Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | Clinical Clues to Hypercortisolism
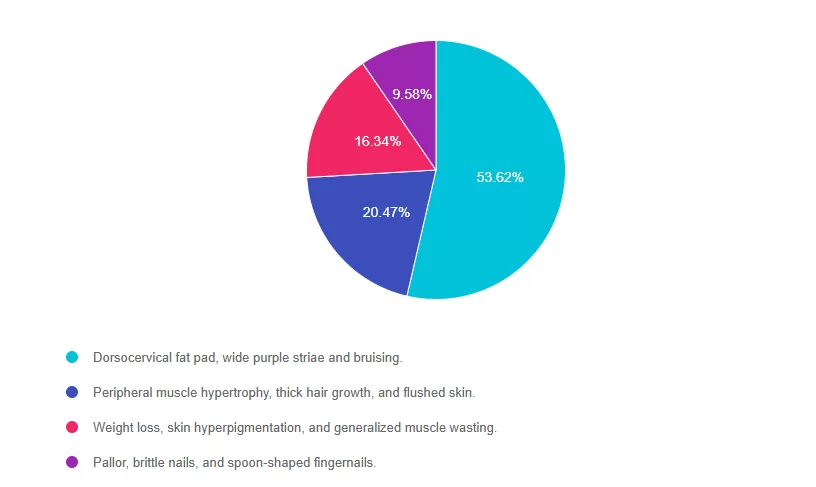
For last week’s practice question, we quizzed participants on clinical clues to hypercortisolism. 53% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

AJ is a 52-year-old with type 2 diabetes presents with worsening hyperglycemia despite taking three diabetes medications. AJ says, “No matter what I do, I can’t seem to get my blood sugars down”.
Which of the following clusters of physical findings would increase your suspicion that AJ is struggling with hypercortisolism?
- Dorsocervical fat pad, wide purple striae and bruising.
- Peripheral muscle hypertrophy, thick hair growth, and flushed skin.
- Weight loss, skin hyperpigmentation, and generalized muscle wasting.
- Pallor, brittle nails, and spoon-shaped fingernails.
Getting to the Best Answer
Answer 1 is correct. 53.62% chose this answer, “Dorsocervical fat pad, wide purple striae and bruising.” YES, GREAT JOB! These are classic physical features of hypercortisolism. Dorsocervical fat pad, wide purple striae and easy bruising along with proximal muscle weakness, and poor wound healing, should prompt evaluation for hypercortisolism in people with elevated glucose and hypertension, despite being on several medications for blood glucose and blood pressure.
Answer 2 is incorrect. 20.47% of you chose this answer, “Peripheral muscle hypertrophy, thick hair growth, and flushed skin.” These features are not characteristic of hypercortisolism; thick hair growth and muscle hypertrophy point to other conditions.
Answer 3 is incorrect. 16.34% of respondents chose this, “Weight loss, skin hyperpigmentation, and generalized muscle wasting.” These features are more consistent with Addison’s disease (adrenal insufficiency) or chronic illness, not hypercortisolism.
Finally, Answer 4 is incorrect.9.58% chose this answer, “Pallor, brittle nails, and spoon-shaped fingernails.” These findings are typically seen in iron-deficiency anemia, not hypercortisolism.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
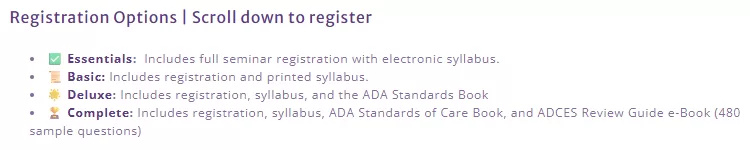
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
We Had a Sizzling Time at ADCES in Phoenix
We had a sizzling time at the ADCES National Diabetes Meeting—connecting with new colleagues and joyfully reuniting with old friends. I wore a special white suit inherited from my husband’s lovely aunt, Serpouhi, who passed away just before her 60th birthday. With every step I took in one of her treasured outfits, I felt her cheering me on.
This was my first time attending ADCES as an exhibitor in the big hall, and we went all out! Our booth sparkled with glittery pancreases, shimmering purple accents, and vibrant energy. One of the highlights was our “I DID IT!” banner, where proud course graduates stopped by to sign their name in bold felt-tip marker—celebrating their CDCES or BC-ADM success using our study materials. I was bursting with pride as the banner filled with names, each one representing countless hours of dedication and perseverance. Even the incredible Diana Isaacs made sure to add her name to this tapestry of achievement!
What truly filled my heart was the stream of hundreds of educators who came by to express their gratitude—offering hugs, sharing success stories, snapping photos, picking up signed books, and radiating joy. Scroll down to see some of their beautiful, beaming faces!
Adding even more love to this experience, my two sons, Robert (23) and Jackson (20), braved the Phoenix heat to support their mom. From answering questions and taking photos to selling books and making sure I was fed, they were unwavering in their support. They’ve been helping with the business since their teen years—and seeing them shine at the booth made me tear up more than once.
And of course, my husband of 27 years, Kris, was the perfect greeter and passionate advocate for our mission. He chatted about diabetes and healthcare with visitors, beaming with belief in our work. His dedication and enthusiasm are a gift I never take for granted.
✨ Thank you to everyone who made this such a meaningful and unforgettable experience. My heart is full.
September 2025 eNews
Featured Articles ___________________________ |
Upcoming Programs ___________________________ |
Happy September!💚
Greetings, wonderful healthcare colleagues!
This was my first time attending ADCES as an exhibitor in the big hall, and we went all out! Our booth sparkled with glittery pancreases, shimmering purple accents, and vibrant energy. One of the highlights was our “I DID IT!” banner, where proud course graduates stopped by to sign their name in bold felt-tip marker—celebrating their CDCES or BC-ADM success using our study materials. I was bursting with pride as the banner filled with names, each one representing countless hours of dedication and perseverance.
What truly filled my heart was the stream of hundreds of educators who came by to express their gratitude and share their stories. Please scroll down to see some of their beautiful, beaming faces!
We have two exciting articles to share this month. The first one considers the importance of evaluating and staging Cardiovascular-kidney-metabolic (CKM) syndrome and taking action to reduce risk. In our technology corner, we explore the latest features of the Tandem insulin pump, uncover the details of the new algorithm, and review the compatible CGM options.
Test your knowledge with our question and rationale of the week, and check out our upcoming online courses. We still have space in our San Diego Conference, but seats are selling fast. You don’t want to miss this fun and super informative experience!
With appreciation,
Coach Beverly, Bryanna, & Katarina
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Rationale of the Week | Diabetes Distraction in the Clinic
For last week’s practice question, we quizzed participants on Diabetes Distraction in the Clinic. 97% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

In the clinic today, you are seeing L.K., a 28-year-old with type 1 diabetes who was diagnosed at the age of 10. She was referred by the healthcare team for carb counting education and to discuss insulin pump options. During the session, L.K. appears preoccupied with her phone, avoids eye contact, and appears disinterested. When you ask what L.K.’s goals are for today’s session, she reports, “No matter how hard I try, no one is ever happy with my readings. Going on a pump isn’t going to change that”.
As a diabetes care and education specialist, what would you do?
- Point out to L.K. that she appears distracted and ask her if she wants to reschedule the appointment.
- Educate L.K. on diabetes-related complications related to chronic hyperglycemia.
- Continue the education session as planned, but make sure to provide handouts she can use later.
- Pause the session to explore L.K.’s feelings and beliefs about her diabetes care and previous experiences.
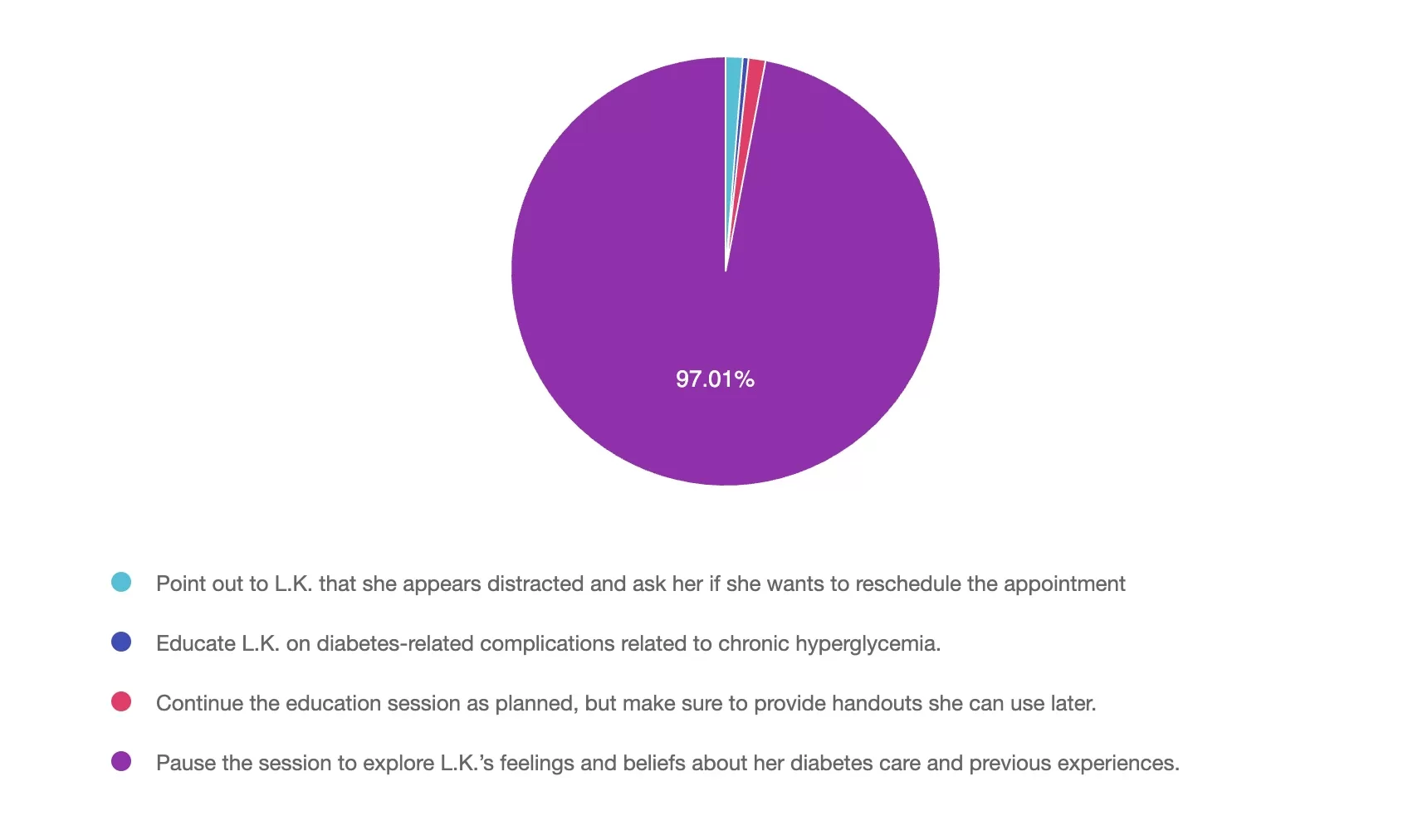
Getting to the Best Answer
Answer 1 is incorrect. 1% chose this answer, “Point out to L.K. that she appears distracted and ask her if she wants to reschedule the appointment.” L.K. verbalized her frustration with her diabetes and the healthcare system. As the diabetes healthcare provider, you are poised not only to provide information, but also to build a trusting relationship using person-centered approach. Stopping the session and rescheduling might derail collaboration and forward movement.
Answer 2 is incorrect. 1% of you chose this answer, “Educate L.K. on diabetes-related complications related to chronic hyperglycemia.” Although educating clients about the potential health outcomes of chronic hyperglycemia is essential, it does not constitute a person-centered approach in this situation. L.K. has made it clear that she is frustrated with her diabetes and healthcare experience.
Answer 3 is incorrect. About 1% of respondents chose this, “Continue the education session as planned, but make sure to provide handouts she can use later.” Continuing the education session with L.K. after she has verbalized her frustration is not a person-centered approach to care. She will not be engaged and an active participant in her care if she does not feel heard and validated.
Finally, Answer 4 is correct. 97% chose this answer, “Pause the session to explore L.K.’s feelings and beliefs about her diabetes care and previous experiences.” Every client has both positive and negative experiences in their diabetes journey that will influence their diabetes self-management and health outcomes. The statement she made in the diabetes education session must be addressed and discussed to build trust and understand her specific concerns. This approach is person-centered, leading to a shared decision-making approach to her personal diabetes goals.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Question of the Week | Lifestyle Therapy for MASLD and MASH
PJ has had type 2 diabetes for 8 years and is here for a follow-up visit. Labs indicate A1c at 7.2%, lipids at target, eGFR of 78 mL/min/1.73m², and urine albumin-to-creatinine ratio (UACR) of 65 mg/dL. Blood pressure at the office visit today was 142/86, which is consistent with home monitored values. PJ confirms taking medications, metformin and simvastatin. PJ inquires about recently completed lab work.
According to the ADA Standards of Care, what would be an appropriate next step in the diabetes care plan?
- No changes are needed because kidney function is within normal range.
- Initiate an ACE inhibitor or ARB to reduce progression the of diabetic kidney disease.
- Discontinue metformin due to the risk of kidney injury with reduced eGFR.
- Increase statin therapy to target albuminuria reduction.
Want to learn more about this question?

Invite a colleague to our DiabetesEd Seminar in San Diego and get $75 off each registration.
Use code FriendDiscountSD during check out to save.
Join us live in San Diego October 22nd – 23rd, 2025 for our upcoming
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
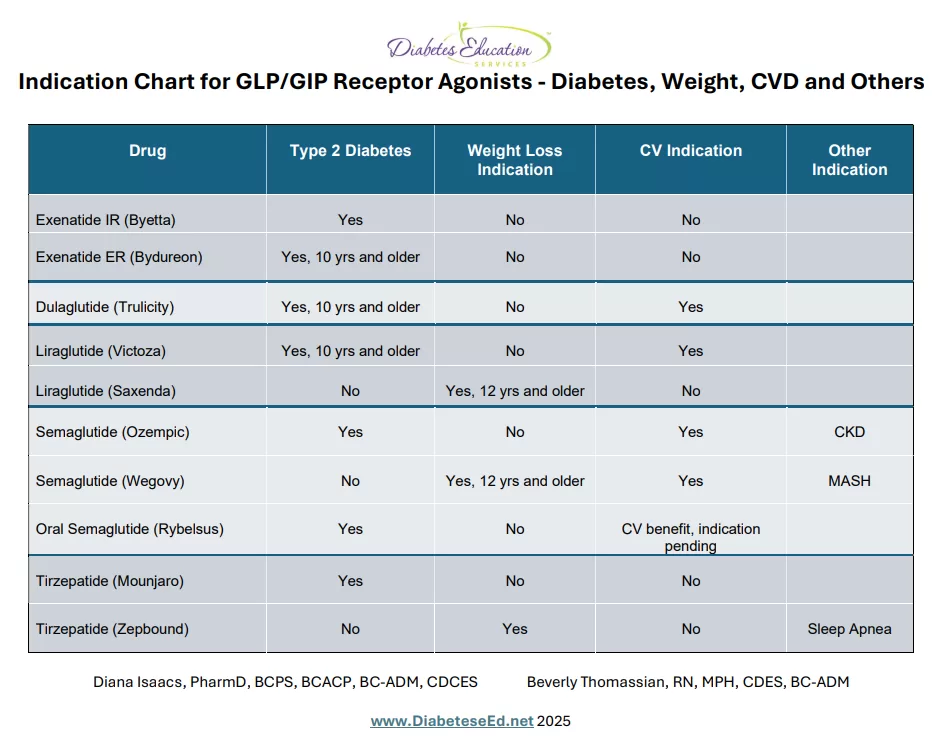
Indications for GLP-1/GIP RA Summary Sheet and Beyond!
GLP-1 receptor agonists and GLP-1/GIP combination therapies have become foundational treatments for type 2 diabetes and obesity. Their benefits now extend well beyond glycemic control and weight loss, with growing evidence supporting their use in the management of steatosis liver disease, obstructive sleep apnea, cardiovascular disease, and chronic kidney disease. Emerging studies even suggest potential therapeutic benefits in heart failure, further expanding the clinical utility of this powerful drug class.
Summary Table to Keep Track of Indications for GLP-GIP RA’s
We are excited to share this summary sheet of all the current indications for the incretin class of medication over the past ten years. This article provides a brief summary of all the indications plus you can refer to our newly published GLP-GIP RA Indication Cheat Sheet here. We created this summary so busy healthcare professionals (YOU) could keep track of all these evolving developments. Keep checking back, because we will keep updating this chart based on the lasts research findings and FDA Approvals.
✔️ Approval for Diabetes and Weight Management
Over the past decade, three GLP-1/GIP receptor agonists—liraglutide, semaglutide, and tirzepatide—initially approved by the FDA for adults with type 2 diabetes, have also gained FDA approval for chronic weight management in people without diabetes, provided they meet specific criteria: a BMI of ≥30, or ≥27 with at least one weight-related condition such as hypertension, dyslipidemia, or type 2 diabetes.
✔️ Expanded Approval for Pediatrics
With rising rates of diabetes and excess weight in children, the FDA has expanded the use of incretin-based therapies to younger populations. Three diabetes incretin medications are now approved for pediatric use starting at age 10 (see cheat sheet), and two incretin-based weight management medications are approved for children aged 12 and older.
✔️ Approval for Cardiovascular Risk Reduction
Ongoing cardiovascular outcomes trials (CVOT) studies clearly demonstrated that three of the diabetes incretin medications (liraglutide, dulaglutide and semaglutide) and one of the weight loss versions of this class (Wegovy) also reduce cardiovascular disease risk. The CVOT results for the oral version of semaglutide (Rybelsus) are pending, with results expected soon.
✔️ Approval for Sleep Apnea, MASH, CKD
Tirzepatide (Zepbound) — originally approved for weight loss — now also holds FDA approval for the treatment of moderate to severe obstructive sleep apnea in adults with obesity. Semaglutide (Wegovy) has been granted FDA approval for the treatment of metabolic-associated steatohepatitis (MASH, or NASH with fibrosis). Meanwhile, semaglutide (Ozempic) is now FDA‑approved for reducing the risk of kidney disease progression and renal outcomes in people with type 2 diabetes and chronic kidney disease. And there is more to come!
Looking toward the future
The wheels of progress on multi-agonists, oral small molecules, and tissue-targeted approaches are moving forward at breakneck speed.
This brilliant JAMA review by Gonzalez-Rellan & Drucker — one of the original discoverers of GLP-1 biology. In a single piece, he concisely captures:
– the state of the field
– the most important clinical trials
– where the pipeline is headed
These Clinical trials are raising the bar and expanding future treatment options:
• Retatrutide → ~24% weight loss (triple agonist)
• MariTide → 12–16% weight loss (GLP-1 + GIP antagonist)
• CagriSema → up to 20% weight loss + ~2% HbA1c drop
• Orforglipron → oral GLP-1, HbA1c –1.5%, weight –7.6%
• IcoSema → weekly semaglutide + once-weekly insulin
Even more exciting? There are clinical trials evaluating if these GLP-1 and multi-agonists can address neurodegeneration, addiction, inflammation, and beyond.
Access, Cost and Shifting Landscape
As people on these agents meet their weight and diabetes goals, there is concern that insurance companies will reduce or stop coverage given the high price tag of lifelong incretin therapy. Hopefully, competition may drive price pressure or encourage development of biosimilars/generics in the long term. In addition, as new agents enter the market, payer coverage and prior-authorization landscapes will shift—especially with expanded medication benefits.
Diabetes Healthcare Professionals Consider Whole Person
As diabetes healthcare professionals, we want to carefully consider which medication best matches the people in our care, considering individual values and preferences along with co-conditions including diabetes, cardiorenal metabolic co-conditions, MASH, sleep apnea and weight goals.
Download Summary Sheet Here!
Join us live in San Diego Next Week

It’s not too late to register!
Get ready for certification & take your practice to the next level
October 22nd – 23rd, 2025
DiabetesEd Training Seminar
30+ CEs with Expanded Accreditation!

Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Question of the Week | Clinical Clues to Hypercortisolism
AJ is a 52-year-old with type 2 diabetes presents with worsening hyperglycemia despite taking three diabetes medications. AJ says, “No matter what I do, I can’t seem to get my blood sugars down”.
Which of the following clusters of physical findings would increase your suspicion that AJ is struggling with hypercortisolism?
- Dorsocervical fat pad, wide purple striae and bruising.
- Peripheral muscle hypertrophy, thick hair growth, and flushed skin.
- Weight loss, skin hyperpigmentation, and generalized muscle wasting.
- Pallor, brittle nails, and spoon-shaped fingernails.
Live in San Diego
DiabetesEd Training Seminar
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!

 Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Expert Faculty:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Faculty Bios & Disclosures
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
- Consultant, advisor, and speaker for Abbot Labratories, Dexcom, Medtronic, Insulet, Lilly, Cequr, Sanofi, and Undermyfork
- Board member at Association for Diabetes Care and Education Specialists
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Expanded Accreditation
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Hormone Replacement Therapy Warnings Removed
By: Astraea Ballinger and Beverly Thomassian

Hormone Replacement Therapy (HRT) is an important topic of conversation due to its vast untapped benefits for women and people with uteruses. Due to a two decade misinterpretation of study results and black box warnings, HRT has been mostly denied as an intervention for individuals who could benefit from treatment.
Flaws in the Women’s Health Initiative Study
In the early 2000s, prescriptions for HRT products dropped significantly due to the FDA’s addition of black box warnings. The application of the black box warnings stemmed from a Women’s Health Initiative (WHI) study that warned of a significantly increased risk of breast cancer diagnosis for those using HRT. These findings were later shown to be inaccurate or overstated, but the initial conclusions caused long-lasting caution, leading to many years of limited progress and underutilization of HRT therapy.
Say goodbye to the Black Box Warning and Hello to HT
There is a renewed recognition of the benefits of hormone therapy. According to the recent press release on November 10th, the FDA is removing the boxed warnings following a comprehensive review of the scientific literature by an expert panel. The FDA is working with companies to update language in product labeling to remove references to risks of cardiovascular disease, breast cancer, and probable dementia. The FDA is not seeking to remove the boxed warning for endometrial cancer for systemic estrogen-alone products.² Of course, ongoing studies are needed to monitor long term safety and efficacy of hormone therapy.*
Of note, many menopause specialists are now using the term Hormone Therapy (HT) instead of HRT. The reason being that the goal is not to replace hormones to premenopausal levels – just to add back enough hormones to reduce symptoms and prevent other chronic conditions. HT is also a broader term that includes replacement of hormones or using hormones to treat a disease.
Benefits of Hormone Therapy (HT)*
- Randomized studies show that individuals who initiate HT within 10 years of the onset of menopause (generally before age 60) have a reduction in all-cause mortality and fractures.
- FDA-approved HT containing estrogen and progesterone (or estrogen alone as indicated for postmenopausal individuals) can restore declining hormones, and relieve symptoms such as hot flashes, night sweats, sleep disturbances, and bone loss.²
- Estrogen is a key hormone for women and people with uteruses’ health. Every single part of the body depends on estrogen to operate at optimal levels—including the brain, bones, heart, and muscles.
- Women and people with uteruses who use HT reduce their risk of:
- Cardiovascular diseases by as much as 50%,
- Cognitive decline and Alzheimer’s disease by 35%.*
- Bone fractures by 50 to 60%.
- Estrogen also helps collagen production, and collagen disappears from the vulva by up to 30% in the five years after menopause. ³
- Vaginal estrogen can be used by most breast cancer survivors, too, and it’s a win-win on the physical intimacy front.
- Vaginal estrogen can be used alongside HT.³
- Oral vs. Transdermal: Transdermal estrogen is associated with a lower risk of venous thromboembolism (blood clots) compared to oral HT because it avoids first-pass metabolism in the liver.
Cancer Considerations with Hormone Therapy
For individuals with a history of hormone-sensitive conditions like certain breast cancers, non-hormonal options are often recommended. While the general recommendation is to avoid systemic HT for people with breast cancer history, some experts are calling for a more personalized approach, suggesting that for certain individuals with severe symptoms, a risk-benefit assessment might be considered, especially if non-hormonal treatments have failed.
*Limitations & Uncertainties:
Due to the longstanding limited use of HRT, data from ongoing and future longitudinal studies will provide additional evidence about the risks/benefits of long term HT treatment. Careful consideration of individual factors need to go into making decisions to pursue HT (including, age, comorbidities, health history, current medication etc.) As with any therapy there can be potential risks associated with HT use.
More upcoming approvals for HT
In addition to the removal of boxed warnings, the FDA is also approving two new drugs to expand treatment options for menopausal symptoms. The first is the approval of a generic version of Premarin (conjugated estrogens), the first such approval in more than 30 years for this widely used form of hormone replacement therapy. The new generic product is expected to improve affordability and access while maintaining the same quality, safety, and effectiveness as the brand-name drug.
The second approval is for a non-hormonal treatment for moderate to severe vasomotor symptoms, such as hot flashes, associated with menopause. This option provides relief for women who cannot or choose not to use hormone therapy. ²
HT and Urinary Tract Infections (UTI)
More than half of people with uteruses will have at least one UTI in their lifetime. One in four women and people with uteruses have a UTI strain resistant to certain common antibiotics. Younger women and people with uteruses do suffer from infections, dehydration and post-sex cystitis, but the brunt is borne by older women. UTI rates shoot upwards when women hit 45 and are perimenopause. Plus, lack of estrogen means the lactobacilli and other good bacteria in the vaginal microbiome are at risk of being replaced by pathogenic ones.
SGLT-2 Reduction of UTI with estrogen
Estrogen deficiency after menopause is an important predisposing factor for reoccurring UTIs (r UTI). Another recent study in 2020 was designed to observe the risk and frequency of UTI due to SGLT2 Inhibitors among post-menopausal individuals with T2DM and the preventive effect of vaginal e HRT for r UTI among them.
Study Design: Forty-two, post-menopausal individuals with type 2 diabetes, using vaginal e HRT were selected as cases whereas controls were 38 matched individuals not using e HRT. Subjects in both groups were prescribed SGLT2 I considering eligibility and simultaneously adjusted the doses of other OHA’s or insulin to maintain the glycemic targets. They were targeted to follow for 12 months and evaluated periodically for symptomatic UTI and maintenance of glycemic targets. Diagnosis of symptomatic UTI was made using standard definition and guidelines.
The results? The 42 participants who were using vaginal e HRT compared to the 38 who did not use e HT, demonstrated significantly lesser frequency of UTIs. Estrogen HT after menopause significantly reduces the frequency of UTI among people with type 2 diabetes using SGLT2 I. Or said in another way, not using eHT for those with diabetes on SGLT-2I may significantly increase risk of complicated UTI.¹
Genitourinary Syndrome of Menopause (GSM)
The estrogen hormone deficiency associated with menopause has been renamed Genitourinary Syndrome of Menopause (GSM). This describes the chronic decrease in estrogen levels, resulting in a combination of genital, sexual, and urinary symptoms. While most common after menopause, GSM can affect premenopausal women experiencing low estrogen levels due to other medical conditions or treatments. This syndrome is associated with the hormone estrogen leaves the vulva dry in menopause (and sometimes post-pregnancy), a condition previously called “vaginal atrophy.”
Case Study Highlighting HT Benefits for GSM
In a recent 2020 case study, a 64-year-old woman (MS) was referred for recurrent urinary tract infections (UTIs). She presented with progressive complaints of vaginal dryness, sensitivity, and pain at the introitus with associated dyspareunia despite the use of over-the-counter vaginal lubricants. MS was offered treatment with vaginal estrogen therapy for her GSM.
For relief, MS was initiated on a 2-week course of nightly estradiol cream followed by maintenance therapy twice weekly. She returned for a 3-month follow-up and reported significant improvements in vaginal dryness, with resolution of her introital irritation and dyspareunia. She had not had a UTI in this time frame. MS also reported significant improvements in her quality of life and sexual function. 4
Both the lower urinary tract in women and the vaginal and introital tissues are rich in estrogen receptors. We can prevent GSM in perimenopause and menopause by giving individuals a safe, low dose of vaginal estrogen, which plumps the tissue, feeds the vaginal microbiome and reduces UTIs by 50%.²
Effective care of women and people with uterus’s is enhanced by gaining knowledge and being aware of current recommendations for treating both menopausal symptoms in general and GSM. 4
There are currently 7 FDA-approved vaginal estrogen products for the treatment of GSM. Shared decision making to determine the best choice of vaginal estrogen product is important and can improve satisfaction with therapy. ¹
Let’s Get the Word Out!
As healthcare professionals caring for people with diabetes, we can discuss the benefits for HT for individuals in perimenopause and menopause. We can also advocate for use of vaginal estrogen for individuals experiencing frequent UTIs, especially for those taking SGLT-2 inhibitors.
References
- ASHISH GAUTAM, PRABHAT K. AGRAWAL, NIKHIL PURSNANI, RUCHI RANI; 140-LB: Effect of Vaginal Estrogen as Hormone Replacement Therapy for Menopause on SGLT2 Inhibitor–Associated Urinary Tract Infection: A Prospective Cohort Study. Diabetes 1 June 2020; 69 (Supplement_1): 140–LB. https://doi.org/10.2337/db20-140-LB
- FDA. (2025, November 10). HHS advances women’s health, removes misleading FDA warnings on hormone replacement therapy. U.S. Food and Drug Administration. https://www.fda.gov/news-events/press-announcements/hhs-advances-womens-health-removes-misleading-fda-warnings-hormone-replacement-therapy
- Muir, K. (2023, December 17). “Millions of women are suffering who don’t have to”: Why it’s time to end the misery of UTIs. The Guardian. https://www.theguardian.com/society/2023/dec/17/millions-of-women-are-suffering-who-dont-have-to-why-its-time-to-end-the-misery-of-utis
- Rosenblum, N. (2020, December). Update in female hormonal therapy: What the urologist should know: NYU case of the month, December 2020. Reviews in urology. https://pmc.ncbi.nlm.nih.gov/articles/PMC8058921/