
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards
For last week’s practice question, we quizzed participants on Lower Extremity Recommendation for JT? . 77% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question:
JT is a 58-year-old with type 2 diabetes presents for a routine exam. Has a 20-year history of diabetes, hypertension, and peripheral neuropathy. Reports no foot pain, but partner notes they have been walking with a slight limp. On exam, you note dry skin, thickened toenails, a callus on the plantar aspect of the first metatarsal head, and diminished monofilament sensation at multiple sites on both feet. Pedal pulses are diminished bilaterally, and ABI (Ankle-Brachial Index) is 0.6 on the right and 0.7 on the left.
Which of the following is the most appropriate next step in managing this JT’s foot care?
Answer Choices:
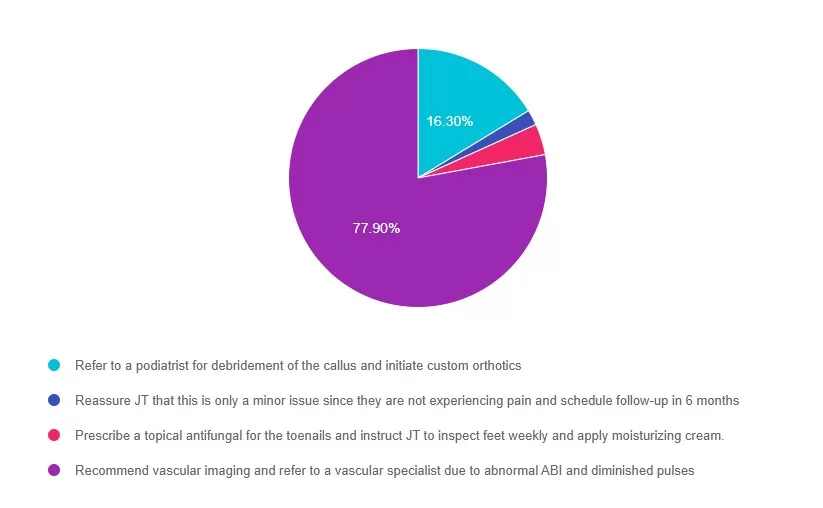
Answer 1 is incorrect. 16% chose this answer, “Refer to a podiatrist for debridement of the callus and initiate custom orthotics.” While podiatry referral is important, vascular compromise must be evaluated first. Debridement in a patient with peripheral arterial disease (PAD) could lead to poor healing or ulceration.
Answer 2 is incorrect. 1% of you chose this answer, “Reassure JT that this is only a minor issue since they are not experiencing pain and schedule follow-up in 6 months.” Absence of pain does not exclude serious pathology, especially in individuals with neuropathy.
Answer 3 is incorrect. About 3% of respondents chose this, “Prescribe a topical antifungal for the toenails and instruct JT to inspect feet weekly and apply moisturizing cream.” This addresses a minor issue (onychomycosis), but ignores signs of ischemia and neuropathy.
Finally, Answer 4 is correct. 77% chose this answer, “Recommend vascular imaging and refer to a vascular specialist due to abnormal ABI and diminished pulses.” ABI values <0.9 indicate PAD; values <0.5 are considered severe. Given the ABI of 0.6 and 0.7, along with diminished pulses and gait change, vascular referral is necessary to assess perfusion and prevent future ulceration or amputation.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. This course is free to attend without earning CEs, or you can choose the paid option if you wish to receive CE credits.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Featured Articles
_________________________
Upcoming Programs
___________________________
Free Webinars
___________________________
|
|---|
Happy August!
Greetings, wonderful healthcare colleagues. This newsletter is full of exciting content, important announcements, and new programs.
Did you know that over 30% of HCP taking their CDCES for the first time don’t pass? Not passing can feel very discouraging, but be reassured that this does not define you, and you are not alone. Join our Free webinar on August 26th to regroup, reconfigure, and get re-energized to pass this exam!
AI is becoming an integral part of our everyday life, and for people with diabetes, it may offer significant benefits in helping determine the amount of carbs in food. Our expert delves into this topic, exploring different apps and the potential benefits of AI.
Speaking of carb counting, our next article examines the Beta Bionics insulin pump, which eliminates the need for users to manually enter the carbs they consume. Read more to learn about the ins and outs of this innovative insulin pump.
If you are working toward your CDCES, I encourage you to apply for our DiabetesEd Training Seminar San Diego Scholarship. Two recipients will be awarded the cost of registration ($559) to our fantastic two-day training seminar in October. Applications due August 29th.
You won’t want to miss our newest course, ‘Hyperglycemia and Hot Flashes,’ taught by our guest expert, Dr. Jill Schramm, on August 27th. If you are looking for a reason to go to Hawaii, join Coach Bev in Honolulu in September.
This month, you are invited to join our free webinars on DeFeeting Amputation and Prepping for your CDCES & BC-ADM. Challenge yourself with our Question and Rationale of the Week, Too!
I hope to see you in Phoenix, Booth 527! Stop by and say hello to me and my boys. We can’t wait to meet you!
With appreciation,
Coach Beverly, Bryanna, Tiffany, Christine, & Katarina
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
C.K. is a 55-year-old elementary school teacher diagnosed with type 1 diabetes ten years ago and is managing glycemic control with multiple daily injections (MDI) and a CGM. You are seeing C.K. for diabetes education due to an increasing hemoglobin A1c from 7.0% to 9.9%. During the appointment, C.K. reports missing mealtime doses due to being “too busy to get all that stuff out” at both work and home. C.K. notes that a friend from church has an insulin pump and asks if an insulin pump would help improve their A1c.
As the diabetes care and education specialist, what factors do you need to assess before determining if C.K. is ready for insulin pump therapy?
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. Earn 1.25 CEs/CPEUs or join for FREE!
Register above or simply visit our Online Store at DiabetesEd.net.
For more information or any questions, please email [email protected].
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our Level 4 | The Impact of Adverse Childhood Experiences on Health awards 1.0 CPEUs in accordance with the Commission on Dietetic Registration’s CPEU Prior Approval Program.
All hours earned count toward your CDCES Accreditation Information
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.

Summer offers an excellent opportunity to engage with fresh, seasonal eating and a local farmer’s market offers an ideal starting point for both inspiration and nutrition. In diabetes care, fruit and vegetable consumption are cornerstone nutrition recommendations, yet most Americans don’t get enough.
Increased consumption is associated with diabetes prevention, diabetes management, and reduced risk of cardiovascular and kidney disease. A recent meta-analysis found for individuals with Type 2 Diabetes, an additional 200 grams per day (about 2.5 servings) was associated with a 26% lower risk of all-cause mortality.¹
Despite these benefits, 2019 national data showed adults met only 12.3% of daily fruit recommendations (1.5-2 cups) and 10.0% of daily vegetables recommendations (2-3 cups).² The lowest intakes were found among males for fruit consumption and in individuals living at or below the poverty line for vegetable consumption. Barriers such as cost, limited access, lack of preparation skills, and previous food experiences all contribute to these gaps; however, by supporting access and confidence in use, we can help bridge this gap.
In 2019, I experienced these challenges firsthand while working at a rural health clinic in Northern California serving individuals living with type 1 and type 2 diabetes. While we were making progress using population health strategies to support outreach and engagement, as a dietitian, I recognized we could do more to address food quality and access for our rural community.
A chance conversation at a community health event led to a grant opportunity and the creation of a Fruit and Vegetable Prescription program. Individuals attending diabetes care visits could be eligible to receive farmer’s market vouchers, aligning with the recent launch of a local downtown market. Although the market was not year-round, we saw this as an opportunity to help connect individuals at risk of low intakes with seasonal produce found at farmers’ markets.
Each week, we partnered with farmers to provide recipe cards, seasonal produce challenges, and activities that encouraged trying new foods into traditional meals. Although early outcomes were limited by the onset of COVID the following year, similar programs continue across the U.S.³, with studies suggesting potential long-term benefits for fruit and vegetable intake, food security, and clinical markers linked to diabetes and cardiovascular disease.⁴
In addition to Prescription Programs, several other, currently funded⁵, nutrition assistance programs can help increase food dollars for farmers’ market spending. Many farmers’ markets across the U.S. now accept SNAP/EBT and programs like Market Match, WIC, and the Senior Farmers’ Market Nutrition Program, offering incentives by matching the value of EBT dollars spent on fruits and vegetables. Identifying participating markets in our communities and sharing how individuals can access these benefits may help reduce financial barriers and support more equitable access to fresh, healthy foods.
A helpful resource is the USDA Farmers Market Directory, which allows users to search by zip code for local markets and filter results to show those that accept SNAP or other benefits.
Familiarity, exploring new foods, and obtaining skills for preparation can be another challenge. Tools such as the Seasonal Food Guide offers information by state and month on what produce is in season. Within this guide, you will find links to information on each type of food, including purchasing, storing, and cooking. Fruitsandveggies.org offers resources for health professionals, consumer handouts, information about each fruit or vegetable, seasonal guides, and recipes.
Clients have shared wonderful resources from Tiktok, Instagram, or YouTube for how to cook videos for new foods. Many farmers’ markets have their own pages, which can tell you what is in season at your local market that week. Planning meals and determining what to eat can be one of the most challenging aspects of nutrition management in diabetes. Knowing what is available, exploring meal planning ideas, helping shop with a plan, sharing tips, and engaging with farmers for preparation and storage advice can help build confidence in food selection.
At our local market in Northern California, produce such as berries, cucumbers, zucchini, cherry tomatoes, bell peppers, and leafy greens are plentiful and align well with diabetes nutrition therapy. Berries are high in antioxidants and fiber. Zucchini and cucumbers are hydrating non-starchy vegetables, perfect for raw salads or simple sautéed side dishes. Leafy greens, such as arugula, spinach, and Swiss chard, are rich in vitamins and minerals and pair well with many summer meals.
Ideas for incorporating these foods could include zucchini noodles tossed in pesto or a basic marinara sauce, a cucumber and tomato salad with vinaigrette, a berry and Greek yogurt bowl, or sautéed peppers and greens served with grilled chicken or a bean of choice. When healthcare providers connect individuals to accessible nutrition strategies, they support sustainable, community-based diabetes care that can promote health beyond the clinic walls.
3- Minute Skillet Beans & Greens⁶
Time: 5 minutes, Cook Time: 3 minutes
Servings: 4 (¾ cup each)
Ingredients:
🫒 1 tbsp olive oil
🫘 1 (15-oz) can no-salt-added garbanzo beans (or rinse regular beans), drained
🌶️ 1 tsp curry powder
🌿 ½ tsp ground ginger
🧂 ¼ tsp black pepper
🥬 5 oz fresh baby spinach
🧂 ¼ tsp salt
💡 No spinach? Swap with kale, collard greens, or other leafy greens! (Note: heartier greens will need 2–3 more minutes to cook!)
🔥 Just heat, stir, and enjoy your speedy, healthy, and super tasty dish! 😋✨
Instructions:
-Heat the olive oil in a large skillet over medium heat.
-Add garbanzo beans, curry powder, ground ginger, and black pepper. Stir to coat the beans evenly in the spices.
-Add spinach and salt. Stir gently and cook for about 2½ minutes, or until the spinach is wilted and the beans are heated through.
-Serve warm.
Optional Add-Ins:
-For a saucier dish, add a few spoonfuls of the reserved bean liquid to the pan.
-Add a splash of coconut milk for a creamy, richer version.
Nutrition Facts (Per ¾ Cup Serving):
-Calories: 155, Total Fat: 6g (Saturated Fat: 0.7g), Carbohydrates: 21g (Dietary Fiber: 7g, Sugars: 4g), Protein: 8g, Sodium: 170mg, Potassium: 415mg
For More Information:
-Farmer’s Market Programs: https://www.fns.usda.gov/farmersmarket
-Find a local Farmer’s Market: Local Food Directory https://www.usdalocalfoodportal.com/fe/fdirectory_farmersmarket/
-Seasonal Food Guide: www.seasonalfoodguide.org
-Have a Plant: Fruit and Veggies.org: www.fruitsandveggies.org
References:

Get ready for two days of expert-led, info-packed learning at our in-person DiabetesEd Live Seminar! Whether you’re preparing for your certification exam or looking to sharpen your clinical skills, this intensive event is designed to give you the tools, confidence, and knowledge you need.
💡Ideal for exam prep and clinical refresh
💡 Interactive sessions with real-world applications
💡Network with peers and diabetes care experts
📅 Mark your calendar — October 22–23
📍 San Diego – beautiful location, powerful learning!
Diabetes Education Services has teamed up with Partners for Advancing Clinical Education (Partners) to expand our accreditation offerings.
You can now earn CE credit for the Live San Diego Conference through the following accrediting bodies:

JT is a 58-year-old with type 2 diabetes presents for a routine exam. Has a 20-year history of diabetes, hypertension, and peripheral neuropathy. Reports no foot pain, but partner notes they have been walking with a slight limp. On exam, you note dry skin, thickened toenails, a callus on the plantar aspect of the first metatarsal head, and diminished monofilament sensation at multiple sites on both feet. Pedal pulses are diminished bilaterally, and ABI (Ankle-Brachial Index) is 0.6 on the right and 0.7 on the left.
Which of the following is the most appropriate next step in managing this JT’s foot care?

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting. This course is free to attend without earning CEs, or you can choose the paid option if you wish to receive CE credits.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
For last week’s practice question, we quizzed participants on What best describes the action of GLP-1 Receptor Agonists? 54% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

Question: Which of the following is accurate statement regarding Glucagon Like Peptides (GLP-1)?
Answer Choices:
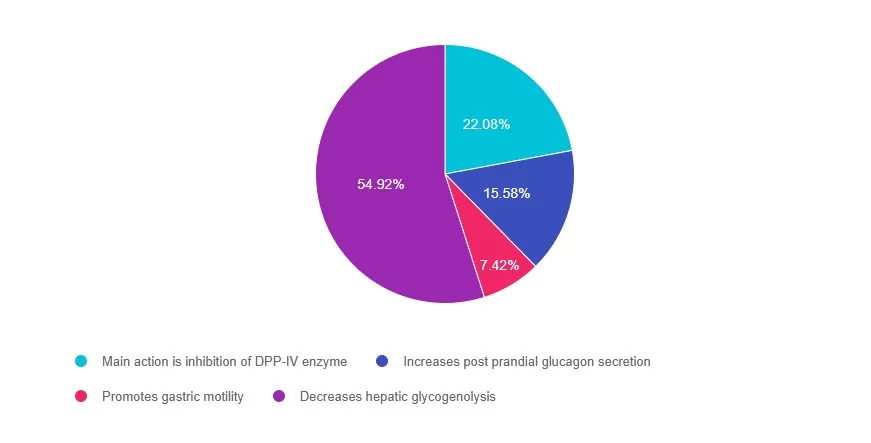
Answer 1 is incorrect. 22% chose this answer, “Main action is inhibition of DPP-IV enzyme.” The GLP-1’s do not inhibit the action of the DPP-IV enzyme (that is the DPP-IV inhibitor class). GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 2 is incorrect. 15% of you chose this answer, “Increases post prandial glucagon secretion.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon, slow gastric emptying and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Answer 3 is incorrect. About 7% of respondents chose this, “Promotes gastric motility.” GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They slow gastric emptying, inhibit the release of glucagon, and stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
Finally, Answer 4 is correct. 54% chose this answer, “Decreases hepatic glycogenolysis.” YES – GREAT JOB! GLP-1 agonists work by activating the GLP-1 receptor found on cells in the pancreas and brain. They inhibit the release of glucagon which decreases hepatic glycogenolysis. They also slow gastric emptying, stimulate insulin production, promote satiety and reduce hyperglycemia in people with type 2 diabetes.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Join us live October 22nd – 23rd, 2025!
30+ CEs with Expanded Accreditation!


Join our expert team for engaging, interactive sessions that bring the ADA Standards of Care to life—covering medications, behavior change, technology, and more. Ideal for CDCES or BC-ADM exam prep, this course also includes a 4-hour Virtual Medical Nutrition Therapy Toolkit and bonus content that also meets CDCES renewal requirements.
Upon completion of this activity, participants should be able to:

Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES

Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Our expert team transforms complex diabetes science into clear, practical insights—keeping it real, engaging, and fun!
Program Faculty Disclosures:
Partners for Advancing Clinical Education (Partners) requires every individual in a position to control educational content to disclose all financial relationships with ineligible companies that have occurred within the past 24 months. Ineligible companies are organizations whose primary business is producing, marketing, selling, re-selling, or distributing healthcare products used by or on patients.
All relevant financial relationships for anyone with the ability to control the content of this educational activity are listed below and have been mitigated according to Partners policies. Others involved in the planning of this activity have no relevant financial relationships.
Faculy Bios & Disclosures:
 Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd Services
Coach Beverly Thomassian RN, MPH, CDCES, BC-ADM – CEO of DiabetesEd ServicesDisclosures:
Beverly Thomassian has no financial disclosures
Bio:
 Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Diana Isaacs, PharmD, BCPS, BCACP, CDCES, BC-ADM, FADCES, FCCPCES
Disclosures:
Dr. Diana Isaacs has the following relevant financial relationships:
Bio:
Diana Isaacs was awarded 2020 ADCES Diabetes Educator of the Year for her educational platform promoting the use of CGM for people with diabetes and other innovations. She serves in leadership roles for several pharmacies and diabetes organizations. She has numerous diabetes publications and research projects with a focus on medications, CGM and diabetes technology.
For the past three year, Dr. Isaacs has served as a contributing author for the 2023 ADA Standards of Care.
As the Program Coordinator and clinical pharmacist specialist in the Cleveland Clinic Diabetes Center, Dr. Isaacs brings a wealth of clinical knowledge combined with extensive research and speaking experience to this program.
Activity Start and End Date: 10/22/25 – 10/23/2025
Estimated time to complete the activity: 15 hours and 30 minutes
_____________________________________
Jointly provided by Partners for Advancing Clinical Education and Diabetes Education Services
![]()
![]()
Joint Accreditation Statement:
 In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
In support of improving patient care, this activity has been planned and implemented by Partners for Advancing Clinical Education (Partners) and Diabetes Education Services. Partners is jointly accredited by the Accreditation Council for Continuing Medical Education (ACCME), the Accreditation Council for Pharmacy Education (ACPE), and the American Nurses Credentialing Center (ANCC), to provide continuing education for the healthcare team.
Physician Continuing Education:
Partners designates this enduring material for a maximum of 15.50 AMA PRA Category 1 Credit(s)™. Physicians should claim only the credit commensurate with the extent of their participation in the activity.
Nursing Continuing Professional Development:
The maximum number of hours awarded for this Nursing Continuing Professional Development activity is 15.50 contact hours.
Pharmacy Continuing Education:
Partners designates this continuing education activity for 15.50 contact hour(s) (1.550 CEUs) of the Accreditation Council for Pharmacy Education.
(Universal Activity Number – JA4008073-9999-25-206-L01-P)
Type of Activity: Application
For Pharmacists: Upon successfully completing the activity evaluation form, transcript information will be sent to the NABP CPE Monitor Service within 4 weeks.
Dietitian Continuing Education:
This program offers 15.50 CPEUs for dietitians.
Interprofessional Continuing Education:
![]() This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
This activity was planned by and for the healthcare team, and learners will receive 15.50 Interprofessional Continuing Education (IPCE) credit for learning and change.
For additional information about the accreditation of this activity, please visit https://partnersed.com.
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
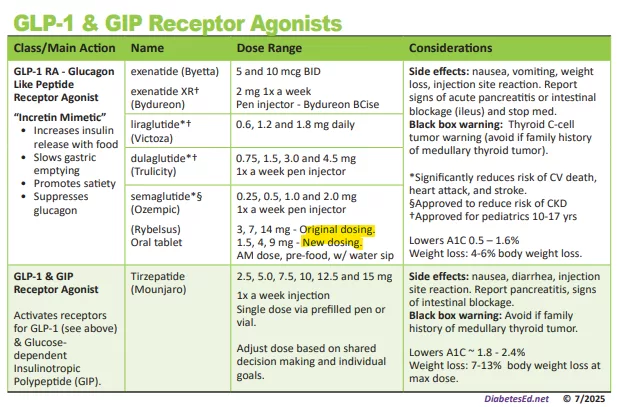
In the world of incretin therapy, there are two important updates for your clinical practice. Staying informed about dosing updates and FDA actions remains essential in this dynamic GLP-1/GIP landscape.
First, the oral version of semaglutide (Rybelsus) now offers two dosing options. In addition to the original R1 formulation of 3, 7 and 14mg, there is now a more conservative R2 dosing formulation of 1.5, 4 and 9mg. This lower dosing option was recently introduced to help reduce gastrointestinal side effects while maintaining efficacy and enabling smoother escalation than the original dosing strategy.
We have updated our FREE Medication PocketCards to reflect this latest information. You can also purchase your own laminated version!
Second, Eli Lilly has launched single dose vials of tirzepatide (Zepbound), to provide more accessibility and pricing options for self-pay individuals who need a safe, less expensive option. This “twincretin” is FDA approved to treat people living with obesity and sleep apnea. Eli Lilly also just announced they will stop production of single dose vials of tirzepatide (Mounjaro) for treatment of diabetes. The Mounjaro pens will continue to be available.
Novo Nordisk’s FDA-approved oral GLP-1 therapy, Rybelsus, now comes in two formulations:
💊 Formulation R1 tablets: 3 mg, 7 mg, and 14 mg
💊 Formulation R2 tablets: 1.5mg, 4mg, and 9?mg
▶️R1: Start at 3mg daily (days 1–30), increase to 7mg (days 31–60); thereafter, remain at 7mg or escalate to 14mg if needed.
🔹R2: Starting dose is 1.5mg daily for 30 days, then increase to 4 mg (days 31–60); after that, maintain 4mg or advance to 9mg based on glycemic control
See Rybelsus Package Insert for more detailed information.
A supplemental new drug application (sNDA) is under review to broaden Rybelsus’s indication to include major adverse cardiovascular events risk reduction in type 2 diabetes patients with cardiovascular or kidney disease. The FDA is expected to rule by October 2025.
Eli Lilly has launched single dose vials of tirzepatide (Zepbound) —a dual GLP-1/GIP agonist approved for obesity and sleep apnea treatment—offering a more accessible and flexible self-pay option.
✅ Affordability: Prices are considerably lower than injector pens, which often cost around $1,000 monthly before insurance
✅ Accessibility: Targets self-pay patients not eligible for insurance or savings programs.
✅ Precision: Enables titration beyond currently approved pen doses; however, it requires self-administration via syringe, increasing complexity and risk of dosing errors.
More info health.com.
⚠️ The FDA continues to crack down on compounded (non-FDA-approved) semaglutide and tirzepatide products due to serious safety reports tied to misdosing and sterility issues.
⚠️ Lilly, in turn, is using its vial rollout and legal action to provide safer, legitimate alternatives to compounding pharmacies.
🫀 Rybelsus: Benefit from the new R2 protocol that eases GI side effects and may soon gain cardiovascular protection indications.
💰 Tirzepatide (Zepbound): Vials offer cost savings and dosage flexibility, but require extra care in administration. Safe sourcing is key
🚫 Market impact: The FDA’s crackdown on compounding and Lilly’s legal and pricing strategies reflect a shift toward ensuring access to approved, reliable options over risky alternatives.
💊 Rybelsus: The new R2 dosing regimen improves tolerability while maintaining efficacy and supports potential future cardiovascular indications.
💸 Tirzepatide (Zepbound) vials: A welcome, lower-cost, flexible injection option—but users must handle dosing themselves and steer clear of unsafe compounded products.

Get ready for two days of expert-led, info-packed learning at our in-person DiabetesEd Live Seminar! Whether you’re preparing for your certification exam or looking to sharpen your clinical skills, this intensive event is designed to give you the tools, confidence, and knowledge you need.
💡Ideal for exam prep and clinical refresh
💡 Interactive sessions with real-world applications
💡Network with peers and diabetes care experts
📅 Save your space today for this unique conference on October 22 & 23rd.
📍 San Diego – beautiful location, powerful learning!
Diabetes Education Services has teamed up with Partners for Advancing Clinical Education (Partners) to expand our accreditation offerings.
You can now earn CE credit for the Live San Diego Conference through the following accrediting bodies: