Welcome New Content Expert – Christine Craig, MS, RDN, CDCES

We are thrilled to welcome our newest member of the Diabetes Education Services faculty and blog team. Winner of the 2023 Impact on Diabetes Award, Christine Craig, MS, RD, CDCES is a leader in the field of nutrition, technology, and diabetes care. Her years of expertise combined with her person-centered approach and work ethic, make her a perfect fit for our company. In addition to writing a monthly blog and question of the week, Christine will also be providing nutrition lectures as part of Diabetes Fundamentals and Boot Camp. We are excited to integrate her fresh perspective and breadth of knowledge into our courses and blog offerings.
On a personal note, Christine loves to adventure. Travel, hiking, and snow skiing are her favorite pastimes. For Christine, having a moment to take in the landscape and beauty around us can re-energize and fuel a busy life.
Learn more about Christine’s approach to diabetes and nutrition education in this brief interview and you can read more about Christine here. Welcome, Christine!
Interview Christine Craig, MS, RDN, CDCES
What advances in nutrition therapy are you excited to explore?
Nutrition is a constantly evolving field that is both a science and an art; we know there is no one-size-fits-all approach. In the science of nutrition, I am excited by the emerging field of precision nutrition, which may give us better insight into an individual’s needs. Precision nutrition uses the complexity of genetics, metabolic profiles, individual microbiomes, wearables, lifestyle, and environmental exposures to better predict an individual’s nutrition needs. This science is still in the very early stages, but the ability to integrate precision nutrition with the art of nutrition has the potential to transform our approach to medical nutrition therapy.
How do you integrate social determinants of health when developing a diabetes management plan?
Developing a diabetes management plan involves finding out about the individual, asking questions, and not making assumptions that you know what is best for the person living with diabetes at that time. Life is complex and managing health can be complex. As a healthcare provider, we can’t always solve structural obstacles, which can feel overwhelming at times. We can, however, through shared decision-making, constant learning, and linking to community resources, develop a collaborative self-care plan that considers the individual’s social determinants of health.
What communication strategies do you find most effective when providing nutrition therapy?
As a dietitian and diabetes educator, I have worked across modalities of care including in-person visits, telehealth, chat-based message communication, and group classes. Like nutrition therapy, there is no one-size-fits-all approach; each person can respond differently to different style types. For me, what has always been effective is using non-judgmental language and open-ended questions. People want to feel heard; this opens the doors to trust and developing an effective nutrition plan.
What do you love most about being a diabetes nutrition specialist?
I love that diabetes care supports health throughout the lifespan, we care for individuals with diabetes over time and at different transition points in their lives. I love that we can walk into work each day and present a breadth of options to support the person living with diabetes or our care teams. I love that I can talk diabetes tech in one moment, nutrition meal planning in the next, and then end my day reviewing coping strategies. This profession is never boring and I love bringing the latest research into my daily practice.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Upcoming webinars | How to Assess Well-Being & Meds Management for Type 2 Diabetes

Be a part of our diabetes community while learning about the latest in diabetes care. Plus, Coach Beverly provides an interactive question and answer session at the end of each live webinar.
Join us for our upcoming Nutrition & Exercise class
Airs live on January 16th, 2023, at 11:30 am PT

Topics:
- Discuss Self-management strategies.
- Listing Nutrition Guidelines for people with diabetes.
- Describe current MNT recommendations.
- List 3 teaching strategies for success.
- State ADA Exercise Guidelines highlights.
- Discuss goals and safety precautions for diabetes and exercise.
This course reviews the latest national nutrition guidelines and provides strategies to translate this information to individuals. We delve into the recent exercise recommendations and provide realistic strategies to help keep individuals active and engaged.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Meds Overview for Type 2
Airs live on January 18th, 2024, at 11:30 am PT

Topics:
- Describe the main action of the different categories of type 2 diabetes medications.
- Discuss strategies to determine the right medication for the right individual.
- List the side effects and clinical considerations of each category of medication.
- State how to use the ADA Medication algorithm to improve care
This course is an introduction to the abundance of medications available to treat type 2 diabetes. We explore the different classes of diabetes medications including action, considerations & side effects. Case studies help students with problem solving & immediate application of this complex topic.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
ADA Standards of Care CE Course
Airs live on February 1, 2024, at 11:30 am PT
Topics:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
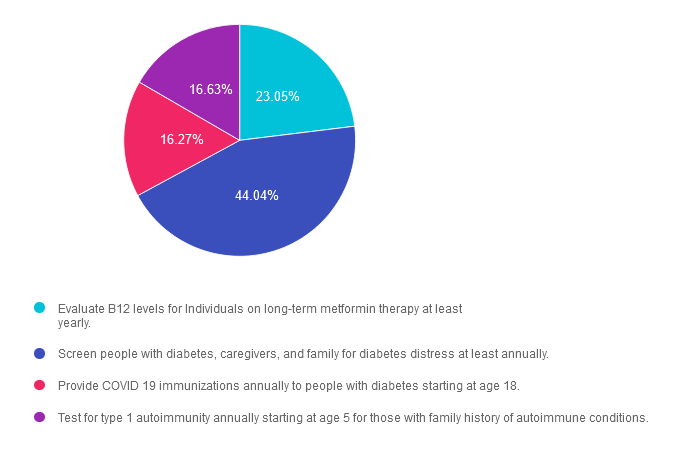
Rationale of the Week | Which is an Accurate 2024 ADA Standard?

For last week’s practice question, we quizzed participants on 2024 ADA Standards. 44% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new ADA 2024 Standards of Care include dozens of updates to diabetes clinical practice.
Which of the following statements has actually been added to the ADA 2024 Standards of Care?
Answer Choices:
- Evaluate B12 levels for Individuals on long-term metformin therapy at least yearly.
- Screen people with diabetes, caregivers, and family for diabetes distress at least annually.
- Provide COVID 19 immunizations annually to people with diabetes starting at age 18.
- Test for type 1 autoimmunity annually starting at age 5 for those with family history of autoimmune conditions.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 23.05% chose this answer. “Evaluate B12 levels for Individuals on long-term metformin therapy at least yearly.” This juicy answer is very tempting. It is true the metformin can be associated with lower B12 levels. However, the ADA does not recommend checking B12 levels annually for people taking this biguanide. Instead, they suggest regularly monitoring B12 levels in people on metformin therapy who have signs of B12 deficiency such as neuropathy or anemia.
Answer 2 is correct. 44.04% of you chose this answer. “Screen people with diabetes, caregivers, and family for diabetes distress at least annually.” Yes, this is the BEST answer! Many individuals with diabetes experience unrecognized and undertreated diabetes distress, which can lead to decreased engagement in self-management activities and worsen outcomes. We address diabetes distress and discuss strategies to address this common emotional response to diabetes in our ReVive 5 Training Program.
Answer 3 is incorrect. About 16.27% of respondents chose this. “Provide COVID 19 immunizations annually to people with diabetes starting at age 18.” The ADA recommends starting COVID 19 immunizations in people with diabetes starting at 6 months and follow-up with boosters as recommended,
Finally, Answer 4 is incorrect. 16.63% chose this answer. “Test for type 1 autoimmunity annually starting at age 5 for those with family history of autoimmune conditions.” Autoimmune testing is recommended for those with immediate family members with type 1 diabetes and other risk factors. There is no age cut-off nor is there a recommendation for annual testing.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
Enroll in our ADA Standards of Care Update
Airs live on February 1st, 2024, at 11:30 am PT
Objectives:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
What’s New for CDCES in 2024?
Important updates for the CDCES exam
If your New Year’s resolution includes getting ready for diabetes certification exams, keep reading!

The Certification Board for Diabetes Care and Education Specialists (CBDCE) has posted a few critical updates on its website regarding CDCES testing blackout dates and an extension of COVID-19 pandemic professional practice requirements. This information will help as you plan your exam dates and work toward acquiring professional practice hours.
Blackout Periods for Application Submission, Scheduling, and CDCES Testing
According to the CBDCE website, to improve the candidate experience, they will be moving to a new application platform in early 2024. Due to this change, there will be specified periods where no applications are accepted, and testing will be closed.
Blackout period for exam application
To accomplish the transition to a new platform, there will be a two-week blackout period from February 9, 2024, to February 27, 2024, when individuals cannot apply for the CDCES exam.
Blackout period for exam application AND testing
In addition, there will be a blackout period where scheduling or testing is unavailable from February 19, 2024, to February 27, 2024.
Please consider this important information as part of your plan to apply, schedule, and take your CDCES exam. We will keep you updated and let you know if any changes occur.
Professional Practice Experience Updates
Starting in 2021, the CBDCE increased the period of time allowed to accumulate professional practice hours from 4 years to 5 years. This additional time allotment addressed the impact of the COVID-19 pandemic on the ability of health professionals to accrue practice experience in diabetes care and education (DCE). The CBDCE also decreased by half the number of diabetes care and education hours required within 12 months prior to taking the application.
The good news is that the CBDCE Board of Directors approved making these initial temporary changes to the professional practice requirement for initial certification to a permanent state (see table below).
According to the CBDCE Website, Professional Practice Experience Requirement Changes are identified
below:
- For applications submitted through 2024*, the minimum DCE experience needed in the prior 12 months is reduced from 400 hours to 200 hours, and
- For applications submitted through 2026**, minimum 1000 hours (or 2000 hours for unique qualifications pathway) of DCE experience needed can be accrued over a longer period of time. The time frame is increased from 4 years from application date to 5 years from application date.
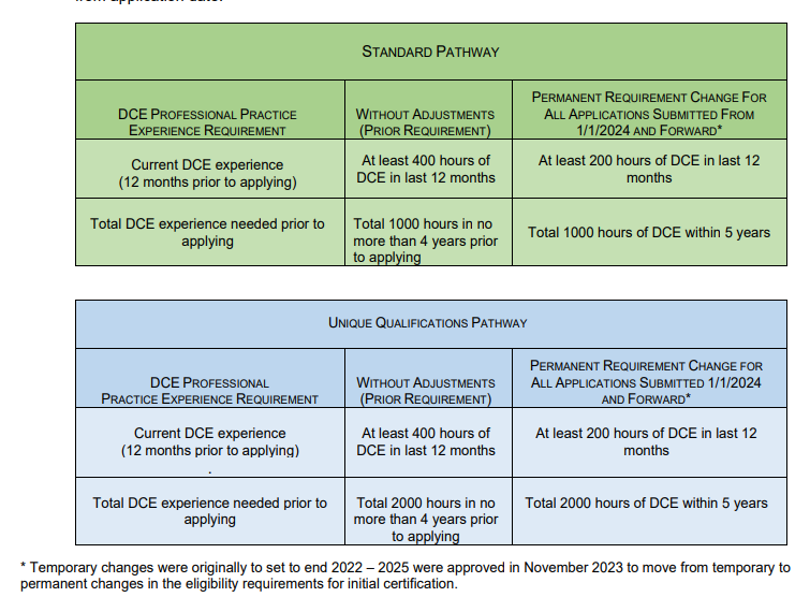
Learn more about changes in the Pandemic Impact Certification Statement or visit CBDCE website.
Plus, you can join our FREE webinar coming up soon (see below)
CDCES Prep with Coach Bev – 2024 Updates | Jan 24 at 11:30 am
Starting your journey to becoming a CDCES? You won’t want to miss our FREE Preparing for CDCES Exam Webinar! This course will transform your test anxiety into calm self-confidence and test-taking readiness. Coach Beverly has taken (and passed) the CDCES exam 7 times and loves sharing her insights on exam success. She will include the latest exam updates with her clear spoken and engaging approach.
A perfect way to kick off your New Year and it’s FREE!
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Question of the Week | Best Hypoglycemia Treatment according to 2024 ADA Standards?
The 2024 ADA Standards of Care includes expanded content on the prevention and treatment of hypoglycemia.
Based on the updated guidelines for the treatment of hypoglycemia, which of the following is true?
- If blood glucose is less than 70 mg/dL, treat with a combination of fast acting glucose and protein to sustain blood glucose levels.
- Avoid use of glucagon emergency treatment for those with type 2 diabetes to prevent rebound hyperglycemia.
- In community settings, check blood sugar to verify hypoglycemia before providing glucagon emergency treatment.
- If individual has one or more episode of clinically significant hypoglycemia, consider short-term relaxation of glucose goals.
Click Here to Test your Knowledge
Want to Learn More About this Question?
Enroll in our ADA Standards of Care Update
Airs live on February 1st, 2024, at 11:30 am PT
Objectives:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting.
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
January 2024 eNews | Happy New Year & 2024 Updates
Happy January

Every year, Coach Beverly excitedly waits for the release of the new ADA Standards of Care. She loves scanning the content pages to discover updates and advances leading to improved diabetes care. She then takes on the task of translating this new information into her presentations, Cheat Sheets, and web content to reflect the latest guidelines.
This first 2024 newsletter features the updated risk screening guidelines and immunization recommendations. We share our library of Cheat Sheets that integrate the new Standards and are ready to download and share with your colleagues and people living with diabetes alike.
For those taking the CDCES exam, we highlight updated information about practice requirements and blackout periods. Plus, we answer the most commonly asked question about the CDCES in our blog.
We invite you to read our interview with Christine Craig, MS, RD, CDCES, nutrition expert, and winner of the 2023 Impact Award. As the newest member of our team, We are excited to integrate her fresh perspective and breadth of knowledge into our blogs, questions of the week, and online presentations.
We encourage you to test your knowledge with our Question and Rationale of the Week.
January kicks off our Level 1 Fundamental Series, followed by our annual ADA Standards of Care update and Level 3 Boot Camp Course Series in February. We hope to see you there!
Here is to a 2024 filled with self-compassion and moments of awe.
Coach Beverly and Bryanna
Featured Articles
- 2024 Standards Cheat Sheets Screening & Vaccine Updates
- Most Commonly Asked Question in January
- CDCES Exam Updates
- Meet Christine Craig, MS, RD, CDCES
- Question of the Week
- Rationale of the Week
- Free Resource Catalog
FREE Webinars & Resources
- FREE Test Taking Practice – Jan 9th
- FREE CDCES Prep – Jan 24th
- Level 1, 2024 Updates
- Level 3, 2024 Updates
- Virtual Conference April 17-19th
- ReVive 5 Training Program
Upcoming Events – See the complete calendar listing
Test-Taking Toolkit
Airs live on January 9th, 2024, at 11:30 am PT

This course facilitated by Coach Beverly will help you transform your nervousness into focused energy that will help you succeed. She will provide test taking tips based on her experience taking the certification exam six times. She will explain how to dissect the question, eliminate wrong answers, and avoid getting lured in by juicy answers.
Plus, the Test Taking Toolkit provides you over 220+ sample practice online practice questions, simulating the exam experience. A perfect way to assess your knowledge and create a focused study plan, while increasing your test taking confidence.
This Test Taking Practice Exam Toolkit is designed to prepare you for exam success. This Webinar includes:
- 90 minute On-Demand course, where Coach Beverly details the content of the exam and test taking tips. Plus, Coach Beverly reviews a sampling of the questions and explains how to dissect the question, eliminate the wrong answers and avoid getting lured in by juicy answers.
- 220 questions in total divided into Four 50+ computerized quizzes. These quizzes include clinical practice exam questions that provide vignette-style situations and other critical content that will prepare you for the actual exam.
Intended Audience: These courses are knowledge-based activities designed for individual or groups of diabetes educators, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in preparing for Certification Exam Success!
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
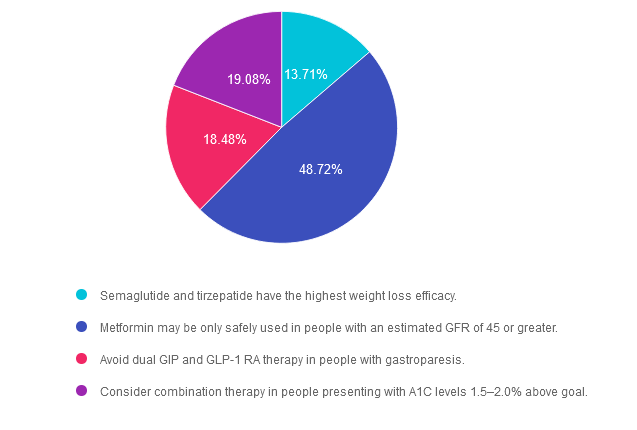
Rationale of the Week | New ADA 2024 Standards – Meds for Type 2 Diabetes

For last week’s practice question, we quizzed participants on the new ADA Standards for type 2 diabetes medication. 49% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Based on the newly released 2024 American Diabetes Association (ADA) Standards of Care, which of the following statements is NOT accurate regarding treatment for hyperglycemia?
Answer Choices:
- Semaglutide and tirzepatide have the highest weight loss efficacy.
- Metformin may be only safely used in people with an estimated GFR of 45 or greater.
- Avoid dual GIP and GLP-1 RA therapy in people with gastroparesis.
- Consider combination therapy in people presenting with A1C levels 1.5–2.0% above goal.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.71% chose this answer. “Semaglutide and tirzepatide have the highest weight loss efficacy.” This statement is accurate. These two incretin mimetics not only substantially lower A1C levels, they also are associated with the highest percentage of weight loss of all the diabetes medications. See Diabetes Med PocketCards for more information.
Answer 2 is correct. 48.72% of you chose this answer. “Metformin may be only safely used in people with an estimated GFR of 45 or greater.” YES, great job! This answer is FALSE (making it the best answer). If a person with diabetes is taking metformin and their GFR drops below 30, then we stop the medication. However, we can start or continue metformin therapy if the GFR is 45 or greater. In addition, metformin doesn’t harm the kidneys, it actually protects them by lowering blood glucose levels. See Diabetes Med PocketCards for more information.
Answer 3 is incorrect. About 18.48% of respondents chose this. “Avoid dual GIP and GLP-1 RA therapy in people with gastroparesis.” This answer is also accurate. Tirzepatide (Mounjaro) can substantially slow gastric emptying which could exacerbate gastroparesis. For that reason, it is not a recommended therapy for people with gastroparesis.
Finally, Answer 4 is incorrect. 19.08% chose this answer. “Consider combination therapy in people presenting with A1C levels 1.5–2.0% above goal.” This answer is also accurate. The ADA Standards of Care recommend more intensive pharmacologic intervention for those with substantially elevated A1C to improve and prolong pancreatic function.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this question?
ADA Standards of Care Course 2024
Airs Live February 1, 2024 at 11:30 AM PT
Topics:
- A review of changes & updates to the annual ADA Standards of Medical Care in Diabetes.
- Identification of key elements of the position statement.
- Discussion of how diabetes educators can apply this information in their clinical setting
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the annual updates to the American Diabetes Association’s (ADA) Standards of Medical Care in Diabetes & provides critical teaching points & content for healthcare professionals involved in diabetes care & education.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.
Question of the Week | Which is an Accurate 2024 ADA Standard?
Which of the following is an accurate new 2024 ADA Standard of Care?
The new ADA 2024 Standards of Care include dozens of updates to diabetes clinical practice. Which of the following statements has actually been added to the ADA 2024 Standards of Care?
- Evaluate B12 levels for Individuals on long-term metformin therapy at least yearly.
- Screen people with diabetes, caregivers, and family for diabetes distress at least annually.
- Provide COVID 19 immunizations annually to people with diabetes starting at age 18.
- Test for type 1 autoimmunity annually starting at age 5 for those with family history of autoimmune conditions.
Click Here to Test your Knowledge
Level 1 | Diabetes Fundamentals
Airs live on January 11th-30th, 2024, at 11:30 am PT
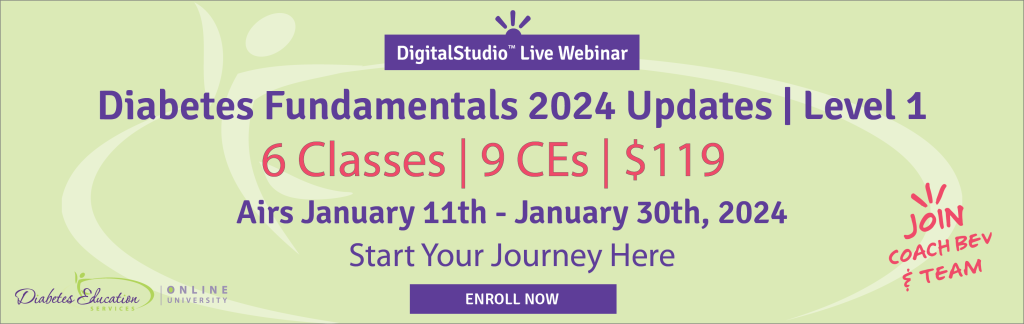
Class Topics & Webinar Dates:
- January 11, 2024 – Class 1: Getting to the Nitty Gritty | 1.5 CEs
- January 16, 2024 – Class 2: Nutrition & Exercise 1.5 | CEs
- January 18, 2024 – Class 3: Meds Overview for Type 2 | 1.5 CEs
- January 23, 2024 – Class 4: Insulin Therapy & Pattern Management | 1.75 CEs
- January 25, 2024 –Class 5: Goals of Care & Lower Extremity Assessment | 1.5 CEs
- January 30, 2024 – Class 6: Hypoglycemia, Sick Days, & Monitoring | 1.5 CEs
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
Accreditation: Diabetes Education Services is an approved provider by the California Board of Registered Nursing, Provider 12640, and our CPEU courses have received Prior Approval* from the Commission of Dietetic Registration (CDR), Provider DI002. Since our CPEU courses received Prior approval* from the CDR, these CPEU courses satisfy the CE requirements for the CDCES /BC-ADM regardless of your profession!
The use of DES products does not guarantee the successful passage of the certification exam. CBDCE and ADCES do not endorse any preparatory or review materials for the CDCES or BC-ADM exams, except for those published by CBDCE & ADCES.