Rationale of the Week | C’est la vie with Different Time Zones & Diabetes

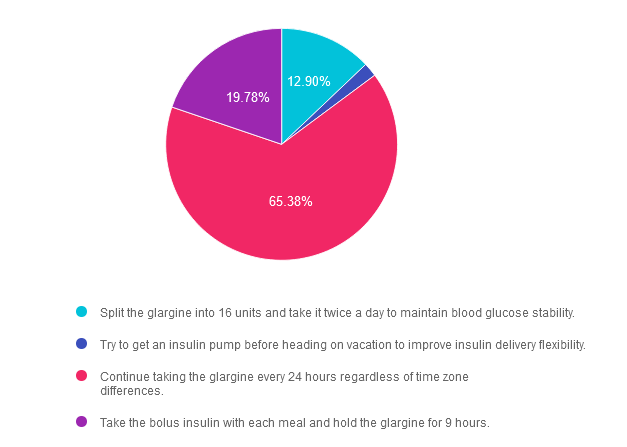
For last week’s practice question, we quizzed participants on living with diabetes & traveling to different timezones. 65% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: BT is heading to the south of France for a 25th wedding anniversary vacation. They usually take 32 units of glargine at 10 PM each night along with 5-7 units of bolus insulin with meals. There is a nine hour time difference between the United States and France.
They ask you how to adjust their basal insulin. What is the best response?
Answer Choices:
- Split the glargine into 16 units and take it twice a day to maintain blood glucose stability.
- Try to get an insulin pump before heading on vacation to improve insulin delivery flexibility.
- Continue taking the glargine every 24 hours regardless of time zone differences.
- Take the bolus insulin with each meal and hold the glargine for 9 hours.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 12.90% chose this answer. “Split the glargine into 16 units and take it twice a day to maintain blood glucose stability.” Although a tempting answer, this action does not address or solve the issue of determining insulin injection timing in a different time zone.
Answer 2 is incorrect. 1.94% of you chose this answer. “Try to get an insulin pump before heading on vacation to improve insulin delivery flexibility.” This approach offers too big of an intervention based on BT’s question of when to dose their insulin in a different time zone.
Answer 3 is correct. About 65.38% of respondents chose this. “Continue taking the glargine every 24 hours regardless of time zone differences.” YES, GREAT JOB. Sometimes the most direct and simplest answer is the best answer. While traveling across time zones, as long as BT takes the basal insulin about every 24 hours and the bolus insulin with meals, they will be able to maintain their usual approach. However, accurate carb counting for French pastries and three course meals is a whole different challenge. : -)
Finally, Answer 4 is incorrect. 19.78% chose this answer. “Take the bolus insulin with each meal and hold the glargine for 9 hours.” The first part of this answer is correct, but the second part isn’t really accurate and it is too vague and confusing to make this answer the best choice. This is a great example of a “juicy answer”.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
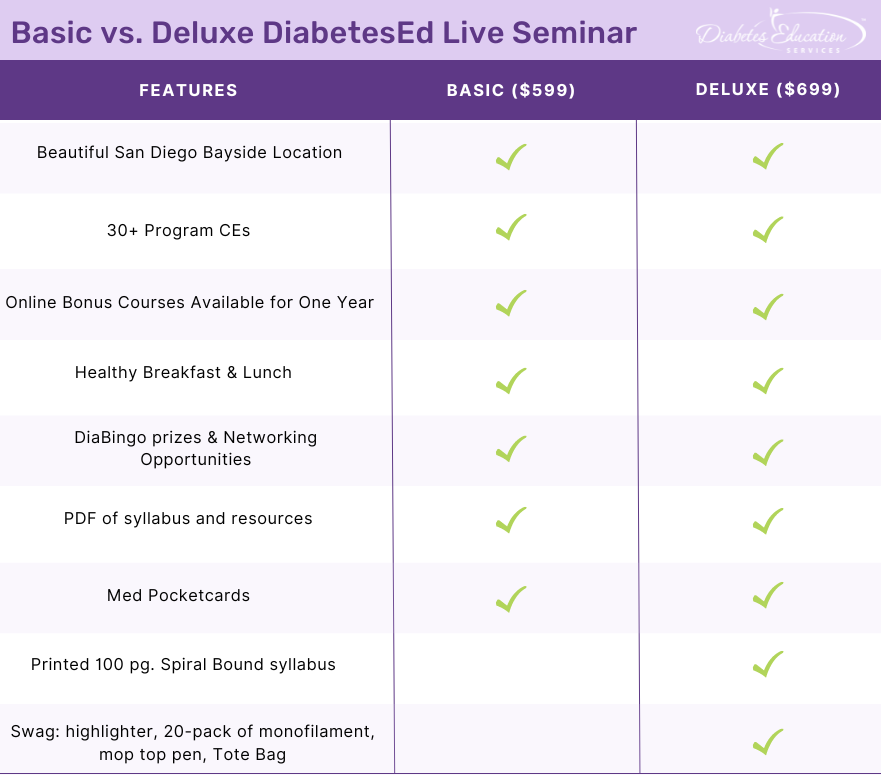
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
Revitalizing Your Diabetes Program or Business – FREE Webinar, Sept 28th

Attending the national ADCES meeting in Houston, Texas, in August was special for me this year. I had a great time presenting on a topic near and dear to my heart: Strategies to Revitalize your Diabetes Program or Business.
This legacy talk allowed me to share actions to innovate, revitalize, and kick-start programs and projects that I have implemented in my practice settings and communities over the past 30 years.
In addition to presenting, I met new diabetes advocates and educators from across the United States, I had the opportunity to connect with old friends, catch up, and share hugs! I also took lots of notes on the presentations, ranging from therapy to stop the progression of type 1 diabetes to the co-relationship between mental health and diabetes.
To celebrate 25 years as the CEO of Diabetes Education Services and 30 years of specializing in diabetes, I am excited to offer my ADCES presentation, Strategies to Revitalize your Diabetes Program or Business for FREE on September 28th at 11:30 am PST. If you are starting a diabetes self-management program or want to revitalize your current practice, we invite you to join this one-hour webinar full of practical tips on advocating for the best health care in a variety of practice settings.
In addition, we will be discussing successful marketing strategies that work. We know that less than ten percent of people with diabetes attend a Diabetes Self-Management Program or see a registered dietitian. Yet, there is ample evidence that people with diabetes experience improved outcomes when receiving DSMES. Plus, the ADA recommends that all people with diabetes receive MNT and DSME regularly. As diabetes healthcare professionals, we need to actively close this gap and increase participant engagement within our communities.
Question of the Week | Why is annual kidney testing so important?
Only about 40% of individuals with diabetes get their kidney function tested annually.
Why is the evaluation of glomerular filtration rate (GFR) and Urinary Albumin Creatinine Ratio (UACR) of critical importance for people with diabetes?
- Evaluate if peritoneal or hemodialysis is necessary for the individual.
- Determine best anti-hypertensive and glucose pharmacotherapy.
- Protect against immune mediated renal complications.
- Slow the progression of chronic kidney disease development.
Click Here to Test your Knowledge
Want to learn more about this question?
FREE Preparing for the BC-ADM Exam Webinar
This course will transform your test anxiety into calm self-confidence and test-taking readiness.
Preparing for the BC-ADM Exam Webinar Topics
- exam eligibility and test format,
- strategies to succeed
- study tips and test-taking tactics
She will also review sample test questions and the reasoning behind choosing the right answers. We hope you can join us.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
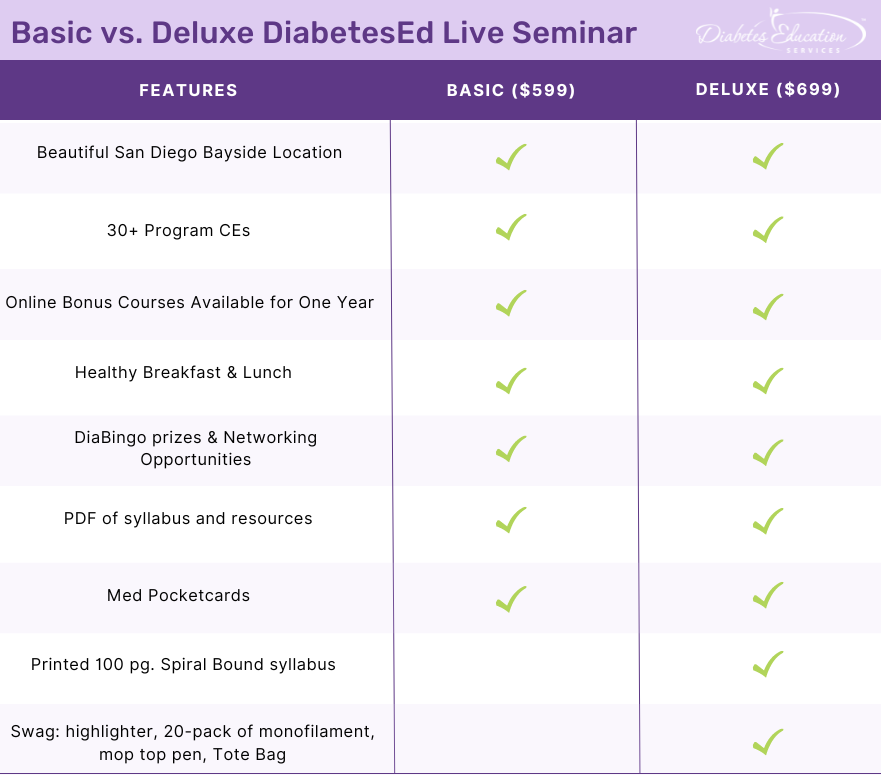
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
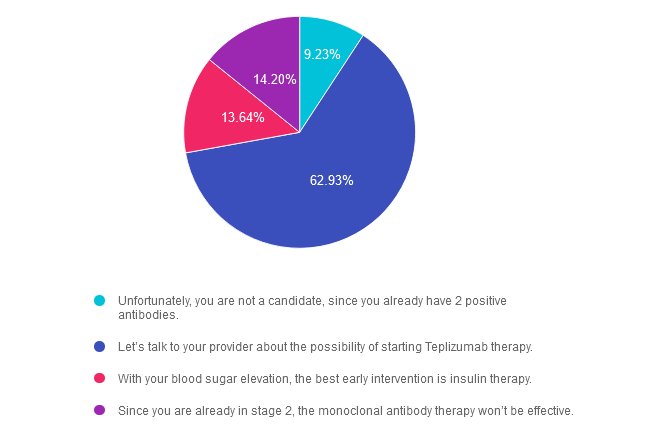
Rationale of the Week | What is best action for stage 2, type 1 diabetes?

For last week’s practice question, we quizzed participants on actions for managing stage 2, type 1 diabetes. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: LT has just been diagnosed with stage 2, type 1 diabetes. They have 2 positive antibodies and their blood sugars are slightly elevated. They ask you if they are a candidate for “that therapy” that can protect their beta cells and slow progression of type 1 diabetes.
What is the most accurate response?
Answer Choices:
- Unfortunately, you are not a candidate, since you already have 2 positive antibodies.
- Let’s talk to your provider about the possibility of starting Teplizumab therapy.
- With your blood sugar elevation, the best early intervention is insulin therapy.
- Since you are already in stage 2, the monoclonal antibody therapy won’t be effective.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 9.23% chose this answer. “Unfortunately, you are not a candidate, since you already have 2 positive antibodies.” Teplizumab IS indicated for the individual in stage 2 type 1 diabetes, or for those with two or more islet autoantibodies and abnormal glycemia but still asymptomatic. People with stage 2 type 1 diabetes, have a nearly 100% lifetime risk of progression to clinical (stage 3) type 1 diabetes and a 75% risk of developing the condition within 5 years.
Answer 2 is correct. 62.93% of you chose this answer. “Let’s talk to your provider about the possibility of starting Teplizumab therapy.” YES, this is the BEST ANSWER, According to ADA Standards, Teplizumab is the first disease-modifying therapy that impedes the progression of type 1 diabetes by binding to the surface of T cells to dampen the unwanted immune system response. It can delay the onset of symptomatic stage 3 type 1 diabetes in adults and children 8 years and older with stage 2 type 1 diabetes (see staging chart). It is administered by intravenous infusion once daily for 14 consecutive days and is expected to cost in the region of $200,000 for the course of treatment. Based on current data, it can delay the expression of stage 3 diabetes by 2 years or longer.
Answer 3 is incorrect. About 13.64% of respondents chose this. “With your blood sugar elevation, the best early intervention is insulin therapy.” Actually, according to ADA Guidelines, LT is a perfect candidate, since Teplizumab IS indicated for the individual in stage 2 type 1 diabetes, or for those with two or more islet autoantibodies and abnormal glycemia but still asymptomatic.
Finally, Answer 4 is incorrect. 14.20% chose this answer. “Since you are already in stage 2, the monoclonal antibody therapy won’t be effective.” Actually, according to ADA Guidelines, LT is a perfect candidate, since Teplizumab IS indicated for the individual in stage 2 type 1 diabetes, or for those with two or more islet autoantibodies and abnormal glycemia but still asymptomatic.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
For more information, see our blog on Teplizumab Therapy to Delay Type 1 Diabetes.
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
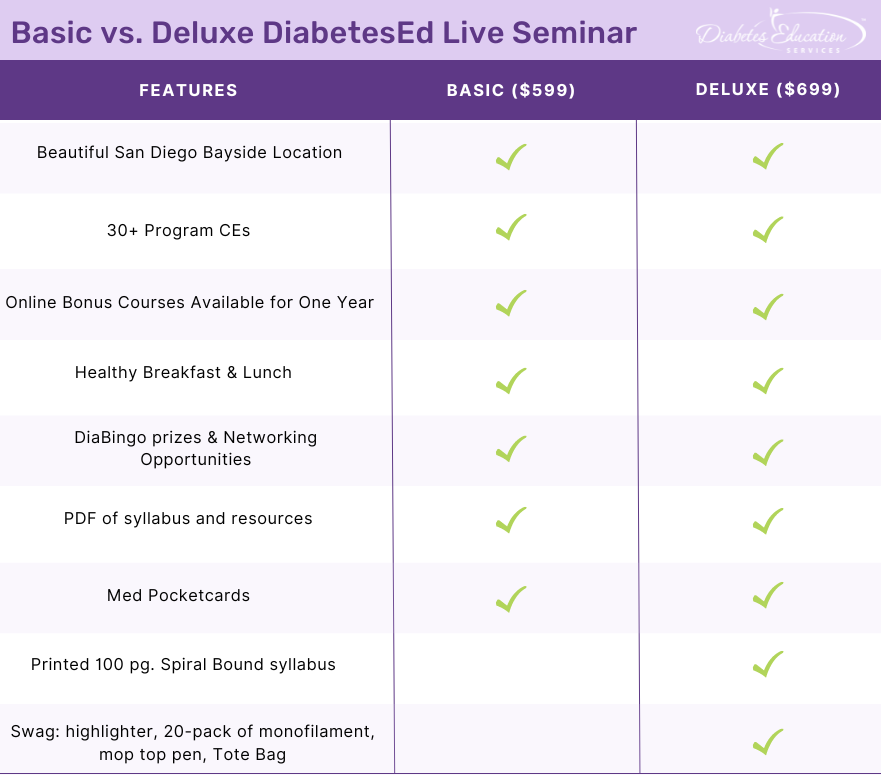
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
Diabetes Drugs & Medicare Negotiations | Diana Issacs, PharmD Breaks it Down

Diana Isaacs, PharmD, BCPS, BCACP, BC-ADM, CDCES is a thought leader in the field of diabetes and has the opportunity to share her expertise as a podcast host, along with colleague Natalie Bellini, DNP, as part of HCP Live and Diabetes Dialogue’s educational series. In a recent program episode, “What Medicare Drug Price Negotiations Mean for Diabetes”, Dr. Isaacs and Dr. Bellini provide an informative and lively discussion on the newly announced Medicare Medication Price negotiation program.
What is this Medicare Drug Hubbub all about?
In order to improve the affordability of medications for those 65 and older with Medicare Part D, the Centers for Medicare & Medicaid Services (CMS), announced the first 10 drugs covered under Medicare Part D selected for negotiation as part of the Inflation Reduction Act,
The drugs chosen include the 10 drugs with the highest gross annual spending total, accounting for $50.5 billion in total Part D gross covered prescription costs per year and more than $3.4 billion in out-of-pocket costs.
Diabetes Medications Included:
There are four diabetes medications included among the ten drugs named for price reductions in this first go-round, which if approved, would take effect in January 2026.
The diabetes agents chosen for negotiation include:
- The SGLT’s empagliflozin (Jardiance) and dapagliflozin (Farxiga)
- An DPP-IV sitagliptin (Januvia)
- and Novo Nordisk-specific insulin aspart products.
In the podcast, Dr. Isaacs and Dr. Bellini, comment on the lack of any GLP-1 or GLP-1 /GIP combo medications in the initial list and are curious about the inclusion of two SGLT-2 inhibitors and no basal insulin. In addition, there was some head-scratching around including insulin in the negotiations, since there is already a $35 Medicare payment cap on insulin therapy.
This group of medications was chosen in part, because according to CMS statistics, these agents accounted for more than $16 billion in total Part D spending from June 1, 2022, through May 31, 2023, which served as the evaluation period for the decision-making process.
As far as when this program will start, negotiated prices for the selected drugs will be announced by September 1, 2024, and those prices will come into effect starting January 1, 2026. The long-term goal is to expand this program as part of the Inflation Reduction Act. By 2027, the goal is to have 15 more medications covered under Part D for negotiation and up to 15 more drugs for negotiation in 2028, including drugs covered under Part B and Part D, and up to 20 more drugs for each year after.
Expect push backs from pharmaceutical companies. Drugmakers have said the new provisions are unconstitutional and have filed a series of lawsuits to try to stop them.
Thank you to hosts Diana Isaacs, PharmD, an endocrine clinical pharmacist, director of Education and Training in Diabetes Technology, and codirector of Endocrine Disorders in Pregnancy at the Cleveland Clinic, and Natalie Bellini, DNP, program director of Diabetes Technology at University Hospitals Diabetes. Click this link to listen to the complete program episode, “What Medicare Drug Price Negotiations Mean
for Diabetes”.
Diana Issacs Speaks for 2 Days in San Diego at our DiabetesEd Specialist Conference – You are invited
If you want to meet Diana in person and benefit from her expert knowledge, she will be co-teaching at our three-day DiabetesEd Specialist Training Program in San Diego on October 11-13th. You won’t want to miss her ADA Standards of Care update, along with her expertise on diabetes medications and her hands-on diabetes technology explanations.
Join Dr. Isaacs & team LIVE in San Diego for our
DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
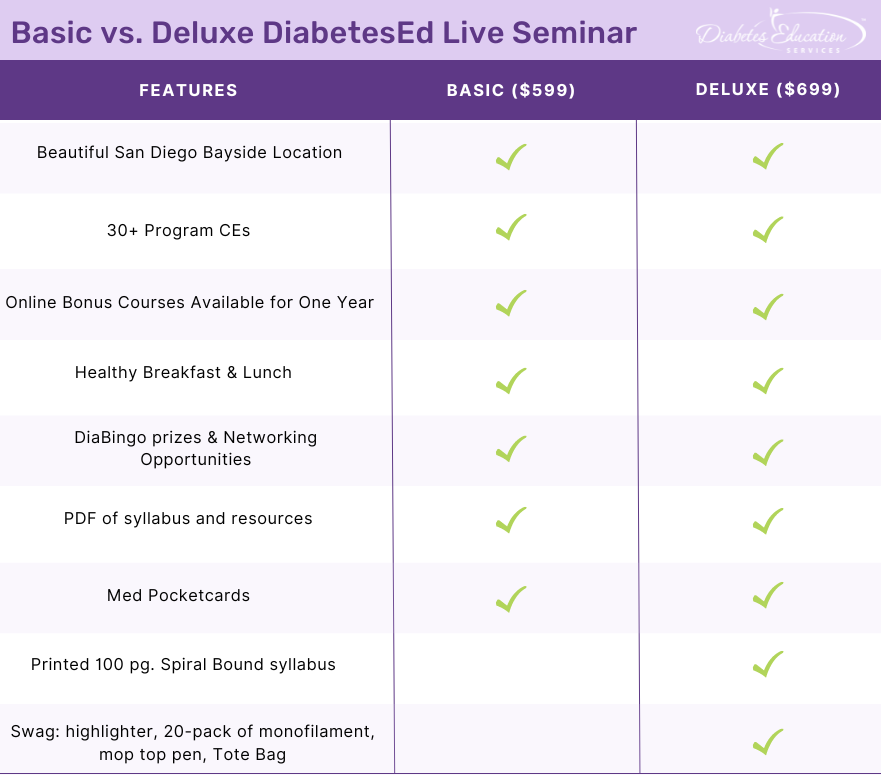
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | C’est la vie with Different Time Zones & Diabetes?
BT is heading to the south of France for a 25th wedding anniversary vacation. They usually take 32 units of glargine at 10 PM each night along with 5-7 units of bolus insulin with meals. There is a nine hour time difference between the United States and France.
They ask you how to adjust their basal insulin. What is the best response?
- Split the glargine into 16 units and take it twice a day to maintain blood glucose stability.
- Try to get an insulin pump before heading on vacation to improve insulin delivery flexibility.
- Continue taking the glargine every 24 hours regardless of time zone differences.
- Take the bolus insulin with each meal and hold the glargine for 9 hours.
Click Here to Test your Knowledge
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
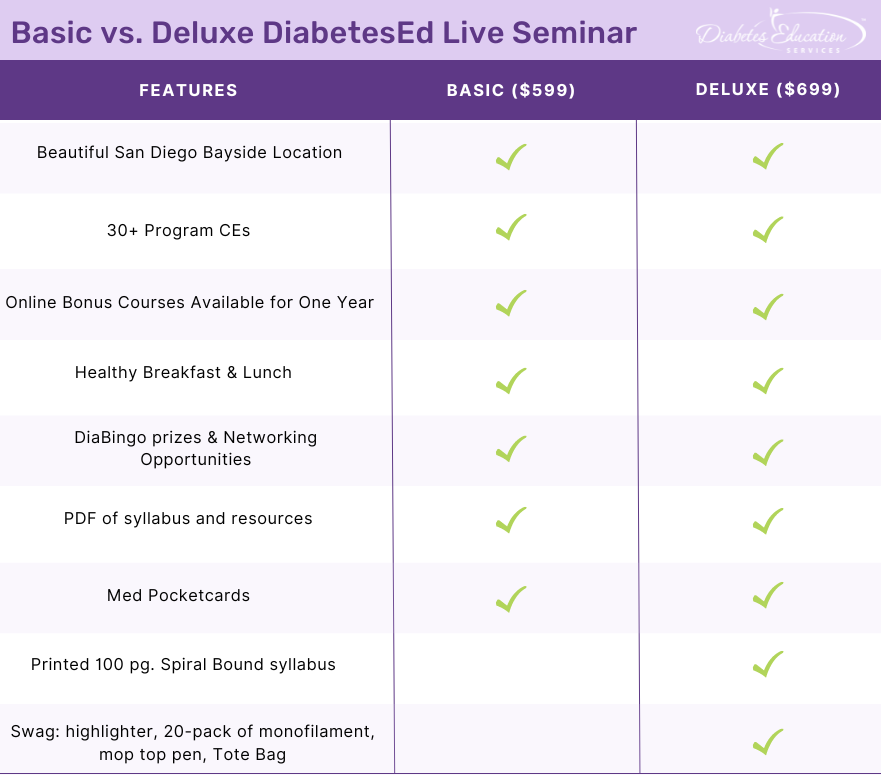
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
September 2023 eNews | Revitalize Your Diabetes Program – New FREE Webinar
Happy September

As temperatures cool and kids head back to school, we begin switching gears to prepare for an exciting line-up of Fall activities.
We are thrilled to offer a brand-new webinar, “Revitalizing Your Diabetes Program or Business,” on September 28th. We are offering this for FREE as part of our ongoing 25-year celebration. Please know that if you can’t join us live, once you register for any of our programs, you will receive a link to the recorded version, usually within 24 hours.
We also invite you to join three FREE webinars we are offering in September. You can pop in for our CDCES or BC-ADM Prep webinars, which Coach Beverly will be broadcasting from her international office in France.
Next, we feature Dr. Diana Isaacs discussing the proposed Medicare (CMS) drug price negotiations designed to make commonly used and expensive medications more affordable. Four of the ten medications outlined are used to treat people with diabetes. You can learn more about this proposal and view a podcast where Dr. Isaacs and Dr. Bellini provide more details in our featured article.
Eating more fruits and vegetables as part of a prescription program improved the health of study participants at over twelve different sites. The goal is to create sustainable, community-based programs that will enhance access to these healing foods for the long term.
After working at Diabetes Education Services for over a decade, my son, Jackson, is kicking off his chemistry studies at UC Berkeley. We sure miss him, but we are excited to cheer him on as he enters this next phase of life. Thank you, Jackson, for your contributions and for recommending Ginger Nichols to continue your legacy.
We invite you to challenge yourself with our question and rationale of the week. We hope you can join our three-day live conference and 25-Year celebration party, cupcakes and swag included, in San Diego.
With gratitude and appreciation,
Coach Beverly and Bryanna
Featured Articles
- Revitalize You Diabetes Program & Business – Sept. 28th
- Diabetes Drugs & Medicare Negotiations
- Fruit & Veggie RX Improves Health
- Jackson Heads to College
- Question of the Week
- Rationale of the Week
- DiabetesEd Training October 11-13, San Diego
FREE Webinars & Resources
- Prep for CDCES FREE Webinar on Sept. 12th
- Prep for BC-ADM Exam FREE Webinar Sept. 14th
- Revitalize Diabetes Program Webinar with Coach Bev, Sept 28th
- New: ADCES Review Guide Book
Upcoming Events – See the complete calendar listing
Join us LIVE in San Diego for our DiabetesEd Training Conference with 4 Hours of Medical Nutrition Therapy
October 11-13th, 2023

Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
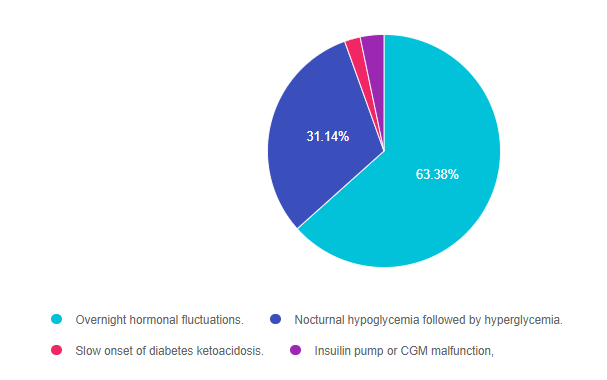
Rationale of the Week | What explains nocturnal hyperglycemia?

For last week’s practice question, we quizzed participants on the effects of nocturnal hyperglycemia. 63% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: JR is 11 years old with type 1 diabetes and their parent shares their concern that the blood glucose seems to be rising overnight with morning hyperglycemia. The parent is worried that JR may be sneaking snacks in the night.
As a diabetes specialist, you know that this glucose rise is most likely due to:
Answer Choices:
- Overnight hormonal fluctuations.
- Nocturnal hypoglycemia followed by hyperglycemia.
- Slow onset of diabetes ketoacidosis.
- Insulin pump or CGM malfunction.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 63.38% chose this answer. “Overnight hormonal fluctuations.” YES, this is the best answer. There is an increased release of counterregulatory and growth hormones during the night, that is especially noteworthy during the teen years. These hormones contribute to insulin resistance and can cause morning hyperglycemia, often referred to as the Dawn Phenomena. For this reason, basal insulin dosing and rates need ongoing adjustment to address this nocturnal insulin resistance.
Answer 2 is incorrect. 31.14% of you chose this answer. “Nocturnal hypoglycemia followed by hyperglycemia.” Even though this phenomena, referred to as Somogyi effect, could cause morning hyperglycemia, there is no information in the test question that indicates JR is experiencing lows over night. Symptoms of hypoglycemia during the night might include; morning headaches, night sweats, vivid dreams or waking up hungry.
Answer 3 is incorrect. About 2.19% of respondents chose this. “Slow onset of diabetes ketoacidosis.” Even though hyperglycemia is associated ketoacidosis, JR has no symptoms of ketoacidosis like lethargy, fruity breath, urine ketones or dehydration.
Finally, Answer 4 is incorrect. 3.29% chose this answer. “Insulin pump or CGM malfunction.” While pump malfunction can lead to hyperglycemia, there is no information contained in the test question that would lead us to believe that JR is using any diabetes technology.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference
October 11-13th, 2023

Two Registration Options
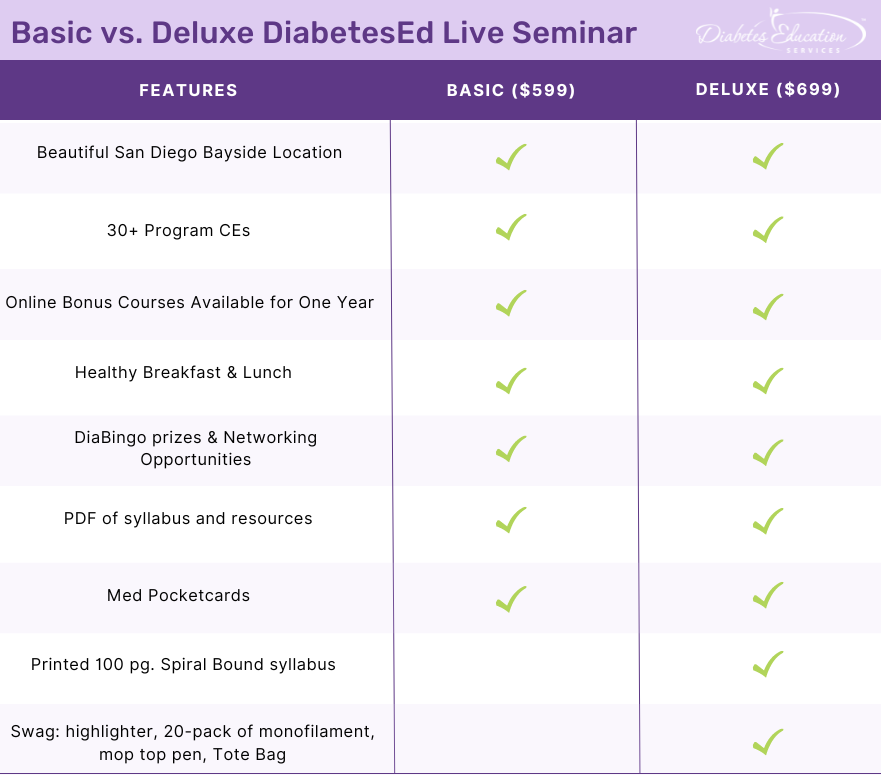
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








