a glucagon rescue medication, the first goal is to prevent severe hypoglycemia. In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
Answer 3 is incorrect. About 3.18% of respondents chose this. “Reduce insulin dose and start a SGLT-2i to prevent hypoglycemia.” In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. SGLT-2’s are off label for people living with type 1 diabetes and since AR is not in a stable situation, this would not be a good time to evaluate the effectiveness of adding on an SGLT. Of course, we would also need to connect AR and their family with social services and other resources.
Finally, Answer 4 is incorrect. 6.36% chose this answer. “Make sure AR is wearing identification that says they have type 1 diabetes.” Yes, wearing identification is recommended for people living with type 1 diabetes, but more importantly, we want to prevent hypoglycemia. In this situation, the first action is to adjust the insulin dose to prevent dinnertime hypoglycemia. Of course, we would also need to connect AR and their family with social services and other resources.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Join us live on November 13, 11:30 am PST for our
FREE Prep for CDCES Exam Webinar
Join us to get ready to succeed a the CDCES Exam. This course will transform your test anxiety into calm self-confidence and test taking readiness. Topics covered include:
- Changes in requirements for 2024
- Exam eligibility and the updated test format
- Strategies to succeed
- Review of study tips and test taking tactics.
We will review sample test questions, and the reasoning behind choosing the right answers.
After registering, you will receive a confirmation email containing information about joining the webinar.
Intended Audience: This FREE webinar is designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in achieving excellence in diabetes care and becoming Certified Diabetes Care and Education Specialists®.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 7 times. She is a nationally recognized diabetes expert for over 25 years.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | JR arrives late and out of sorts
For last week’s practice question, we quizzed participants on helping someone flustered and late to an appointment. 73% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: JR is a 22-year-old living with type 1 diabetes who arrives late for their appointment and seems out of sorts. When looking at the ambulatory glucose profile, you notice that time in range is less than 40% and coefficient of variation is also over 40%. You remember from a previous visit that JR had experienced almost half a dozen adverse childhood experiences and had elevated diabetes distress.
Based on this information, what is the next best step?
Answer Choices:
- Use the empowerment approach to help JR take charge of their life.
- Request that JR is referred to a mental health specialist.
- Utilize motivational interviewing techniques to help JR through this rough spot.
- Create a judgement free zone and explore with JR how they are feeling.
Getting to the Best Answer
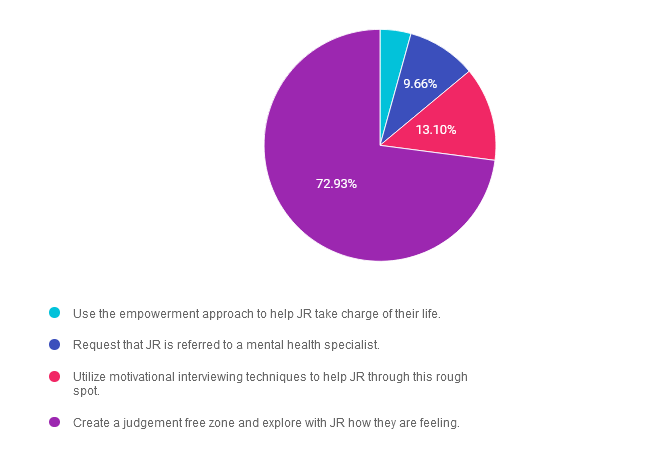
Answer 1 is incorrect. 4.31% chose this answer. “Use the empowerment approach to help JR take charge of their life.” Even though the empowerment approach can be used as a tool to help people take a more active role in their self-care, given JR’s level of distress, this would not be the best approach. We will need to first assess the situation and discuss next steps as part of collaborative care.
Answer 2 is incorrect. 9.66% of you chose this answer. “Request that JR is referred to a mental health specialist.” Even though JR is clearly struggling with diabetes distress and being “out of sorts’, this does not automatically mean he needs to be referred to a mental health specialist. We will need to first assess the situation and discuss next steps as part of collaborative care.
Answer 3 is incorrect. About 13.10% of respondents chose this. “Utilize motivational interviewing techniques to help JR through this rough spot.” Even though motivational interviewing can be used as a tool to help people take a more active role in their self-care, given JR’s level of distress, this would not be the best approach. We will need to first assess the situation and discuss next steps as part of collaborative care.
Finally, Answer 4 is correct. 72.93% chose this answer. “Create a judgement free zone and explore with JR how they are feeling.” YES, GREAT JOB. We need to provide a safe environment for JR to have the freedom to share what is happening in their life and support them in taking action to decrease their distress.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
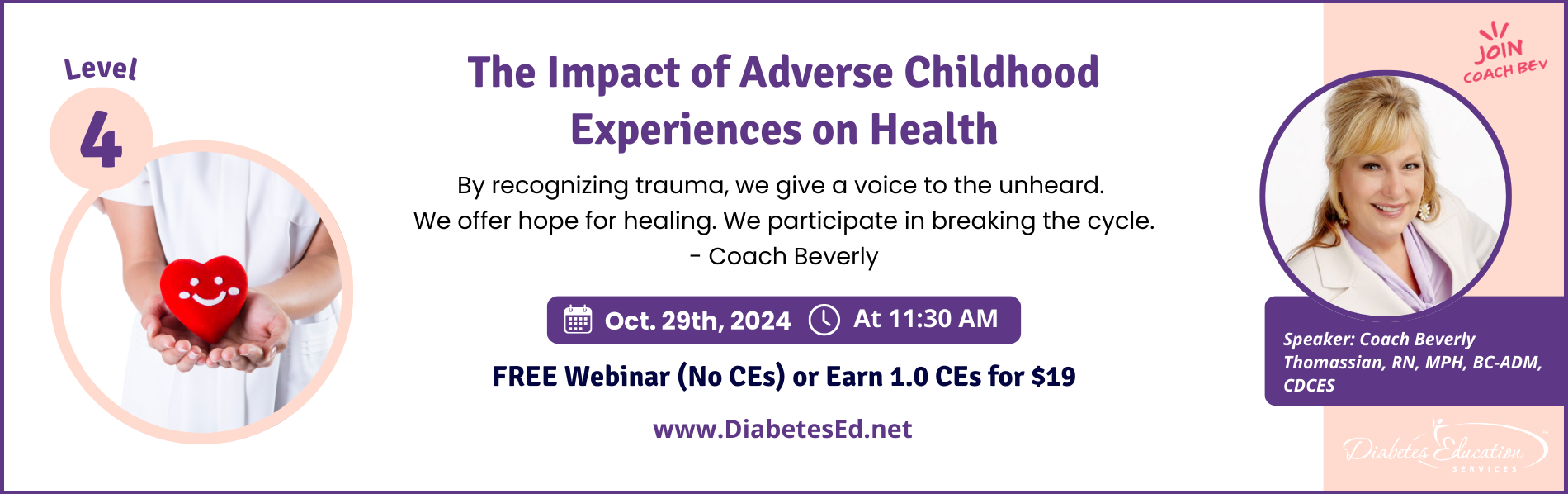
Join us live on October 29, 2024 for our
The Impact of Adverse Childhood Experiences on Health
Level 4 | Advanced & Specialty Topic Courses
Adverse childhood experiences (ACE) are associated with an increased risk of diabetes, heart disease, cancer & a variety of other health consequences for adults. This session reviews how diabetes care & education specialists can provide screening, assessment, & trauma-informed care to individuals who experienced ACEs & are living with toxic stress. We will explore strategies to address ACES & improve outcomes for individuals & communities. Throughout, we will focus on supporting self-care with a focus on recognizing & promoting resilience.
Objectives:
- Discuss the benefits of assessing Adverse Childhood Experiences (ACE) in individuals with diabetes.
- State the relationship between ACE Scores & the risk of future health complications.
- Describe a person-centered approach to fostering resilience & self-care for individuals with toxic stress.
- Identify two strategies to provide trauma-informed care in your work setting.
Learning Outcome:
Participants will identify how trauma can impact diabetes and self-management along with strategies to support hope when working with people with diabetes.
Target Audience:
This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs/RDNs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions. The practice areas for RDs/RDNs for CDR reporting are healthcare, preventative care, wellness, and, lifestyle along with, education and research.
CDR Performance Indicators:
- 9.2.1
- 9.2.3
- 9.4.3
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 15 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert.
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | The Impact of Adverse Childhood Experiences on Health awards 1.0 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | JR and Donut Fridays – What is the wise approach?
For last week’s practice question, we quizzed participants on helping people address special treat days. The majority of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
You are reviewing JR’s ambulatory glucose profile and it is over 70% time in range. JR usually takes bolus insulin before each meal and basal insulin at night. However, you notice that once a week on Fridays, JR’s blood glucose levels are above target between 2-5pm. When you bring this Friday glucose elevation to JR’s attention, they tell you it’s because the boss always brings in donuts after lunch on Fridays to celebrate everyone’s hard work. JR asks you about strategies to address this time above target.
What is the wise approach?
Answer Choices:
- Have you considered eating a piece of fruit instead?
- Can you let your boss know that you appreciate the gesture, but your diabetes doesn’t allow for this treat.
- Would you consider giving a little extra bolus insulin and enjoying the donut?
- Would you be willing to bring in a special low carb treat for everyone to enjoy?
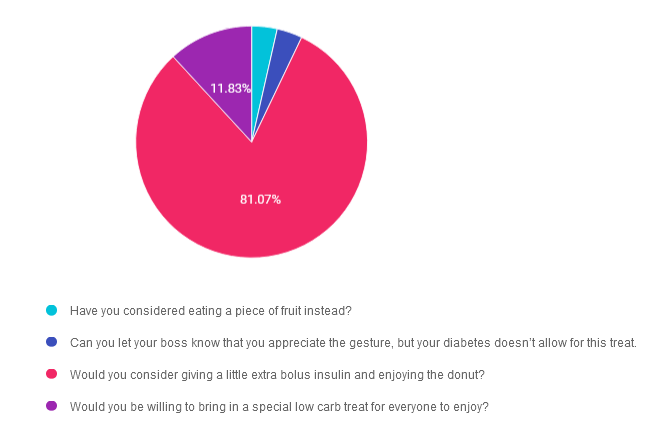
Getting to the Best Answer
Answer 1 is incorrect. 3.55% chose this answer. “Have you considered eating a piece of fruit instead?” Even though fruit might be a healthier choice, it may not be the “wise” choice for this situation. The ADA Standards encourage us to help individuals “maintain the pleasure of eating.” An occasional donut to celebrate hard work can certainly be included in JR’s meal plan.
Answer 2 is incorrect. 3.55% of you chose this answer. “Can you let your boss know that you appreciate the gesture, but your diabetes doesn’t allow for this treat.” JR can choose to make a “wise” decision and participate in the festivities. The ADA Standards encourage us to help individuals “maintain the pleasure of eating.” An occasional donut to celebrate hard work can certainly be included in JR’s meal plan.
Answer 3 is correct. About 81.07% of respondents chose this. “Would you consider giving a little extra bolus insulin and enjoying the donut?” JR can choose to make a “wise” decision and participate in the festivities and take a little extra insulin to prevent post treat hyperglycemia. The ADA Standards encourage us to help individuals “maintain the pleasure of eating.” An occasional donut to celebrate hard work can certainly be included in JR’s meal plan.
Finally, Answer 4 is incorrect. 11.83% chose this answer. “Would you be willing to bring in a special low carb treat for everyone to enjoy?” JR can choose to make a “wise” decision and participate in the festivities. The ADA Standards encourage us to help individuals “maintain the pleasure of eating.” An occasional donut to celebrate hard work can certainly be included in JR’s meal plan.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Invite Coach Beverly Thomassian to Speak – In Person or Virtually!
An Innovative Approach to Diabetes Education
With over two decades as a thought leader in diabetes care and education, Beverly is an inspiring and informational presenter. She can delve deep into the science of diabetes while incorporating real-life applications coupled with a compassionate approach that resonates with healthcare professionals.
Beverly is a relentless advocate for non-judgmental and inclusive diabetes care and believes that we are at our best when we are curious, kind, and engaging.
As a nurse entrepreneur and professional speaker, Beverly champions person-centered and evidence-based diabetes care through her live courses, keynote speeches, and webinar presentations.
Coach Beverly makes it a priority to make time to teach at conferences and organizations across the country. In addition to providing the latest research-based information, she incorporates story telling, games, movement breaks and small group activities.
She believes people learn best when the content is meaningful and fun!
Participants leave feeling energized, inspired, and excited about providing best diabetes care.
See more info here >>
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve of continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.
Rationale of the Week | Screening for Celiac Disease
For last week’s practice question, we quizzed participants on screening for celiac disease. Almost half of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: TC is a 15-year-old who was diagnosed with type 1 diabetes just over a year ago. Following their diagnosis, they quickly transitioned to sensor-augmented pump therapy and are not currently taking any other medications. Recent lab results show normal lipid and renal profiles, a hemoglobin A1c of 7.5%, and a fasting glucose level of 148 mg/dL. Despite following a nutrient-rich diet, TC reports experiencing fatigue, difficulty gaining weight, frequent nausea, and diarrhea.
What Standard of Care recommendation may help explain TC’s reported symptoms?
Answer Choices:
- TC’s Hemoglobin A1c is above target. Elevated glucose values could be contributing to fatigue and difficulty with weight gain.
- Ensure IgA tissue transglutaminase (tTG) antibodies, with documentation of normal total serum IgA levels have been checked.
- Recommend a gluten-free diet since individuals with type 1 diabetes can be at higher risk of celiac disease.
- Consider referral for a gastric emptying study given complaint of frequent nausea and diarrhea.
Getting to the Best Answer
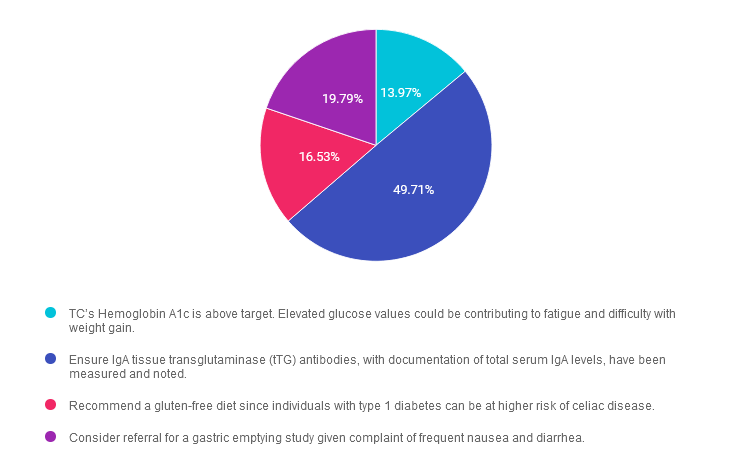
Answer 1 is incorrect. 13.97% chose this answer. “TC’s Hemoglobin A1c is above target. Elevated glucose values could be contributing to fatigue and difficulty with weight gain.” 1. Answer 1 is incorrect, as it is not the best answer. Although the ADA Standards of Care state an A1C of <7% is appropriate for many children and adolescents, we must provide additional assessment for TC’s case. Keep reading below.
Answer 2 is correct. 49.71% of you chose this answer. “Ensure IgA tissue transglutaminase (tTG) antibodies, with documentation of normal total serum IgA levels have been checked.” 2. Answer 2 is correct. Screening for celiac disease is recommended in individuals with type 1 diabetes soon after diagnosis or when symptoms occur, such as those reported by TC. It is recommended that IgA tissue transglutaminase (tTG) antibodies be checked, with documentation of normal total serum IgA levels, or IgG tTG and deamidated gliadin antibodies if IgA is deficient.
Answer 3 is incorrect. About 16.53% of respondents chose this. “Recommend a gluten-free diet since individuals with type 1 diabetes can be at higher risk of celiac disease.” 3. Although a gluten-free diet is recommended if TC is diagnosed with celiac disease, it is essential to complete appropriate screening before implementation of a gluten-free diet.
Finally, Answer 4 is incorrect. 19.79% chose this answer. “Consider referral for a gastric emptying study given complaint of frequent nausea and diarrhea.” 4. Although we can see an increased risk of gastroparesis in diabetes, determined by a gastric emptying study, gastroparesis typically develops as a long-term complication of diabetes. Initial recommendations would be to rule out other causes and ensure recommended screening and treatment.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
FREE Webinar:
The Impact of Adverse Childhood Experiences on Health
Join us October 29th, 2024 at 11:30 am
Adverse childhood experiences (ACE) are associated with an increased risk of diabetes, heart disease, cancer & a variety of other health consequences for adults. This session reviews how diabetes care & education specialists can provide screening, assessment, & trauma-informed care to individuals who experienced ACEs & are living with toxic stress. We will explore strategies to address ACES & improve outcomes for individuals & communities. Throughout, we will focus on supporting self-care with a focus on recognizing & promoting resilience.
Topics include:
- Discuss the benefits of assessing Adverse Childhood Experiences (ACE) in individuals with diabetes.
- State the relationship between ACE Scores & the risk of future health complications.
- Describe a person-centered approach to fostering resilience & self-care for individuals with toxic stress.
- Identify two strategies to provide trauma-informed care in your work setting.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants and other health care providers interested in enhancing their knowledge of management of inpatient hyperglycemia.
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator and a nationally recognized diabetes expert.
Two registration options:
- Enroll for FREE (No CEs): Click here to enroll.
- Earn 0.5 CEs – Fee: $19.00 – Click here to enroll in the course.
Enroll in our entire Level 4 | Advanced & Specialty Topic Courses
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | KR is Overwhelmed with Insulin Regimen
For last week’s practice question, we quizzed participants on feeling overwhelmed with insulin regimen. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: KR is a 49-year-old with a learning disability and diabetes for over 20 years and is taking the following classes of diabetes medications at maximum doses; SGLT-2, Sulfonylurea, GLP-1 RA, biguanide and a TZD. Over the past month, KR’s blood glucose levels have increased to over 300 despite a 20-pound weight loss. The endocrinologist starts KR on basal insulin plus bolus insulin at each meal based on blood glucose and carbohydrates consumed. KR arrives for their education appointment in tears, saying “I feel completely overwhelmed and confused about all this insulin stuff.”
What is the best response?
Answer Choices:
- This must seem overwhelming, but I believe that you can do this.
- Let’s review carb counting again, so you feel more confident about calculating your dose.
- Many people starting on insulin feel overwhelmed, but with time it gets easier.
- Let’s start the basal insulin first, then we can tackle the meal bolus when you are ready.
Getting to the Best Answer
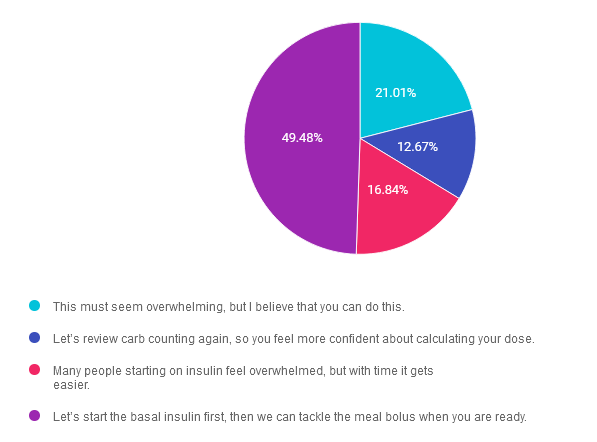
Answer 1 is incorrect. 21.01% chose this answer. “This must seem overwhelming, but I believe that you can do this.” Even though this response affirms KR’s ability to count carbs and adjust insulin coverage, it is not a realistic expectation. Given KR’s learning disability and his feelings of being overwhelmed, this complicated insulin management strategy is not the best approach for KR. We need to keep the insulin plan simple, until KR is ready to move forward.
Answer 2 is incorrect. 12.67% of you chose this answer. “Let’s review carb counting again, so you feel more confident about calculating your dose.” While this is a compassionate response, it does not take into account the complexity of the overall insulin management strategy and KR’s feelings of being overwhelmed. We need to keep the insulin plan simple, until KR is ready to move forward.
Answer 3 is incorrect. About 16.84% of respondents chose this. “Many people starting on insulin feel overwhelmed, but with time it gets easier.” This is a compassionate response that doesn’t address the main issue. The insulin plan is not realistic for this individual with a learning disability. We need to keep the insulin plan simple, until KR is ready to move forward.
Finally, Answer 4 is correct. 49.48% chose this answer. “Let’s start the basal insulin first, then we can tackle the meal bolus when you are ready.” YES, this is the best answer and most of you chose this. GREAT JOB. We need to keep the insulin plan simple, until KR is ready to move forward. Start with basal insulin first, until KR seems ready to add on bolus insulin at meals.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
There is still time to join us Live in Beautiful San Diego for our
Annual DiabetesEd Training Conference
October 9th-11th, 2024

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego on October 9-11, 2024.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Each day, we provide a healthy breakfast, including fresh coffee, to kick off your morning. Our instructors co-teach the content to keep things fresh and lively. Plus, we play DiaBingo to reinforce key content and give away prizes. In addition, we provide plenty of movement breaks led by volunteers from the audience. Did we mention delicious lunches and a conference meeting space just minutes from San Diego Bay?
Friend Discount: 3 or more only $559-$799 (based on registration package) per person. Email us at [email protected] with the name and email of each registrant to get the discount!
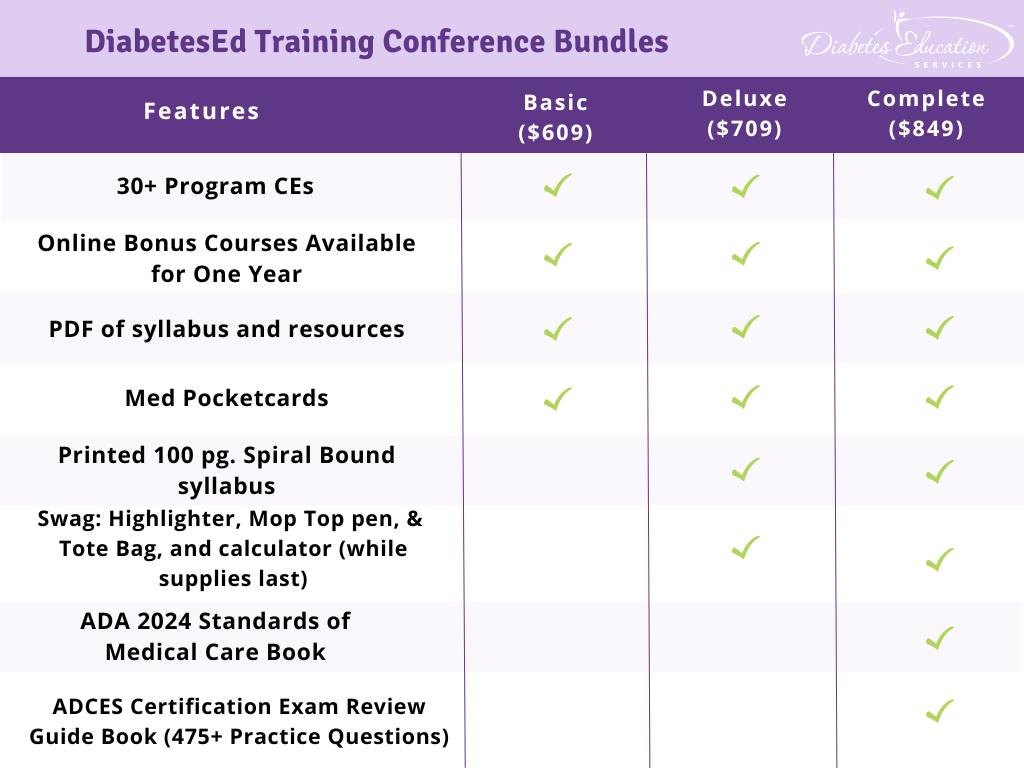
Time: The course is Wednesday through Friday. Join us for breakfast at 7:00 a.m. each day. The class begins at 8:00 a.m. and ends at 5:00 p.m. on Wednesday and Thursday and at 3:00 p.m. on Friday.
- 3 Days: of critical information delivered by passionate speakers in an engaging and fun format!
- 18+ CEs: earned at the Live Seminar (RDs earn 18.75 CEs while Nurses & CA Pharmacists earn 22.75 CEs)
- 10 Bonus Online Courses, Earn 10+ CEs: As a course attendee, you automatically receive a bonus online course bundle of 13 online courses valued at over $179. Coach Beverly carefully chose each of these courses based on student feedback on which content best helped them succeed at the certification exams and in their clinical practice. You will be given instructions after you purchase the course on how to enroll in our Online University and get started!
- Healthy breakfast all days, gourmet lunch both days and refreshments.
- E-version of the syllabus
Sign up for Diabetes Blog Bytes – we post weekly Blog Bytes that are informative and FREE! Every week we post one exam practice Question of the Week and Rationale of the Week. Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.