Renewing My CDCES – What is Required?
You have passed the CDCES Exam (yay) and 5 years have flown by, now you are up for renewal. How do you maintain your certification?
The rules around renewing can be a little confusing, so here are excerpts from the CBDCE Website and Newsletter that we hope you find helpful! Of course, for any additional questions or special situations, we recommend you visit the CBDCE Website or check out the links toward the end of the article.
For CDCES Recertification, there are three paths you can take.
Path 1. Renew through earning CEs
Path 2. Renew by taking the Exam
Path 3. Renew by taking the Exam and earning CEs
For Path 1 and 2 you need to:
- Accrue 1,000 hours of professional practice experience during the 5-year cycle
- Continue to hold the license or registration (e.g. RN, RD, MD, PA, etc.) for the same discipline held at the time of initial certification. This license or registration must be current, active, and unrestricted at the time of renewal.
- Renew by taking an Exam or earning 75 CE’s (see details below)
Path 3, this option is for those not able to meet the 1000 hour practice experience requirement, but applicants must:
- Continue to hold a license ( (e.g. RN, RD, MD, PA, etc.)
- Take the CDCES Exam
- Earn 75 CE’s (see details below)
Cost and Time Frame
The cost to renew your CDCES Certification is well worth the $250 dollars ($50 per year). This certification is widely recognized and respected by people with diabetes, health care professionals, and employers alike.
Time Frame: Certification is valid for a five-year time frame with an expiration date that ends on December 31st of the last year of the certification cycle.
- Example: Coach Beverly last renewed her CDCES in March of 2017. She will need to renew her certification (by exam or CEs) by December 31st of 2022.
As many of you know, I choose to take the exam every 5 years to renew my CDCES. But, most people choose to renew through CEs. See the information below.
How do you Earn the 75 CEs required for Path 1 & 3?
When renewing by Renewal Pathway 1 and 3, you will need to earn a minimum of 75 CE hours during your accrual cycle. You can do this by only accruing 75 CE hours under the “Formal Activities” or you can mix and match with “Formal” and “Expanded Activities.”
Formal activities include:
- Continuing education courses
- Independent study
- Seminars
- Online programs
- Workshops
- Telephonic or video conference programs
- Conferences
Expanded activities include:
- Academic courses
- Presentations or lectures led by the certificant
- Publications – articles or books written by the certificant
- Service as a Mentor in CBDCES’s Mentorship Program
If you are using “Expanded Activities,” there are limits on each “Expanded Activity,” and the maximum hours you can claim during your accrual cycle is 30 CE hours from the “Expanded Activities” Category.
Feel free to mix and match from both the “Formal” and “Expanded” categories as long as at least 45 hours of CE activities fall under the “Formal” category.
Formal Category CE Requirements
The Activities in the “Formal” Category must meet identified requirements. All of the 75 CE hours can be accrued under the “Formal” category.
Continuing Education Hour Defined: – All continuing education activities must be reported in clock hours. One clock hour equals 60 minutes.
For the “Formal” category of continuing education, activities must be:
- Provided by or approved by a provider on the CBDCE List of Recognized Providers.
- *Since Diabetes Education Services is Accredited by the Commission on Dietetic Registration (CDR), all of our courses can be applied toward your CDCES Renewal.
- Applicable to diabetes. All subject matter on the Certification Exam Content Outline is considered applicable.
- Completed before the application deadline and before submitting the application, or by December 15 if using the Grace Period.
- At a professional level that enhances the quality and effectiveness of the practice of diabetes care and education.
For more details on the qualifying activities, review Guidelines for Reporting Continuing Education Activities and the Renewal Handbook.
Is it Worth all this Work? – YES!
Achieving my CDCES is one of the best and most meaningful investments in professional career! ~ Coach Beverly
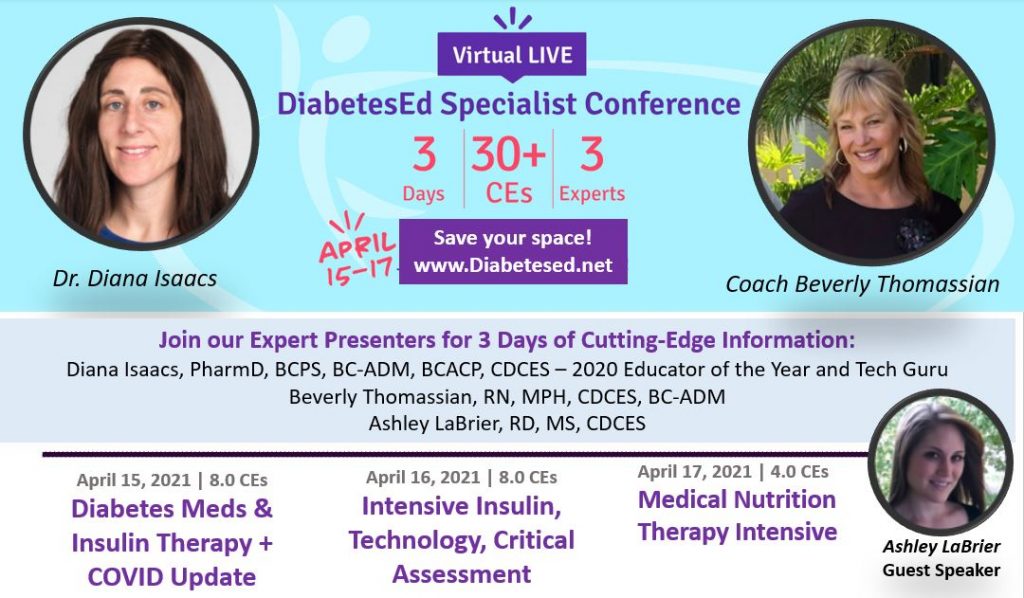
It’s not too late to reserve your spot for our
Virtual DiabetesEd Specialist Conference | April 15-17, 2021
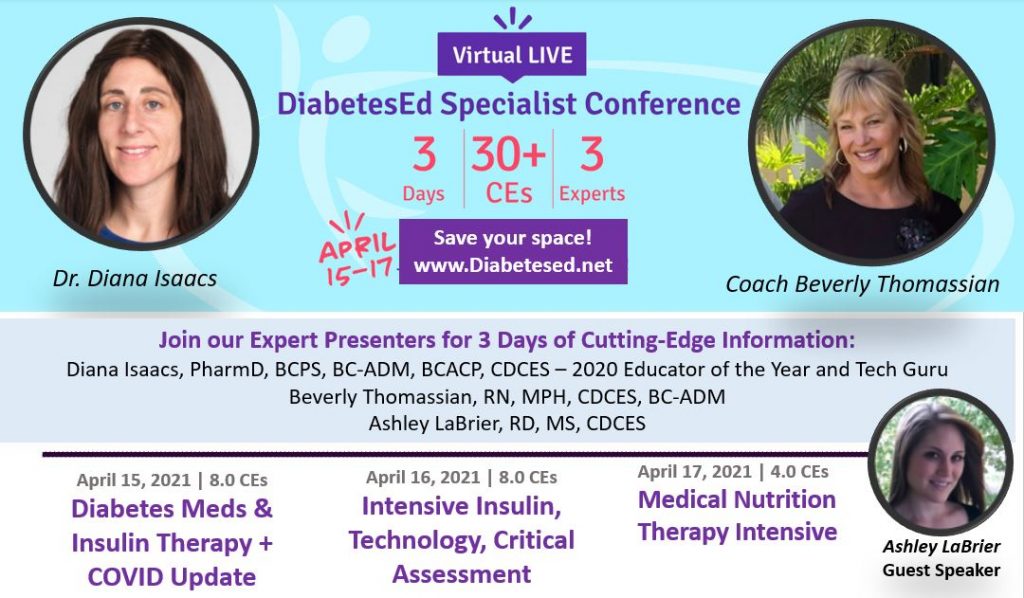
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. If you are interested in taking the CDCES or BC-ADM exam or are seeking a state-of-the-art review of current diabetes care, this course is for you.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Entire Program Fee: $399
Dates: April 15-17, 2021
3 Expert Speakers
CEs: 30+ CE hours
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Come join our Virtual DiabetesEd Specialist Program.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
- Live Q & A Session with the instructor after each webinar
- Presentations by our team of experts
- Handouts and Resources for each session
- Post-test questions
- A sense of community
- If you can’t attend the live webinars, a recorded version will be posted later the same day for viewing.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
*The use of DES products do not guarantee successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.”**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve continuing education.
Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”
Question of the Week | Type 1, Ramadan & Fasting

RS observes Ramadan and fasts from sunrise to sunset. RS is 13 years old, has type 1 diabetes, uses an insulin pump and CGM. RS’s insulin-to-carb ratio is 1:12 and correction is 1:45. Basal settings range from 0.5 -1.2 units an hour.
What would be the best recommendation for RS to keep blood sugars in the target range during Ramadan?
- See if RS can get a note from their doctor to allow eating during the day.
- Take bolus insulin when RS eats a meal or snack.
- Decrease basal insulin rate by 50% during periods of fasting.
- Monitor urine ketones at least twice a day.
Click here to test your knowledge!
Want to learn more about Medical Nutrition Therapy?
You are invited to join our Virtual Conference on April 26th – 28th with our Nutrition expert speaker, Ashley LaBrier, MS, RD, CDCES, who will be providing a half-day presentation on this important topic!

Ashley LaBrier, MS, RD, CDES, is an innovator in the field of diabetes, nutrition, and technology. Ashley is a consultant and the Diabetes Education Program Coordinator at the Salinas Valley Medical Clinic’s Diabetes & Endocrine Center.
Ms. LaBrier is passionate about providing person-centered education to empower those who live with diabetes. Having been diagnosed with type 1 diabetes herself nearly 20 years ago, she combines her professional knowledge with personal experience and understanding.
Virtual DiabetesEd Training Conference
April 26th – 28th, 2023
Your team is invited to our Virtual DiabetesEd™ Training Conference! Set your team apart and prepare for diabetes certification!
Join this state-of-the-art conference taught by content experts, Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES, Beverly Thomassian RN, MPH, CDCES, BC-ADM, and Ashley LaBrier who are passionate about improving diabetes care.
Group discounts are available!*
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparator
Prep for BC-ADM Exam 2021 Free Webinar | April 8th
Studying for the BC-ADM exam?
Join Coach Bev for a FREE Webinar to get the info you need for success.

April 8, 2021, from 11:30 a.m. – 12:45 p.m. (PST)
Unsure about updates for this mastery level 2021 exam?
Join us to get ready to succeed at the BC-ADM Exam. This course will transform your test anxiety into calm self-confidence and test taking readiness.
Topics Covered Include:
This free webinar will review BC-ADM requirements for the current year.
- exam eligibility and test format,
- strategies to succeed
- study tips and test-taking tactics.
She will also review sample test questions and the reasoning behind choosing the right answers. We hope you can join us.
See our Prep for BC-ADM Resource Page
Instructor: Beverly Thomassian RN, MPH, CDCES, BC-ADM is a working educator who has passed her CDCES Exam 6 times and first earned her BC-ADM credential 20 years ago. She is a nationally recognized diabetes expert for over 25 years.
Studying for the BC-ADM?
Try one of our bundles!
BC-ADM Prep Bundle | Levels 2, 3, & 4 | 39+ CES
Beverly has custom designed this course bundle to prepare you for your BC-ADM Exam. Including Level 2 (Standards of Care Intensive), Level 3 (Boot Camp), and Level 4, you can start studying now with 29 On-Demand webinars and practice tests to build your diabetes education foundation and prepare for the BC-ADM Exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
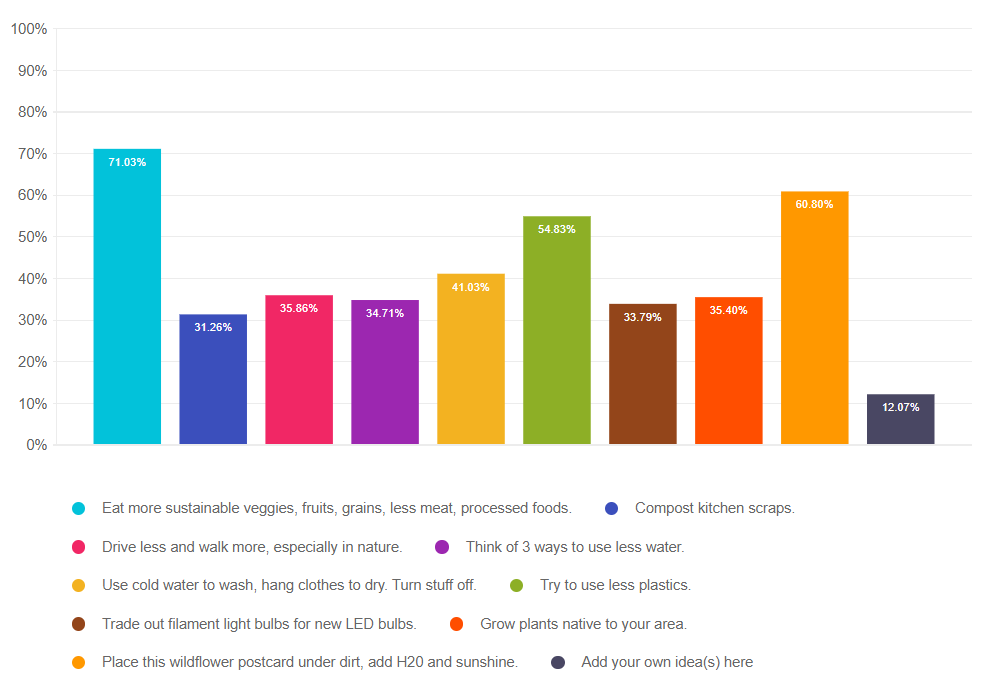
Planetary Pledges for a PocketCard Tops 900
Overjoyed by your commitment to take action
For Earth Day we encouraged our community to take action to protect our earth. In return, we promised to mail a Medication PocketCard and a plantable Wildflower Postcard to say thanks.

We couldn’t believe the response.
To date, 936 of you chose one or more action to take from our list of ten and hundreds of you added dozens of fantastic additional ideas. See the list below.
Originally, we had planned to stop when we reached 500 promises, but we couldn’t help but expand our vision. We decided to honor each person who is willing to commit to taking action with a PocketCard. We even hired additional staff to help us stuff, stamp, and seal the 900 plus envelopes.
It’s worth it. As a company, we are taking action to decrease our footprint on the earth. We went paperless over 5 years ago, we turn off our computers and A/C at the end of the day, we work remotely to decrease driving and we work to share information that promotes social justice and environmental conservation.
As an individual, Coach Beverly is committing to actualizing these 10 Actions in her life and will share her stories as she stumbles, moves forward, and incorporates these changes. It’s not going to be pretty or perfect, but behavior change never is.
Today is the Last Day to Take the Pledge!
We have decided that we will keep this offer on the table for one more week. Although we might run out of plantable Wildflower Postcards, we will send you a PocketCard in exchange for your commitment. We believe in our ability to contribute to positive change. We are proud of our community of diabetes educators and advocates. You rock.
Your Planet Saving Ideas
- Bike, walk or take public transit instead of driving (7 of you made this commitment)
- Compost food scraps (2 of you made this commitment)
- Convert to solar energy (3 of you made this commitment)
- Drive eco-friendly car (2 of you made this commitment)
- Eat less meat and animal products (5 of you made this commitment)
- Encourage others to take the pledge (7 of you made this commitment)
- Grow a native garden or your own fruits, vegetables, and herbs (20 of you made this commitment)
- Participate in earth day festival
- Pick up litter (4 of you made this commitment)
- Plant trees (5 of you made this commitment)
- Preserve foods for longer storage
- Reduce energy usage and insulate the house for energy efficiency (7 of you made this commitment)
- Reduce paper usage or use natural brown and recycled paper when needed (5 of you made this commitment)
- Reduce plastic usage by doing things like bringing your own Tupperware for leftovers at a restaurant or reusable bags to stores (4 of you made this commitment)
- Recycle, reuse items instead of replacing them, only buying necessities, and donating used items (25 of you made this commitment)
- Shop at local farmer’s markets
- Spread kindness to all living creatures
- Start apiary for honey bees (2 of you made this commitment)
- Unplug and go outdoors more
- Use gray or rainwater for garden (3 of you made this commitment)
10 Ways to Help the Planet
Change isn’t easy. We aren’t going for perfect, we are starting with intention and slowly moving to action, giving ourselves lots of grace along the way. I am excited to share my successes and wrong turns with you on this journey and we would love to hear from you too!
- Grow plants native to your area.
- Compost kitchen scraps and cut down on waste
- Eat more sustainable veggies, fruits, grains and less meat, processed foods.
- Drive less and walk more, especially in nature
- Think of 3 ways to use less water
- Use cold water to wash, hang clothes to dry.
- Turn appliances, lights and computers off when not in use.
- Purchase used items and re-use everything you can. Swap and trade instead of buying new.
- Try to use less plastics
- Trade out filament light bulbs for new LED bulbs.
Read more on our blog, Earth Day Secrets to Improving Planet Health
Stay tuned and we share details and resources on each of these 10 Steps over the next few months. And, please send us your stories too at [email protected]. We want to hear from you!
How to Protect the Planet Resources Page
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | How Many Insulin Pens?

Our March 23rd Question caused a lot of commotion. Less than half (43%) of respondents chose the best answer, so we wanted to dive deeper into this question of how many pens are needed.
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer below: Answer Question
Question: JR is 24 years old and uses an insulin pen for their basal insulin injections each evening. JR takes 30 units a night and each insulin pen holds 300 units of insulin.
How many insulin pens would JR need for one month?
Answer Choices:
- 3 pens
- 4 pens
- 10 pens
- 1 box
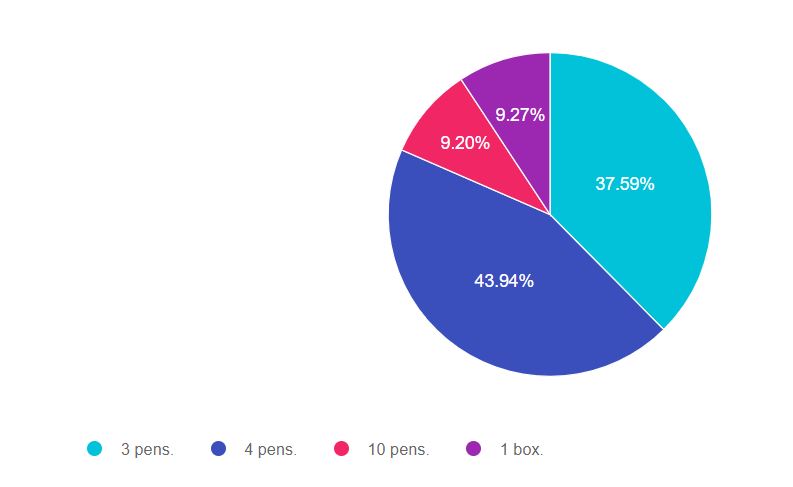
As shown above, the most common choice was option 2, the second most common answer was option 1, then option 4, and finally option 3.
Getting to the Best Answer
We had over 1,500 attempts at getting to the best answer. If you are thinking about taking the certification exam, the content of this practice test question will set you up for success. The exam will present questions that require test takers to make sure the answer matches the key intent of the question. This is also a word problem. Setting up the problem correctly before doing the math is very important.
In this situation, we are asked to answer, “How many insulin pens would JR need for one month?” The main goal of this question is to make sure that test-takers incorporate the 2 unit air shot into calculating how much insulin is needed for the month.
Answers & Rationale
Answer 1 is incorrect, 37.59% chose this answer, “3 pens.” JR takes 30 units of basal insulin a night. However, we know that JR needs to prime their insulin pen with a 2 unit air shot before each injection. To make sure the insulin pen and needle are working correctly, we instruct people to use a new pen needle and to prime the pen before injection. This means that JR will use 32 units of insulin each night (30 units for the injection, 2 units to prime the pen).
32 units x 30 days = 960 units. If each pen holds 300 units, 3 pens only hold 900 units. JR would run out of insulin at least 2 days ahead of time. For this reason, this answer is not correct.
Answer 2 is correct, 43.94% of you chose this answer, “4 pens.” Great job. You considered that JR needs to prime their pen before each injection.
JR takes 30 units of basal insulin a night. We know that JR needs to prime their insulin pen with a 2 unit air shot before each injection. To make sure the insulin pen and needle are working correctly, we instruct people to use a new pen needle and to prime it before injection. This means that JR will use 32 units of insulin each night (30 units for the injection, 2 units to prime the pen).
32 units x 30 days = 960 units. If each pen holds 300 units, JR will need 4 insulin pens for the month.
Answer 3 is incorrect, 9.20% of you chose this answer, “10 pens.” This was a juicy answer. Respondents who chose this probably looked quickly at the question and divided 300 by 30 to get 10 pens. In this question, paying attention to the details before diving into math is really important.
Each pen holds 300 units and JR takes 30 units of insulin a night. When you add in the 2 units to prime the pen, JR needs 4 insulin pens a month.
Answer 4 is incorrect, 9.27% of you chose this answer, “1 box.” This is another juicy answer. But, it doesn’t match the unit of measure of the question. The question asks, how many insulin pens and this response answers with a different unit, 1 box. The question also doesn’t ask how the prescription would be written. It only asks for how many pens. For this reason, this is not the best answer.
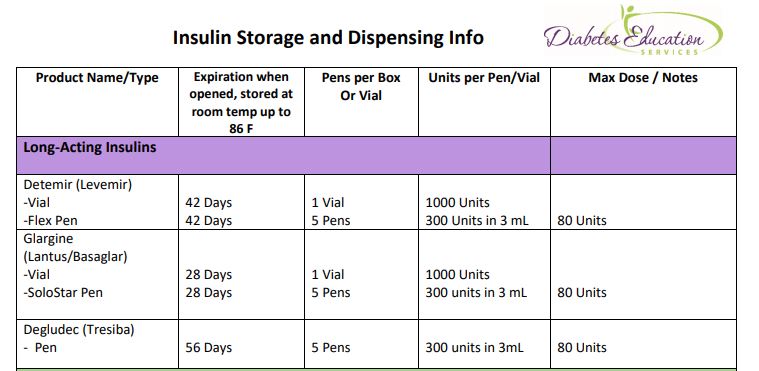
However, in the clinical setting, the prescription would be written for a box of 5 pens, since that is the usual dispensing unit.
Insulin Storage Cheat Sheet – Download for FREE. Provides all kinds of important details on the storage of different types of insulin pens, vials, and more!
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Interview with Coach Bev | Her Journey to Become a CDCES
CDCES – Practice Hours Requirement Changed due to Pandemic
This blog highlights important changes in required practice hours experience, celebrates 35 years of the CDCES Credential, and provides helpful study resources.
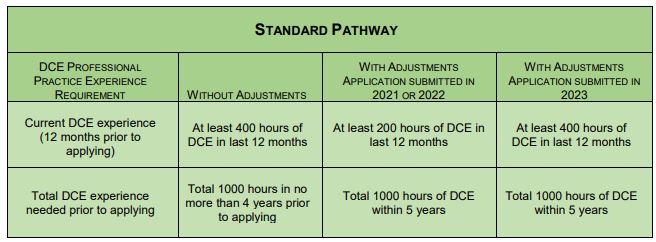
Taking the CDCES Exam in 2021 or 2022? The Certification Board for Diabetes Care and Education (CBDCE) has announced some important adjustments to the Professional Practice Experience Requirements due to the COVID pandemic.
To address the impact of the COVID-19 pandemic on the ability of health professionals pursuing the CDCES credential to accrue practice experience in diabetes care and education (DCE), the CBDCE Board of Directors has approved temporary changes to the professional practice requirement relating to DCE for initial certification.
CBCDE View Full statement here
Practice Experience Changes take effect April 1, 2021.
1) For applications submitted through 2022, minimum Diabetes Care and Education (DCE) experience needed in prior 12 months reduced from 400 hours to 200 hours;
2) For applications submitted through 2023, minimum of 1000 hours (or 2000 hours for unique qualifications pathway) of DCE experience needed can be accrued over a longer period of time. The time frame is increased from 4 years from application date to 5 years from the application date
Resources to Help
Coach Beverly remembers taking her first CDCES Exam in1992 (29 years ago). Back then, applicants needed 2000 hours of practice experience to qualify and a #2 pencil to bubble in the right answers on the exam scantron. She remembers how nervous she felt as she opened her test booklet and the lack of study tools to prepare for the exam. Because of this experience, Coach Beverly wants to make sure you have the tools you need to realize your professional dream of achieving certification.
Our passion is supporting health care professionals on their journey to gain mastery and become certified diabetes specialists.
Answer 4 Questions to see what Study Tools are Right for You.
CDCES FREE Webinar and Resource Page – Join Coach Beverly on April 1 (no joking)
Practice Hours Spreadsheet Tracker. Download this sheet to easily track your practice hours.
CDCES Coach App – We send you a Question of the Week and Rationale of the Week for FREE!
10 Steps to Success – Coach Beverly has custom-designed your road map to CDCES success!
CDCES First Time Pass Rate
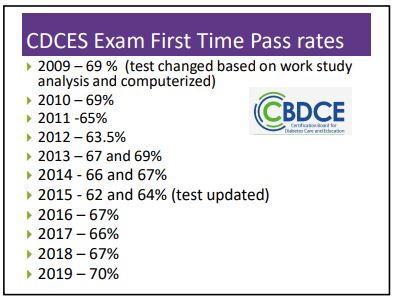
If you are taking the exam for the first time, you may be interested in a historical look back on passing rates.
As you can see, over the past ten years, about two-thirds pass the exam on their first go-round. This informs us that the test is challenging and requires a clear study plan to achieve success with special attention to those content areas that aren’t in our usual daily practice (for example, pediatrics, in-hospital, pregnancy, technology, type 1, etc.).
We offer a myriad of resources to help you on your journey (see list above).
CBDCE Celebrates 35 Years
This year, the CDCES (formerly CDE) celebrates its 35th Anniversary. There are currently over 19,500 health professionals in the diabetes care and education community that hold the CDCES credential.
And just in case you are wondering, the Certification Board for Diabetes Care and Education (CBDCE) is an independent specialty board responsible for the development and administration of the certification program for diabetes care and education programs. They are separate and independent from any other organization or association.
CBDCE’s mission is to promote comprehensive and ongoing quality diabetes clinical management, education, prevention, and support by defining, developing, maintaining, and protecting the certification and credentialing processes.
Interested in joining the CBDCE Board Of Directors?
If you already have your CDCES and are looking to get more involved with the CBDCE, they are actively seeking applicants for their Board of Directors. Find our more here!
It’s not too late to reserve your spot for our
Virtual DiabetesEd Specialist Conference | April 15-17, 2021
Whether you are new to diabetes or a seasoned expert, you’ll benefit from this virtual conference with the latest research plus critical content that you can immediately apply to your clinical practice. If you are interested in taking the CDCES or BC-ADM exam or are seeking a state-of-the-art review of current diabetes care, this course is for you.
DiabetesEd Virtual Conference Flyer 2021
Diabetes Ed Virtual 3-Day Schedule 2021
Entire Program Fee: $399
Dates: April 15-17, 2021
3 Expert Speakers
CEs: 30+ CE hours
Live Webinar Schedule: All webinars start and end times are in Pacific Standard Time
Come join our Virtual DiabetesEd Specialist Program.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
In addition to informative lectures, we also use group activities and case studies to highlight the essential knowledge, skills, and strategies needed to succeed in diabetes education today!
Prepare for CDCES or BC-ADM certification or earn hours for renewal.
Your registrations include access to all the Online Sessions plus Bonus Courses through December 31st, 2021.
This virtual program includes:
3 day live webinar courses from April 15th-17th (20 CEs) + enrollment in our Bonus Bundle (14.0+ CEs) from now through December 2021.
- Live Q & A Session with the instructor after each webinar
- Presentations by our team of experts
- Handouts and Resources for each session
- Post-test questions
- A sense of community
- If you can’t attend the live webinars, a recorded version will be posted later the same day for viewing.
View full Conference Schedule and Faculty.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
[yikes-mailchimp form=”1″]Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and Commission on Dietetic Registration (CDR), Provider DI002. Since these programs are approved by the CDR it satisfies the CE requirements for the CDCES regardless of your profession.*
The use of DES products do not guarantee successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.”**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.”