Ready to get certified?
Free CDCES Coach App

Subscribe
eNewsletter
Download
Free Med Pocket Cards
Rationale of the Week | TIR (Time of Range) of 89% – What Is Your Concern?
For last week’s practice question, we quizzed participants on TIR (Time of Range) of 89% , and what is your concern. % of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

JZ is proud of their Time of Range of 89%. You notice their time below range is 7%. JZ uses a rapid-acting insulin pen 4–6 times daily to keep glucose in target range and occasionally increases the glargine dose when evening glucose is elevated.
What is your primary concern?
- Is JZ consistently rotating injection sites to prevent lipohypertrophy?
- What is JZ’s rationale for adjusting the glargine dose?
- How is JZ feeling about their frequency of hypoglycemia?
- Does JZ adjust insulin for physical activity?
Getting to the Best Answer
Answer A is incorrect: % chose this answer, “Is JZ consistently rotating injection sites to prevent lipohypertrophy?” Injection site rotation is important for preventing lipohypertrophy and absorption variability, but not the most immediate safety risk.
Answer B is incorrect: % chose this answer, “What is JZ’s rationale for adjusting the glargine dose?” Basal insulin is generally titrated based on overnight and fasting blood glucose levels, not reactively based on the evening glucose. This is clinically relevant, but still secondary to hypoglycemia risk.
Answer C is correct: % chose this answer, “How is JZ feeling about their frequency of hypoglycemia?” Since JZ is experiencing hypoglycemia more than the target below target range of 5%, we want to explore their feelings around their diabetes and diabetes distress.
Answer D is incorrect: % chose this answer, “Does JZ adjust insulin for physical activity?” Adjusting insulin for exercise is essential for self-management, yet the first priority is identifying whether dangerous lows are occurring.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Learn More From the Experts:
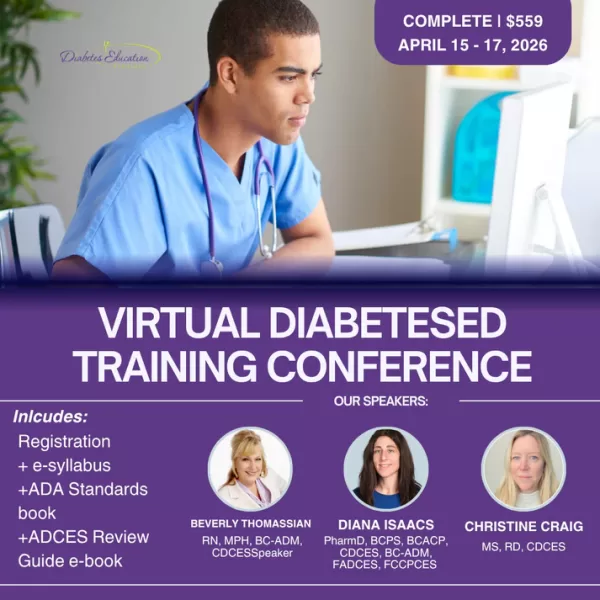
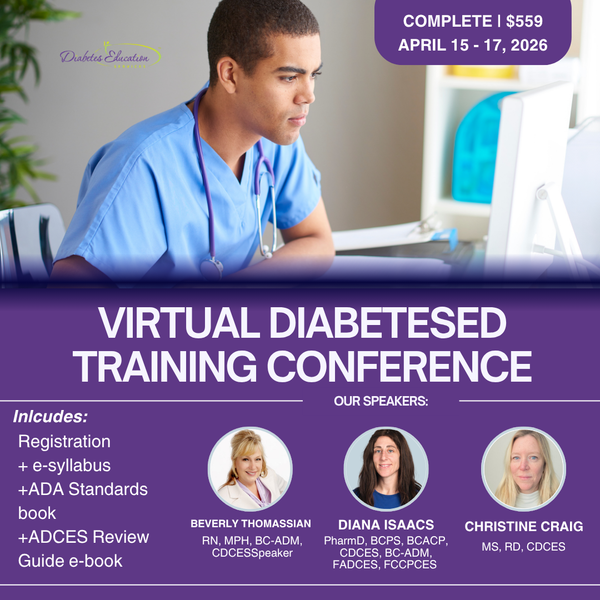
Coach Beverly Thomassian, Dr. Diana Isaacs, & Christine Craig
Virtual DiabetesEd Training Conference
April 15th-17th, 2026
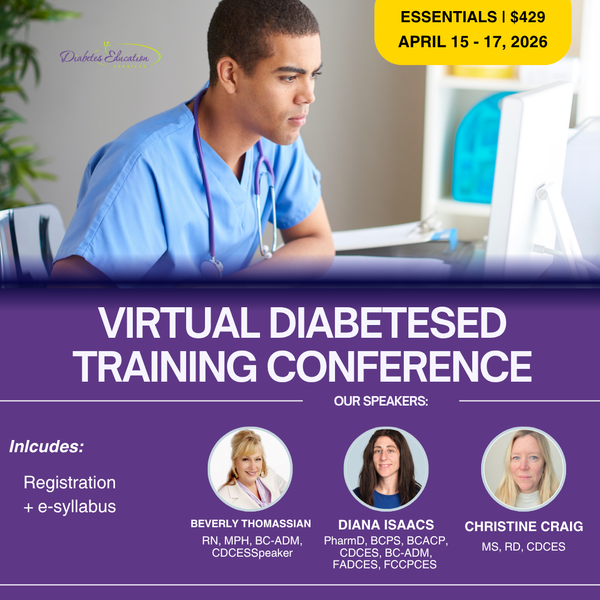
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Keeping You in the Loop: twiist Insulin Pump

Have you heard about the twiist insulin pump? If not, don’t worry – we are here to keep you in the loop! The twiist is the latest automated insulin delivery (AID) system to join the diabetes treatment toolbox. This insulin pump features a unique algorithm powered by Tidepool Loop Technology, offering clients another option in insulin management.
Meet twiist
The twiist is an AID system that looks and acts a bit differently than current insulin pumps. FDA-approved for individuals 6 years old and older, it is a circular-shaped insulin pump. There is a bladder-type reservoir, called a cassette, that holds up to 300 units of insulin. The twiist AID system is currently compatible only with the Libre 3+ continuous glucose monitor (CGM) and iPhone. Meal and correction boluses are delivered via the phone app or Apple Watch for discreet diabetes management. Humalog (insulin lispro) U-100 and Novolog (insulin aspart) are the insulins approved for use with the twiist insulin pump.
iiSure Technology and Tidepool Loop
The twiist AID system uses iiSure technology within the pump and the cassette to dose insulin. Sound waves are used for direct volume measurement to ensure accurate insulin dosing. This feature also identifies occlusions faster than other currently available AID
systems.¹ Insulin moves through the pump chamber into the iiSure chamber, where sound waves use four checkpoints to verify insulin flow and correct dosing:
1. A baseline measurement is taken of the empty iiSure chamber before the insulin reaches this part of the cartridge.
2. The iiSure chamber fills with the determined dose of insulin and is measured for accuracy.
3. A second check of the iiSure chamber is verified for accuracy.
4. After insulin delivery, the pump measures the iiSure chamber to calculate the amount of insulin delivered. ¹ Tidepool Loop is the algorithm that powers the twiist AID system. Tidepool Loop creates a 6-hour glucose prediction forecast based on pump settings, insulin on board, recent carbohydrate entries, and CGM history. This information is collected every 5 minutes to create a 6-hour glucose forecast. Clients using twiist can view this glucose forecast to help make treatment decisions.
How Is twiist Different?
As we have discussed, twiist not only looks different but also functions slightly differently from other AID systems.
Here are a few more unique features:
Target Range: One of the most interesting twiist differences is that the lowest target range setting is 87 mg/dL, with the highest being 180 mg/dL for insulin delivery recommendations.
Retroactive Meal Adjustment: Users can adjust the CHO amount for a meal or snack bolus if they consume fewer carbs than planned.
Emojis: Using meal emojis helps the algorithm set a personalized prediction of food absorption based on carb, fiber, and fat content. If emojis aren’t used, the system defaults to a 3-hour food absorption.
No contracts: The twiist is a pharmacy benefit (rather than a Durable Medical Equipment benefit) and does not require a long-term contract commitment.
Premeal Preset: This option allows the user to temporarily lower the correction range before a meal to help prevent a post-meal glucose spike.
Workout Preset: This optional setting allows for glucose ranges from 87 mg/dL to 250 mg/dL to be set before, during, or after a workout.
Clinical Pearls — With a twiist
Diabetes healthcare professionals are considered experts in insulin pumps. Whether you are discussing insulin pump options, training, or troubleshooting the twiist insulin pump with clients, here are some helpful clinical pearls:
- Assess for physical and cognitive ability to use, manage, and troubleshoot the twiist insulin pump. Also, evaluate clients’ current cell phones or their willingness to change, as twiist can only be used with the iPhone at this time.
- If a user needs to be away from their iPhone, a small button on the pump itself can deliver an insulin bolus.
- The Libre 3+ CGM cannot connect to the Libre family of apps or the reader when using twiist. All CGM alerts will be through the twiist app.
- There are multiple alarms for various conditions. Education is vital to clients about these different alarms for identification and prompt intervention of potential issues.
- The twiist AID system is not safe for MRI, CT scans, x-ray, or any other procedures involving radiation and will need to be removed for these procedures.²
References:
- twiist. (n.d.). iiSure technology: Introducing the next generation of insulin delivery. https://www.twiist.com/iisure-technology#:~:text=Introducing%20iiSure%20Technology,Join%20the%20Insider%20Listhttps://doi.org/10.2337/dc25-S015
- twiist. (n.d.). Support & resources. https://www.twiist.com/twiist-on-support
Learn More From Our Technology Expert:
Dr. Diana Isaacs
During Our Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
Question of the Week | What Do New ADA Standards Say About Development of Type 2?
According to the new 2026 ADA Standards, “type 2 diabetes is associated with insulin secretory defects related to” which of the following?
- BMI and activity level.
- Lifestyle and inflammation.
- Genetics and visceral adipose distribution.
- Epigenetics and metabolic stress.
Learn More About the 2026 ADA Standards
2026 Update Ready to Watch!
Rationale of the Week | What Year ADA Standards Should JR Study?
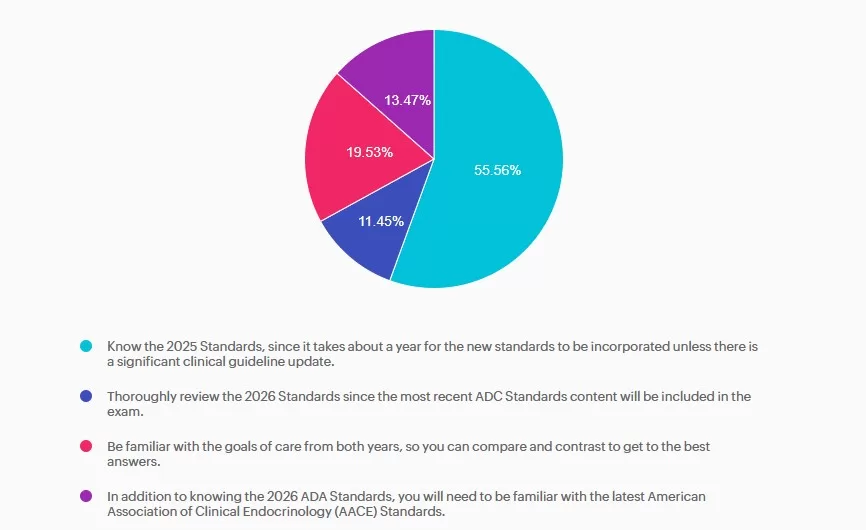
For last week’s practice question, we quizzed participants on JR studying to take their CDCES exam, and they have questions studying for the 2025 or 2026 ADA Standards of Care. 55.56% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

JR has been diligently studying to take their CDCES exam at the end of January 2026. They are wondering if they should study the 2025 or 2026 ADA Standards of Care.
As a mentor to healthcare professionals entering the field of diabetes, what do you recommend?
- Know the 2025 Standards, since it takes about a year for the new standards to be incorporated unless there is a significant clinical guideline update.
- Thoroughly review the 2026 Standards since the most recent ADC Standards content will be included in the exam.
- Be familiar with the goals of care from both years, so you can compare and contrast to get to the best answers.
- In addition to knowing the 2026 ADA Standards, you will need to be familiar with the latest American Association of Clinical Endocrinology (AACE) Standards.
Getting to the Best Answer
Answer A is correct: 55.56% chose this answer, “Know the 2025 Standards, since it takes about a year for the new standards to be incorporated unless there is a significant clinical guideline update.” Answer A is the BEST answer. It takes at least a year for the CBDCE to update the exam based on the ADA Standards. Knowing the 2025 Standards along with any urgent clinical updates announced in 2026 will help prepare JR for success.
Answer B is incorrect: 11.45% chose this answer, “Thoroughly review the 2026 Standards since the most recent ADC Standards content will be included in the exam.” Answer B is not the best answer. Since it takes at least a year for the CBDCE to update the exam based on the ADA Standards, JR can feel comfortable knowing the 2025 Standards along with any urgent clinical updates announced in 2026.
Answer C is incorrect: 19.53% chose this answer, “Be familiar with the goals of care from both years, so you can compare and contrast to get to the best answers.” Answer C is not the best answer. Thinking about comparing and contrasting two consecutive years standards and lead to testing confusion. JR can feel comfortable knowing the 2025 Standards along with any urgent clinical updates announced in 2026.
Answer D is incorrect: 13.47% chose this answer, “In addition to knowing the 2026 ADA Standards, you will need to be familiar with the latest American Association of Clinical Endocrinology (AACE) Standards.” Answer D is not the best answer. Since it takes at least a year for the CBDCE to update the exam based on the ADA Standards, JR can feel comfortable knowing the 2025 Standards along with any urgent clinical updates announced in 2026.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Get Ready For Your CDCES Exam With Our Upcoming Webinars!
Question of the Week | Teens’ A1C climbs after starting CGM
Katie is a 14-year-old living with type 1 diabetes since age 10. She uses multiple daily insulin injections (MDI) therapy to manage her diabetes and started using a continuous glucose monitor (CGM) 3 months ago at the recommendation of her endocrinology team. Her A1c has increased to 9.2% since starting CCM technology.
Her mother reports that Katie has episodes of prolonged hyperglycemia when she is away from home. When at home, her mother will remind Katie to bolus based on the alerts she gets on the CGM share app. Katie reports she mutes alarms and alerts because she doesn’t want her classmates to hear them, afraid they will judge her. When you ask if she has uploaded her data to the school nurse or her endocrinology team she says, “The app is really confusing.” Her mother is frustrated with Katie for not paying attention to the CGM, saying, “She can text her friends without any problem; I don’t know why she struggles with the CGM”.
- Turn on her CGM alarms but increase the high alarm so she doesn’t get as many hyperglycemia related alerts.
- Show her step-by-step how to use the app and how to troubleshoot the alerts and alarms.
- Have the school nurse monitor her CGM trends when Katie is at school, since her mom monitors the CGM trends when she is at home.
- Email Katie’s mother once a week for updates to make sure she is monitoring CGM trends.
Learn more about this Question at our Virtual DiabetesEd Training Conference
April 15th-17th, 2026
Gain fresh insights, practical tools, and a deeper understanding of the latest in person-centered diabetes care. Our expert team brings the ADA Standards of Care to life—covering medications, behavior change, technology, and more!
If you’re preparing for the CDCES or BC-ADM exam, this conference, paired with a handful of free bonus courses, serves as the ideal study companion! Plus, this content counts toward the ADA Standards requirements for CDCES Renewal.
With interactive co-teaching, we keep sessions engaging, relevant, and fun.
Let’s learn and grow together!
Course credits through AMA PRA Category 1 Credits™, ACPE, ANCC, and CDR!
Program Objectives:
Upon completion of this activity, participants should be able to:
- Describe the current ADA Standards for diagnosis, goals, and person-centered diabetes management across the lifespan.
- Demonstrate insulin pattern management and dosing strategies in clinical scenarios.
- Implement timely screening and risk reduction strategies for microvascular and cardiovascular complications.
- Incorporate behavior change techniques and medical nutrition therapy to support people with diabetes self-management and lifestyle adjustment.
December 2025 eNews
Featured Articles ___________________________ |
Upcoming Programs ___________________________
Upcoming FREE Webinars ___________________________ Pre-Order ADA Standards Book for 2026
|
Happy December!💚
Hi friends, we have two pieces of exciting news!
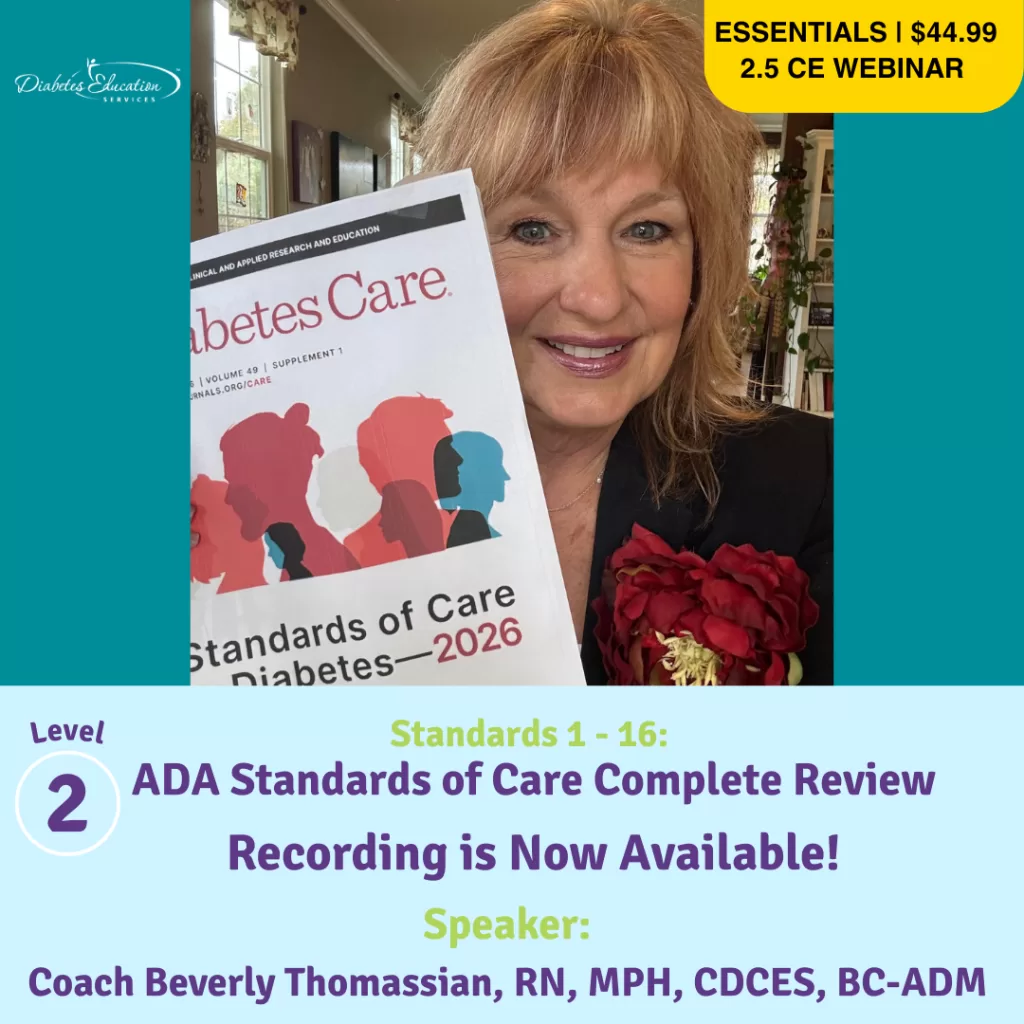
First, the 2026 ADA Standards of Care are here! This updated content is full of evidence-based guidelines and clinical pearls that you can bring back to your practice, prepare for certification exams, and, of course, advocate on behalf of people living with pre-diabetes and diabetes.
As a busy healthcare professional, we understand that you may not have time to read all 350+ pages! We have a solution.
Join Coach Bev on January 29th for a 2.5 CE Live Webinar that summarizes the critical content you need to know. If you can’t join us live, once you register, you have access to the recorded version for a full year.
You can relax as your expert guide, Coach Bev, leads you through a two hour journey highlighting updates to the ADA Standards. You will walk away feeling confident and focused on what’s most important for certification exams and your practice.
Second exciting announcement!
The New CDCES Coach App is NOW available on Apple and Google Play. Best part? It’s still FREE!
After 6 months of renovation (thanks, Bryanna), you are going to love our new and improved CDCES Coach App. Our older version is sunsetting at the end of the month, so download the new version today! Enjoy quick access to the ADA Standards, new sample test questions with rationales, cheat sheets, Question of the Week and more!
Coach Beverly, Bryanna, Astraea & Katarina
Standards Webinar & New CDCES App
New CDCES Coach App - Download Today

Our new, revitalized CDCES Coach app, will equip you with certification exam study tools and clinical resources- right at your fingertips!
✨ Fresh new design with easier navigation.
- Forums to connect with your peers
- Instant access to blogs and news
- Quizzes with rationale
New Quizzes with Rationale for In-app Purchase Option
✨ 25 Practice Test Questions with Rationale – Only $9.99! ✨
📱 Register Today! To take advantage of all these enhanced features, you will need to sign up for the new CDCES Coach App! The old app sunsets on 12/31/2025.
You have been asking for these app improvements. We are happy to deliver new features while keeping your favorite resources at the ready!
- Medication PocketCards, Cheat Sheets
- ADA Standards of Care. Free Webinars
- Study materials
📱 Works on mobile, tablet, and desktop-friendly!
Upcoming Free Webinars & CE Course Series
Rationale of the Week | Storing insulin in work bag?
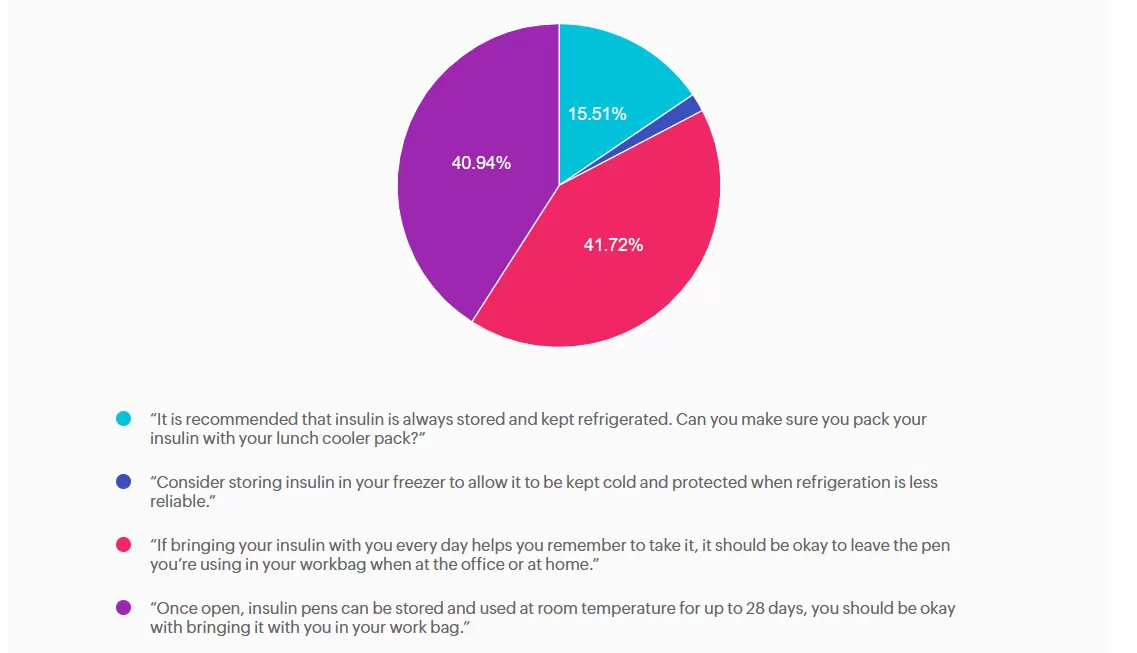
For last week’s practice question, we quizzed participants on SJ having questions about their insulin pen, and what would be the best response. 41.72% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

SJ is 52 years old with a 10-year history of type 2 diabetes. They recently started on insulin degludec U-100 Flex Touch pen 15 units per day. At a follow-up visit, SJ brings their insulin pen and mentions they have been keeping it in their work bag since starting therapy. They are unsure how long they can continue to use this same pen.
What is the best advice for SJ for insulin storage in this situation?
- “It is recommended that insulin is always stored and kept refrigerated. Can you make sure you pack your insulin with your lunch cooler pack?”
- “Consider storing insulin in your freezer to allow it to be kept cold and protected when refrigeration is less reliable.”
- “If bringing your insulin with you every day helps you remember to take it, it should be okay to leave the pen you’re using in your workbag when at the office or at home.”
- “Once open, insulin pens can be stored and used at room temperature for up to 28 days, you should be okay with bringing it with you in your work bag.”
Getting to the Best Answer
Answer A is incorrect: 15.51% chose this answer, “It is recommended that insulin is always stored and kept refrigerated. Can you make
sure you pack your insulin with your lunch cooler pack?” While refrigeration is ideal for insulin storage, insulin does not always need to be refrigerated. Once in use, most insulins, including degludec, are stable at room temperature (below 86F or 30 C). Advising refrigeration may create unnecessary barriers and does not reflect degludec’s stability profile.
Answer B is incorrect: 1.83% chose this answer, “Consider storing insulin in your freezer to allow it to be kept cold and protected when
refrigeration is less reliable.” Freezing damages insulin molecules, making the insulin ineffective and unsafe to use. This option contradicts manufacturer and clinical safety guidance.
Answer C is correct: 41.72% chose this answer, “If bringing your insulin with you every day helps you remember to take it, it should be
okay to leave the pen you’re using in your workbag when at the office or at home.” Insulin degludec is stable at room temperature below 86°F (30°C) for up to 56 days (8 weeks) once opened. If SJ’s work bag is not exposed to excessive heat or freezing, keeping the pen there is acceptable and may in fact support consistent dosing. We can also calculate SJ’s monthly insulin pen usage (15 units per day + 2 unit prime per injection = 510 units per month or 2 pens per month), knowing he will easily use more insulin than open insulin pen stability time window.
Answer D is incorrect: 40.94% chose this answer, “Once open, insulin pens can be stored and used at room temperature for up to 28 days, you should be okay with bringing it with you in your work bag.” While it is correct that insulin does not always require refrigeration once in use, the specific duration varies by insulin type; degludec lasts longer than 28 days.
To learn more, check out our Insulin Storage Cheat Sheet.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
ADA Standards of Care Complete Review 2026
With Coach Beverly - Join us live on January 29th
Course Credits through AMA PRA Category 1 Credits, ACPE, ANCC and CDR
The Power of Medical Nutrition Therapy (MNT)

What is MNT, and how is it beneficial?
Medical Nutrition Therapy (MNT) is effective because it is both
personalized and evidence-based. It can adapt to an individual while being guided by care standards. MNT is defined as a nutrition-based treatment delivered by a Registered Dietitian Nutritionist (or other qualified health professional) for the prevention, treatment and management of medical conditions. It includes nutrition assessment, diagnosis, therapeutic and counseling interventions, monitoring of outcomes, and coordination with care teams. ¹
The nutrition care process can be applied across a wide range of settings, from community, outpatient clinics, hospitals, private practice, long‐term care, telehealth, and more. A recent position paper ², released before publication in the Journal of the Academy of Nutrition and Dietetics, highlighted the effectiveness of MNT in the Prevention and Treatment of Chronic Diseases. They found that despite evidence of the benefit of RDN-delivered nutrition interventions for many chronic conditions, significant
barriers remain in reimbursement, referral processes, and access to care.
Can MNT Be Covered By Insurance?
Coverage for MNT in the United States varies considerably by payer type. Federally, for Medicare Part B, MNT is covered when a beneficiary has diabetes, non-dialysis chronic kidney disease (stage 3-5), or has had a kidney transplant within the past 36 months. A Medicare-enrolled RDN can schedule and bill for services after obtaining a physician signed (MD or DO) referral, at this time mid-level providers currently do not qualify to sign MNT referrals for Medicare benefit. Medicare provides for up to three hours of MNT in the first year of referral and up to two hours in each subsequent year (with allowance for additional hours if deemed medically necessary). ³ As of January 2025, RDNs can also bill for Direct Training Caregiver Services, which means they can provide education and training to unpaid caregivers who help with tasks like meal preparation and wound care. ²
Medicaid programs are financed by both the state and federal governments, but each state can determine its own coverage and
reimbursement for specific services. State Medicaid programs exhibit significant variability in their coverage and reimbursement rates for MNT services. A recent mapping project by the Academy of Nutrition and Dietetics 4 found that while 37 states recognize MNT billing codes, in only 26 states can RDNs enroll as Medicaid providers (one additional state for pediatric services only), and in only 23 states can RDNs bill independently (others can bill incident-to services). Coverage for MNT services also varies, with some limiting depending on the diagnosis to other states providing reimbursement for a broad range of preventive and medical nutrition therapy. 5
Commercial insurance plans also vary widely in their benefit structure, with some limiting coverage while others extending beyond Medicare-covered diabetes and CKD to also include pre-diabetes, obesity, malnutrition, cardiovascular disease (including hypertension and dyslipidemia), cancer, eating disorders, gastrointestinal conditions, and more.
Although some plans have expanded their coverage, it is not universal and understanding coverage requires knowing an individual’s insurance plan benefits, the RDN network status, diagnosis and referral requirements, the number of covered visits/hours/units, medical or preventive benefit coverage, and, if applicable, telehealth eligibility. Benefits can change annually, and reimbursement rates can also vary widely depending on the state and payer.
When the Affordable Care Act was implemented in 2010 it help provide premium subsidies and increased coverage of preventive and chronic disease services. This led to an increase in MNT coverage expectation and waived share-of-cost for individuals receiving MNT. However, in practice, coverage remains patchwork, with substantial variability in approved diagnoses, covered hours, cost-sharing requirements, and provider networks across plans.
Why MNT Is Important
Coordinated care and collaboration are essential for managing chronic conditions, and timely referrals to MNT play a key role in this process. Deciding when to refer should follow disease or area-specific screening criteria (such as validated malnutrition screenings) or as per the Standards of Care in Diabetes, should occur at diagnosis, annually, and whenever treatment goals are unmet, complications develop, or significant life transitions take place. 6
While referral protocols can streamline MNT referrals, access to RDNs remains a challenge in many communities and is further complicated by the need to understand differences in Medicare, Medicaid, and commercial payer coverage so individuals can fully benefit from available services.
How Can I Help?
Healthcare providers can support individuals receiving care by helping them interpret their plan’s benefits, identify coverage barriers (including limited preventive coverage within Medicare and some Medicaid and commercial plans), and connect them to alternative or complementary resources such as Diabetes Prevention or DSMES programs, community health initiatives, or sliding-scale RDN services when MNT is not covered. Providers can also increase their awareness of policy and advocacy efforts to expand MNT benefit eligibility. ⁷ By working together, the entire care team can strengthen care coordination, enhance access to nutrition services, and support the implementation of MNT to improve our population’s health.
References:
- Medical-Nutrition-Therapy. Downloaded from
https://www.eatrightpro.org/career/payment/medical-nutrition-therapy on November 17, 2025. - Moloney L, Rozga M, Steiber A, Handu D, The Effectiveness of Medical Nutrition Therapy in Prevention and Treatment of Chronic Disease: A Position Paper of the Academy of Nutrition and Dietetics. Journal of the Academy of Nutrition and Dietetics. 2025. doi: https://doi.org/10.1016/j.jand.2025.10.010
- CMS: National Coverage Determination. Downloaded from https://www.cms.gov/medicare-coverage-database/view/ncd.aspx?ncdid=252 on November 17th, 2025.
- Mapping Medicaid Coverage for Medical Nutrition Therapy: Why Access Matters. Downloaded from https://www.eatrightpro.org/news-center/public-policy-news/mapping-medicaid-coverage-for-medical-nutrition-therapy-why-access-matters
nutrition-therapy-why-access-matters on November 17th, 2025. - Markus A, Léon C, Blankenship J. Integrating Registered Dietitian Nutritionists’ Medical Nutrition Therapy Benefit Into Existing State Medicaid Coverage and Reimbursement Policy: Results From a Nationwide Medicaid Medical Nutrition Therapy Mapping Project. Journal of the Academy of Nutrition and Dietetics. 2025, SSN 2212-2672. https://doi.org/10.1016/j.jand.2025.08.009.
- American Diabetes Association Professional Practice Committee; 5. Facilitating Positive Health Behaviors and Well-being to Improve Health Outcomes: Standards of Care in Diabetes—2025. Diabetes Care 1 January 2025; 48 (Supplement_1): S86-S127. https://doi.org/10.2337/dc25-S005
- MNT Act. Downloaded from https://www.eatrightpro.org/advocacy/federal-policy-initiatives/all-legislation/medical-nutrition-therapy-act on November 17th, 2025.