
Subscribe
eNewsletter

Ready to get certified?
Free CDCES Coach App
Download
Free Med Pocket Cards
Welcome to our first 2023 Question of the Week. We decided to freshen up some of our images and are excited to share our new purple light bulb graphic for Question of the Week. Thanks for joining us and Happy New Year.
The clinic where JR works as a Diabetes Specialist wants to set up a screening program to identify people with undiagnosed prediabetes or diabetes based on risk status. According to the 2023 ADA Standards of Care, which of the following indicates that an individual is at increased risk of having prediabetes and diabetes and needs further testing?
Click Here to Test your Knowledge
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
All hours earned count toward your CDCES Accreditation Information
Join us live on February 2, 2023, at 11:30 am PST for our
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the 2023 updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
The new ADA 2024 Standards of Care include dozens of updates to diabetes clinical practice.
Which of the following statements has actually been added to the ADA 2024 Standards of Care?
Click Here to Test your Knowledge
Topics:
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other healthcare providers interested in staying up to date on current practices of care for people with prediabetes, diabetes, and other related conditions.
Can’t make it live? No worries. We will send post the recorded version to the Online University within 24 hours of the broadcast
Instructor: Beverly Thomassian RN, MPH, CDCES, has been Board Certified in Advanced Diabetes Management for over 20 years. She is an Associate Clinical Professor at UCSF, a working educator, and a nationally recognized diabetes expert. She has a Master’s Degree in Public Health from UCLA, with a focus on behavioral health and education.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
For last week’s practice question, we quizzed the new ADA 2023 standards on hypertension. 48% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
The new 2023 ADA Standards of Care are out, and they include several important clinical updates that are critical for our practice and certification exams.
What best represents the updated definition of hypertension in the 2023 Standards?
Answer Choices:
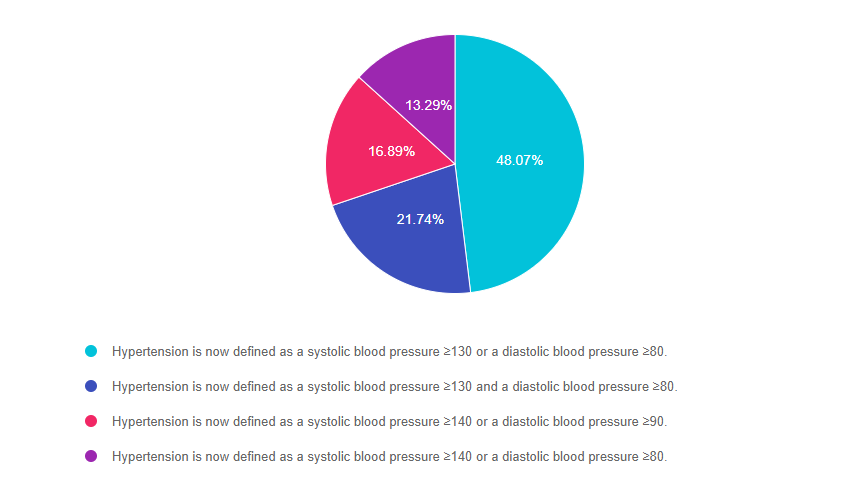
Answer 1 is correct. 48.07% chose this BEST answer – GREAT JOB. According to Standard 10, Cardiovascular Disease and Risk Management, hypertension is now defined as a systolic blood pressure greater than or equal to 130 or a diastolic blood pressure greater than or equal to 80. This is in agreement with the definition of hypertension by the American College of Cardiology and American Heart Association. People with diabetes and hypertension qualify for antihypertensive drug therapy when the blood pressure is persistently elevated and is greater than or equal to 130/80. The on-treatment target blood pressure goal is less than 130/80, if it can be safely attained.
Answer 2 is incorrect. 21.74% of you chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 130 and a diastolic blood pressure greater than or equal to 80.” This is so close to being the being the best answer, but it is not accurate. If either the diastolic or systolic pressure meet the cut-off, the person is considered to have a blood pressure reading that is above target.
Answer 3 is incorrect. 16.89% of respondents chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 90.” This was the definition of hypertension in the 2022 and older standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Finally, Answer 4 is incorrect. 13.29% chose this answer, “Hypertension is now defined as a systolic blood pressure greater than or equal to 140 or a diastolic blood pressure greater than or equal to 80.” This is a blending of hypertension definition from the 2022 and 2023 standards. The 2023 definition of hypertension is blood pressure equal to or greater than 130/80.
Thank you so much for reading this “Rationale of the Week”.
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES and BC-ADM Certification Accreditation Information
As the shortest day of the year, Winter Solstice marks a turning point in the rhythms of life. Tomorrow, the sun will start shining longer and longer each day, bringing increased illumination and the promise of new growth and hope. Thank you for being a messenger of hope and light for people living with diabetes. Love, Coach Beverly
“Make of yourself a light,”
said the Buddha,
before he died.
I think of this every morning
as the east begins
to tear off its many clouds
of darkness, to send up the first
signal — a white fan
streaked with pink and violet,
even green.
An old man, he lay down
between two sala trees,
and he might have said anything,
knowing it was his final hour.
The light burns upward,
it thickens and settles over the fields.
Around him, the villagers gathered
and stretched forward to listen.
Even before the sun itself
hangs, disattached, in the blue air,
I am touched everywhere
by its ocean of yellow waves.
No doubt he thought of everything
that had happened in his difficult life.
And then I feel the sun itself
as it blazes over the hills,
like a million flowers on fire —
clearly I’m not needed,
yet I feel myself turning
into something of inexplicable value.
Slowly, beneath the branches,
he raised his head.
JR has a bunch of insulin pens at home and is wondering if they are still good to use. Most of the unopened insulin pens are stored in the fridge, but JR has 2 degludec (Tresiba) pens that they left out of the refrigerator by accident. They ask you if they are still good.
What is the most accurate response for the shelf life of degludec (Tresiba) pens stored at room temperature of up to 86 degrees Fahrenheit?
Click Here to Test your Knowledge
This bundle includes our CDCES Online Prep Bundle (featured above) plus the ADCES Review Guide – 5th Edition-Revised. The online bundle includes Level 1, Level 2, and Level 3 (Boot Camp), plus two bonus courses. The ADCES Review Guide offers over 480+ practice questions and is a fantastic independent study tool and comprehensive resource for the Diabetes Care and Education Specialist Exam.
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.
For last week’s practice question, we quizzed test takers on Rezvoglar insulin. 75% of respondents chose the best answer. We want to clarify and share this important information, so you can pass it on to people living with diabetes and your colleagues, plus prepare for exam success!
Before we start though, if you don’t want any spoilers and haven’t tried the question yet, you can answer it below: Answer Question
Question:
RZ takes 30 units of glargine (Lantus) each night. However, when they went to the pharmacy to pick up their prescription, they received glargine insulin Rezvoglar instead of their usual Lantus.
RZ asks how the pharmacy can give them a different brand of insulin without checking first? After addressing their emotional response, you provide the following, most accurate Information.
Answer Choices:

Answer 1 is incorrect. 12.73% chose this answer, “Rezvoglar is the generic version of (glargine) Lantus.” This is a very tempting answer, but since insulin is a biologic medication, (biologic medications are large, complex molecules, often made from living cells or tissue) the term “generic” is replaced with “biosimilar”. In addition, the better answer below is more accurate, and offers additional information.
Answer 2 is correct. 74.97% of you chose this answer, “Rezvoglar is an interchangeable biosimilar insulin.” YES, GREAT JOB. The FDA just announced that Rezvoglar has also been approved as an interchangeable biosimilar along with Semglee. An “interchangeable biosimilar,” means that pharmacists can substitute a person’s Lantus prescription with these cheaper alternatives without needing to consult the healthcare prescriber.
Answer 3 is incorrect. 9.17% of respondents chose this answer, “Rezvoglar can not be switched for glargine (Lantus) without provider approval.” With recent FDA approval, Rezvoglar is now an “interchangeable biosimilar,” which means that pharmacists can substitute a person’s Lantus prescription with this cheaper alternative without needing to consult the healthcare prescriber.
Finally, Answer 4 is incorrect. 3.13% chose this answer, “Rezvoglar is a rapid-acting human biosimilar insulin analog.” Rezvoglar is the biosimilar of basal insulin glargine.
Thank you so much for reading this “Rationale of the Week”.
Newly Approved Biosimilar Interchangeable Basal Insulin – PocketCard Update
Under basal insulin glargine, there are now 3 biosimilars listed; Basaglar, Semglee and Rezvoglar. The FDA just announced that Rezvoglar has also been approved as an interchangeable biosimilar along with Semglee. An “interchangeable biosimilar,” means that pharmacists can substitute a person’s Lantus prescription with these cheaper alternatives without needing to consult the healthcare prescriber.
Get Your Own PocketCard
These updates are now posted on the latest version of our Insulin PocketCards, which are available for FREE download, or on our CDCES Coach App. You can also purchase your very own 2023 laminated version and they make perfect gifts for team members.
This bundle is specifically designed for healthcare professionals who want to learn more about diabetes fundamentals for their clinical practice or for those who are studying for the Certified Diabetes Care and Education Specialist (CDCES) exam.
Intended Audience: This library of critical information is designed for individuals or groups of diabetes specialists, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with diabetes and preparing for the CDCES Certification Exam.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES Accreditation Information
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.

The new 2023 ADA Standards of Care are out, and they include several important clinical updates that are critical for our practice and certification exams.
What best represents the updated definition of hypertension in the 2023 Standards?
Click Here to Test your Knowledge
This course, updated annually, is an essential review for anyone in the field of diabetes. Join Coach Beverly as she summarizes the updates to the American Diabetes Association’s Standards of Medical Care in Diabetes and provides critical teaching points and content for healthcare professionals involved in diabetes care and education.
Objectives:
Intended Audience: This course is a knowledge-based activity designed for individuals or groups of diabetes professionals, including RNs, RDs, Pharmacists, Nurse Practitioners, Clinical Nurse Specialists, Physician Assistants, and other health care providers interested in staying up to date on current practices of care for people with prediabetes, diabetes and other related conditions.
Don’t worry if you can’t make it live. Your registration guarantees access to the recorded version in the Online University.
All hours earned count toward your CDCES and BC-ADM Certification Accreditation Information

We decided to get a little personal and share some tenderness, alongside our newsy pieces, for this month’s newsletter.
For Coach Beverly, three words come to mind when she considers her family and business this year: reopening, celebration, and reflection. In her article, Beverly shares insights on the evolution of her company and her family over the past 24 years, including a historical photo of her first-ever Medication PocketCard.
Bryanna shares news on her two recent adoptees, Biscuit and Muffin. They are each adorable in their own way, and Bryanna hopes that they will eventually bring out the best in each other.
We welcome Andrew, a nursing student and new team member to our Diabetes Education Services family.
On the news front, we made significant changes to the timing section of our Insulin Medication PocketCards. We have also added Rezvoglar to the Lantus biosimilar list.
You’re invited to take the Question of the Week and read about the ADA/EASD consensus report with our Rationale of the week.
Finally, we want to turn the spotlight on you! We are forever grateful for your willingness to support and believe in a young Diabetes Specialist who had the vision to create a company that uplifts people with diabetes through a blend of science and compassion.
To thank you, our amazing community of diabetes educators and advocates, we will be celebrating our 25th Anniversary throughout 2023 with special events and giveaways. We can’t wait!
In celebration,
Coach Beverly and Bryanna
Featured Articles
FREE Resources
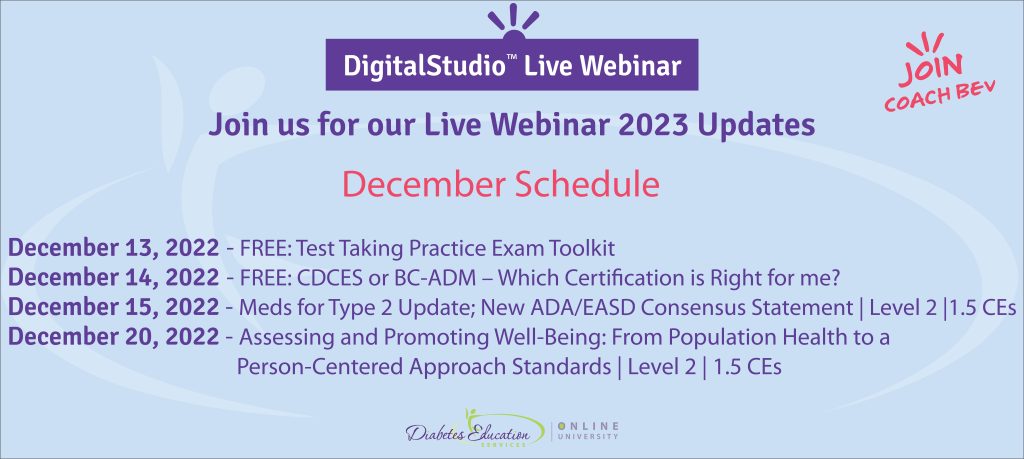
December 13, 2022 – FREE: Test Taking Practice Exam Toolkit
December 14, 2022 – FREE: CDCES or BC-ADM – Which Certification is Right for me?December 15, 2022 – New ADA/EASD Meds Consensus Update| Level 2 |1.5 CE’s
December 20, 2022 – Assessing Well-Being: A Person-Centered Approach | 1.5 CEs
Sign up for Diabetes Blog Bytes – we post one daily Blog Byte from Monday to Friday. And of course, Tuesday is our Question of the Week. It’s Informative and FREE! Sign up below!
The use of DES products does not guarantee the successful passage of the CDCES exam. CBDCE does not endorse any preparatory or review materials for the CDCES exam, except for those published by CBDCE.