
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards

eNewsletter

Free CDCES Coach App
Free Med Pocket Cards

Medical Nutrition Therapy (MNT) is effective because it is both
personalized and evidence-based. It can adapt to an individual while being guided by care standards. MNT is defined as a nutrition-based treatment delivered by a Registered Dietitian Nutritionist (or other qualified health professional) for the prevention, treatment and management of medical conditions. It includes nutrition assessment, diagnosis, therapeutic and counseling interventions, monitoring of outcomes, and coordination with care teams. ¹
The nutrition care process can be applied across a wide range of settings, from community, outpatient clinics, hospitals, private practice, long‐term care, telehealth, and more. A recent position paper ², released before publication in the Journal of the Academy of Nutrition and Dietetics, highlighted the effectiveness of MNT in the Prevention and Treatment of Chronic Diseases. They found that despite evidence of the benefit of RDN-delivered nutrition interventions for many chronic conditions, significant
barriers remain in reimbursement, referral processes, and access to care.
Coverage for MNT in the United States varies considerably by payer type. Federally, for Medicare Part B, MNT is covered when a beneficiary has diabetes, non-dialysis chronic kidney disease (stage 3-5), or has had a kidney transplant within the past 36 months. A Medicare-enrolled RDN can schedule and bill for services after obtaining a physician signed (MD or DO) referral, at this time mid-level providers currently do not qualify to sign MNT referrals for Medicare benefit. Medicare provides for up to three hours of MNT in the first year of referral and up to two hours in each subsequent year (with allowance for additional hours if deemed medically necessary). ³ As of January 2025, RDNs can also bill for Direct Training Caregiver Services, which means they can provide education and training to unpaid caregivers who help with tasks like meal preparation and wound care. ²
Medicaid programs are financed by both the state and federal governments, but each state can determine its own coverage and
reimbursement for specific services. State Medicaid programs exhibit significant variability in their coverage and reimbursement rates for MNT services. A recent mapping project by the Academy of Nutrition and Dietetics 4 found that while 37 states recognize MNT billing codes, in only 26 states can RDNs enroll as Medicaid providers (one additional state for pediatric services only), and in only 23 states can RDNs bill independently (others can bill incident-to services). Coverage for MNT services also varies, with some limiting depending on the diagnosis to other states providing reimbursement for a broad range of preventive and medical nutrition therapy. 5
Commercial insurance plans also vary widely in their benefit structure, with some limiting coverage while others extending beyond Medicare-covered diabetes and CKD to also include pre-diabetes, obesity, malnutrition, cardiovascular disease (including hypertension and dyslipidemia), cancer, eating disorders, gastrointestinal conditions, and more.
Although some plans have expanded their coverage, it is not universal and understanding coverage requires knowing an individual’s insurance plan benefits, the RDN network status, diagnosis and referral requirements, the number of covered visits/hours/units, medical or preventive benefit coverage, and, if applicable, telehealth eligibility. Benefits can change annually, and reimbursement rates can also vary widely depending on the state and payer.
When the Affordable Care Act was implemented in 2010 it help provide premium subsidies and increased coverage of preventive and chronic disease services. This led to an increase in MNT coverage expectation and waived share-of-cost for individuals receiving MNT. However, in practice, coverage remains patchwork, with substantial variability in approved diagnoses, covered hours, cost-sharing requirements, and provider networks across plans.
Coordinated care and collaboration are essential for managing chronic conditions, and timely referrals to MNT play a key role in this process. Deciding when to refer should follow disease or area-specific screening criteria (such as validated malnutrition screenings) or as per the Standards of Care in Diabetes, should occur at diagnosis, annually, and whenever treatment goals are unmet, complications develop, or significant life transitions take place. 6
While referral protocols can streamline MNT referrals, access to RDNs remains a challenge in many communities and is further complicated by the need to understand differences in Medicare, Medicaid, and commercial payer coverage so individuals can fully benefit from available services.
Healthcare providers can support individuals receiving care by helping them interpret their plan’s benefits, identify coverage barriers (including limited preventive coverage within Medicare and some Medicaid and commercial plans), and connect them to alternative or complementary resources such as Diabetes Prevention or DSMES programs, community health initiatives, or sliding-scale RDN services when MNT is not covered. Providers can also increase their awareness of policy and advocacy efforts to expand MNT benefit eligibility. ⁷ By working together, the entire care team can strengthen care coordination, enhance access to nutrition services, and support the implementation of MNT to improve our population’s health.
References:

JR has been diligently studying to take their CDCES exam at the end of January 2026. They are wondering if they should study the 2025 or 2026 ADA Standards of Care.
As a mentor to healthcare professionals entering the field of diabetes, what do you recommend?

SJ is 52 years old with a 10-year history of type 2 diabetes. They recently started on insulin degludec U-100 Flex Touch pen 15 units per day. At a follow-up visit, SJ brings their insulin pen and mentions they have been keeping it in their work bag since starting therapy. They are unsure how long they can continue to use this same pen.
What is the best advice for SJ for insulin storage in this situation?
For last week’s practice question, we quizzed participants on RT forgetting their insulin, and what would be the best response. 62.93% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question

JR was recently diagnosed with type 2 diabetes, but based on their history of pancreatitis, you suspect JR actually has Diabetes Type 3c.
Which of the following symptoms match a diagnosis of Diabetes Type 3c?
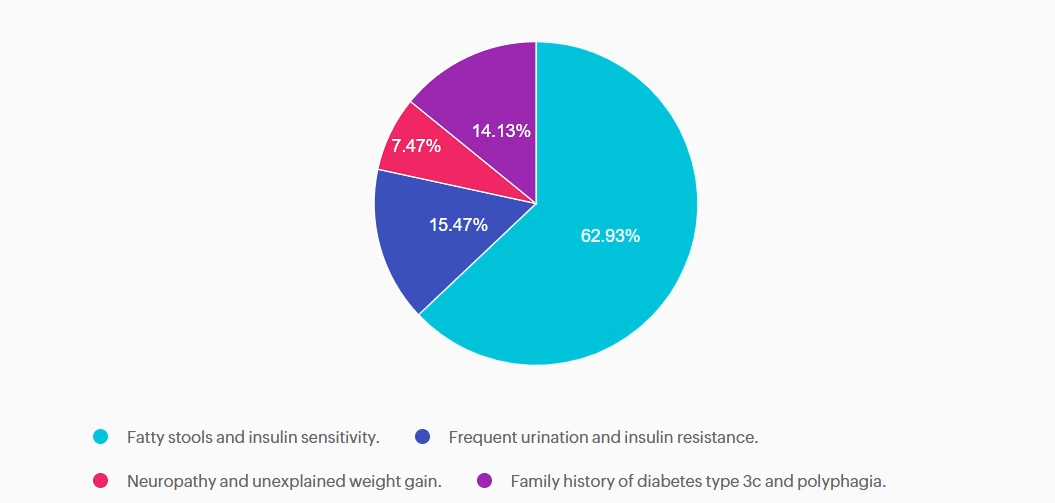
Answer A is correct: 62.93% chose this answer, “Fatty stools and insulin sensitivity.” Steatorrhea, or fatty stools, results from poor fat digestion due to insufficient pancreatic enzymes—a key feature of type 3c diabetes, with it’s hallmark exocrine enzyme insufficiency. People with diabetes type 3c, can also be very insulin sensitive, since they don’t have the insulin resistance associated with type 2 diabetes. In addition to diabetes medications, they may benefit from pancreatic enzyme replacement therapy (PERT) to improve absorption of fatty foods and decrease steatorrhea.
Answer B is incorrect: 15.47% chose this answer, “Frequent urination and insulin resistance.” Frequent urination and insulin resistance is associated with type 2 diabetes. With type 3c, since many of the beta cells are destroyed due to trauma not genetics, these individuals may have polyuria from hyperglycemia, but they are not usually insulin resistant, just deficient.
Answer C is incorrect: 7.47% chose this answer, “Neuropathy and unexplained weight gain.” They may get neuropathy if their blood glucose is elevated for a long period of time, but that is not part of the differential. People with type 3c usually experience weight loss due to the lack of pancreatic enzymes that help with nutrient absorption.
Answer D is incorrect: 14.13% chose this answer, “Family history of diabetes type 3c and polyphagia.” Type 3c diabetes is not passed on through genes, it is due to exocrine damage to the pancreas which can lead to destruction of beta cells. Most common causes of diabetes type 3c include pancreatitis, cystic fibrosis, pancreatic cancer, and hemochromatosis. Some people could experience extreme hunger if their glucose levels are elevated for an extended period of time.
We hope you appreciate this week’s rationale! Thank you so much for taking the time to answer our Question of the Week and participate in this fun learning activity!
The holiday season can bring joy—but also stress, disrupted routines, late nights, and rich meals that may affect blood glucose levels and emotional well-being. For people with diabetes, this time of year can stir feelings of self-doubt and distress, especially if glucose levels veer outside their usual target range.
To help you and your community feel more grounded, we’ve created two helpful resources:
🎁 Holiday Survival Guide
This handout offers 10 practical strategies to stay balanced and navigate holiday gatherings with confidence. Even trying just one or two of the suggestions can make a big difference.
💡 Reframe & Reset: Coping with Diabetes Distress
This companion sheet provides tools to recognize, reframe, and release feelings of shame, guilt, or overwhelm that can surface during the holidays—and beyond.
These printable Cheat Sheets are designed for easy sharing with your friends, clients, and colleagues. Feel free to distribute widely—they’re full of tips to promote self-compassion, support balanced choices, and bring more ease to the season.


1. Be a sleep warrior – People living in the United States are chronically underslept. Not getting enough sleep is associated with increased hunger, higher blood sugars, poor concentration, frequent illness, and impaired problem-solving. Make sure to give yourself the gift of at least 7 hours of sleep a night. This sleep will help you make the best choices for your health and will protect against illness and fatigue. You got this.
Goal: Get at least 7 hours of sleep a night. You deserve it.
2. Keep active – Holidays can put our exercise plans to the test, but we have a few ideas for you. Take an after-meal stroll instead of plopping on the couch. After meal walks lower post-meal blood sugars and increases energy by getting muscles activated. Just 10 minutes of walking after meals can make a big difference. You can even put music on and have a small dance session, anything to get your body moving.
Goal: Work toward 30 minutes of activity a day.

3. Don’t forget the Fiber – With all the snacks and tempting foods, whole healthy foods may take a back seat. Enjoy the abundance of seasonal vegetables, fruits, nuts, and grains that are fiber-rich and that decrease inflammation. Examples include; yams, squash, mandarin oranges, almonds, pistachios, quinoa, kale, brown rice, warm oatmeal, salads, and broth-based soups.
Goal: Strive to eat at least 25gms of fiber a day.

4. Enjoy the ultimate beverage – H20. Water is the perfect way to keep hydrated, replenished, and keeps appetite in check. Add a splash of flavor with a jigger of fruit juice or fresh cucumbers, lime slices, or a sprig of rosemary. Be creative. Sparkling waters come in a vast variety of flavors, are calorie-free, and contain no artificial sweeteners.
Goal: Keep hydrated by enjoying plenty of water.
5. Keep an eye on alcohol – While it’s true that red wine offers a beneficial anti-inflammatory compound called resveratrol, drinking too much alcohol can lead to unintended outcomes. Studies show that we make poorer food choices if alcohol is on board. This can offer special challenges in party settings, where temptations are abundant. A drink of alcohol contains about 100 calories and mixed drinks have even more. In addition, alcohol can lead to low blood sugars, especially for those taking insulin or sulfonylureas.
Goal: Limit alcohol to one drink a day for women, two drinks a day for men.

6. You are already sweet enough – Holidays and sugar go hand in hand. If possible, try and eat less than 6 teaspoons of added sugar (does not include natural sugars found in fruit and milk). This goal may not be realistic on all days, but aim for success most of the time. Excess sugar intake can cause inflammation and buildup of fat in the liver. One strategy is to limit sugar intake during the day and save your 6 teaspoons for that special dessert or parties. When looking at labels, it is helpful to know that 1 teaspoon equals 4 gms of sugar.
Goal: Limit sugar to 6 teaspoons a day.

7. Your teeth need extra special attention – Taking care of our teeth and gums improves health. Gum inflammation is associated with blood vessel inflammation. Swollen gums can also lead to an increase in blood sugars. During the holidays, find time for regular oral hygiene. Your mouth (and dental team) will thank you.
Goal: Brush teeth at twice daily and floss at least once daily.
8. Keep connected to friends and family who love you just the way you are! – As enjoyable as holidays can be, reuniting with family can also cause stress and stir-up emotions. Feeling out of sorts can lead to stress eating and decrease self-care. If possible, reach out to a trusted friend to share your feelings or keep a holiday journal. Consider bringing a favorite book along during your travels that you find inspiring and comforting. Give yourself permission to steal away for some quiet time.
Goal: Self-care is important during the holidays.
9. Enjoy an Oxygen Cocktail – Studies show that when humans venture into natural outdoor settings, heart rate and blood pressure improve. Take a moment to appreciate the feeling of the air on your skin, take a deep breath of fresh air, try to find nests in leafless trees, listen to the animal sounds and bird songs and just enjoy that moment.
Goal: Step into nature daily.
10. Take inventory of things that you are grateful for – Find a moment each day to reflect on a few things that brought you joy or good feelings. Maybe it was your cousin who lent you her favorite sweater. Or an Aunt who gave you the best hug. Special moments with a best friend or an after-dinner walk enjoying the fall leaves. These small moments of connection and beauty are one of the most treasured gifts of the holiday season that linger in our hearts and memory long after we say our goodbyes.
Goal: Take note of special moments.

I love this time of year because we get to celebrate you, the hard-working and dedicated diabetes healthcare professionals.
To allow more healthcare professionals to join the Diabetes Education and Care Specialist community, we have expanded our accreditation.
With our evidence-based courses, we are now providing CEs for physicians, nurses, dietitians, and pharmacists. We want to make sure that anyone who wants to enter the field of diabetes has ample opportunity.
Thank you so much for the lives you touch every day.
Coach Beverly, Bryanna, Astraea & Katarina

Grace is a 38-year-old female who has lived with type 1 diabetes for 20 years. She is a nurse and works variable shifts. She voices concern today about her hemoglobin A1c being elevated at 8.4% over the past 6 months. She is doing everything she can to manage her diet, daily exercise routine, and reports rarely missing insulin doses. She is currently using a Dexcom G7 CGM.
She has never pursued insulin pump therapy because she was fearful that she would no longer be in control of her diabetes if she used a pump. She is now interested in an automated insulin delivery system and asks you which pump is “best” for controlling blood sugar.
What is the best way to answer this question?
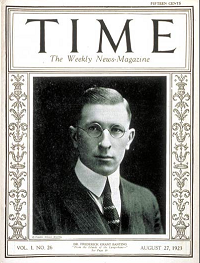
Dr. Banting was born on November 14, 1891. That is why we celebrate World Diabetes Day on November 14th.
On October 25th, 1923 the Nobel prize in physiology or medicine was awarded to Frederick Grant Banting and John James Richard MacLeod “for the discovery of insulin”. The discovery was made in 1921, which makes the two-year time period between the detection and this prize one of the shortest in the history of the Nobel Prize.

During a hot summer in 1921, Dr. Banting secured space to test out his theory in the University of Toronto. Along with his colleague, Charles Best, and a bare bones lab, they conducted dozens of experiments on dogs, which ultimately led to the discovery of insulin.
Dr. Banting and Charles Best began their experiments ligating the pancreases of dogs, thinking this would prevent destruction by the digestive pancreatic juices, and then isolating the extract from the islet cells. They then processed the extract from the islet cells and injected this extract they called “insulin” into diabetic dogs. According to an audio Interview with Dr. Best, by July 1921, they had 75 positive examples of insulin lowering blood glucose levels in dogs.

In February 1922, doctor Frederick Banting and biochemist John Macleod published their paper on the successful use of a alcohol based pancreatic extract for normalizing blood glucose levels in a human patient.
Here are some photos of the first insulin bottles produced by the University of Toronto and Eli Lilly.
Soon, word of their discovery got out and the race was on to produce enough insulin to treat the flood of type 1 patients arriving in Toronto to receive this miracle injection.
First Children to Receive Insulin

The first patient to receive insulin was a ‘welfare’ case at Toronto General Hospital – no clinical trial structure to say the least. People from Canada/US flooded into Toronto to receive treatment. Banting struggled with the lack of accessibility of insulin – volume needed and issues of purification.
The earliest patients were “selected”, some youths from Canada/US, some soldiers with diabetes (probably because of Banting’s service in the First World War) and then later some select private patients. During this time they were working hard to increase the volume and continue to improve the purification process. Insulin was available for testing in US, namely through Dr. Elliot Joslin in the late summer 1922.
Dr. Banting – Fun and Interesting Facts
Takes a Team
While Best played a critical and important role, credit must also go to Professor Macleod, from the University of Toronto, who provided the lab space, showed Dr. Banting how to operate on dogs, provided his student Best and suggested they switch from a saline to alcohol to purify the ‘extract’. Dr. Macleod also secured the support of JB Collip, the 4th man on the team and the fist person to purify insulin for human use. Best is also known for pushing Banting to return to the research during a particular dark period of failure.
Historical Insulin Powerpoint Slides – here is a collection of some of my favorite powerpoint slides, depicting the discovery of insulin.
Visit Banting House Facebook Page
Canadian Broadcast that highlights the first patient, Ted Ryder, the first patient to receive insulin from Dr. Banting. Some great historic video footage of Dr. Banting shaking hands with the young man..
The Quest – 1958 This short film is a re-enactment of the critical year in Dr. Frederick Banting’s life when he discovered insulin for the treatment of diabetes at the University of Toronto. It depicts the odds against which he and his assistant, Charles Best, worked; the scepticism of other doctors and the final victory that gave thousands of diabetics hope for a healthier life.
The Flame – Banting House Historical Site Newsletter