
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.

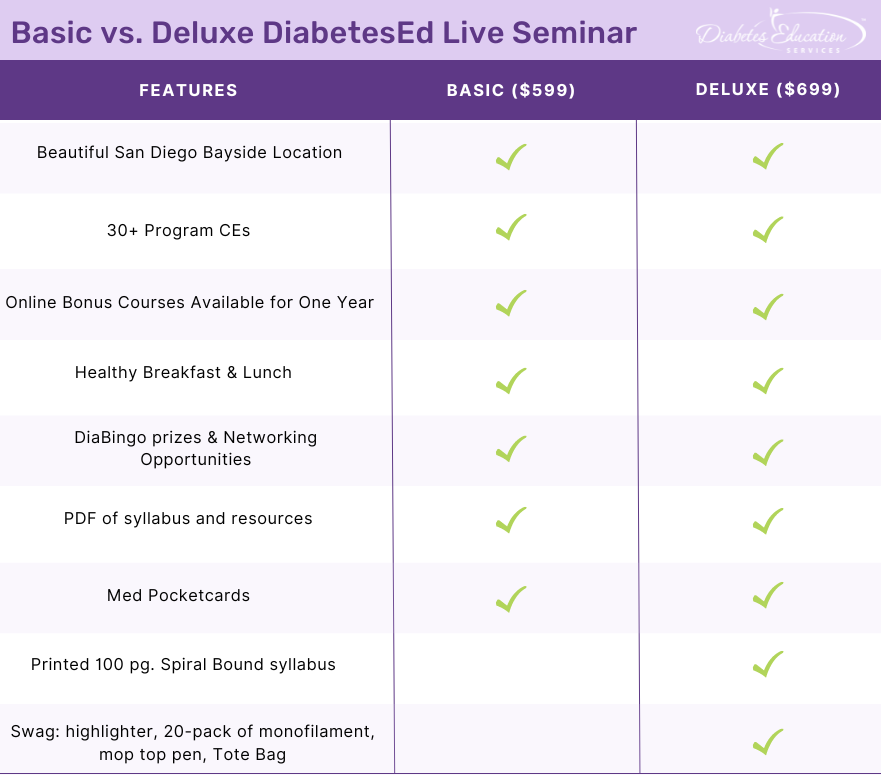
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

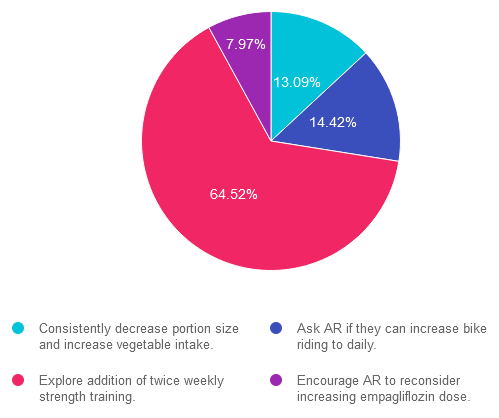
For last week’s practice question, we quizzed participants on getting A1C to goal. 65% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: AR’s has an A1C of 7.5% and is taking empagliflozin (Jardiance) 10mg daily, plus trying to eat healthy and ride their bike 4-5 days a week for 30 minutes. The provider suggests increasing the empagliflozin dose to 25mg to get the A1C below 7%. AR says that they don’t want to increase their medication dose and says they are dedicated to lowering their A1C through more activity.
Based on this scenario, what ADA recommended activity addition or change would help AR reach their A1C target?
Answer Choices:
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 13.09% chose this answer. “Consistently decrease portion size and increase vegetable intake.” This juicy answer is tempting, since it addresses portion size and includes more vegetable intake. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
Answer 2 is incorrect. 14.42% of you chose this answer. “Ask AR if they can increase bike riding to daily.” Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Asking AR to increase bike to riding to daily, is not the best approach in this scenario to achieve A1C targets.
Answer 3 is correct. About 64.52% of respondents chose this. “Explore addition of twice weekly strength training.” YES, this is the best answer. Based on the ADA Standards, individuals are encouraged to maintain 150 minutes of activity a week, plus strengthening activities twice weekly. Studies show that increasing muscle mass significantly lowers glucose and A1C.
Finally, Answer 4 is incorrect. 7.97% chose this answer. “Encourage AR to reconsider increasing empagliflozin dose.” This juicy answer is tempting, since increasing the empagliflozin dose would most likely decrease AR’s blood sugar. However, it is not the best answer since it doesn’t match AR’s stated goal that “they are dedicated to lowering their A1C through more activity.”
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!.
JR has lived with type 1 diabetes for over 30 years and has been complaining that they feel full and bloated after eating and experiencing more post meal hypoglycemia.
Based on this information, what is the most appropriate recommendation for JR?
Click Here to Test your Knowledge

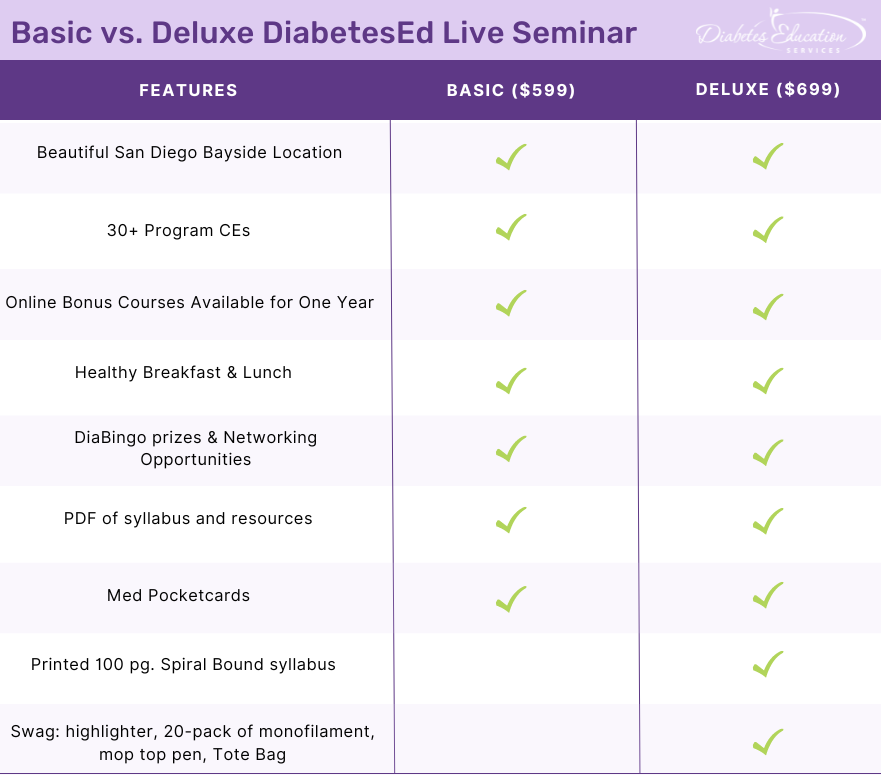
Join Coach Beverly and Team for two and a half days of knowledge-sharing, fun, networking, games with prizes, and “aha” moments in beautiful San Diego.
You don’t want to miss this one-of-a-kind learning opportunity. Get away from all those daily responsibilities and immerse yourself in a fun and intensive conference with plenty of networking opportunities.
Attendees will leave this conference with new tools and a more complete understanding of the latest advances in diabetes care, from medications to technology to Medical Nutrition Therapy!
Bring your colleagues and enjoy our friend discount.
Our team expertly translates the complex science of diabetes into understandable terms while keeping it real, practical, and fun.
Team of expert faculty includes:
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

You passed the CDCES Exam (yay)! Now five years have flown by, you are up for renewal. How do you maintain this hard-earned certification?
This year, the CBDCE published new rules to renew certification which you might have missed. To make sure there are no surprises during your renewal process, here are key considerations from the CBDCE Website that we hope you find helpful!
To promote quality and inclusive diabetes care and education, the CBDCE Board changed the continuing education (CE) content requirements. Certificants will still need to complete 75 CE units over a five-year period. However, to make sure CDCES’s stay abreast of the latest standards and promote inclusive care, the Board is now requiring participation in CE courses that provide updates on the ADA Standards of Care at least twice during the individual’s renewal cycle.
This means that starting in 2023, certificants will need to start acquiring these more specific CEs in preparation for 2025 renewal.
According to the CBDCE, to successfully renew their CDCES, applicants must participate in CE activities that are focused on the American Diabetes Association’s Standards of Care for Diabetes* two separate times during your renewal cycle.
2. In addition, the following CE Activities are encouraged:
If you are renewing your CDCES in 2025 or later by completing 75 CE units over the five-year period, the CBDCE requires that you demonstrate completion of the following type of CE Activities (you can immediately start accumulating these needed CEs). The CBDCE encourages the following CE activities at least once during your renewal cycle:
Diabetes Education Services Online University is Here to Help
*Since Diabetes Education Services is Accredited by the Commission on Dietetic Registration (CDR), all of our courses can be applied toward your CDCES Renewal.
Our content incorporates the ADA Standards and Content Requirements
Our Level 2 ADA Standards of Care series, CDCES Basic Prep Bundle, and our new “Everything” Bundle are perfect options for those working toward CDCES renewal requirements. Plus, we update our entire library of content yearly to reflect the latest ADA Guidelines.
In addition, our DiabetesEd Training Programs cover the ADA Standards of Care with clarity and intention by a trio of experts, including Diana Issacs, PharmD, BC-ADM, CDCES, and FADCES a contributing author to the ADA Standards.
Plus, all of our content incorporates education principles and teaching strategies, with a special emphasis on population health, equity, diversity, and inclusion.
We are here to help you succeed. Whether you are starting your journey or working toward recertification, our Standards of Care Intensive, Register Now!, and our new “Everything” Bundle or DiabetesEd Training Conferences are perfect options to meet your goals.
For more information, visit CBDCE Renewal Webpage and/or the current Renewal Handbook for details on the requirements.
Achieving my CDCES is one of the best and most meaningful investments in professional career! ~ Coach Beverly
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.
**To satisfy the requirement for renewal of certification by continuing education for the Certification Board for Diabetes Care & Education (CBDCE), continuing education activities must be applicable to diabetes and approved by a provider on the CBDCE List of Recognized Providers (www.ncbde.org). CBDCE does not approve continuing education. Diabetes Education Services is accredited/approved by the Commission of Dietetic Registration which is on the list of CBDCE Recognized Providers.

For last week’s practice question, over 1,900 participants submitted their answers for how LR could improve glucose while preparing for pregnancy. 37% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
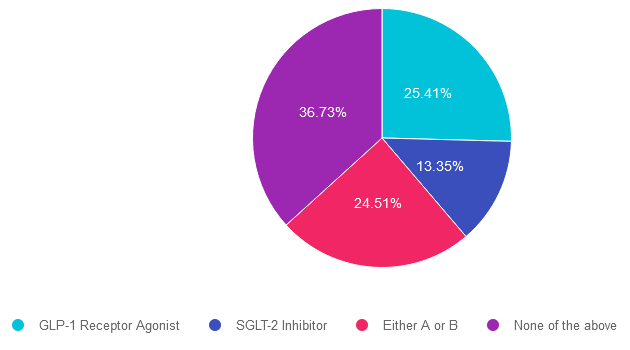
Question: LR is 29 years old, has newly discovered diabetes and polycystic ovary syndrome (PCOS) and is trying to get pregnant. In addition to treating the diabetes and PCOS, LR would like to lose weight. LR was referred to the RD/RDN and encouraged to increase activity level. To treat PCOS and diabetes, LR was started on metformin ER 500mg BID. After a month of treatment, LR’s A1C was still above 8%.
According to ADA Standards, besides increasing the metformin dose, what additional therapy could be added to get LR’s glucose to goal?
Answer Choices:
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is incorrect. 25.41% chose this answer. “GLP-1 Receptor Agonist.” Given that LR has elevated blood glucose and wants to lose weight, starting a GLP-1 seems like a reasonable idea. However, GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 2 is incorrect. 13.35% of you chose this answer. “SGLT-2 Inhibitor.” Given that LR has elevated blood glucose and wants to lose weight, starting a SGLT-2i seems like a reasonable idea. However, SGLT-2i’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, this class of medication would not be recommended.
Answer 3 is incorrect. About 24.51% of respondents chose this. “Either A or B.” Given that LR has elevated blood glucose and wants to lose weight, starting either a SGLT-2i or a GLP-1 seems like a reasonable idea. However, SGLT-2i’s and GLP-1’s are not FDA approved for use during pregnancy. Since LR is trying to get pregnant, neither class of medication would not be recommended.
Finally, Answer 4 is correct. 36.73% chose this answer. “None of the above.” YES, This is the Best Answer. Metformin is the only non-insulin diabetes medication the ADA recommends for the first trimester of pregnancy. Many people with PCOS are treated with metformin to decrease insulin resistance and ovulation can resume, resulting in pregnancy. The ADA recommends stopping metformin after the first trimester and starting insulin if blood glucose levels remain above target.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.

Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
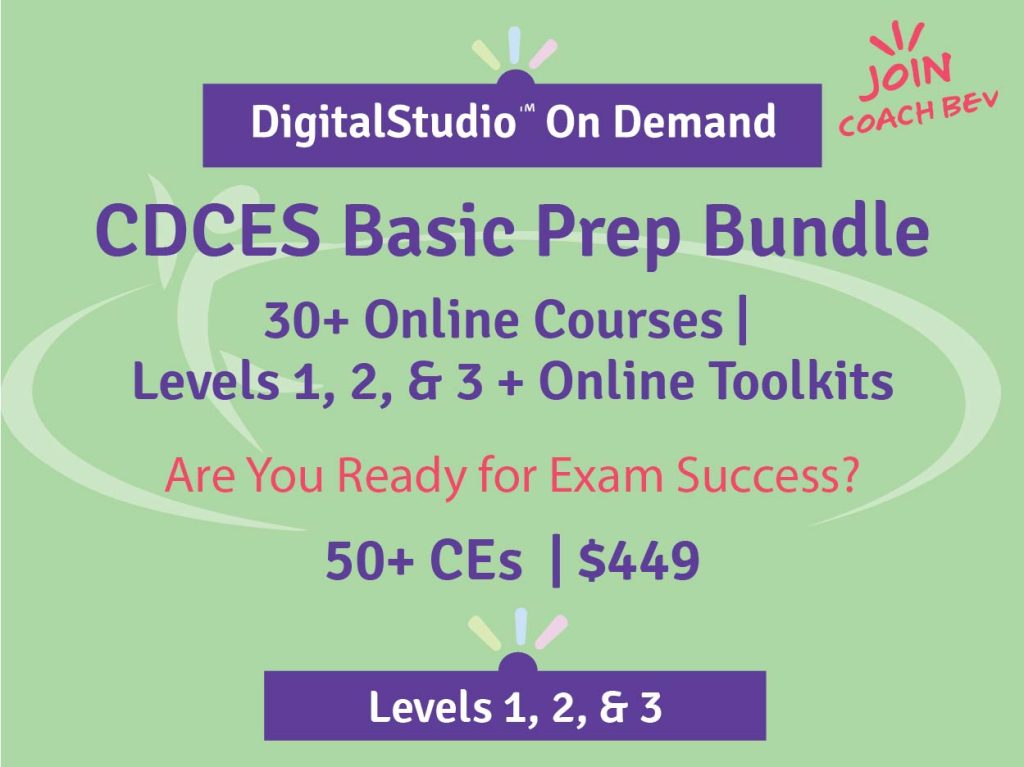
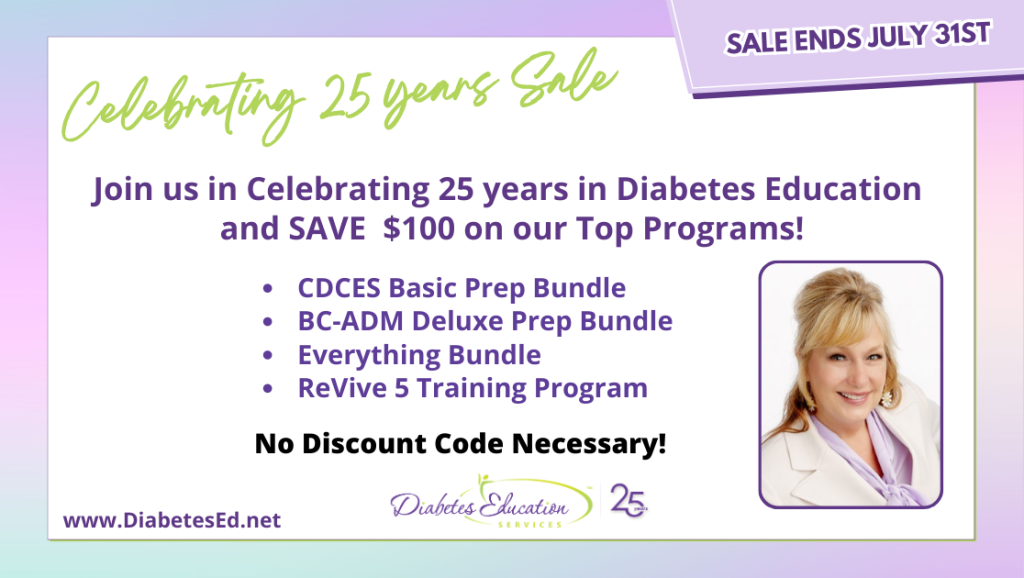
This bundle is specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus online Technology & Test-Taking Toolkits.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
This bundle includes our Level 2, Level 3 (Boot Camp), and Level 4, plus online Technology & Test-Taking Toolkits.
The next edition of the Review Guide will be released in August. We will be preselling as soon as we get the thumbs up.

This exclusive Everything Bundle provides access to ALL of our Online University Courses and Training Programs. This bundle is perfect for those who need CEs to renew their license or diabetes certification or are looking for a comprehensive update on all topics of diabetes.
Subscribers enjoy over 40 courses taught by Coach Beverly and her team of experts on topics ranging from Diabetes Distress to MNT, Technology to Pattern Management with a focus on providing evidence-based, person-centered diabetes care.
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
All hours earned count toward your CDCES Accreditation Information
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
AR’s has an A1C of 7.5% and is taking empagliflozin (Jardiance) 10mg daily, plus trying to eat healthy and ride their bike 4-5 days a week for 30 minutes. The provider suggests increasing the empagliflozin dose to 25mg to get the A1C below 7%. AR says that they don’t want to increase their medication dose and says they are dedicated to lowering their A1C through more activity.
Based on this scenario, what ADA recommended activity addition or change would help AR reach their A1C target?
Click Here to Test your Knowledge

Addressing diabetes distress can be challenging, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Lawrence Fisher, Ph.D., ABPP, Professor Emeritus, UCSF
Susan Guzman, PhD
Beverly Thomassian, RN, MPH, CDCES, BC-ADM
Accredited Training Program:
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
This bundle is specifically designed for healthcare professionals who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus online Technology & Test-Taking Toolkits.
This bundle is specifically designed for healthcare professionals who are studying for the Board Certified in Advanced Diabetes Management (BC-ADM) exam.
This bundle includes our Level 2, Level 3 (Boot Camp), and Level 4, plus online Technology & Test-Taking Toolkits.
The next edition of the Review Guide will be released in August. We will be preselling as soon as we get the thumbs up.

This exclusive Everything Bundle provides access to ALL of our Online University Courses and Training Programs. This bundle is perfect for those who need CEs to renew their license or diabetes certification or are looking for a comprehensive update on all topics of diabetes.
Subscribers enjoy over 40 courses taught by Coach Beverly and her team of experts on topics ranging from Diabetes Distress to MNT, Technology to Pattern Management with a focus on providing evidence-based, person-centered diabetes care.
The first person who purchases our Everything Bundle wins our last copy of the Diabetes Review Guide 5th Ed.
All hours earned count toward your CDCES Accreditation Information
The ADCES (formerly AADE) Art and Science of Diabetes Care and Education, 5th Edition is a specialist’s one-volume, go-to resource for the core knowledge and skills for providing person-centered care and education to persons with diabetes and related chronic conditions. This is a core resource for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
ADCES will be releasing an updated edition of the Art & Science Desk reference in August 2023
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
Like many seasoned diabetes educators, I used to worry that I wasn’t “teaching” enough during my initial one-hour individual assessment. Over time, I realized that listening to and acknowledging the persons’ feelings about diabetes distress and their living situation was the most critical part of this interview process. This initial meeting provides a vital opportunity to make a meaningful connection and start the long-term collaborative problem-solving process.

In addition, according to researchers on the seven sources of distress, the most significant are feelings of powerlessness, followed by management, hypoglycemia, and eating distress.
Good news! The findings from the EMBARK Trial presented at the American Diabetes Scientific Session in June validated the effectiveness of this whole-person approach. The EMBARK study results demonstrated that providing education, combined with careful listening and attunement to the emotional side of diabetes, significantly decreased diabetes distress.
Coach Beverly Participated in EMBARK Trial
I was asked to participate in the EMBARK Trial as a diabetes educator. My role was to provide a three-hour informational online program for a cohort of people with type 1 diabetes. In addition, I provided six to eight 20-minute individual sessions with this same cohort over the next few months. In this study, my role was not to answer clinical questions or make insulin adjustments. Instead, I provided “coaching” to help the individuals discover their own best answers to make needed adjustments.
Participating in this study opened my eyes to a new approach to diabetes education and gave me permission not to know all the answers. The truth is that individuals with diabetes hold the solution in themselves. Our most important job is to help them with the process of self-discovery. The EMBARK Trial provided guidelines and tools for diabetes educators, so we had a clear framework for providing effective coaching.
ReVive 5 Program Shares Strategies that worked in EMBARK
After we completed the study, the lead researchers on this trial, Dr. Lawrence Fisher and Dr. Susan Guzman, reached out to see if we could take the information learned from the EMBARK Trial and create a comprehensive CE program for healthcare professionals. One year later, we launched the ReVive 5 Program to share the steps involved in providing whole-person education and increasing comfort and confidence in addressing emotions. Our next ReVive 5 program starts July 19th, and we would love to have you join us.
More About the EMBARK Trial
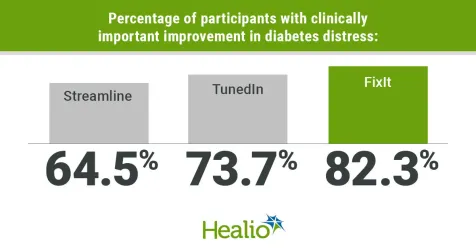
The EMBARK study was a randomized controlled trial that compared three diabetes distress interventions: Streamline, which was a diabetes educator-led program focused on education and management; TunedIn, which was a psychologist-led program focusing exclusively on the emotional side of diabetes; and FixIt, which integrated elements from the Streamline and TunedIn programs. All sessions were held virtually in groups of eight to 12 adults and occurred over 3 to 4 months. Sessions included initial workshops, one-on-one phone calls, and follow-up group meetings.
There were reductions in diabetes distress with all three interventions, with Streamline participants having a reduction in score of 0.48 points, TunedIn participants reporting a 0.59-point decrease and FixIt participants having a 0.88-point decrease. The reduction in diabetes distress for FixIt participants was greater than what was observed in Streamline (P = .005).
According to lead researcher, Danielle Hessler Jones, PhD, “We feel that these findings suggest that these distress reductions are greatest when interventions integrate education alongside a focus on the emotional side of diabetes.”
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.

Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Accredited Training Program:
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.

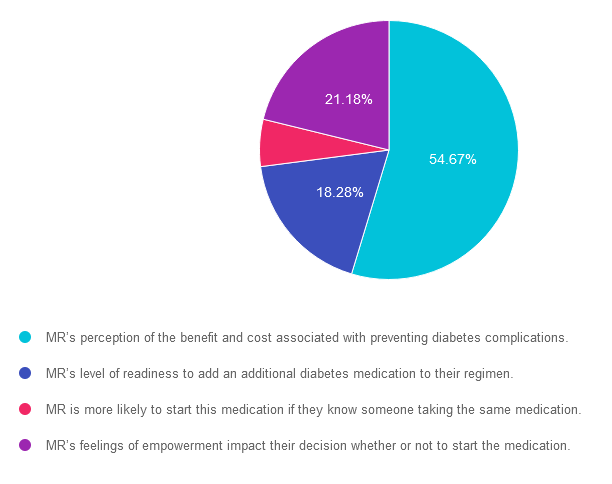
For last week’s practice question, we quizzed participants on person-centered care. 55% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question: MR has an A1C of 9.6% and is deciding whether or not to start another diabetes medication to help lower their glucose. MR’s parent had diabetes and severe complications due to chronic hyperglycemia.
What would best describe the application of the Health Belief Model in this situation?
Answer Choices:
If you are thinking about taking the certification exam, this practice test question will set you up for success. Test writers anticipate possible answers based on the details in the question. They will wave those “juicy answers” right under your nose. Your job is to weed through the particulars, pluck out the most important elements and choose the BEST answer.
Answer 1 is correct. 54.67% chose this answer. “MR’s perception of the benefit and cost associated with preventing diabetes complications.” GREAT JOB. The Health Belief Model (HBM) focuses on individual beliefs and perceptions about health-related behavior change. It suggests that behavior change is influenced by an individual’s perception of the severity of a health problem, their susceptibility to it, the benefits of behavior change, and the barriers or cues to action. In other words it looks at the cost-benefit of a given situation.
Answer 2 is incorrect. 18.28% of you chose this answer. “MR’s level of readiness to add an additional diabetes medication to their regimen.” This answer actually refers the Stages of Change (transtheoretical) Model: This model proposes that individuals go through a series of stages when changing behavior: precontemplation, contemplation, preparation, action, and maintenance. It suggests that people move through these stages in a cyclical manner and that interventions should be tailored to each stage.
Answer 3 is incorrect. About 5.88% of respondents chose this. “MR is more likely to start this medication if they know someone taking the same medication.” This answer reflects the Social Cognitive Theory (SCT): This theory emphasizes the reciprocal interaction between personal factors (such as cognition and self-efficacy), environmental factors, and behavior. It suggests that behavior change is influenced by observing others (social modeling), self-regulation, and the belief that one can successfully perform the behavior (self-efficacy).
Finally, Answer 4 is incorrect. 21.18% chose this answer. “MR’s feelings of empowerment impact their decision whether or not to start the medication.” This answer refers to the empowerment model which is a theoretical framework that focuses on empowering individuals or communities to take control of their own lives and make informed decisions. It emphasizes the importance of promoting autonomy, self-efficacy, and participation in decision-making processes. The empowerment model is often applied in various fields, including social work, community development, healthcare, and education.

Learning behavior change theories and getting to the best answer for certification exams can be tricky. To say thanks for 25 years, Coach Beverly is going to host a FREE Webinar where she dissects common learning theories that are not only helpful for your clinical practice, but also for exam preparation.
Join her August 23rd at 11:30 am PT. For live webinars, Coach Beverly stays after class to answer any lingering questions you may have on the topic.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
“ReVive 5 Program is the best program I have ever attended – should be required for all diabetes educators! Thank you so much for translating this research into practical approaches!!” – Sarah F.

Addressing diabetes distress can be tricky, even for seasoned healthcare professionals.
We invite you to attend this hands-on training program that provides the essential steps to address diabetes distress combined with an innovative approach to glucose management. Our experts offer realistic strategies to address diabetes distress that you can immediately apply to your practice setting. Plus, the ReVive 5 Program provides a breadth of tools and resources to create more meaningful connections with people with diabetes.
Team of Experts: ReVive 5 is taught by a team of 3 Interdisciplinary Experts:
Accredited Training Program:
“ReVive 5” breathes new life into our relationship with diabetes, bringing a fresh perspective to both the person with diabetes and the provider.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the diabetes certification exams. CBDCE & ADCES does not endorse any preparatory or review materials for the certification exams, except for those published by CBDCE & ADCES.