Question of the Week | Preventing Hypo During Exercise
JR has type 1 and tells you they limit their carbohydrate intake to 30 gms a day to prevent hyperglycemia. Their A1C is 6.7% and time in range is over 70%. They tell you their main goal is to figure out how to prevent hypoglycemia during exercise.
What would be the best response using a person-centered approach?
- Explore how they are currently managing blood sugars around exercise.
- Reinforce that glucose needs to be above 100 mg/dL according to ADA Standards to prevent exercise induced hypoglycemia.
- Gently suggest referral to a RD to evaluate actual daily carbohydrate needs.
- Redirect the conversation to evaluate if JR might be experiencing disordered eating.
Click Here to Test your Knowledge
Want to learn more about this question?
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

ReViVE 5 Diabetes Training Program:
Unlocking Hidden Barriers to Diabetes Management
Enroll Now and Save $100!
Recorded & Ready to Watch
Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
- Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
- Susan Guzman, PhD
- Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
FREE Webinars in August with Coach Beverly
Coach Beverly is so excited about celebrating 25 years in business, that due to popular demand, she created a FREE course to de-mystify those complicated and confusing behavior change theories. Our community kept asking for this class and we are ready to deliver! In addition, we are thrilled to offer a FREE webinar designed to DeFEET Amputation, designed for all level of health care providers. Together, we CAN make a difference!
From Behavior Change Theory to hand’s on assessment of lower extremities, diabetes care and education specialists have so much to offer individuals living with diabetes.
Behavior Change Theories Made Easy
Airs live on August 23, 2023, at 11:30 am PT

Join us live on August 23rd from 11:30 am to 12:30 pm for our Free Webinar: Behavior Change Theories Made Easy
Keeping all the behavior change and learning theories straight can be daunting, especially if you are trying to get to the “best” answer for certification exams. Coach Beverly feels your pain and wants to help out. To say thanks for 25 years, she’s hosting a FREE Behavior Change Webinar to sort out and dissect the theories most relevant in clinical practice and for exam preparation.
Objectives:
- Describe 4 of the most common behavior change theories.
- Discuss how to apply these theories in clinical practice.
- List the steps in the transtheoretical model
- Have fun testing these theories out in real life.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Two Ways to Register
Intended Audience: All health care professionals who are coaching individuals to support healthier self-management or who are taking the CDCES or BC-ADM exam.
All hours earned count toward your CDCES Accreditation Information
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
3 Steps to DeFEET Amputation; Assess, Screen, & Report | 1.0 CEs
Airs live on August 10, 2023, at 11:30 am PT

Coach Beverly will walk participants through the 3-Step Process to Save Feet; Assess, Screen, & Report. She will provide simple and clear instructions on how to assess and inspect feet, along with risk assessment & action steps. We will share free teaching tools, strategies, & documentation forms adapted from the Lower Extremity Prevention Program (LEAP) that you can immediately implement in your practice setting.
Objectives:
- Describe steps involved in effective foot assessment made easy.
- Demonstrate how to use a monofilament to assess sensation.
- Discuss the use of screening forms to report findings
Two Ways to Register
Intended Audience: This course is designed for all health care providers and educators, who are interested in learning more about assessing and saving feet in people living with diabetes.
All hours earned count toward your CDCES Accreditation Information
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
All hours earned count toward your CDCES Accreditation Information
On Sale Now – Save $90 on the
ADCES Art & Science Desk Reference 5th Edition
Only a few copies are left! Order now
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Save $50: Art & Science Desk Reference Book | Only a few left!
On Sale Now – Save $50 on the
ADCES Art & Science Desk Reference 5th Edition
Only a few copies are left! Order now
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023

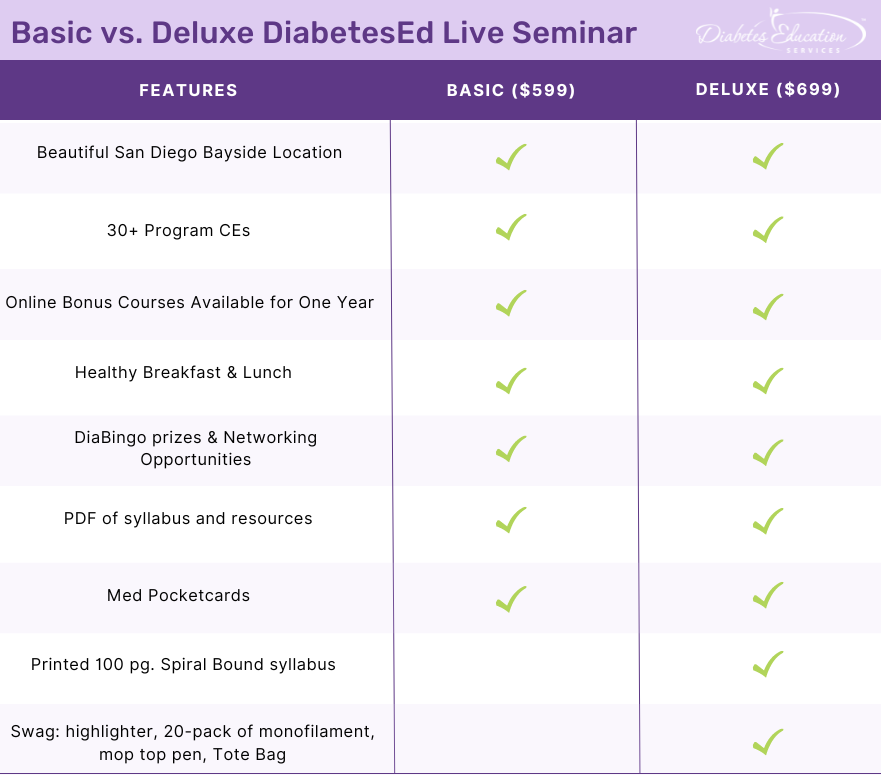
Two Registration Options
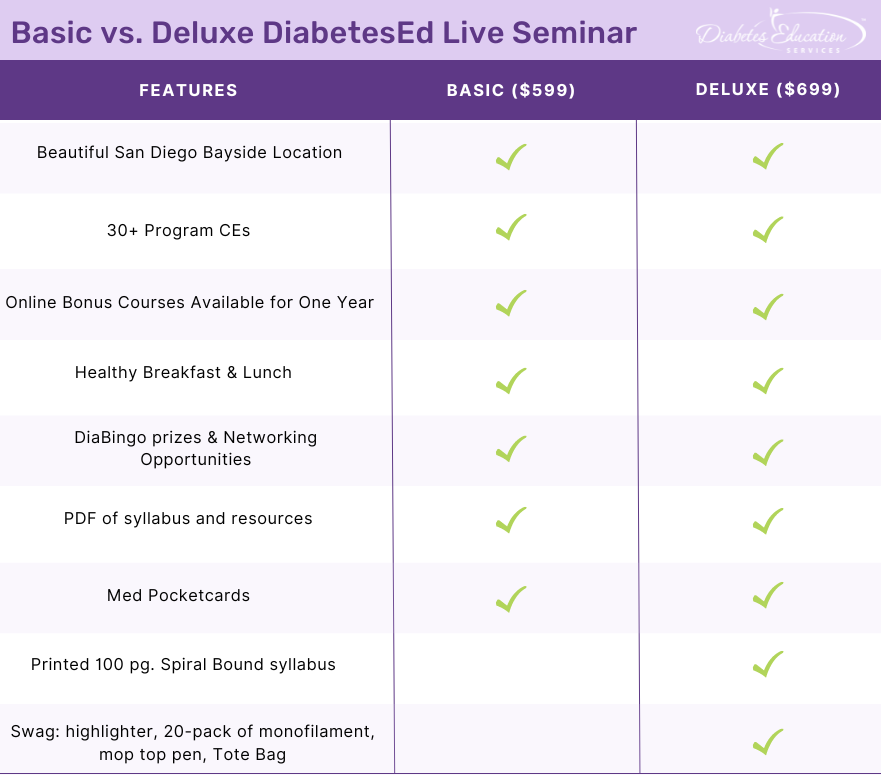
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Rationale of the Week | Give me a Chance to Drop A1C

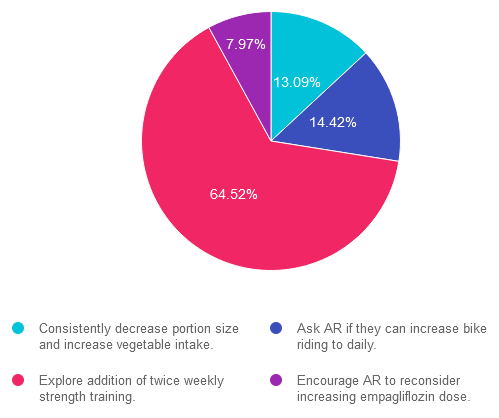
For last week’s practice question, we quizzed participants on getting A1C to goal. 65% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR’s has an A1C of 7.5% and is taking empagliflozin (Jardiance) 10mg daily, plus trying to eat healthy and ride their bike 4-5 days a week for 30 minutes. The provider suggests increasing the empagliflozin dose to 25mg to get the A1C below 7%. AR says that they don’t want to increase their medication dose and says they are dedicated to lowering their A1C through more activity.
Based on this scenario, what ADA recommended activity addition or change would help AR reach their A1C target?
Answer Choices:
- Consistently decrease portion size and increase vegetable intake.
- Ask AR if they can increase bike riding to daily.
- Explore addition of twice weekly strength training.
- Encourage AR to reconsider increasing empagliflozin dose.
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.09% chose this answer. “Consistently decrease portion size and increase vegetable intake.” This juicy answer is tempting, since it addresses portion size and includes more vegetable intake. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
Answer 2 is incorrect. 14.42% of you chose this answer. “Ask AR if they can increase bike riding to daily.” Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Asking AR to increase bike to riding to daily, is not the best approach in this scenario to achieve A1C targets.
Answer 3 is correct. About 64.52% of respondents chose this. “Explore addition of twice weekly strength training.” YES, this is the best answer. Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Studies show that increasing muscle mass significantly lowers glucose and A1C.
Finally, Answer 4 is incorrect. 7.97% chose this answer. “Encourage AR to reconsider increasing empagliflozin dose.” This juicy answer is tempting, since increasing the empagliflozin dose would most likely decrease AR’s blood sugar. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!.
Question of the Week | Post Meal Hypoglycemia
JR has lived with type 1 diabetes for over 30 years and has been complaining that they feel full and bloated after eating and experiencing more post meal hypoglycemia.
Based on this information, what is the most appropriate recommendation for JR?
- Evaluate transglutaminase levels.
- Encourage small, frequent, low fiber meals.
- Suggest a consult for a gastric pacemaker.
- Recommend they try avoiding foods with gluten for a few weeks to see if they feel better.
Click Here to Test your Knowledge
Want to learn more about this practice question?
Join us LIVE in San Diego for our DiabetesEd Training Conference with 4 Hours of Medical Nutrition Therapy
October 11-13th, 2023

Two Registration Options
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
- Diana Isaacs, PharmD, BCPS, BC-ADM, BCACP, CDCES – Educator of the Year, 2020
- Coach Beverly Thomassian, RN, MPH, CDCES, BC-ADM
- Ashley LaBrier, MS, RD, CDCES, Diabetes Program Coordinator
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Renewing Your CDCES? Important Updates you need to know
You passed the CDCES Exam (yay)! Now five years have flown by, you are up for renewal. How do you maintain this hard-earned certification?
This year, the CBDCE published new rules to renew certification which you might have missed. To make sure there are no surprises during your renewal process, here are key considerations from the CBDCE Website that we hope you find helpful!
2025 CDCES Renewal Updates
To promote quality and inclusive diabetes care and education, the CBDCE Board changed the continuing education (CE) content requirements. Certificants will still need to complete 75 CE units over a five-year period. However, to make sure CDCES’s stay abreast of the latest standards and promote inclusive care, the Board is now requiring participation in CE courses that provide updates on the ADA Standards of Care at least twice during the individual’s renewal cycle.
This means that starting in 2023, certificants will need to start acquiring these more specific CEs in preparation for 2025 renewal.
- Required CE Activities now include ADA Standards Update
According to the CBDCE, to successfully renew their CDCES, applicants must participate in CE activities that are focused on the American Diabetes Association’s Standards of Care for Diabetes* two separate times during your renewal cycle.
2. In addition, the following CE Activities are encouraged:
If you are renewing your CDCES in 2025 or later by completing 75 CE units over the five-year period, the CBDCE requires that you demonstrate completion of the following type of CE Activities (you can immediately start accumulating these needed CEs). The CBDCE encourages the following CE activities at least once during your renewal cycle:
- education principals/teaching strategies
- diabetes-related technology;
- leadership/strategy (e.g., CQI, change agent, program development);
- population health; or
- diversity, equity, inclusion, and accessibility (e.g., social determinants of health, cultural competency).
Diabetes Education Services Online University is Here to Help
*Since Diabetes Education Services is Accredited by the Commission on Dietetic Registration (CDR), all of our courses can be applied toward your CDCES Renewal.
Our content incorporates the ADA Standards and Content Requirements
Our Level 2 ADA Standards of Care series, CDCES Basic Prep Bundle, and our new “Everything” Bundle are perfect options for those working toward CDCES renewal requirements. Plus, we update our entire library of content yearly to reflect the latest ADA Guidelines.
In addition, our DiabetesEd Training Programs cover the ADA Standards of Care with clarity and intention by a trio of experts, including Diana Issacs, PharmD, BC-ADM, CDCES, and FADCES a contributing author to the ADA Standards.
Plus, all of our content incorporates education principles and teaching strategies, with a special emphasis on population health, equity, diversity, and inclusion.
We are here to help you succeed. Whether you are starting your journey or working toward recertification, our Standards of Care Intensive, Register Now!, and our new “Everything” Bundle or DiabetesEd Training Conferences are perfect options to meet your goals.
For more information, visit CBDCE Renewal Webpage and/or the current Renewal Handbook for details on the requirements.
Is it Worth all this Work? – YES!
Achieving my CDCES is one of the best and most meaningful investments in professional career! ~ Coach Beverly
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.
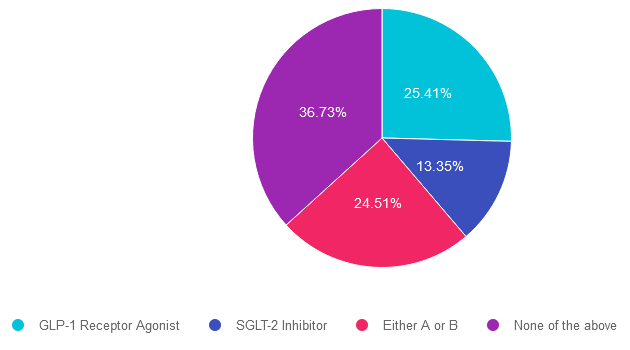
Rationale of the Week | Best Next Step for LR?

For last week’s practice question, over 1,900 participants submitted their answers for how LR could improve glucose while preparing for pregnancy. 37% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: LR is 29 years old, has newly discovered diabetes and polycystic ovary syndrome (PCOS) and is trying to get pregnant. In addition to treating the diabetes and PCOS, LR would like to lose weight. LR was referred to the RD/RDN and encouraged to increase activity level. To treat PCOS and diabetes, LR was started on metformin ER 500mg BID. After a month of treatment, LR’s A1C was still above 8%.
According to ADA Standards, besides increasing the metformin dose, what additional therapy could be added to get LR’s glucose to goal?
Answer Choices:
- GLP-1 Receptor Agonist
- SGLT-2 Inhibitor
- Either A or B
- None of the above
Getting to the Best Answer
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 25.41% chose this answer. “GLP-1 Receptor Agonist.” Given that LR has elevated blood glucose and wants to lose weight, starting a GLP-1 seems like a reasonable idea. However, GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 2 is incorrect. 13.35% of you chose this answer. “SGLT-2 Inhibitor.” Given that LR has elevated blood glucose and wants to lose weight, starting a SGLT-2i seems like a reasonable idea. However, SGLT-2i’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 3 is incorrect. About 24.51% of respondents chose this. “Either A or B.” Given that LR has elevated blood glucose and wants to lose weight, starting either a SGLT-2i or a GLP-1 seems like a reasonable idea. However, SGLT-2i’s and GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, neither class of medication would not be recommended.
Finally, Answer 4 is correct. 36.73% chose this answer. “None of the above.” YES, This is the Best Answer. Metformin is the only non-insulin diabetes medication the ADA recommends for the first trimester of pregnancy. Many people with PCOS are treated with metformin to decrease insulin resistance and ovulation can resume, resulting in pregnancy. The ADA recommends stopping metformin after the first trimester and starting insulin if blood glucose levels remain above target.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
Celebrating 25 Years Sale!!!
Save $100 on our Most Popular Online Programs! Sale ends July 31st!
Prepare for Certification and Earn CEs
ReVive 5 Diabetes Training Program
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.
Save $100! Enroll now to watch the webinar on-demand

Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
CDCES Basic Prep Bundle
30+ Online Courses | 50+ CEs
This bundle is specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus online Technology & Test-Taking Toolkits.
BC-ADM Deluxe Prep Bundle
35 online courses | 50+ CEs
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
This bundle includes our Level 2, Level 3 (Boot Camp), and Level 4, plus online Technology & Test-Taking Toolkits.
NEW: Everything Bundle
40+ online courses | 85+ CEs
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
The next edition of the Review Guide will be released in August. We will be preselling as soon as we get the thumbs up.

This exclusive Everything Bundle provides access to ALL of our Online University Courses and Training Programs. This bundle is perfect for those who need CEs to renew their license or diabetes certification or are looking for a comprehensive update on all topics of diabetes.
Subscribers enjoy over 40 courses taught by Coach Beverly and her team of experts on topics ranging from Diabetes Distress to MNT, Technology to Pattern Management with a focus on providing evidence-based, person-centered diabetes care.
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
All hours earned count toward your CDCES Accreditation Information
ADCES Art & Science Desk Reference
5th Edition
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Question of the Week | Give me a Chance to Drop A1C
AR’s has an A1C of 7.5% and is taking empagliflozin (Jardiance) 10mg daily, plus trying to eat healthy and ride their bike 4-5 days a week for 30 minutes. The provider suggests increasing the empagliflozin dose to 25mg to get the A1C below 7%. AR says that they don’t want to increase their medication dose and says they are dedicated to lowering their A1C through more activity.
Based on this scenario, what ADA recommended activity addition or change would help AR reach their A1C target?
- Consistently decrease portion size and increase vegetable intake.
- Ask AR if they can increase bike riding to daily.
- Explore addition of twice weekly strength training.
- Encourage AR to reconsider increasing empagliflozin dose.
Click Here to Test your Knowledge
Celebrating 25 Years Sale!!!
Save $100 on our Most Popular Online Programs! Sale ends July 31st!
Prepare for Certification and Earn CEs
ReVive 5 Diabetes Training Program
Save $100! Enroll now to watch the webinar on-demand

Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
- 15.0 CEs – Includes the 7-hour ReVive 5 Training Program, Certificate, and 5 FREE bonus courses to supplement content.
- A comprehensive set of assessment tools, educational materials, log sheets, and resources.
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
CDCES Basic Prep Bundle
30+ Online Courses | 50+ CEs
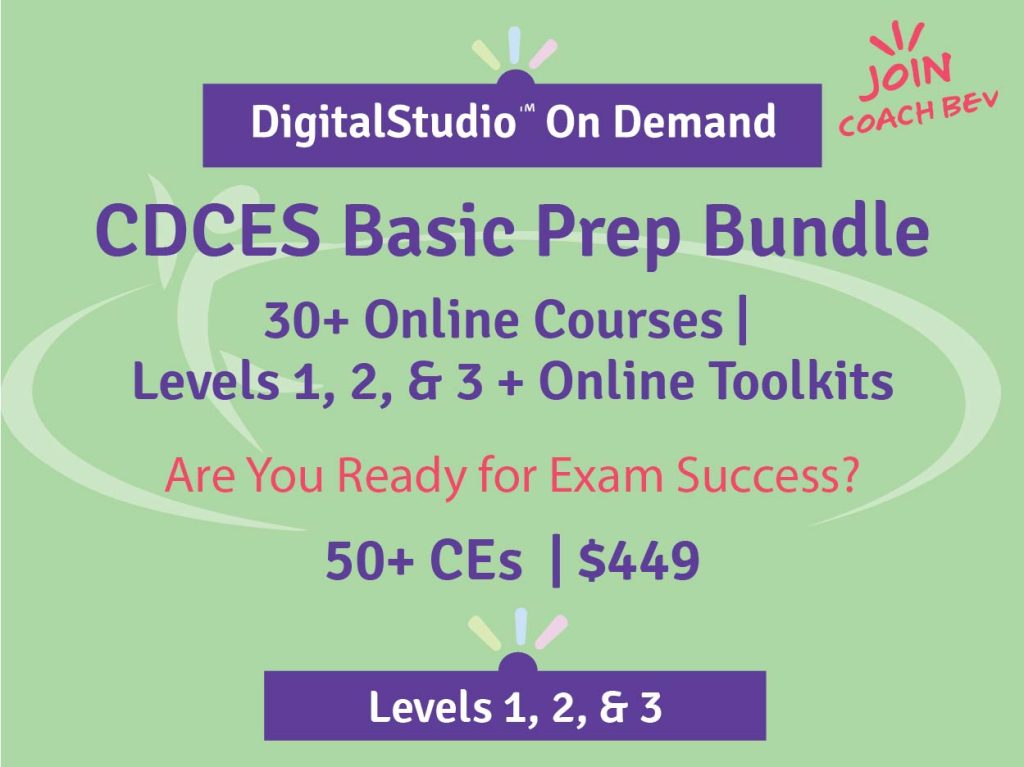
This bundle is specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus online Technology & Test-Taking Toolkits.
BC-ADM Deluxe Prep Bundle
35 online courses | 50+ CEs
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
This bundle includes our Level 2, Level 3 (Boot Camp), and Level 4, plus online Technology & Test-Taking Toolkits.
NEW: Everything Bundle
40+ online courses | 85+ CEs
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
The next edition of the Review Guide will be released in August. We will be preselling as soon as we get the thumbs up.

This exclusive Everything Bundle provides access to ALL of our Online University Courses and Training Programs. This bundle is perfect for those who need CEs to renew their license or diabetes certification or are looking for a comprehensive update on all topics of diabetes.
Subscribers enjoy over 40 courses taught by Coach Beverly and her team of experts on topics ranging from Diabetes Distress to MNT, Technology to Pattern Management with a focus on providing evidence-based, person-centered diabetes care.
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
All hours earned count toward your CDCES Accreditation Information
ADCES Art & Science Desk Reference
5th Edition
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.








